Abstract
In contemporary dental practice, clinicians have a variety of materials and options for restoring single teeth compromised by carious or non-carious diseases. According to studies and new concepts in biomimetic restorative dentistry, indirect ceramic restorations will play an increasingly important role in daily practice. We follow up and evaluate clinically three times over a 10-year period on eighty-six indirect restorations (n = 86) of lithium disilicate e.Max Press (Ivoclar, Schaan, Liechtenstein) in 32 patients. Restorations are evaluated in the 2nd, 5th, and 10th years after the fixation. Four of the restorations studied (n = 86) had to be replaced at year 5 follow-up because of fracture (failure rate: 4.65%; Kaplan–Maier). There are no restorations with bulky, cohesive fractures. Lithium disilicate ceramic restorations provide a good treatment alternative for a 5- to 10-year period of observation, and they can be successfully applied in dental practice in 91.73% to 98.84% of cases. Advancements in digital dentistry, including the use of intraoral scanners and CAD/CAM technology, are set to further refine the precision and efficiency of indirect restorations for distal teeth, enabling quicker turnaround times and improved fit. Additionally, ongoing developments in biomaterials promise to enhance the durability and biocompatibility of these restorations, potentially leading to better long-term success rates and patient satisfaction. The goal of this clinical study was to look at how well biomimetic ceramic overlays and onlays made of lithium disilicate held onto teeth with a IV-generation adhesive system for 10 years. The study also looked at how well the edges of the teeth adjusted and how strong the teeth were overall.
1. Introduction
At the beginning of the 21st century, the proportion of metal indirect restorations exceeded the percentage of esthetic ceramic or composite tooth color indirect restorations. Only after 20 years was the ratio changed at the expense of esthetic indirect restorations [1]. The requirements for modern restorations of distal teeth are that they have similar characteristics to those of natural tooth structures, such as color, brightness, surface texture, fracture resistance, and abrasion resistance. Restorative techniques with modern dental ceramics have also greatly improved, both due to the advanced composition of ceramic materials and advancements in adhesive systems. Choosing the right adhesive system is important for the durability and resistance of ceramic restorations. For years, clinicians were limited to the use of indirect restorations made of metal (gold or gold alloys) or, in some cases, metal–ceramic. However, dentistry has been using ceramic partial restorations for over 100 years. Problems in the early years of the introduction of ceramic restorations included unsatisfactory fracture resistance required for distal teeth, micro-leakage, unsatisfactory cement characteristics, and poor adaptation in the marginal zone. In the last two decades, some new materials have appeared that provide more esthetic possibilities and increase resistance [2]. In contemporary dental practice, clinicians have a wide range of materials and options to restore single teeth compromised by carious or non-carious diseases. Numerous laboratory studies and clinical studies have shown that the preservation of healthy tooth structure is an important factor in the longevity of restorations and teeth [3,4,5,6,7,8]. Based on studies and new concepts, indirect restorations will play an increasingly important role in restorative dentistry [9]. Both scientific and practical dentistry focus on minimally invasive and biomimetic restorations. Several laboratory studies and clinical trials have compared the effectiveness of onlays and overlays with full crowns in distal teeth [10,11,12,13]. However, a thorough evaluation of the comparison between the two types of restorations remains incomplete. Sometimes, it is difficult and confusing for the clinician to judge which type of restoration should be used to restore damaged posterior teeth. During the polymerization of the cement, high internal stresses can be generated, causing the adhesive bond to rupture (the adhesive interface between the cement and hard tooth tissues on the one hand and the cement and the internal ceramic surface on the other), leading to marginal leakage, especially when the borders are in dentin. In the case of inlay/onlay preparations, the presence of peripheral enamel is crucial to the success and longevity of the healing approach. We have assessed the clinical success of indirect restorations by measuring marginal adaptation and leakage and correlating these parameters with the loss of attachment integrity to the peripheral hard dental tissues [14]. Loss of this integrity is associated with the development of a secondary carious process, postoperative sensitivity, and staining of the tooth/restoration interface [15,16,17]. However, there is no combination of restorative material and cementation protocol capable of achieving complete (100%) marginal sealing [18].
Restoring distal teeth, such as molars, poses significant clinical challenges due to their limited accessibility and visibility, making it difficult for dental professionals to perform precise treatments. The complex anatomy of these teeth, with their multiple roots and cusps, complicates procedures such as cavity preparation and the placement of restorative materials. Additionally, the high occlusal forces exerted on distal teeth increase the risk of restoration failure, necessitating the use of durable materials and advanced techniques to ensure longevity and functionality.
The aim of the present clinical study was to evaluate the fracture resistance, marginal adaptation, and integrity of teeth adhesively restored with biomimetic ceramic overlays and onlays from lithium disilicate fixed with a IV-generation adhesive system for a 10-year period.
2. Materials and Methods
Eighty-six indirect restorations (n = 86) of lithium disilicate e.Max Press (Ivoclar AD, Schaan, Liechtenstein) placed in 32 patients, of which 18 were women and 14 men aged 20 to 65 years, were followed up and evaluated clinically three times over a 10-year period. The patient’s informed consent was provided before performing the treatment. The treated teeth were divided into two main groups: Group I (premolars) and Group II (molars). The restorations were fixed with composite cement Variolink II (Ivoclar AD, Schaan, Liechtenstein) using the IV-generation adhesive system Syntac Classic (Ivoclar AD, Schaan, Liechtenstein) under rubber dam isolation. We strictly followed the manufacturer’s recommended steps in the adhesive procedure. Restorations were evaluated in the 2nd, 5th, and 10th years after the fixation (Table 1).

Table 1.
Distribution of clinical cases by groups in the three follow-up periods.
All clinical procedures were performed by a single investigator (A.G.). The clinical assessment of the monitored parameters was carried out by two researchers (A.G. and N.N.), using Optagate (IvoclarVivadent, Schaan, Liechtenstein), air, a probe for caries diagnostics (Dental Explorer 23/17A Double Ended), and magnification (x4.0 Dental microscope, Carl Zeiss, Oberkochen, Germany) for marginal zone analysis and the presence of cracks and fractures (adhesive or cohesive). We also assessed and recorded factors such as fracture incidence, esthetic changes, carious process, staining in the cementum area, soft tissue tolerance, and patient discomfort. Esthetic parameters were evaluated clinically in terms of color match and surface roughness. Indirect ceramic restorations were graded as perfect, clinically acceptable, or clinically unacceptable in each grading category. We confirm that we have read the Helsinki Declaration and followed the guidelines for this investigation.
