Abstract
Tic disorders (TDs) are neurodevelopmental conditions which affect 0.3–0.9% of individuals aged < 18 years. Although tics often improve or resolve spontaneously over time, treatment is often recommended. Pharmacological approaches are widely used as primary interventions. However, their side effects encouraged the development and the interest in nonpharmacological approaches, whose efficacy in pediatric populations remains poorly understood. This systematic review aimed to evaluate the efficacy of nonpharmacological treatments for children and adolescents with TDs. A literature review was performed using PubMed, EBSCOhost, and JABA databases up to 16 May 2024. Eligible articles were randomized controlled trials, written in English and published in peer-reviewed journals, investigating the efficacy of nonpharmacological treatments in pediatric populations diagnosed with TDs. Significant evidence supported the efficacy of behavioral interventions such as the Comprehensive Behavioral Intervention for Tics (CBIT), its reduced version the Habit Reversal Therapy (HRT), and the Exposure and Relapse Prevention (ERP) in reducing tics and tic-related impairment among young people, as assessed through the Yale Global Tic Severity Scale. Behavioral interventions were generally effective in reducing tics, although some studies reported higher effects on motor tics when compared to vocal tics. High level of efficacy was observed for both face-to-face and online treatments. While future studies are needed to improve treatment effects, especially on vocal tics, as well as to have a better understanding of treatment components and modalities, taken together, the present findings support the use of nonpharmacological intervention for TDs in youth.
1. Introduction
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines tics as sudden, rapid, recurrent, nonrhythmic motor movements or vocalizations. They can be classified as either simple or complex, based upon their duration, ranging from short (i.e., milli-seconds) to long (i.e., seconds). A diagnosis of tic disorder (TD) is made when a subject under the age of 18 shows motor and/or vocal tics for a specific period of time, which are not attributable to another medical condition or substance use [1]. TDs are highly prevalent in the developmental age population, although prevalence estimates vary widely (0.03–5.26%) [2]. Current studies indicate that the prevalence of TDs in children and adolescents ranges between 0.3–0.9% [2,3]. There are three main diagnostic categories of TD: Tourette’s Disorder (or Tourette’s Syndrome, TS), persistent (chronic) motor or vocal tic disorder (CTD), and provisional tic disorder (PTD). These categories are hierarchical, with variations in the presence and duration of motor and/or vocal tics. TS requires both motor and vocal tics, CTD requires only one type, while PTD may include either or both types of tics, differing primarily in duration. TS and CTD symptoms must occur for at least one year, whereas PTD symptoms last less than one year [1]. The worldwide prevalence of these three diagnostic categories of TD indicates that PTD is the most common with a prevalence of 2.99%, followed by CTD and TS with prevalence of 1.61% and 0.77%, respectively [4]. Given the neurodevelopmental nature of TDs, which therefore must be diagnosed before age 18, and their high prevalence in children and adolescents, this systematic review focuses on the group aged < 18 years.
Understanding the etiopathogenesis of TDs provides crucial insights into their development and progression. A key factor in the pathophysiology of TDs is the dysfunction of the cortico–striatal–thalamus–cortical circuit, which involves motor, sensory, and limbic regions. A critical aspect involves the dysregulation of dopaminergic pathways, where presynaptic regulatory abnormalities, combined with phasic dysfunctions in dopaminergic transmission, seems to disrupt normal motor control. Furthermore, the serotonergic system has been repeatedly reported to be impaired, adding complexity to the neurochemical profile. Even though genetic studies highlight the strong hereditary nature of these disorders, the onset seems to be ultimately driven by a complex interplay between genetic predispositions and environmental factors that shapes their development and progression [5].
Moreover, tics often improve over time, with a significant reduction in adolescence continuing into adulthood, when the intensity and frequency of tics may decrease to the extent that they no longer cause impairment [6]. Although tics often resolve spontaneously over time without treatment, some individuals need interventions to reduce difficulties in social, emotional, and behavioral functioning [7]. Given the severity of tic-related impairments and their long-term implications, having a thorough understanding of the best treatment options for TDs in developmental age is highly relevant and clinically important.
