Abstract
(1) Background: The aim of this study was to identify the practice management software (PMS) attributes required by physiotherapists to improve software design and development in order to increase the adoption and implementation of software and minimize the impact on the workflow of the clinic. (2) Methods: In total, 27 graduated physiotherapists with clinical and management expertise and experience in management software for physiotherapy services participated in six focus groups. Research staff members recorded, transcribed, and analyzed the focus groups, using a thematic analysis to code and classify the comments. (3) Results: A total of 43 categories of coded statements divided into 12 subthemes and five broad themes were identified and compiled in two core areas of content: clinical care and administrative tasks. In order to improve the adoption and implementation of physiotherapy PMS, this research provides experiential knowledge on the inefficiencies perceived by physiotherapists regarding current software programs and the specific attributes to assist practice management and facilitate workflows. The focus group analyses led us to map the multifaceted framework for physiotherapy PMS. (4) Conclusion: These findings provide valuable information as to what aspects are meaningful for the future design and development of physiotherapy PMS, thus providing guidance to both software developers and to end-users when benchmarking software solutions.
1. Introduction
The field of software in healthcare and physiotherapy clinics has been growing quickly in the last ten years [1,2]. The global physiotherapy software market size was valued at USD 1.09 billion in 2021 and is estimated to grow at a compound annual growth rate of 10.1% during 2023–2030 to USD 2.52 billion in 2030. North America dominated the p market with a share of over 52% in 2021 [3]. The two most adopted tools by physiotherapists in their clinics are electronic health records (EHRs) and practice management software (PMS) [1,2]. On the one hand, software for EHRs enables clinicians to document, store, and retrieve electronic patients’ healthcare information [4]. On the other hand, PMS was initially more focused on business and administrative operations in the practice clinic, although they have more recently included EHRs among their functionalities. Furthermore, there has been an explosion in other software packages (e.g., eHealth applications, financial systems, and applications to communicate or interoperate with other systems) that often interact/integrate with PMS [2].
According to the literature, the adoption and implementation of these digital technologies in physiotherapy clinics is associated with benefits such as efficiency in the workflow of the clinic, improved communication among members of the team, improved quality and security of care, easy data retrieval, etc. [5,6]. Despite the potential benefits, the adoption of these technologies in physiotherapy clinics is low and slow over time [5,6,7,8,9]. Thus, for example, in Belgium, out of 18,355 active physiotherapists in the first lustrum of the 21st century, only 30–50% of physiotherapists stored their data electronically, according to the National College of Physiotherapists, and similar data can be found in other European countries [7]. In 2015, only 19% of physiotherapy clinics in British Columbia (Canada) were using an electronic medical record, while 81% were still working on paper [1]. In 2016, only 28% of the physiotherapists from the United States of America (USA) were using an electronic system, 33% were using a system combining paper and electronic, and 38% were not using any electronic system at all [10]. Meanwhile, in Australia and New Zealand, around 60% (68.6 and 56%) of physiotherapists in two recent surveys used an electronic format for recording clinical records [11,12]. Low adoption rates are also one of the most common problems reported with electronic systems designed for healthcare [13,14,15,16,17]. An early systematic review in 2006 [5] identified barriers to the implementation of EHRs in physiotherapy (e.g., the inadequacy of software, the challenge of staff training, and modifying the functioning of the practice). Also, the lack of information system developers’ knowledge on physiotherapy processes and workflow, not addressing tangible and practical needs, and the lack of cooperation between physiotherapists and ICT developers were indicated as barriers to ICT adoption by physiotherapists [18]. Multiple recommendations, focused on software design and implementation, have been proposed for overcoming these barriers. Regarding implementation, previous and adequate planning before implementation was suggested, including staff training and considerations of potential changes required in the clinic [1,5,10,19]. Aware of these recommendations and barriers, professional physiotherapy associations have been guiding their members in regard to the process of planning and adopting PMS and/or EHRs [1,2,10].
