4. Discussion
This study of IHD mortality, prevalence, incidence, and rates of medical interventions over three decades revealed pronounced differences between new and old Mediterranean EU country members.
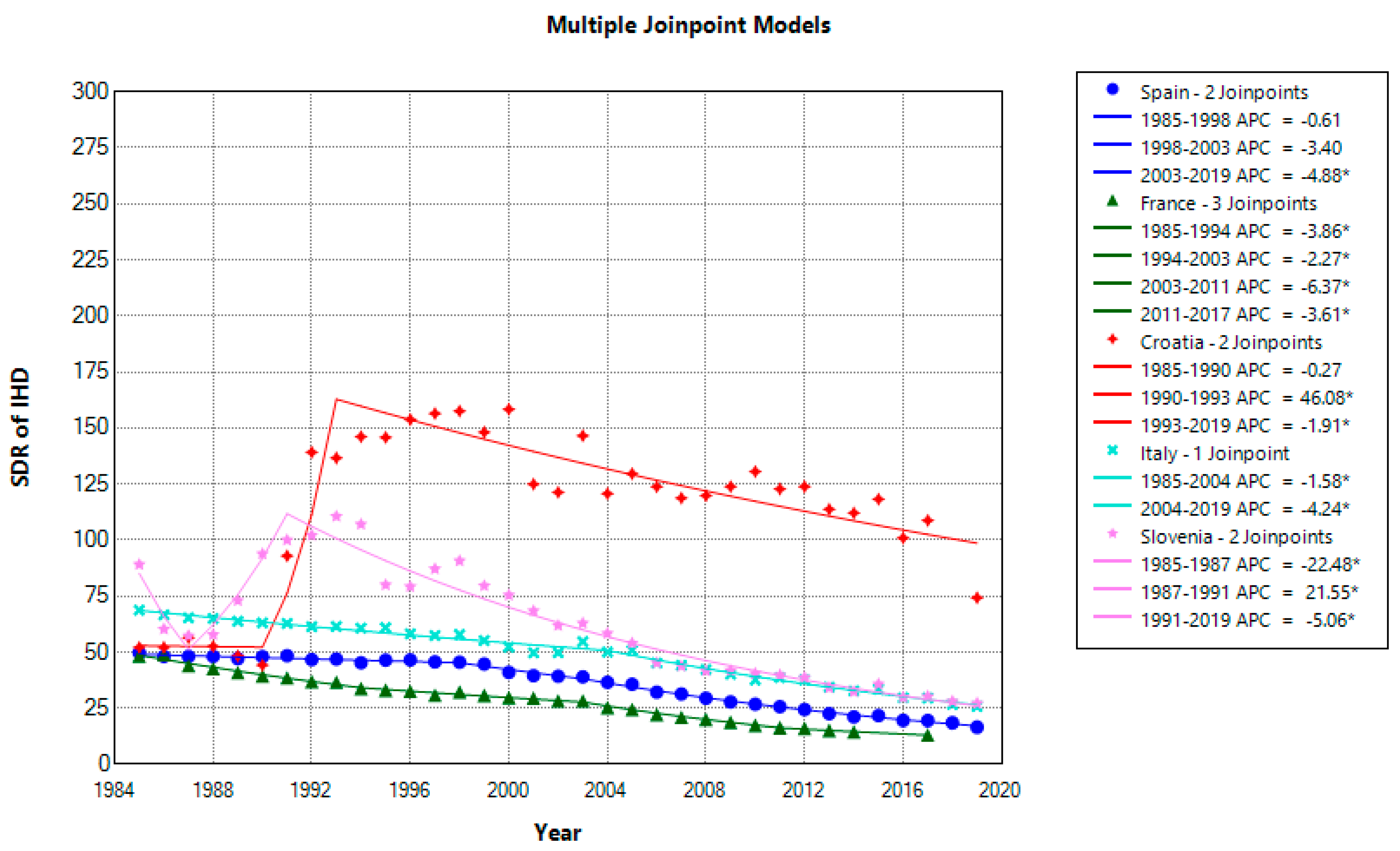
Female IHD mortality has significantly decreased from 1985 to 2019 in all countries except Croatia (+1.85%). The extent and patterns differ. France had the highest average reduction (AAPC) at −4.01%, while Italy had the lowest at −2.76%. Croatia and Slovenia had irregular patterns and upward IHD trends that could have been attributable to massive political, social, and healthcare changes accompanied by war. Nonetheless, potential changes in coding practice also cannot be excluded (
Figure 1 and
Figure 2). The comparison of mean mortality rates among females over the last ten years showed a significantly higher rate in Croatia (112.92) than in Slovenia (33.66), Italy (32.63), Spain (21.65), and France (17.49). France and Spain had similar rates, as well as Italy and Slovenia, which, as opposed to Croatia, narrowed the gap with old EU country members in female IHD mortality.