2.1. Cases Selection
The selection of clinical cases was made randomly, including patients admitted to the dental clinic for the treatment of severely decayed distal teeth (premolars and molars), missing more than 1/2 of the occlusal surface, frequent fractures of the direct restorations in the last 2–3 years, missing at least one axial edge from the clinical crown, insufficient proximal contacts, and finally, a lack of satisfactory esthetics. During the selection and follow-up process, we excluded patients with periodontal diseases, diabetes, opening limitations, allergy problems reported in the anamnesis, unsatisfied oral hygiene, and advanced stages of temporomandibular joint diseases. The patients included in the clinical study were admitted to the clinic for treatment in the period 2010–2011.
2.2. Clinical Preparation Protocol
After clinical and radiographic examination, recorded patient history, and signed informed consent, a silicone impression was taken for temporary obturation. Anesthesia was applied according to indications; isolation was performed with a rubber dam. Next, we prepared the cavity by removing the old obturation and the carious lesion. The cavity walls were shaped with a 40 μm diamond bur (for occlusal part—#845KR-F-025 and #845KR-F-18, and for the proximal part—#845KR-F-18 and #846KR-F-016). Immediate dentin sealing was performed after cavity preparation with the IV-generation OptiBond FL (Kerr, Boca Raton, FL, USA)-filled adhesive. Glycerin gel was placed to achieve complete polymerization of the adhesive layer. Finishing of the enamel margins was performed with a diamond bur (40 μm) to remove adhesive in the marginal areas. After the silicone impression with a two-phase one-step technique (Express™, 3M ESPE, Irvine, CA, USA), rigid temporary restorations were made of ProtempTM 4 (3M ESPE, Irvine, CA, USA) by a preliminary preoperative impression.
2.3. Ceramic Restorations Fabrication
Indirect ceramic restorations were fabricated from lithium disilicate glass-ceramic (LS2) e.Max Press (Ivoclar, Schaan, Liechtenstein) in the same dental laboratory with calibrated laboratory parameters.
2.4. Clinical Cementation Protocol
Eighty-six lithium disilicate ceramic restorations (n = 86) were cemented with dual cement, Variolink II (Ivoclar, Schaan, Liechtenstein). Removal of the temporary obturation was followed by surface treatment with alumina (Rondoflex, KaVo, Biberach, Germany). After etching the hard dental tissues, mainly enamel for 20” with 37% orthophosphoric acid, they were prepared for adhesive bonding with IV-generation adhesive, Syntac (Ivoclar, Schaan, Liechtenstein), which included three steps: Syntac primer, Syntac adhesive, and the light-curing Heliobond adhesive, for a sound chemical bond between composite material/cement and tooth structure. The Syntac adhesive system was used according to the manufacturer’s recommendations to prepare tooth structures and the inner surface of the ceramic restoration. Lithium disilicate was prepared for adhesive bonding by etching for 20” with hydrofluoric acid (Ivoclar, Schaan, Liechtenstein). The hydrofluoric acid was thoroughly washed, and the restorations were additionally placed in an ultrasonic bath to remove the resulting surface precipitates. After drying, Monobond S (Ivoclar, Schaan, Liechtenstein) was applied to the inner ceramic surface for 60”. After the silane, Heliobond (Ivoclar, Schaan, Liechtenstein) was applied, which was also applied to the hard dental tissues as the third step of the Syntac adhesive system. After the composite cement was selected by type, the base and catalyst were mixed and applied to the prepared inner surface of the ceramic restoration. The pre-fixed stick or holder for correct placement in the oral cavity provides the possibility of precise placement in the cavity prepared for adhesive bonding. The finishing and polishing procedures concluded with the application of fluoride-protective varnish.
2.5. Clinical Evaluation Periods
Eighty-six indirect ceramic restorations by e.Max Press (Ivoclar, Schaan, Liechtenstein) were analyzed. Two cases could not be evaluated in the second period and five in the third period; therefore, only the ceramic restorations (n = 86) that were clinically evaluated three times by two investigators (A.G. and N.N.) were subject to statistical processing and evaluation. The data are from the first, second, and third periods: in the 2nd year (2012–2013), in the 5th year (2015–2016), and in the 10th year (2021–2022).
2.6. Clinical Evaluation Criteria
Distal teeth restored with ceramic overlays/onlays were evaluated clinically three times in the 2nd, 5th, and 10th year after the fixation using the modified United States Public Health Service (USPHS) criteria [19]:
| 1. Color matching: | —Alfa: the color of the restoration matches that of the tooth; |
| —Bravo: the discrepancy is not beyond normal perception; | |
| —Charlie: the discrepancy is beyond normal perception; clinically | |
| unacceptable. | |
| 2. Marginal discoloration: | —Alfa: no discoloration is detected; |
| —Bravo: discoloration that does not penetrate in the pulpal direction; | |
| —Charlie: discoloration that penetrates in the pulpal direction; | |
| clinically unacceptable. | |
| 3. Postoperative hypersensitivity: | —Alfa: postoperative hypersensitivity is absent; |
| —Bravo: has postoperative hypersensitivity. | |
| 4. Anatomical shape: | —Alfa: the restoration conforms to the anatomical shape of the tooth; |
| —Bravo: the restoration does not conform to the existing anatomical shape, but the missing material is not sufficient to expose dentin; | |
| —Charlie: a significant volume of material is missing, and dentin is exposed. | |
| 5. Proximal contact: | —Alfa: excellent proximal contact; |
| —Bravo: proximal contact weak but present; | |
| —Charlie: no proximal contact. | |
| 6. Marginal integrity: | —Alfa: no visible gap or crack; |
| —Bravo: visible gap or crack; the probe enters a gap, but no dentin was detected; | |
| —Charlie: there is a fracture of the restoration: a part is missing or the entire obturation. | |
| 7. Secondary carious lesion: | —Alfa: no carious lesion in the marginal zone; |
| —Bravo: caries in the marginal zone of the restoration resulting in an area repair or replacement of the entire restoration. |
2.7. Statistical Analysis
SPSS version 23 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. The Shapiro–Wilk test showed a non-normal data distribution. Kruskal–Wallis testing was used for mean comparison. A series of Mann–Whitney tests were applied for multiple comparisons. Significance for the purposes of post hoc tests was adjusted using the Bonferroni method; a p-value < 0.001 was considered significant. The Bonferroni adjustment method was used to counteract the statistical type I error in the study resulting from performing multiple Mann–Whitney comparisons.
3. Results
The choice of restoration method and restoration material is determined by several different parameters. These include the condition of the hard dental tissues of the tooth, the color of the existing tooth and adjacent teeth, the position of the tooth in the dental arch, the esthetic expectations of the patient, and the skills of the treating team—the clinician and dental technician who will implement the treatment. The use of composite cement improved the integration between the tooth and the restoration, transferring the external forces to the dentin. As a result, we observed an increase in ceramic resistance, which enhances the clinical durability of these restorations [20,21].