The main recommendations intended for software design focused on including both clinicians and a workflow analysis in the software development activities to incorporate the physiotherapists’ perspectives in order to help identify and understand their requirements and processes [5]. The application of these recommendations is expected to identify the specific software attributes required by physiotherapists for practical use and minimize the impact on the workflow of the clinic. The adaptation to the needs of physiotherapists would improve the design and functionality of the software to meet the expectations of physical therapists to avoid dissatisfaction with its use [5]. However, despite these expectations, evidence about software requirements identified from the participation of physiotherapists in activities of design is limited and focused on very specific issues [19,20]. Some studies focused on physiotherapists’ perspectives on ICT (use, acceptability, requirements, and barriers to adoption) [9,21] and factors influencing practical use during the therapeutic process and the skills needed to use ICT [19]. In the meantime, some surveys have evidenced that there are PMS attributes required by physiotherapists that are still absent in their current PMS [2], and physiotherapists report low job satisfaction with some functionalities of their PMS [5]. However these are based on the experience in other health professions, interviews, and opinions [1,2]. To the best of our knowledge, no focus groups have been conducted to address the specific needs of physiotherapists for the practical use of a PMS for their day-to-day professional practice from a global perspective.
The aim of this study was to examine the perceptions of physiotherapists in relation to the practical use of PMS in their clinics in order to identify their needs and requirements. The identification of the physiotherapists’ needs and requirements would allow us to address the software inadequacy and inefficiencies, enhancing physiotherapists’ satisfaction and facilitating the adoption and implementation. The research questions for this study were as follows: (1) What PMS inefficiencies do you find for your clinical and administrative work? (2) What PMS attributes would you require to facilitate your work and improve workflow on clinical and administrative tasks? This work could provide manufacturers with new and valued attributes for software design and development, and also guide physiotherapists on relevant attributes when benchmarking PMS solutions.
2. Materials and Methods
2.1. Qualitative Approach
The study was undertaken using a grounded theory approach, involving an inductive-reasoning process [22]. Given the dearth of research on the specific software attributes required by physiotherapists, this study used a constructionist approach to build an understanding and knowledge of the theoretical framework of the physiotherapists’ perceptions of the practical use of PMS, using focus groups with physiotherapists with clinical and management expertise and experience in management software for physiotherapy services [23]. The selected approach was considered the most appropriate for the research question [22,24,25].
The focus groups were carried out by a moderator (EAM, one co-author), with the help of one assistant. The moderator graduated as a physiotherapist in the year 2000 and had some experience with PMS. Only six of the focus group participants were previously known by the moderator, who had no actual professional or commercial relationship with any of them.
2.2. Context
We conducted the study among graduated physiotherapists in Spain during the year 2020. Due to the origin of the researchers, the study was mainly carried out in the Valencian Community of Spain, with the assistance of the ICOFCV (Illustrious Official College of Physical Therapists of The Valencian Community). The Valencian Community is representative of the physiotherapy situation in Spain, where there are no major differences from the rest of the country regarding the healthcare system and physiotherapy practice. Five of the six focus groups were carried out after the general lockdown in Spain, due to COVID-19. The pandemic conditioned the implementation of the focus groups due to confinement, meeting, and geographical mobility restrictions.
A purposive sampling strategy was used to identify physiotherapists with clinical and management expertise, with any experience (either regular or occasional) in management software for physiotherapy services. Consultations with the ICOFCV (Illustrious Official Society of Physiotherapists of the Valencian Community) were held to identify professionals working in different fields of practice (musculoskeletal, pediatrics, neurology, sports, and higher education) and different sectors (public and private).
Although the final sample size was dependent on the saturation of information, 42 candidates were initially selected and contacted over the phone by the investigators to explain the project and find out their availability. The study information document (explaining the details of the research project) and consent were sent to read fully. Candidates were invited to a suitable focus group. When a candidate cancelled or did not attend his/her meeting, efforts were made to reschedule in other groups.
Previous consultations were made with the Ethics Committee at the Universitat de València to verify the need for research approval. No health or particularly sensitive data were collected. However, participants were fully informed about the content of the study and the benefits associated with the research. Participants were asked to give informed consent to participate. The data collected were completely anonymous so that neither the participants nor their responses could be identified. No compensation was received for participation.
2.3. Data Collection Methods
The qualitative design of this study involved focus groups because group interaction provides a wider range of responses that might not arise from individual interviews [26,27]. Focus groups have been used in previous studies to learn about the physicians’ perceptions of electronic medical records [28,29].
Firstly, a topic guide and a script were developed based on a literature review, including a review of the functionalities of the most significant management software for several physiotherapy associations [1,2]. Secondly, a preliminary focus group was conducted to evaluate the appropriateness of the focus group script. A software engineer (with experience in designing and developing healthcare management software) and a family doctor (with experience founding and training a healthcare management software) participated and contributed to the group; changes to the script and guide were made accordingly. Posteriorly, six focus groups were conducted with the help of the revised script with predetermined (see Table 1) and backup questions in the field of clinical care and administrative tasks. Adjustments to the focus group protocol and questions were made according to early experience and the information provided by participants. Each focus group included three-to-six participants and lasted 90–120 min. Videotape, audio, and field notes were used for data collection.