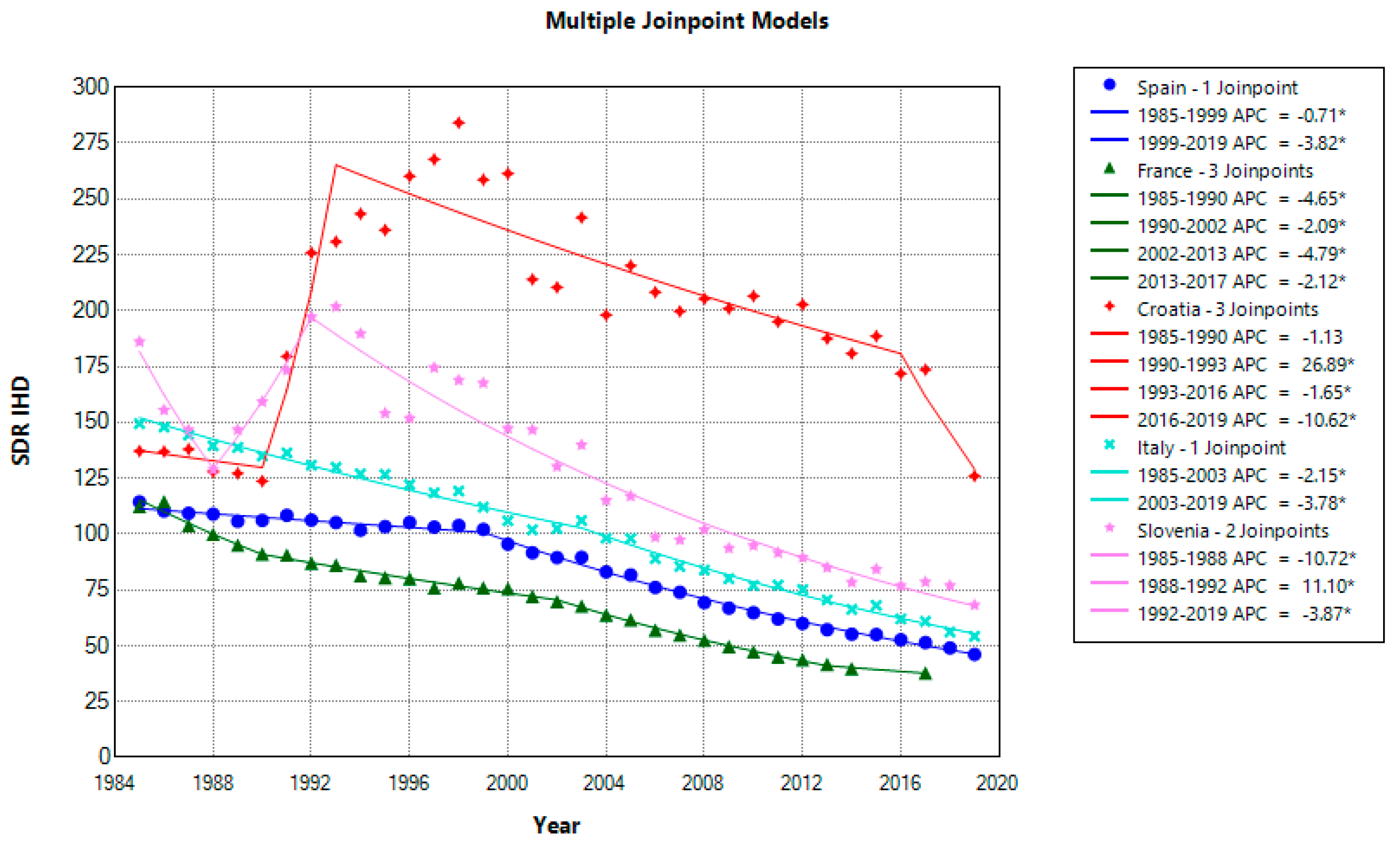
Male mortality has also significantly decreased in all countries except Croatia, with a negligible and non-significant reduction of −0.18%. As in the case of female IHD mortality, France had the highest average decrease over the 1985–2019 period of −3.43%. Within the last decade, Croatian males had a significantly higher mortality (183.38) compared to males in Slovenia (82.46), Italy (66.78), Spain (55.38), and France (46.97). Still, Slovenia managed to reduce the gap but less successfully compared with the reduction in female IHD mortality.