The results after the clinical evaluation of the indirect ceramic restorations in the 2nd, 5th, and 10th years after cementation are shown in Table 2.

Table 2.
Percentage distribution, frequency, and USPHS criteria scores for the three periods.
During the first follow-up period, postoperative sensitivity was found to be 2.32% (Table 2), and on detailed analysis, it was found that this was grade “Bravo” 4.55% from observed molars in Group II (Table 3). In 2.38% of the restorations in Group I, they do not conform to the existing anatomical form but lack exposed dentin for the first period of observation (Table 3).

Table 3.
Distribution of the results according to the criteria of USPHS from the first period (2nd year) of follow-up in the two groups.
In contrast to the results obtained during the first follow-up period, during the second period (5th year), there was a decrease in the value for Criterion 3 (1.16%), preservation of the same value for Criterion 4 (1.16%), and appearance of grade “Bravo” and grade “Charlie” in Criteria 5 and 6. Regarding the assessment of proximal contacts, the grade “Bravo” is 5.95% (for 5 clinical cases) and the grade “Charlie” is 2.32% in two clinical cases (Table 2). The group distribution shows higher values for grade “Bravo” in molars and both Criteria 5 and 6, specifically 6.82% and 4.55% in Group II, and 4.76% and 2.38% in Group I of premolars (Table 4).

Table 4.
Distribution of the results according to the criteria of USPHS from the second period (5th year) of follow-up in the two groups.
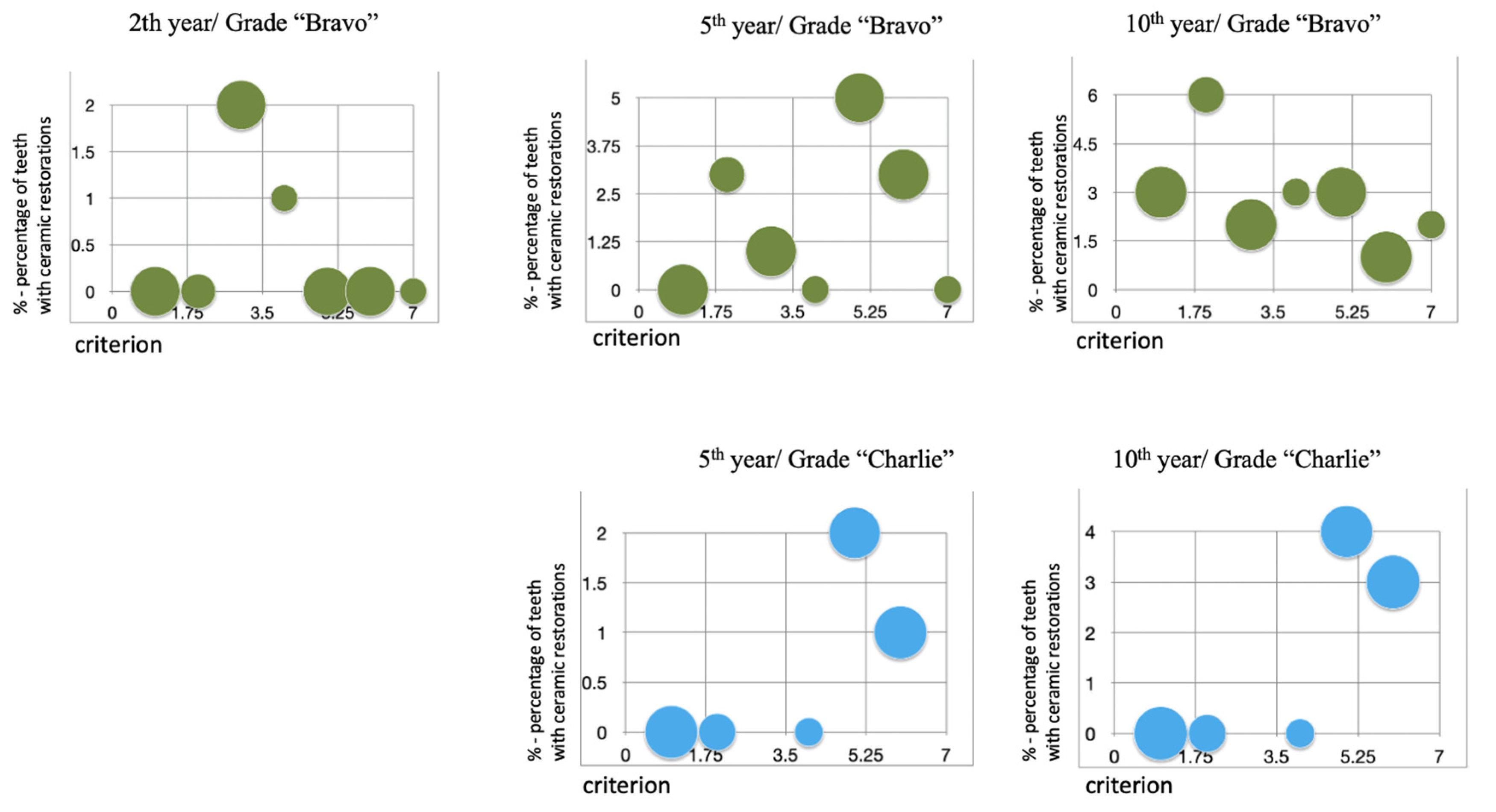
The 10-year long-term follow-up shows an entrainment of the “Bravo” grade in all USPHS criteria studied. There was an increase in Criteria 2 to 6 over the second follow-up period (Table 5). The “Charlie” rate remained unchanged at Criterion 5 over the 5-year evaluation period (4.54%). In Criterion 6, an increase was found for the 10-year follow-up compared to the 5-year follow-up, from 2.27% to 4.54% (Table 5). Data analysis identified the first occurrence of a grade of “Bravo” in Criteria 1, 4, and 7 over the 10-year follow-up period; the same for both criteria was 4.55% (Table 5). Four of the all-studied restorations (n = 86) had to be replaced at year 5 follow-up because of fracture (failure rate 4.65%; Kaplan–Maier). There are no restorations with bulky, cohesive fractures. Group II demonstrated a satisfactory success rate in terms of color matching and secondary carious lesions during the 5-year follow-up period (Table 5, Figure 1).

Table 5.
Distribution of the results according to the criteria of USPHS from the third period (10th year) of follow-up in the two groups.
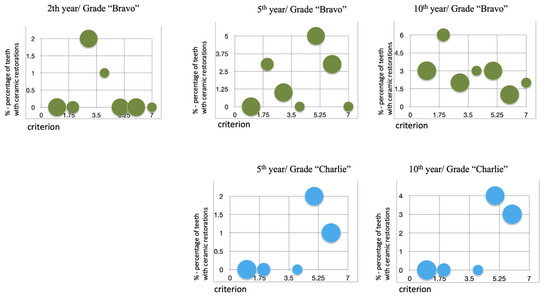
Figure 1.