Table 1.
Thematic guide for focus group discussion.
Out of the initial sample of 42 eligible participants, 27 participated in this study. The progress of the selection stages and the reasons for non-participation are presented in Figure 1. Table 2 summarizes the demographic characteristics of the participants in the focus groups. They had an average of 18.7 years of clinical experience; a big majority of participants were owners/managers (18) of physiotherapy centers. Recruitment stopped when saturation was reached, which was when no new categories or coded statements were identified. The analyses showed the adequacy and generalizability of the content, and sufficient depth of understanding was achieved in the emergent theoretical categories [30].
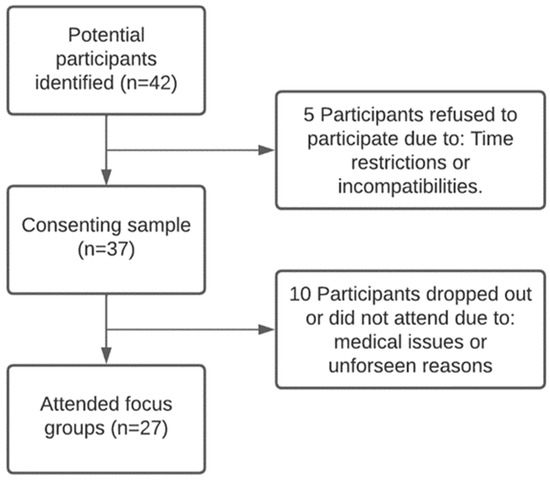
Figure 1.
Flow of participant recruitment.

Table 2.
Focus group participants’ demographic characteristics.
2.4. Data Processing and Analysis
The sessions were fully transcribed by the researchers. Transcriptions were anonymized, and each participant was assigned a number code. Field notes were also reviewed to improve accuracy. A thematic analysis approach was used to code and classify the comments in the different themes, subthemes, and categories and then compiled into two core areas of content: attributes to improve workflow in clinical care and administrative tasks. An iterative process of reading, analyzing, and coding the data was carried out individually by two of the researchers, using word-processing software to code the categories. These were grouped into similar concepts to form subthemes and themes. The researchers reviewed and compared their findings to reach a consensus throughout the process. The categorization and classification of each coded statement were systematically reviewed, discussed, and consensually validated by the research team. Three rounds of coding and discussion took place to enhance the credibility of the analysis and develop clear categories and themes [31].
To check consistency, a third researcher cross-checked the results via a blind review for the same transcripts [31]. Any disagreements between the researchers were resolved by discussion. Confirmability was enhanced when the same categories emerged from the data of subsequent groups’ transcripts.
3. Results
3.1. Attributes Required for Clinical Care
In this area, the thematic analysis identified six subthemes that defined two broad themes, with three subthemes each. All of them, their categories, the frequency of coded statements, and the word association are summarized in Table 3.

Table 3.
Summary of physiotherapy PMS attributes required for clinical care, frequency of coded statements, and word association.
3.1.1. Theme 1—Data Entry and Issuance of Reports on Patient Clinical Care
Both data entry and the issuance of reports were perceived as highly time-consuming with their current software. In order to streamline these activities, participants regarded it as relevant to integrate additional solutions in the PMS (e.g., templates, digitalized tools, or automatized registration).
- Templates, digitalized tools, and classification codes for data entry
To help reduce the clinical data-collection time for common health problems, participants proposed the integration of structured and editable templates. Moreover, the integration of digitalized tools for assessment, such as body charts to digitally draw and fill in, patient-reported measures to be filled out digitally by patients, and classification systems to code health problems, were seen as useful solutions. Although participants focused on these structured tools, they also expressed their need to customize such tools and have open sections to provide them with additional information to support patient care.
“What I want in the end is to have my templates in the program, and if I’m going to treat a patient with a cervical problem, I can take that template and edit it.”
“In the clinical history, I like to have a body chart, where the patient or the physiotherapist can paint or draw on the chart.”
“And then as it was said, to have outcome measures or questionnaires like the Oswestry or many others specific for each patient that you are attending.”
- Digitalized tools and templates for the issuance of individualized patient reports
Participants felt that the issuance of individualized patient clinical-care reports is a frequent requirement from providers (e.g., insurance companies, lawsuits, colleagues and other healthcare professionals, and patients), but they considered it an additional burden to patient care and a load to be reduced. Specific templates for these reports were the main suggested software solution.