Moreover, comparing the IHD mortality data for new country members, Slovenia and Croatia, for 2019 vs. 1991, showed significant between-country differences. While Slovenia considerably reduced mortality for females and males by −72.85% and −60.60%, this reduction in Croatia was much lower, at −29.80% for males and −20.10% for females. These differences can be explained by unsuccessful Croatian healthcare reforms, which systematically neglected politically sensitive aims. Health efficiency still represents a significant healthcare system problem [
17]. Although the EU makes considerable effort to equalize health care across country members, distinctions deep-rooted in their historical, political, socioeconomic, and health traditions remain prominent. Cardioprotective Mediterranean heritage in the form of diet and lifestyle seems lost in transition, and the East–West health gap is still visible. Croatia has 5.6-fold higher IHD mortality for females and 3.3-fold higher IHD mortality for males compared to France. Despite the short coastline, the French paradox most likely contributed to the lowest mortality among all analyzed countries. Yet, the term Croatian paradox was also coined to address high CVD mortality, which is more similar to that in CEE than in Mediterranean countries [
18,
19] (
Figure 1 and
Figure 2).
The excess of male IHD mortality is expected, and male-to-female ratios ranged from 2.88 in France to 1.70 in Croatia. Male disadvantages can partly explain such variations, but smoking might have a crucial role. More harmful effects of smoking on females narrowed the ratio and often are overlooked. In many European countries, male smoking is declining and/or has reached a plateau, whereas female smoking is increasing [
20]. Besides smoking, sex-specific mortality differences also cannot exclude potential health disparities regarding prevention, diagnosis, treatment strategies, and cardiovascular outcomes [
21,
22].
Countries with a decline in IHD mortality efficiently control major risk factors and provide better medical care but also address relevant political, economic, and social determinants [
23]. Various models consistently indicate that risk factor reduction explains a more significant proportion of mortality decline than medical treatments [
24]. In general, prevention confirmed its effectiveness, and modelling studies suggested that 50–60% of the decrease in IHD mortality in Europe is attributable to prevention strategies at both population and individual levels [
25,
26]. Primordial prevention seems incredibly demanding since social determinants extend outside the health sector. Studies suggest that social factors are equally important as traditional risk factors such as smoking, dyslipidemia, and hypertension [
27,
28]. In high-income countries, a steady decline in IHD mortality since the 1980s has been attributed to primary and secondary prevention. However, the effects of prevention may hardly be distinguishable within the CV risk continuum [
1,
29]. Cardiac rehabilitation, pivotal in secondary prevention, is often neglected, with a fragmented uptake across Europe [
30]. Secondary prevention is focused on mortality reduction among cardiac patients as opposed to primary prevention, which largely reduces the incidence of IHD.
Hypertension, increased cholesterol levels, BMI, and high fasting glucose remain the most important metabolic risk factors for the reduction in IHD mortality [
29,
31]. High systolic blood pressure mostly contributed to CVD mortality in both genders, more in Central than in Western Europe, at 62% vs. 51% in males and 60% vs. 50% in females, respectively. High total cholesterol levels, positioned second for both genders, contributed 20% to 30%. High BMI and high fasting glucose plasma, each responsible for around 20% or less of the CVD mortality burden, were ranked last [
32]. Still, their relative contribution is complex, and significant between-country variations indicate an urgent need for further country-specific studies. Croatia’s highest IHD mortality among analyzed countries is most likely also mainly attributable to hypertension. Insufficient awareness and lack of a formal public health policy, inadequate health promotion, failure to invest in prevention, underdiagnosed and undertreated patients made hypertension one of the most urgent public health problems [
33]. According to the hypertension prevalence, Croatia is among the top-ranked countries in the world [
34,
35].