Graphical distribution of clinical cases by different period for grades “Bravo” and “Charlie” against criteria.
Two of the restorations (2.32%) showed a significant deterioration in marginal adaptation (Friedman’s 2-way ANOVA; p = 0.05) over the presented 10-year period. In total, 97.68% of the restorations showed satisfactory marginal adaptation to the enamel structure (Table 2). In two of the teeth with ceramic restorations, we observed postoperative sensitivity for about two months during the initial follow-up period, and one of the clinical cases maintained longer-term sensitivity to normal irritants for about two years and six months. We found postoperative sensitivity of about two months in indirect restorations in three different individuals, eliminating the speculation that this is an individually determined hypersensitivity. Two of the clinical cases showed sensitivity to thermal irritants that began to manifest around the 8th year after the fixation of the ceramic overlay, and they did not coincide with the clinical cases that showed a short-term sensitivity of two months or a long-term sensitivity of 2.5 years.
4. Discussion
Examinations in clinical practice reveal distal teeth with outdated direct restorations, necessitating their replacement with indirect restorations that are more resilient to masticatory forces. One of the modern materials of interest in recent years is the lithium disilicate ceramic, e.Max Press (Ivoclar AG, Liechtenstein, Schaan). This material has shown esthetic properties approaching or equal to those of leucite-reinforced glass-ceramic materials but has significantly better strength properties and provides a high level of esthetic restoration for restorations in the distal zone. Researchers have conducted numerous in vitro studies on ceramic restorations, primarily focusing on areas such as fit, marginal accuracy, gap location, cement thickness [22,23,24], micro-leakage [25,26,27], nano-leakage, fracture resistance [28], and the impact of different cements [29,30,31].
Hybrid composite blocks (CERASMART), as an alternative material for single indirect restoration, overcome the disadvantages of direct composite resins and the lack of polymerization defects induced during their application [32]. Composite blocks with increased filler loading have better clinical performance under intraoral loading conditions [33]. Accordingly, some researchers suggested using materials with similar elastic moduli as dentin, whatever composite blocks are, to achieve a more reasonable stress distribution [34]. However, the efficiency of machinable composites is still controversial as their mechanical properties are lower than those of ceramics [35].
Some papers discussed that lithium dislocates are not biologically inert, and that many have a similar cytotoxicity dynamic regardless of small differences in composition or processing [36]. Insufficiently effective enamel bonding or material fatigue can lead to failures due to the degradation and destruction of the adhesive layer and cementum. Therefore, the best possible adaptation of the tooth structure is required for these restorations, including the restoration margins and cavity shape [21,37]. The results of this study clearly demonstrate that the main problem is the boundary between restoration and tooth structure. According to Krämer N et al., every clinical study evaluating ceramic restorations reported some deterioration in the marginal zone’s quality. Insufficient bonding to the enamel, degradation of the cementing agent, or fatigue of the materials may cause this [38].