“But it’s not the same if the report is for a lawsuit, a doctor, or a colleague. So, having different basic models of reports about the state of the patient with fields to complete.”
In contrast, participants regarded the issuance of patient educational activities as essential for care. Despite this, they felt that educational reports are underutilized because the current software did not include educational digitalized resources (e.g., images of pathologies and guidelines). Participants reported that an exercise software displaying digitalized videos/images/models and other educational digitalized resources should be integrated into the software.
“Hence, I would like to prepare a document that I can print or send to the patient by email with the therapeutic exercises that I previously explained, the recommendations, so he can take it in writing.”
- Digitalized measures to monitor quality of care
Participants felt that providing information on the quality of the clinical care provided in the practice is a growing need, but their current software did not provide enough tools for its collection and analysis. Two combined software solutions were reported. The first involved integrated digitalized questionnaires (e.g., satisfaction questionnaires) and quality measures of processes and outcomes. The second involved the integration of automatized registration for predefined quality indicators.
“The program can’t rate that if there isn’t a satisfaction survey, and it would be interesting to have it on the software.”
“We do have the option of making statistics (about quality and activity), but it falls short.”
3.1.2. Theme 2—Clinical-Care Electronic Communication with Patients and Other Health Professionals
Participants considered that electronic communication via current software helps them to schedule appointments, send SMSs, and other perform functionalities. Nevertheless, they regarded that their software needed to integrate additional elements (e.g., reminders, video calls, etc.) in order to avoid some interruptions in the practice workflow and dysfunctions in their digital health interventions (DHIs).
- Automatized reminders for patients and professionals within the scheduling agenda
Participants stated that many patients often forgot their appointments, thus creating unjustified interruptions in the practice workflow. Their current scheduling agenda often did not prevent these occurrences. Hence, they expected that the integration of reminders for patients 24–48 h before their appointment would help them avoid these interruptions. Other interruptions were also associated with the agenda (e.g., simultaneous use of the same therapeutic space or equipment by two physiotherapists). Participants also required reminders for professionals that are aimed at reducing these overlaps (e.g., the agenda screen with the spaces and equipment free).
“For us, it is a problem how to fit in the program the availability of physiotherapists and the treatment rooms by time slots.”
“To remind the appointments is also important, because there are patients who systematically miss appointments.”
- Digital health interventions (DHIs)
Participants argued the need to incorporate telehealth care into the practice and expected the integration of DHI at the moment to be easy, because the patients’ willingness to use communication technologies had increased during the COVID-19 pandemic. They reported that many current software programs need to integrate video call, chat, and email to communicate with patients.
“We have been attending patients on the phone and from the hospital we were offered the possibility of installing equipment to make video calls with patients, because many of them were housebound and they were asking for help regarding exercises.”
“Then as well, going further, the future of telerehabilitation, the chat is essential.”
“But what happens with these emails? So it would be great if within this program, each specialty had a corporate email so that communications were registered and stored.”
- Patient portal
Participants considered interesting the possibility of having a portal to be accessed by clients to book appointments online, check pending and made appointments, and simplify the patients’ access to all educational plans (e.g., exercise programs). It was argued that the portal could save time scheduling or making phone calls.
“And the agenda so that the patient can schedule an appointment himself. He could access the program, see a slot, and book it. Because it’s very difficult for me, when I am on my own, I waste a considerable time trying to set an appointment.”
“Normally you send them materials, but if you had the platform to upload what you want them to do, it would be easier.”
3.2. Attributes Required for Administrative Tasks
In this thematic area, six subthemes were identified that defined three broad themes. All of them, their categories, the frequency of coded statements, and the word association are summarized in Table 4.

Table 4.
Summary of physiotherapy PMS attributes required for administrative tasks, frequency of coded statements, and word association.
3.2.1. Theme 1—Management of Administrative Documents and Marketing Communications
Participants often considered that issuance of both administrative documents and marketing communications took too much time with their current software. To streamline these activities and devote more time to clinical care, participants regarded it as relevant to integrate additional solutions in the software (e.g., templates, digitalized tools, or automatized registration).
- Automatized issuance of routine documents
Participants highlighted that filling in, signing, and issuing administrative documents (e.g., attendance certificates, invoices, informed consent, and data protection) is a daily routine, which is growing due to legal requirements. They felt that the load of these tasks notably increases when the patient’s signature must be included and when providers periodically request documents to monitor care. Two software solutions were reported. The first is the integration in the software of structured and editable specific templates, which could automatically be filled using stored data. Thus, the load would be reduced to review, edit (if necessary), and sign it. The second is having an easy digitalization of the signature of patients and professionals (e.g., by means of a tablet or similar).