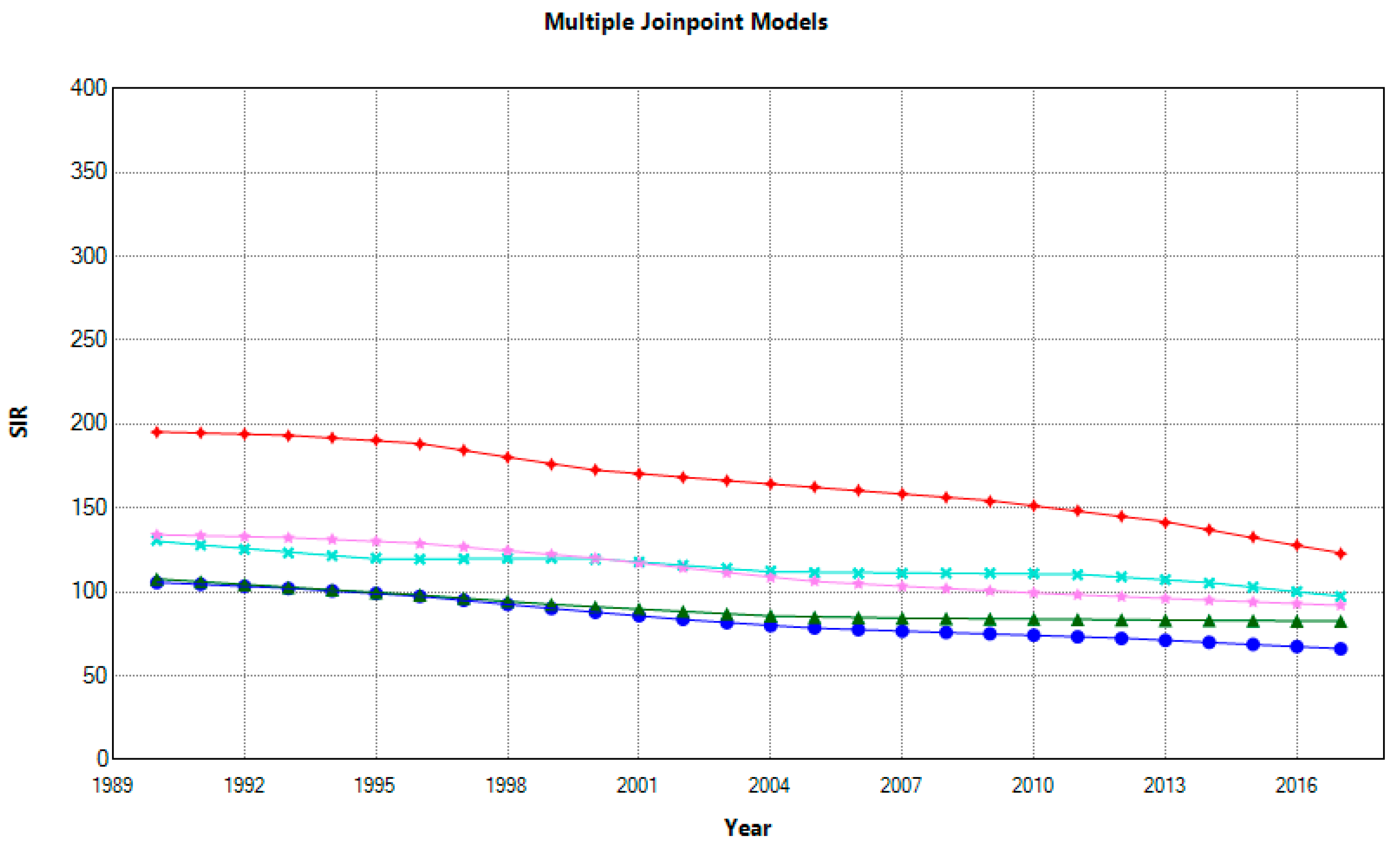
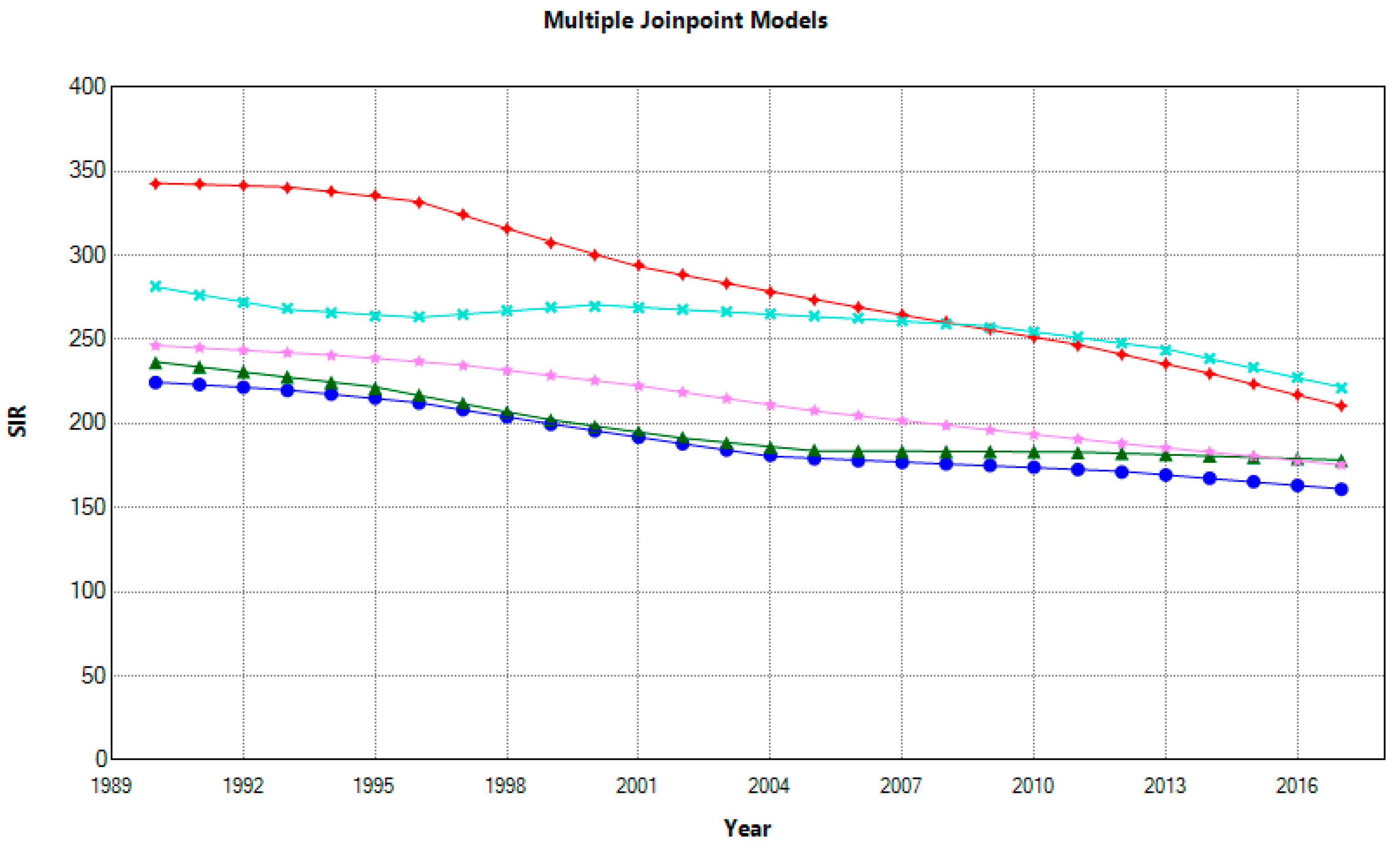
Morbidity measures such as incidence and prevalence also describe the dynamic of disease in the population. All countries decreased incidence, and AAPCs ranged for females from −23% in France to −37% in Croatia and Spain and males from −21% in Italy to −39% in Croatia. In 2017, for females and males in Croatia vs. Spain, high-to-low ratios were 1.85 and 1.3, respectively. Nonetheless, a dynamic pattern of decreasing trends for females narrowed the gap between first-ranked Croatia and second-ranked Italy. Furthermore, over two decades, the incidence rate reduction for males changed, where Croatia lost the disadvantageous first place, subsequently replaced by Italy (
Figure 3). However, despite the SIR reduction, between-country differences for females remained significant. At the same time, males in Croatia and Italy, as well as France and Slovenia, had similar rates. (
Figure 4)
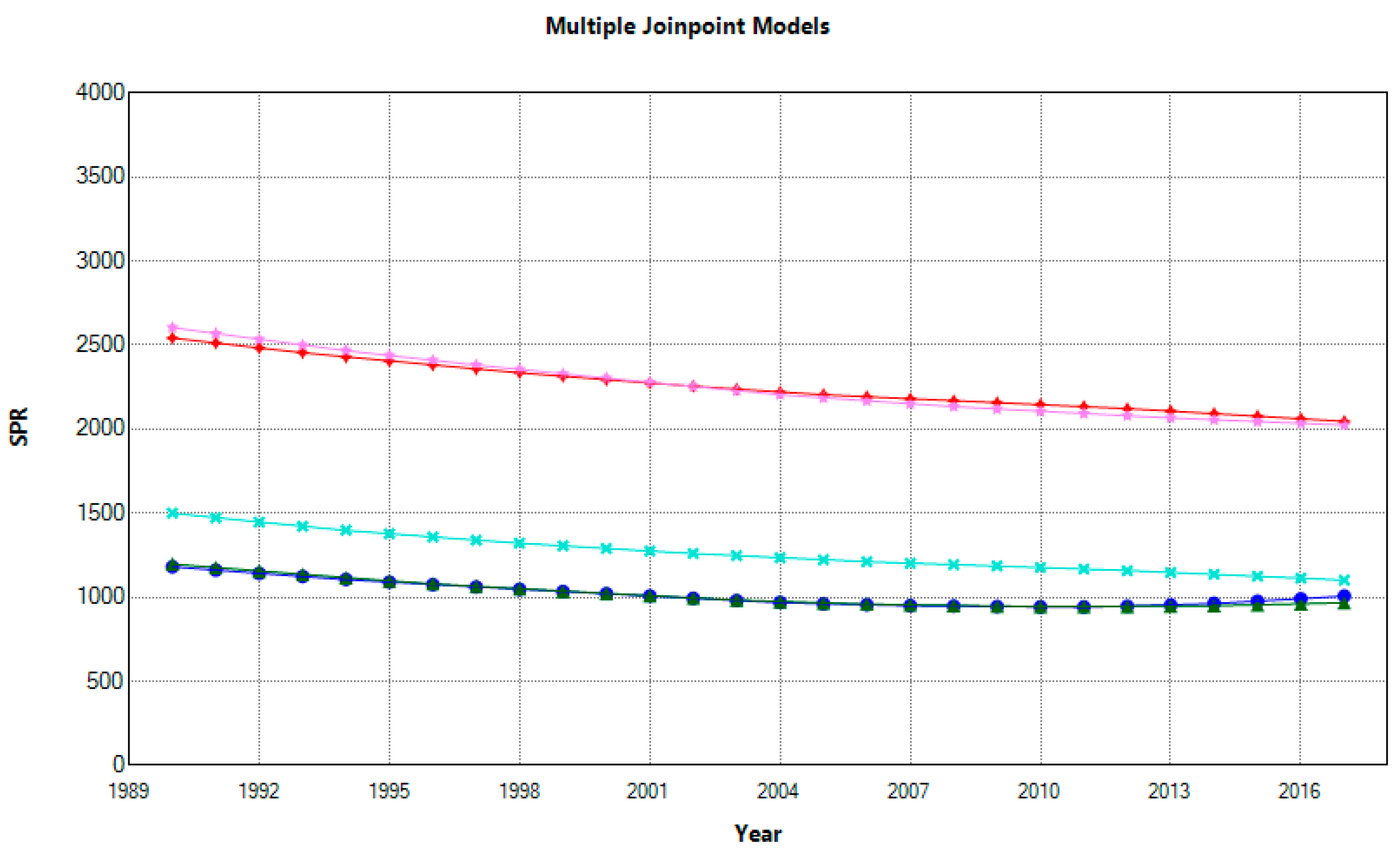
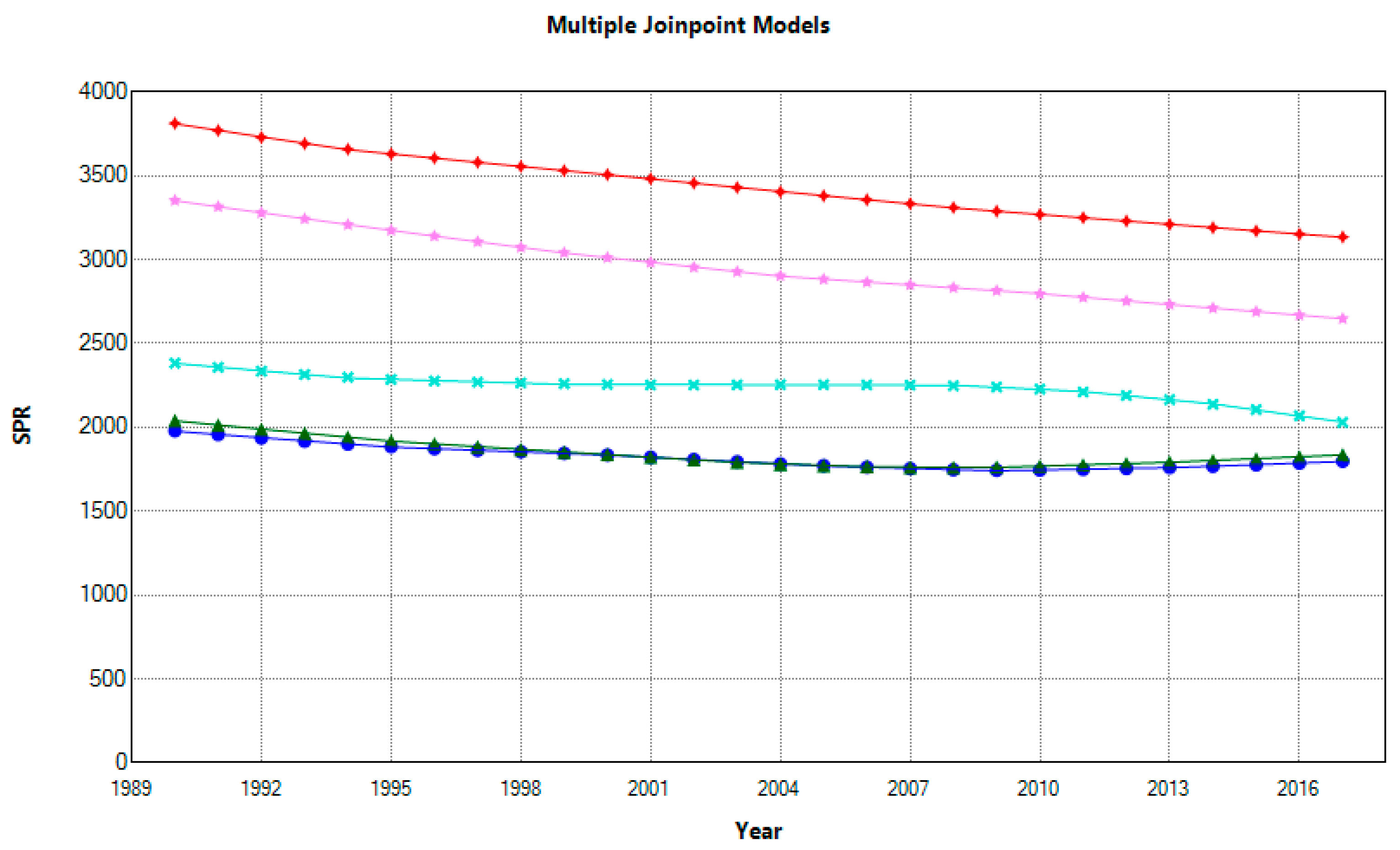
The negative trend in prevalence, as opposed to incidence, is relatively uniform for both genders. As indicated, AAPCs for females ranged from −0.59% in Spain to −1.13% in Italy, and males from −0.35% in Spain to −0.87% in Slovenia (
Figure 5 and
Figure 6).