The negative results observed for marginal adaptation occurred in the first few months. This fact clearly shows that the main concern in this type of restoration should be the initial adaptation of the ceramic material at the time of cementation and the first months of use, as well as the material and technique used to cement these restorations [39,40,41]. Scientific research and clinical experience confirm the use of adhesively fixed restorations to meet tooth esthetic demands, and we may have entered the so-called “post-amalgam era” described by [42]. Regarding the preparation of distal ceramic restorations, some authors have demonstrated that occlusal reduction leads to a reduced chance of restoration failure, thereby increasing the durability of the restoration [43,44]. Fracture resistance tests are used to determine the forces that can induce fracture (cohesive or adhesive) in such restorations, thus enabling a proposed preparation design that can provide the greatest resistance. Coelho Santos et al., in a controlled clinical trial, evaluated the clinical performance of ceramic inlays and onlays made with two systems: sintered (Duceram, Dentsply-Degussa = D) and pressed (IPS Empress, Ivoclar = IPS) after two years. Eighty-six restorations (n = 86), forty-four IPS and forty-two D, were cemented in the mouths of 35 patients. A total of 27 premolars and 59 molars were prepared for Class II, for a total of 33 onlays and 53 inlays. The author’s conclusion is that these two types of ceramic materials demonstrate excellent clinical results after two years [45].
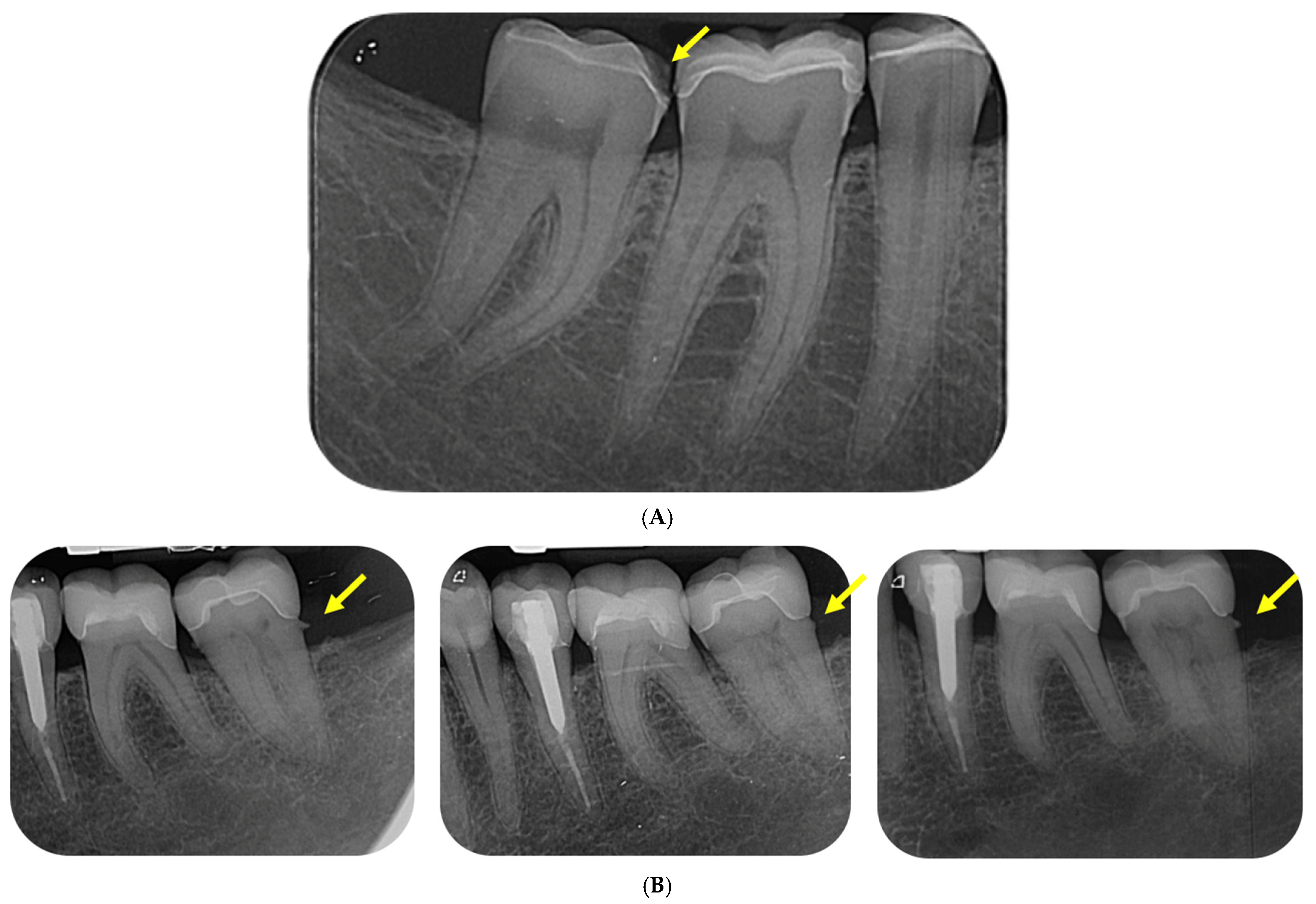
Back in 2000, Hayashi M. et al. evaluated the quality of feldspar ceramics after eight years in vivo. Durability was observed in 80% of feldspar ceramic inlay restorations after eight years (Kaplan–Meier method), although at six-year reporting, it was 92%, which differs from the results obtained in the present study—95.35% for both 5-year and 10-year follow-up. A change was observed from the 5-year period to the 10-year period, where the “Charlie” rate increased from 1.16% to 3.49%, or from one clinical case to three of the total number of followed cases (n = 86) (Table 2). The results show that the “Charlie” grade under criterion 6—“Marginal integrity”—fracture of the restoration or missing part or the entire obturation, leads to the replacement of the ceramic restoration with a new one three times in a 5-year period (from the 5th to the 10th year), but the increase in durability is related to the increase in the resistance of the materials and the increase in their strength (Figure 2 and Figure 3). Hayashi M. et al.’s follow-up revealed marginal fractures in 11 restorations (22%), with 5 (11%) experiencing volume fractures for the first time in the previous two years. We observed recurrent caries in 3 (7%) cases and marginal staining in 14 (31%). SEM evaluation revealed marginal microfractures in 77% of the restorations, wear in 36%, and edge wear in 74% at eight years. No significant difference was observed between molars and premolars [46]. One of the cases (#47) with cohesive fracture in the present clinical trial is presented in Figure 4A.

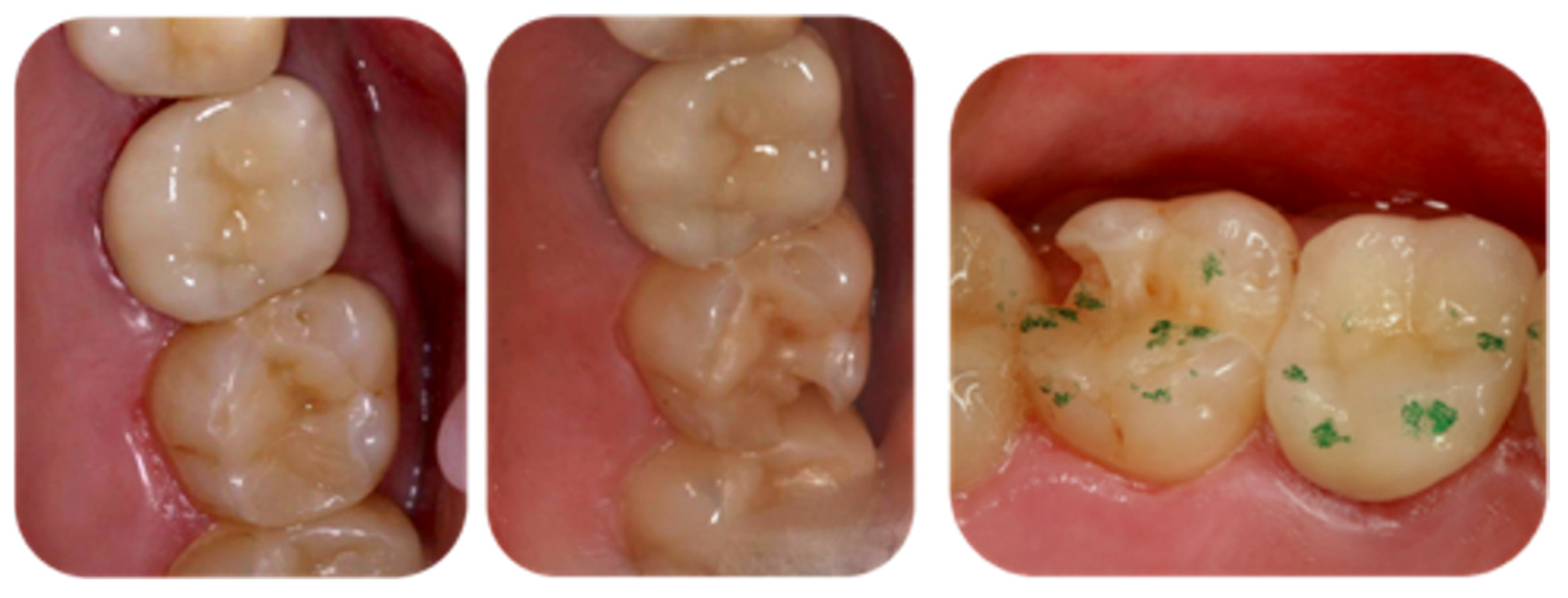
Figure 2.
The M-D fracture on tooth 27, which was restored with e.Max Press indirect ceramic overlay. The fracture was identified in the fifth year after overlay cementation—during the second follow-up period.

Figure 3.
The fracture of occlusal marginal distal ridge was identified during the third follow-up period.
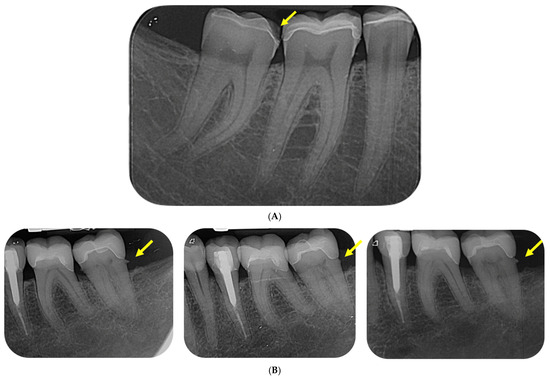
Figure 4.