“We print them out, sign them, and then scan them and save them in the history. They cannot be signed on the computer, there is no digital signature.”
“Like online banking. When we have to make a report, prepare an attendance certificate or an invoice, we could do it automatically.”
- Communication tools for marketing strategies
Participants felt that the use of marketing strategies is a growing need to strengthen customer relationships; hence, their current software needed integrated additional elements for both, improving the efficiency of their current marketing strategies and incorporating news. Participants considered that PMS should have an automatized system to assist them in the selection of usual marketing messages and clients to be contacted and provide links with external communication applications or channels (e.g., email, WhatsApp, and SMS) to select according to marketing needs.
“Newsletters, invitations to workshops, informative talks, I think it is also important that you can filter, for example, who you want to send them to, filtering by age, sex, condition, etc.”
“Software communication with patients should be easy to use, versatile and capable of sending emails, WhatsApp messages or SMS.”
3.2.2. Theme 2—Billing and Accounting of Payments and Supplies
According to participants, the software should facilitate the control of the economic aspects of the center. Private-sector physiotherapists expressed that their current PMS had strong limitations in regard to easy administration, billing and accounting payments, and indicating stock supplies that are available for treatments. New software solutions were proposed for these areas.
- Flexible billing and automatized accounting of payments
To help billing, participants believed that the PMS should provide them the opportunity to easily update fees according to time, demands, or special circumstances and should admit different payment methods. To help accounting, PMS should automatize the registration of payments with the accounting.
“If you work alone, it’s simple, but if you are co-working where there are different sessions and rates, it should allow you to easily modify, quantify and link it to the invoicing.”
- Automatized accounting of supplies to control stock
Physiotherapists reported the need of a section to keep track of consumption (stock available, regular consumption, expenses, sales, alerts, etc.) and notifications to replenish consumables in order to control stock supplies at the clinic.
“The management software should include the control of supplies, I don’t know if exhaustive or at least if you could enter the shopping basket.”
3.2.3. Theme 3—Access to Practice Management Software (PMS)
Participants felt that the need to access their PMS online is increasing in contrast to the traditional on-site access. Nevertheless, they found difficulties in interoperating and exchanging information online with their current software. Moreover, in both modalities, online and on-site, data security and maintenance were a major concern among participants. Emphasis was placed on the need for the PMS to help comply with current regulations.
- Interoperability
Participants requested that software solutions be accessible from different devices and operating systems to facilitate usability. The ability to import and export data with ease in a compatible format was regarded as important to facilitate some clinic management tasks.
“The software should allow the use from a computer, a tablet or a mobile phone, so in the case of attending a home visit, not having to take my computer with me.”
- Data security tools to face failures, inadequate use, and threats
Omissions and system failures were a common cause of data loss and work duplication. Automatic saving and backup copies should be allowed in the software. Furthermore, allowing different hosting options for data maintenance could reduce data loss and recovery.
“Because apart from the fact that sometimes you forget to save, other times it crashes and everything I had posted has been deleted, the program has not saved it automatically.”
Participants agreed on the convenience to regulate and control data access by configuring permissions for software users. Offering security measures for computer threats like viruses or hackers was seen as important functionalities.
“Reviewing data on a patient who is not under your specific care is a serious breach, and that has to be picked up by the documentation system.”
Overall, clinical care took most of the discussion time in all focus groups, with more than 60% of the discussion time and coded statements on average.
4. Discussion
This research provides experiential knowledge on the PMS attributes required by physiotherapists in order to facilitate workflows on both clinical and administrative activities and to overcome the inefficiencies perceived on current software programs. A total of five themes were identified (data entry and issuance of reports on patient clinical care, clinical-care electronic communication with patients and other health professionals, management of administrative documents and marketing communications, billing and accounting of payments and supplies, and access to PMS). In total, 43 specific attributes (categories) emerged and were classified into 12 subthemes.
In general, many issues identified during the focus groups were reflected in the different professional physiotherapy associations’ guides published to counsel their members on assessing and choosing software solutions [1,2]. Some disparities arise due to differences in the national standard requirements to register, the professional duties and responsibilities, or the national regulations (e.g., general data protection regulation). However, these guides were based on a literature review, the experience in other health professions, and informal discussions with members and consultations with leading physiotherapists and health information technology experts [1,2].