Compared with 1990, the SPR percentage change for females ranged from −15% in Spain to −27% in Italy and for males from −9% in Spain to −21% in Slovenia. There are considerable differences in disease burden among countries, and in 2017, Croatia had the highest SPR with a high-to-low ratio for females of 2.11 compared to France, and a ratio of 1.74 for males compared to Spain. During the last decade, Croatian and Slovenian females had significantly higher SPRs than females in other analysed countries. Still, Slovenian males had significantly lower rates than Croatian males. As a measure of disease burden, the prevalence is not the most appropriate way to measure the effect of risk factors. Nonetheless, it can help assess healthcare needs and assist with the future planning of healthcare services and interventions [
36].
CABG and TCA rates also substantially varied between countries over the 2011–2019 period. Old EU country members, namely Italy, Spain, and France, had negative AAPC of CABG rates by −1.8%, −1.5%, and −0.2% in contrast to an increase in Slovenia (+0.9%) and Croatia (+3.2%) (
Figure 7). Differences in average CABG rate were significant, and the high-to-low ratio for Croatia vs. Spain was 3.5-fold. The Croatian CABG rate, previously reported as one of the highest in the EU, exceeded those of OECD countries [
37]. Croatia increased the CABG rate from 1994 to 2002 by as much as 6-fold and reached the Slovenian level in 2002 [