(A). The radiograph shows cohesive fracture of medial side of lower-right second molar (#47); (B). The radiographs show postoperative monitoring status of #36 and 37—in second, fifth, and tenth year. There is a gap formation on the distal gingival base (yellow arrows) of tooth #37. In the monitoring of tooth #36, there are no radiographic signs of gap formation.
The results of the present study clearly show that the main problems are the interproximal contact and the destruction of the marginal integrity between the restoration and the tooth structures (Table 2).
In a review of the scientific literature (PubMed /Medline/, CENTRAL/Cochrane/ and Embase databases), Holme (2021) found that the lowest failure rates were found in metal restorations, ranging from 0–11%. The failure rate of ceramic inlays, onlays, and overlays is 5–9%. The author found that the most common failure of ceramic restorations was fracture of the restoration, while caries was the most common cause of failure of gold restorations. Holme W.’s analysis revealed that the risk of bias was high for all studies, with a low level of evidence. A single meta-analysis has compared conventionally cemented metal and adhesively cemented ceramic restorations, demonstrating a significantly lower relative risk of failure for conventionally cemented metal indirect restorations compared to adhesively cemented ceramic indirect restorations [47].
One of the serious problems that has remained for decades is still the impossibility of maximum adaptation in the marginal approximal areas where the level is below or at that of the interdental soft tissues. The clinical study included a tooth that we have been following for more than 10 years, with a radiographically diagnosed cleft at the distal gingival base. Due to the patient’s lack of symptoms, the case is being followed for longer, but the change in the indirect restoration is also planned (Figure 4B).
Gateva and Kabaktchieva demonstrated that applying the same adhesive system with the same clinical protocol resulted in the formation of an adhesive and hybrid layer with different characteristics [48]. Considering the hybrid layer analysis, we can hypothesize that some of the failures of indirect ceramic restorations are the result of an ineffective hybrid layer [48,49,50].
Tagtekin et al. discovered that ceramic restorations usually fractured in the first 6 to 8 months [51]. However, Table 1 shows that fractures happened in the 5th and 10th years, with three times as many cases going from a gap or fissure where no dentin is visible to a restoration breaking or part of the obturation being missing.
A meta-analysis presented by Naik et al., in 2022, found that partially ceramic restorations (feldspar porcelain and glass-ceramic) outperformed partially composite restorations at both 5-year and 10-year follow-up. When comparing ceramic types, glass-ceramic outperformed feldspar porcelain at 5-year follow-up, and feldspar porcelain outperformed glass-ceramic at 10-year follow-up. Failures were mainly due to fractures (6.2%), endodontic problems (3%), secondary caries (1.7%), and detachment, which was 0.9% [52].
Santos M. et al. found in their clinical study that fractures, recurrent caries, and reduced marginal integrity over time were the main causes of ceramic restoration failure. They believe that careful monitoring of the ceramic–tooth interface can prolong clinical durability [53]. Brandt S. et al., in their evaluation of clinical survival and success rates, find that the use of IPS e.Max could be recommended in the restoration of non-vital as well [54].
The failures may stem from various mechanical, biological, and procedural factors. Understanding the specific types of failures and their causes is essential for optimizing treatment planning and improving long-term outcomes.
They could be grouped as follows: fracture of the ceramic restoration, debonding of the restoration, marginal leakage, wear of the opposing dentition, tooth fracture, esthetic failures, and caries development. Failures of indirect ceramic restorations in the distal area arise from a combination of mechanical stress, biological factors, and procedural errors. Fractures, debonding, marginal leakage, and tooth or restoration wear are common issues, driven by factors such as excessive occlusal forces, material properties, inadequate adhesive techniques, and improper preparation. Understanding these failure modes and their causes is essential for improving the design, material selection, and clinical protocols associated with ceramic restorations in the posterior regions. Long-term success can be enhanced by addressing patient-specific risk factors such as bruxism, optimizing adhesive procedures, and ensuring careful occlusal adjustments during placement and follow-up.
In this clinical study, the application of e.Max Press indirect ceramic restorations for distal teeth demonstrated a high success rate of 99.4% for the 2-year follow-up period, and 97.4 and 95.35% for the 5- and 10-year follow-up periods, respectively. Failure in 4.65% of cases over a 10-year period shows that correctly defined indications, strict adherence to the recommendations of the manufacturer, both in terms of the application of the adhesive system and in terms of laboratory parameters and protocol, make one highly sensitive, risky, and multi-stage manipulation, a technique with a high rate of predictability of 10 years.
5. Conclusions
Despite this study’s limitations, biomimetic restorations demonstrate satisfactory results after a 5-year follow-up period, offering a viable treatment option for dental practices with a success rate ranging from 91.73 to 98.84%. If you obtain a grade “Alfa”, which means that everything went perfectly in terms of color matching, anatomical shape, and secondary carious defects, you can be sure that you followed the manufacturer’s instructions to the letter, both when it came to using the adhesive system and following the lab’s rules and procedures. This is a risky and multi-step process that has a high success rate of 5 years. The obtained satisfactory results, which show a 93.03 percent absence of marginal staining, a 97.68% absence of postoperative sensitivity, and a 95.35% preservation of marginal persistence over a 10-year period, provide sufficient support for the high rate of long-term healing associated with indirect ceramic restorations. It should be noted that the limitation of the present clinical study is related to the number of followed cases (n = 86), which is a prerequisite for future clinical long-term follow-ups with a larger number of indirect restorations included.
Future scientific research and follow-up of the long-term durability of indirect restorations may be directed to a more detailed analysis of indirect restorations in the light of minimally invasive treatment, analysis of the biomimetic factors responsible for this, and creation of a time-resistant hybrid layer.