To the best of our knowledge, this is the first study to globally explore the perceptions of physiotherapists in relation to the practical use of PMS in their clinics using focus groups. Messer and Egger [19] conducted a qualitative study performing interviews with physiotherapists and experts to learn the specific requirements of physiotherapists on the practical use of software in the therapeutic process, and many themes coincide with our research. However, the themes in that study were quite general, involved only the clinical care, and the sample size for the interview (n = 13) was small. Merolli et al. (2021), in their qualitative study, focused on developing survey instruments to collect the physiotherapists’ and patients’ perceptions on the uptake and acceptance of digital health interventions in physiotherapy [21]. Postolache et al. (2017) evaluated the perspectives of physiotherapists and patients on needs, requirements, and barriers for EHR adoption for physiotherapy [9]. All in all, little research has been performed on the specific attributes required by physiotherapists on the practical use of practice management software, which covers not only clinical aspects but all the non-clinical aspects relevant to run a physiotherapy center.
Our study used the grounded theory approach to build an understanding and knowledge of the theoretical framework of physiotherapy PMS. Six focus groups with experienced physiotherapists were carried out, and a thematic analysis was undertaken to code and classify the comments. Measures were adopted to maintain consistency and enhance credibility. As a consequence of all of these methods, our study identified a wide conceptual framework to describe the areas, themes, and subthemes relevant to physiotherapy management software. In our opinion, this framework makes it easy to break and understand a multidimensional and complicated subject. Moreover, our approach appears to be more comprehensive than previous approaches to learn the needs of the physiotherapy collective regarding PMS.
During the development of the focus groups, clinical-care issues took most of the discussion time and coded statements, giving us a good idea of the inadequacy and inefficiencies of the current PMS for physiotherapy. The rest of the time and issues dealt with administrative tasks, security and confidentiality, communication, economic issues, legal and regulatory requirements, or technical aspects, which concerned physiotherapists’ work. These were finally gathered into one broad area called “Administrative tasks” to avoid separating or overlapping issues. The diversity in the demographic characteristics of the participants provided insight into different physiotherapy specialties, which require flexibility and customization in a PMS, for example, in anamnesis and clinical history documents, questionnaires, and scales. Also, the participants working in the private sector had greater concerns about the economic management, business and performance statistics, or marketing strategies than participants working in the public sector, which is public and free of charge. Despite our novel contribution using focus groups, the study was carried out in the Spanish region of the Valencian Community, and most of the participants were living or working in this region, so caution must be applied when trying to extrapolate the results.
Our findings have important applications. This study allows us to identify the PMS attributes required by physiotherapists that may influence in the efficiency and functionality of the software. Given the low levels of adoption and satisfaction with physiotherapy PMS [5,6,7,8,9] these findings might be of great relevance for the design of future software solutions to enhance the adoption and satisfaction with these programs. Furthermore, in the last few years, the COVID-19 pandemic has given a new impulse and greater awareness to digital health technologies in physiotherapy, increasing the use for care delivery [32,33]. However, little research has been published to date after the pandemic; this study provides a valuable insight into the physiotherapists’ experiences and needs post-COVID-19.
The main strength of our study is based on the methodological aspects of the qualitative study, which was based on a literature review of previous studies and qualitative research using focus groups with experienced physiotherapists. This qualitative study allowed us to identify and summarize the issues relevant to physiotherapists regarding PMS requirements and processes in order to solve the inadequacy and inefficiencies present in current PMS for physiotherapy and, ultimately, to improve the adoption and implementation of PMS in physiotherapy. However, a subsequent quantitative study would be necessary in order to validate physiotherapists’ expectations for the identified attributes.
5. Conclusions
In order to improve the adoption and satisfaction with physiotherapy PMS, it is necessary to identify the software attributes that can satisfy the needs and processes of physiotherapists on the practical use. Our study provides an insight into the relevant attributes in a multidimensional construct divided into two areas of content: clinical care and administrative activities. The focus group analyses led us to identify five themes (data entry and issuance of reports on patient clinical care, clinical-care electronic communication with patients and other health professionals, management of administrative documents and marketing communications, billing and accounting of payments and supplies, access to PMS), and twelve subthemes which map the framework for physiotherapy PMS well. The attributes of clinical tasks raised the most debate and concern among physiotherapists. The findings of this study provide valuable information as to what aspects are meaningful for the future design and development of physiotherapy PMS, thus providing guidance to software developers and to end-users when benchmarking PMS.