Historically, pharmacological interventions, including traditional and atypical antipsychotics, analgesics, and anticonvulsants, have been considered the first-line treatment for TS symptoms [8,9]. However, long-term medication use can lead to adverse side effects and treatment discontinuation, suggesting that pharmacological treatments may not provide satisfactory outcome for all, or complete relief of symptoms [8]. Nonpharmacological treatments, therefore, emerged as viable alternative or adjunct to the pharmacological ones [7], reducing concerns associated with side effects of drug use [10]. Behavioral therapies, such as Habit Reversal Therapy (HRT) [11,12], Comprehensive Behavioral Intervention for Tics (CBIT) [11,12], Massed Negative Practice (MNP) [9,13] and Relaxation Therapy (RT) [9,14], are the most commonly studied nonpharmacological treatments for TDs. Overall, these treatments seem to show an efficacy comparable to pharmacological interventions, with sustained post-treatment benefits [15]. Consequently, nonpharmacological treatments are increasingly considered as first-line options for TD management in several countries [10].
Comprehensive systematic reviews of nonpharmacological treatments for children and adolescents with TDs are currently lacking. As the existing literature does not provide evidence on different treatment effects depending on the TD type—TS, CTD, and PTD [7]—it is reasonable to focus on the overall effectiveness of interventions in reducing tic severity. To our knowledge, only a few systematic reviews analyze the efficacy of TD treatments in pediatric age, considering both pharmacological and nonpharmacological (behavioral, physical, and dietary) interventions, either separately or in combination [11,12]. Although some systematic reviews examined nonpharmacological interventions, specifically behavioral therapies, none specifically focused on children and adolescents [16,17]; moreover, the research was often limited to TS, rather than comprehensively addressing TDs [17]. Finally, none of these reviews investigated online treatments, despite recent works on online behavioral therapies for TDs in youth [18,19]. The importance of online interventions for children and adolescents is now established in the treatment of several psychological conditions, accelerated by the COVID-19 global pandemic, which limited their access to traditional face-to-face treatment [11,20,21,22].
Given the growing evidence supporting the use of nonpharmacological treatments for TDs and the gaps in the existing literature, the current review was aimed at assessing the effectiveness of nonpharmacological treatments (both face to face and online) for pediatric TDs, focusing on randomized controlled trials studies. A differential treatment effect on motor tics, vocal tics, and level of impairment was also explored.
2. Methods
2.1. Eligibility Criteria
The eligibility criteria identification was conducted through the PICOS search strategy (Participants, Intervention, Comparison, Outcome, Research Design). Since the present systematic review aimed to analyze randomized controlled trials assessing the efficacy of nonpharmacological treatments for pediatric TDs, the following studies were included: (1) analyzing the efficacy of nonpharmacological treatments, (2) using RCTs, (3) focusing on populations of children and adolescents (aged < 18), (4) focusing on populations with a diagnosis of TD, and (5) having been published in peer-reviewed journals. Articles were excluded according to the following criteria: (1) analyzing the efficacy of pharmacological or neurostimulation treatments, (2) not using standardized diagnostic and outcome measures, (3) focused only on the adult population, (4) without a diagnosis of TD or TD in comorbidity with other disorders, (5) systematic reviews, meta-analyses, theses, and books, and (6) articles not written in English.
2.2. Information Sources and Search Strategy
A comprehensive systematic literature search was conducted in the following databases: PubMed, EBSCOhost (within which the following databases were included: APA PsycInfo, APA PsycArticles, PSYNDEX Literature with PSYNDEX Tests, and ERIC), and JABA. Table A1 provides for each database consulted the name, the interface or the platform used, as well as the coverage dates. The literature search ended on 16 May 2024. The keywords used for article selection across all databases were: (treat*) AND (efficac* OR effectiv*) AND (“tic disorder” OR tics) NOT pharmac*. The keywords were chosen independently of other systematic reviews or scientific articles, and the asterisk at the end of some keywords was used to maximize search results. The lack of evidence of a potential impact of different types of tics (TS, CTD, and PTD) on treatment efficacy led to the decision of not including “Tourette Syndrome” (or any synonym) as a keyword, and resulted in a focus on the overall effectiveness of interventions in reducing tic severity. Finally, to ensure a comprehensive coverage of the literature, no filters were applied regarding publication year, article type, gender, or age groups.
2.3. Selection Process
Four researchers reviewed the titles and abstracts of all articles independently and, in a second step, evaluated full-text articles for inclusion. In case of discrepancies, consensus on which articles to include was achieved through discussion.