Author Contributions
Conceptualization, A.G.; methodology, A.G.; software, A.G.; validation, N.N., M.D.-G. and A.G.; formal analysis, N.N., M.D.-G. and A.G.; investigation, N.N. and A.G.; resources, N.N.; data curation, N.N.; writing—original draft preparation, A.G.; writing—review and editing, N.N. and A.G.; visualization, N.N.; supervision, A.G. and M.D.-G.; project administration, A.G.; and final editing of the manuscript, A.G and M.D.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of CENIMUS (for Grant Project 39/16 September 2009).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Christensen, G.J. Is the rush to all-ceramic crowns justified? J. Am. Dent. Assoc. 2014, 145, 192–194. [Google Scholar] [CrossRef]
- Burian, G.; Erdelt, K.; Schweiger, J.; Keul, C.; Edelhoff, D.; Güth, J.-F. In-vivo-wear in composite and ceramic full mouth rehabilitations over 3 years. Sci. Rep. 2021, 11, 14056. [Google Scholar] [CrossRef]
- Creugers, N.H.; Mentink, A.G.; Fokkinga, W.A.; Kreulen, C.M. 5-year follow-up of a prospective clinical study on various types of core restorations. Int. J. Prosthodont. 2005, 18, 34–39. [Google Scholar] [CrossRef]
- Opdam, N.J.; Bronkhorst, E.M.; Roeters, J.M.; Loomans, B.A. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J. Adhes. Dent. 2007, 9, 469–475. [Google Scholar] [CrossRef]
- Krifka, S.; Anthofer, T.; Fritzsch, M.; Hiller, K.A.; Schmalz, G.; Federlin, M. Ceramic inlays and partial ceramic crowns: Influence of remaining cusp wall thickness on the marginal integrity and enamel crack formation in vitro. Oper. Dent. 2009, 34, 32–42. [Google Scholar] [CrossRef]
- Manhart, J.; Chen, H.Y.; Mehl, A.; Hickel, R. Clinical study of indirect composite resin inlays in posterior stress-bearing preparations placed by dental students: Results after 6 months and 1, 2, and 3 years. Quintessence Int. 2010, 41, 399–410. [Google Scholar]
- Haralur, S.B.; Al-Qahtani, A.S.; Al-Qarni, M.M.; Al-Homrany, R.M.; Aboalkhair, A.E. Influence of remaining dentin wall thickness on the fracture strength of endodontically treated tooth. J. Conserv. Dent. 2016, 19, 63–67. [Google Scholar] [CrossRef]
- Corrêa, G.; Brondani, L.P.; Wandscher, V.F.; Pereira, G.K.R.; Valandro, L.F.; Bergoli, C.D. Influence of remaining coronal thickness and height on biomechanical behavior of endodontically treated teeth: Survival rates, load to fracture and finite element analysis. J. Appl. Oral Sci. 2018, 26, e20170313. [Google Scholar] [CrossRef]
- Laajala, A.; Karhatsu, P.; Pesonen, P.; Laitala, M.L.; Näpänkangas, R.; Raustia, A.; Anttonen, V. Association of indirect restorations with past caries history and present need for restorative treatment in the northern Finland birth cohort. Clin. Oral Investig. 2018, 22, 1495–1501. [Google Scholar] [CrossRef]
- Malament, K.A.; Socransky, S.S. Survival of dicor glass-ceramic dental restorations over 14 years. Part II: Effect of thickness of Dicor material and design of tooth preparation. J. Prosthet. Dent. 1999, 81, 662–667. [Google Scholar] [CrossRef]
- Li, Z.; Gao, C.; Xu, Y.; Xu, J. Three years retrospective clinical evaluation of endodontically treated premolars restored by cast ceramic onlays. West. Chin. J. Stomatol. 2015, 33, 263–266. [Google Scholar] [CrossRef]
- Al Amri, M.D.; Al-Johany, S.; Sherfudhin, H.; Al Shammari, B.; Al Mohefer, S.; Al Saloum, M.; Al Qarni, H. Fracture resistance of endodontically treated mandibular first molars with conservative access cavity and different restorative techniques: An in vitro study. Aust. Endod. J. 2016, 42, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Merrill, T.C.; Mackey, T.; Luc, R.; Lung, D.; Naseem, A.; Abduo, J. Effect of chairside CAD/CAM restoration type on marginal fit accuracy: A comparison of crown, inlay and onlay restorations. Eur. J. Prosthodont. Restor. Dent. 2021, 29, 119–127. [Google Scholar] [PubMed]
- de Assis, C.; Lemos, C.; Gomes, J.; Vasconcelos, B.; Moraes, S.; Braz, R.; Pellizzer, E.P. Clinical Efficiency of Self-etching One-Step and Two-Step Adhesives in NCCL: A Systematic Review and Meta-analysis. Oper. Dent. 2020, 45, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, S.; Rebello de Sampaio, F.B.; Braga, M.M.; Sesma, N.; Özcan, M. Survival Rate of Resin and Ceramic Inlays, Onlays, and Overlays: A Systematic Review and Meta-analysis. J. Dent. Res. 2016, 95, 985–994. [Google Scholar] [CrossRef]
- Srimaneepong, V.; Heboyan, A.; Zafar, M.S.; Khurshid, Z.; Marya, A.; Fernandes, G.V.O.; Rokaya, D. Fixed Prosthetic Restorations and Periodontal Health: A Narrative Review. J. Funct. Biomater. 2022, 13, 15. [Google Scholar] [CrossRef]
- Abdulrahman, S.; Von See Mahm, C.; Talabani, R.; Abdulateef, D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: A retrospective study. BMC Oral Health 2021, 21, 625. [Google Scholar] [CrossRef]
- Piwowarczyk, A.; Lauer, H.C.; Sorensen, J.A. Microleakage of various cementing agents for full cast crowns. Dent. Mater. 2005, 21, 445–453. [Google Scholar] [CrossRef]
- Cvar, J.F.; Ryje, G. Reprint of criteria for the clinical evaluation of dental restorative materials. Clin. Oral Investig. 2005, 9, 215–232. [Google Scholar] [CrossRef]
- Yüksel, E.; Zaimoğlu, A. Influence of marginal fit and cement types on microleakage of all-ceramic crown systems. Braz. Oral Res. 2011, 25, 261–266. [Google Scholar] [CrossRef]
- Forberger, N.; Göhring, T.N. Influence of the type of post and core on in vitro marginal continuity, fracture resistance, and fracture mode of lithia disilicate-based all-ceramic crowns. J. Prosthet. Dent. 2008, 100, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Blunck, U.; Fischer, S.; Hajtó, J.; Frei, S.; Frankenberger, R. Ceramic laminate veneers: Effect of preparation design and ceramic thickness on fracture resistance and marginal quality in vitro. Clin. Oral Investig. 2020, 24, 2745–2754. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Sambrook, R.J. Longevity of ceramic onlays: A systematic review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef]
- Sirous, S.; Navadeh, A.; Ebrahimgol, S.; Atri, F. Effect of preparation design on marginal adaptation and fracture strength of ceramic occlusal veneers: A systematic review. Clin. Exp. Dent. Res. 2022, 8, 1391–1403. [Google Scholar] [CrossRef]