Author Contributions
Conceptualization, F.M.-M. and E.A.-M.; methodology, E.A.-M. and R.M.-S.A.; software, E.A.-M.; validation: A.E.-E., N.M.-S. and R.M.-S.A.; formal analysis, E.A.-M. and R.M.-S.A.; investigation, E.A.-M.; resources, N.M.-S.; data curation, A.E.-E.; writing—original draft preparation, R.M.-S.A. and E.A.-M.; writing—review and editing, F.M.-M.; visualization, A.E.-E.; supervision, F.M.-M.; project administration, F.M.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the subject of the research is a professional situation regarding practice management software and no clinical or sensitive data was collected, the authorization by the Ethics Committee was not required.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is contained within the article.
Acknowledgments
The authors want to thank the volunteers for their participation during this study, as well as Jesús Ramírez-Castillo and the ICOFCV for their support and collaboration during the study development.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Canadian Physiotherapy Association, Physiotherapy Association of British Columbia. PABC EMR Toolkit: Implementing Electronic Medical Records in Private Practice Physiotherapy Settings; Canadian Physiotherapy Association, Physiotherapy Association of British Columbia: Vancouver, BC, Canada, 2016. [Google Scholar]
- Australian Physiotherapy Association (APA). Practice Management Software Insight 2018; Australian Physiotherapy Association: Hawthorn, Australia, 2018. [Google Scholar]
- Physical Therapy Software Market Analysis Report, 2022–2030. Available online: https://www.grandviewresearch.com/industry-analysis/physical-therapy-software-market-report (accessed on 6 October 2023).
- Key Capabilities of an Electronic Health Record System; National Academies Press: Washington, DC, USA, 2003.
- Vreeman, D.J.; Taggard, S.L.; Rhine, M.D.; Worrell, T.W. Evidence for Electronic Health Record Systems in Physical Therapy. Phys. Ther. 2006, 86, 434–446. [Google Scholar] [CrossRef] [PubMed]
- Michel-Verkerke, M.B. The Love-Hate Relationship of Physical Therapists with Electronic Patient Records. Procedia Comput. Sci. 2015, 64, 432–441. [Google Scholar] [CrossRef][Green Version]
- Buyl, R.; Nyssen, M. From a Paper-Based to an Electronic Registry in Physiotherapy. Collab. Patient Centred Ehealth 2008, 141, 75–81. [Google Scholar] [CrossRef]
- Yung, A. Adoption of Electronic Health Record System in Community-Based Physiotherapy Clinics: A Pilot Case Study. Build. Capacit. Health Inform. Future 2017, 2017, 395–400. [Google Scholar] [CrossRef]
- Postolache, G.; Oliveira, R.; Postolache, O. Designing Digital Tools for Physiotherapy. In Interactivity, Game Creation, Design, Learning, and Innovation; Brooks, A.L., Brooks, E., Eds.; Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering; Springer International Publishing: Cham, Switzerland, 2017; Volume 196, pp. 74–88. ISBN 978-3-319-55833-2. [Google Scholar]
- American Physical Therapy Association (APTA). Understanding and Adopting Electronic Health Records (EHR); American Physical Therapy Association: Alexandria, VI, USA, 2016. [Google Scholar]
- Merolli, M.; Gray, K.; Choo, D.; Lawford, B.J.; Hinman, R.S. Use, and Acceptability, of Digital Health Technologies in Musculoskeletal Physical Therapy: A Survey of Physical Therapists and Patients. Musculoskelet. Care 2022, 20, 641–659. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-W. The Perspectives of Physiotherapists in Canterbury on the Use of Electronic Health Records. Ph.D. Thesis, University of Canterbury, Canterbury, UK, 2018. [Google Scholar] [CrossRef]
- Hailey, D.; Yu, P.; Munyisia, E. Pre-Implementation Investigation of the Readiness of Allied Health Professionals to Adopt Electronic Health Records. In Investing in E-Health: People, Knowledge and Technology for a Healthy Future; IOS Press: Clifton, VA, USA, 2014; pp. 47–53. [Google Scholar]