38]. Although the number of cardiac surgery centers improved, this cannot solely explain such an increase. Fragmentation of hospital care and lack of mandatory data collection enable the precise evaluation of appropriate indications.
All countries had increased TCA rates, and the AAPC ranged from +0.6% (Spain) to +11.4 (Croatia), with a high-to-low ratio 3.19 (
Figure 8). Such increased TCA utilization in Europe has been previously described [
39]. It is partly attributable to the higher disease burden and worldwide growth of interventional cardiology, as well as broader indications and benefits of TCA, such as less invasiveness and improvements in stent technology. Individual clinical data could explain the contributions of severity of disease per country, but they are not available at the national level. The striking increase in Croatia can partly be explained by the higher availability of technological and human resources, patient preferences, the extent and application of specific non-invasive diagnostic procedures that enhance downstream testing, and the implementation of evidence-based guidelines [
40]. In the 1990s and early 2000s, Croatia faced a shortage of invasive cardiologists and equipment, but nowadays, interventional cardiology services are widely employed in public and private settings [
41]. Still, evaluation of treatment effectiveness and clinical outcomes, especially those from medium to long-term post-TCA periods and hospital mortality rates, are not routinely available. Nevertheless, the appropriateness of TCA indications and the extent of potential overutilization in clinical practice is the first to be addressed. There is a worldwide trend of overuse, but similar studies in Croatia have not been conducted [
42]. In Italy, the rate of inappropriate TCA and coronary angiography is estimated at 22% and 30%, respectively, as in Spain [
43,
44]. There is a lack of agreement regarding the fundamental definition of this scientifically understudied problem in interventional cardiology. However, some clinical, financial, cultural, and legal drivers of overuse have been previously recognized [
45]. Financial interest does not need further clarification since more interventions mean more direct and indirect financial benefits. Regarding clinical issues, TCA is questioned in patients with stable IHD since they can have more benefits from medications or even CABG. Also, secondary prevention with optimal medical therapy has proved its worth compared with TCA [
46,
47]. Recommendations to reduce overuse require guidelines, a country-specific approach with comprehensive data extraction from hospital databases, and a willingness to conduct economic and cost-effectiveness analyses of invasive cardiology treatments to avoid insufficient cardiovascular care. Also, exposure to unnecessary risk could result in unwanted clinical outcomes and the additional financial burden that continuously strains healthcare budgets.