- Fathpour, K.; Bazazzade, A.; Mirmohammadi, H. A Comparative Study of Cervical Composite Restorations Microleakage Using Dental Universal Bonding and Two-step Self-etch Adhesive. J. Contemp. Dent. Pract. 2021, 22, 1035–1040. [Google Scholar] [CrossRef]
- Duquia Rde, C.; Osinaga, P.W.; Demarco, F.F.; de VHabekost, L.; Conceição, E.N. Cervical microleakage in MOD restorations: In vitro comparison of indirect and direct composite. Oper. Dent. 2006, 31, 682–687. [Google Scholar] [CrossRef]
- Daghrery, A.; Yaman, P.; Lynch, M.; Dennison, J. Evaluation of micro-CT in the assessment of microleakage under bulk fill composite restorations. Am. J. Dent. 2022, 35, 128–132. [Google Scholar]
- Yoon, H.I.; Sohn, P.J.; Jin, S.; Elani, H.; Lee, S.J. Fracture Resistance of CAD/CAM-Fabricated Lithium Disilicate MOD Inlays and Onlays with Various Cavity Preparation Designs. J. Prosthodont. 2019, 28, e524–e529. [Google Scholar] [CrossRef] [PubMed]
- Falacho, R.I.; Marques, J.A.; Palma, P.J.; Roseiro, L.; Caramelo, F.; Ramos, J.C.; Guerra, F.; Blatz, M.B. Luting indirect restorations with resin cements versus composite resins: Effects of preheating and ultrasound energy on film thickness. J. Esthet. Restor. Dent. 2022, 34, 641–649. [Google Scholar] [CrossRef]
- de la Macorra, J.C.; Pradíes, G. Conventional and adhesive luting cements. Clin. Oral Investig. 2002, 6, 198–204. [Google Scholar] [CrossRef]
- Leung, G.K.; Wong, A.W.; Chu, C.H.; Yu, O.Y. Update on Dental Luting Materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- Kirilova, J.; Kirov, D.; Petrova-Pashova, V. Five-year clinical study of indirect aesthetic restorations—Onlays. Medinfo 2023, 10, 1618–1624. [Google Scholar] [CrossRef]
- Papathanasiou, I.; Kamposiora, P.; Dimitriadis, K.; Papavasiliou, G.; Zinelis, S. In vitro evaluation of CAD/CAM composite materials. J. Dent. 2023, 136, 104623. [Google Scholar] [CrossRef]
- Garoushi, S.; Barlas, D.; Vallittu, P.K.; Uctasli, M.B.; Lassila, L. Fracture behavior of short fiber-reinforced CAD/CAM inlay restorations after cyclic fatigue aging. Odontology 2024, 112, 138–147. [Google Scholar] [CrossRef]
- Belli, R.; Wendler, M.; de Ligny, D.; Cicconi, M.R.; Petschelt, A.; Peterlik, H.; Lohbauer, U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017, 33, 84–98. [Google Scholar] [CrossRef]
- Brackett, M.G.; Lockwood, P.E.; Messer, R.L.; Lewis, J.B.; Bouillaguet, S.; Wataha, J.C. In vitro cytotoxic response to lithium disilicate dental ceramics. Dent. Mater. 2008, 24, 450–456. [Google Scholar] [CrossRef]
- Yancheva, S.; Vasileva, R. In vitro study of the marginal adaptation and microleakage in Class II restorations of conventional and matrix-modified composites. Dent. Med. 2013, 95, 19–28. [Google Scholar]
- Krämer, N.; Ebert, J.; Petschelt, A.; Frankenberger, R. Ceramic inlays bonded with two adhesives after 4 years. Dent. Mater. 2006, 22, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Clinical performance of resin-matrix ceramic partial coverage restorations: A systematic review. Clin. Oral Investig. 2022, 26, 3807–3822. [Google Scholar] [CrossRef] [PubMed]
- Thordrup, M. A 5-year clinical study of indirect and direct resin composite and ceramic inlays. Quintessence Int. 2001, 32, 199–205. [Google Scholar]
- Mangani, F.; Marini, S.; Barabanti, N.; Preti, A.; Cerutti, A. The success of indirect restorations in posterior teeth: A systematic review of the literature. Minerva Stomatol. 2015, 64, 231–240. [Google Scholar] [PubMed]
- Magne, P. Composite resins and bonded porcelain: The postamalgam era? J. Calif. Dent. Assoc. 2006, 34, 135–147. [Google Scholar] [CrossRef] [PubMed]
- Nirmala, S.; Goud, S.; Kumar, K.N.; Chukka, R.R.; Reddy, N. Ceramic Onlay: A Case Report. Cureus 2022, 14, e32641. [Google Scholar] [CrossRef] [PubMed]
- Politano, G.; Fabianelli, A.; Papacchini, F.; Cerutti, A. The use of bonded partial ceramic restorations to recover heavily compromised teeth. Int. J. Esthet. Dent. 2016, 11, 314–336. [Google Scholar] [PubMed]
- Coelho Santos, M.; Lauris, J.; Navarro, M. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: Two-year clinical follow up. Oper. Dent. 2004, 29, 123–130. [Google Scholar]
- Hayashi, M.; Tsuchitani, Y.; Kawamura, Y.; Miura, M.; Takeshige, F.; Ebisu, S. Eight-year clinical evaluation of fired ceramic inlays. Oper. Dent. 2000, 25, 473–481. [Google Scholar]
- Holme, W. Gold versus ceramic—Which will last longer for posterior indirect restorations? Evid. Based Dent. 2022, 23, 166–167. [Google Scholar] [CrossRef]
- Gateva, N.; Kabaktchieva, R. Hybrid layer thickness in primary and permanent teeth—A comparison between total etch adhesives. J. IMAB 2012, 18, 191–199. [Google Scholar] [CrossRef][Green Version]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P. Buonocore memorial lecture. Adhesion growth and dentin: Current status and future challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar]
- Walshaw, P.; Tam, L.; McComb, D. Bond failure at dentin-composite interfaces with ‘single-bottle’ adhesives. J. Dent. 2003, 31, 117–125. [Google Scholar] [CrossRef]
- Tagtekin, D.; Ozyöney, G.; Yanikoglu, F. Two-year clinical evaluation of IPS Empress II ceramic onlays/inlays. Oper. Dent. 2009, 34, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Naik, V.B.; Jain, A.K.; Rao, R.D.; Naik, B.D. Comparative evaluation of clinical performance of ceramic and resin inlays, onlays, and overlays: A systematic review and meta-analysis. J. Conserv. Dent. 2022, 25, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.J.; Freitas, M.C.; Azevedo, L.M.; Santos, G.C., Jr.; Navarro, M.F.; Francischone, C.E.; Mondelli, R.F. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: 12-year follow-up. Clin. Oral Investig. 2016, 20, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Brandt, S.; Winter, A.; Lauer, H.C.; Kollmar, F.; Portscher-Kim, S.J.; Romanos, G.E. IPS e.max for All-Ceramic Restorations: Clinical Survival and Success Rates of Full-Coverage Crowns and Fixed Partial Dentures. Materials 2019, 12, 462. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).