- Kruse, C.S.; Kristof, C.; Jones, B.; Mitchell, E.; Martinez, A. Barriers to Electronic Health Record Adoption: A Systematic Literature Review. J. Med. Syst. 2016, 40, 252. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.; Watt, I.; Sheard, L.; Wright, J.; Adamson, J. Implementing Electronic Records in NHS Secondary Care Organizations in England: Policy and Progress since 1998. Br. Med. Bull. 2017, 121, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Al Ani, M.; Garas, G.; Hollingshead, J.; Cheetham, D.; Athanasiou, T.; Patel, V. Which Electronic Health Record System Should We Use? A Systematic Review. Med. Princ. Pract. 2022, 31, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.C.; Warren, R.W.; Ebeling, M.; Andrews, A.L.; Teufel II, R.J. Physician Use of Electronic Health Records: Survey Study Assessing Factors Associated With Provider Reported Satisfaction and Perceived Patient Impact. JMIR Med. Inf. 2019, 7, e10949. [Google Scholar] [CrossRef] [PubMed]
- Postolache, G.; Moreira, I.; Pedro, L.; Oliveira, R. Implementation of Electronic Health Record Systems in Physical Therapy. In Proceedings of the 1st Asia-Oceanian Congress for NeuroRehabilitation, Seoul, Republic of Korea, 3–5 September 2015. [Google Scholar]
- Messer-Misak, K.; Egger, R. Specific Requirements of Physiotherapists on the Practical Use of Software in the Therapeutical Process. Health Inform. Meets Ehealth 2016, 2016, 158–166. [Google Scholar] [CrossRef]
- Postolache, G.B.; Oliveira, R.; Postolache, O. Contextual Design of ICT for Physiotherapy: Toward Knowledge and Innovation Ecosystem. EAI Endorsed Trans. Creat. Technol. 2017, 4, 153334. [Google Scholar] [CrossRef][Green Version]
- Merolli, M.; Hinman, R.S.; Lawford, B.J.; Choo, D.; Gray, K. Digital Health Interventions in Physiotherapy: Development of Client and Health Care Provider Survey Instruments. JMIR Res Protoc 2021, 10, e25177. [Google Scholar] [CrossRef] [PubMed]
- Corbin, J.; Strauss, A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory; SAGE Publications: London, UK, 2014. [Google Scholar]
- Levers, M.-J.D. Philosophical Paradigms, Grounded Theory, and Perspectives on Emergence. SAGE Open 2013, 3, 2158244013517243. [Google Scholar] [CrossRef]
- Bogdan, R.; Biklen, S.K. Qualitative Research for Education: An Introduction to Theory and Methods, 2nd ed.; Allyn and Bacon: Boston, MA, USA, 1992. [Google Scholar]
- Miles, M.B.; Huberman, A.M. Qualitative Data Analysis: An Expanded Sourcebook; SAGE Publications: London, UK, 1994. [Google Scholar]
- Rodas Pacheco, F.D.; Pacheco Salazar, V.G. Grupos Focales: Marco de Referencia Para Su Implementación. INNOVA Res. J. 2020, 5, 182–195. [Google Scholar] [CrossRef]
- Hennink, M.M.; Hennink, M.M. Understanding Focus Group Discussions; Understanding Qualitative Research; Oxford University Press: Oxford, NY, USA, 2014; ISBN 978-0-19-985616-9. [Google Scholar]
- Witry, M.J.; Doucette, W.R.; Daly, J.M.; Levy, B.T.; Chrischilles, E.A. Family Physician Perceptions of Personal Health Records. Perspect. Health Inf. Manag. 2010, 7, 1. [Google Scholar]
- Al Alawi, S.; Al Dhaheri, A.; Al Baloushi, D.; Al Dhaheri, M.; Prinsloo, E.A.M. Physician User Satisfaction with an Electronic Medical Records System in Primary Healthcare Centres in Al Ain: A Qualitative Study. BMJ Open 2014, 4, e005569. [Google Scholar] [CrossRef] [PubMed]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in Qualitative Research: Exploring Its Conceptualization and Operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Lillo-Navarro, C.; Medina-Mirapeix, F.; Escolar-Reina, P.; Montilla-Herrador, J.; Gomez-Arnaldos, F.; Oliveira-Sousa, S.L. Parents of Children with Physical Disabilities Perceive That Characteristics of Home Exercise Programs and Physiotherapists’ Teaching Styles Influence Adherence: A Qualitative Study. J. Physiother. 2015, 61, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Rausch, A.-K.; Baur, H.; Reicherzer, L.; Wirz, M.; Keller, F.; Opsommer, E.; Schoeb, V.; Vercelli, S.; Barbero, M. Physiotherapists’ Use and Perceptions of Digital Remote Physiotherapy during COVID-19 Lockdown in Switzerland: An Online Cross-Sectional Survey. Arch Physiother 2021, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, A.; Awan, N.; Gallagher, P. Physiotherapists’ Perspective of Telehealth during the COVID-19 Pandemic. Int. J. Med. Inform. 2021, 156, 104613. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).