The TCA:CABG ratio represents an effort to quantify the utilization of cardiological interventions. This indicator was previously used as a parameter of potential overutilization of TCA and as a predictor of in-hospital mortality of patients with acute coronary syndrome [
48]. All countries continuously and significantly increased the TCA:CABG ratio in the 2011–2019 period: Croatia at +8.9%, followed by France at +5.1%, Italy at +3.5%, Slovenia at +3.1%, and Spain at +2.2% (
Figure 9). The high-to-low ratio for France vs. Slovenia was 1.74. Still, a detailed TCA:CABG ratio analysis requires evaluating the numerator and denominator. For example, the highest ratio for France can be explained by the augmentation of the TCA rate and reduction in CABG procedures. On the other hand, Croatia simultaneously increased both rates, TCA and CABG, and had lower ratio values. Although the TCA:CABG ratio alone cannot provide accurate conclusions about the overuse of TCA or CABG, it can be indicative and used to quantify the intercountry differences.
IHD causes the most deaths in all analyzed countries [
49,
50,
51,
52,
53]. This study showed significant health gaps among Mediterranean old and new EU country members, especially in standardized mortality and medical intervention rates. These differences are most likely associated with differences in prevention, constantly facing obstacles such as the lack of political will, competing financial and commercial interests, and missing the focus on social determinants [
54]. Unlike prevention, medical interventions can be easily pharmacy-driven, especially in countries without cost-effective preventive strategies and mandatory monitoring of health outcomes, such as Croatia. Cardioprotective Mediterranean diets are rapidly disappearing, especially in transitional countries. Mediterranean heritage has beneficial physical, social, and environmental determinants incorporated not only in a diet but also in a lifestyle. Dietary issues are ranked at fifth place among risk factors that, when combined, are the causes of most deaths and disability in France, Spain, and Italy, while in Croatia and Slovenia, they are ranked at third and fourth place. Mediterranean cuisine represents a fusion of Roman and Greek culture with numerous dishes based on three core ingredients, regardless of region: olives, wheat, and grapes. Socializing around the dining table with Mediterranean dishes followed by a siesta might be as equally relevant in mortality reduction as interventions on surgical tables [
55]. Still, to reduce IHD mortality, preventive cardiovascular healthcare strategies should be adjusted to retain Mediterranean heritage at the country level.
Limitations
This study has several limitations. First, the study is based on secondary data. Cross-country comparison of country-specific aggregated data does not allow conclusions about causality. Second, data have different levels of accuracy. Incidence and prevalence data are obtained from survey-based data and cannot be considered as accurate as mandatory collected mortality data drawn from vital statistics. Usually, they are more vulnerable to bias because only a sample is taken instead of a collection of mortality data across the whole population. Third, although they are less inconsistent, retrospective data collection and death certification are marked with a certain robustness, which should be considered during the interpretation of data. Also, methodologies for deciding on causes of death might differ among countries regardless of the existence of the WHO ICD coding system and efforts to standardize coding. The problem of adequate reporting and filling in the reports on death certificates can never be excluded. This could lead to over or under-reporting of death since in the elderly population, mostly affected with IHD, there may be more than a few possible causes of death. Fourth, the comparisons between countries during certain periods are complex because there are differences in definitions of metrics used, quality of data, and methods of acquisition. Still, changes within a country should be more consistent as each country will likely preserve a generally consistent methodology over time. Fifth, the period before the COVID-19 pandemic was purposefully chosen because the pandemic affected health systems and medical procedures and their outcomes in different ways across countries.
Despite the abovementioned limitations and potential methodological difficulties, this study provides new insights into cardiovascular epidemiology among Mediterranean countries. Standardized rates allow comparisons both over time and between countries. Although aggregated data are challenging to interpret regarding causality, their quantification provides indicative leads for future country-specific research with more complex study designs.