3. Results
3.1. Study Selection
The selection process for the present systematic review was done in accordance with the PRISMA guidelines [23]. After the duplicates’ removal, articles were screened based on their titles and abstracts. Finally, full-text assessment was conducted on the remaining studies, and the suitable articles were selected and included in the systematic review.
The literature search initially yielded 1418 articles from PubMed (n = 584), EBSCOhost (n = 768), and JABA (n = 66) databases, resulting in 1304 articles after duplicates removal. Of these, 1196 were excluded based on the title and the abstract. The remaining 108 articles were filtered through full-text reading. Among these, nine articles (PubMed—n = 7; EBSCOhost—n = 2) met all criteria and were included in the systematic review. The PRISMA flowchart showing the selection process is presented in Figure A1.
Of the fourteen articles initially identified as eligible, three [24,25,26] were excluded as not reporting outcome data. Additionally, one article [27] was removed as a pilot study of the research already included [21], and one [28] because vitamins supplement was provided to the youth in addition to the behavioral treatment.
3.2. Studies Characteristics
All nine articles included in the present systematic review used a RCT design. All articles were recently published, in a period ranging from 2010 [15] to 2024 [29]. Four studies were conducted in Europe: two in England (one in a specialist clinic for Tourette Syndrome in a London hospital [30] and one across two Child and Adolescent Mental Health Services [22]), another one in Sweden, in the Child and Adolescent Psychiatry Research Center in Stockholm [21], and one in the Netherlands, by the Dutch Tourette Association [29]. Two studies were carried out in Israel, one in the Pediatric Movement Disorders Clinic at the Dana-Dwek Children’s Hospital (DDCH) and the other by the Tourette Syndrome Association (TSAI) [20,31]. Another study was conducted across three American universities: Johns Hopkins University in Baltimore (Maryland), the University of California at Los Angeles, and the University of Wisconsin-Milwaukee [15]. The remaining two studies did not specify the research location [18,19]. In all the studies, participants were randomly assigned to the experimental group (the treatment was delivered either via videoconference or face-to-face) or to the control group. While active control groups received a parallel intervention [18,19,20,21,22,30,31], participants of passive control groups did not receive any treatment [15] or received the same intervention after some time [29].
A total of 844 children and adolescents were studied, 428 of which were included in the experimental group, while 416 in the control group. The sample size ranged from 18 [18] to 224 subjects [22], and the age of participants from 7 to 18 years. Moreover, studies were consistent in terms of the measurement tools used (see the Section 3.2.2), although they differed in the intervention methods, number of subjects, and follow-up periods. All study characteristics are summarized in Table A2.
3.2.1. Subject Selection
All studies were consistent in the sample recruitment process. Participants were first required to have a primary diagnosis of TS or CTD according to DSM-5 criteria. They were then asked to complete the Yale Global Tic Severity Scale (YGTS) to determine whether their motor and/or vocal tic severity was over the YGTSS cutoff for identifying TD according to the specific thresholds adopted by the authors (among the studies, a cutoff score of 14 was often used for TD). Another criterion concerned participants’ intellectual level (IQ > 75 or 80) and proficiency in their native language. Moreover, most of the studies investigated participants’ clinical history in order to identify potential comorbidities, such as Attention Deficit Hyperactivity Disorder (ADHD) [18,20,21,22,29,30,31], anxiety disorders (all studies), and Obsessive-Compulsive Disorder (OCD) [15,18,20,21,22,29,30,31]. Subjects with comorbidities were not excluded unless they required immediate treatment; however, the influence of these co-occurring conditions was not thoroughly analyzed. Subjects were excluded when they showed one of the following conditions: a current diagnosis of substance abuse/dependence, suicidality or self-injurious tics, psychotic disorders, a history of behavioral treatments for tics, recent changes (e.g., within the previous four weeks) in drug treatment status, or planned changes in drug treatment status over the course of the treatment.
For studies involving Internet-based interventions, additional requirements included the cooperation of caregivers/parents [15,18,19,20] and access to a computer with Internet access and a web camera.
3.2.2. Assessment Method: The Yale Global Tic Severity Scale (YGTSS)
The Yale Global Tic Severity Scale (YGTSS) has been recognized as the gold standard for assessing tic severity in patients with TS and other TDs [32]. The YGTSS is a clinician-administered instrument that includes a symptom checklist, evaluating motor and vocal tic severity, and an overall impairment scale. To evaluate tic severity, the examiner rates five dimensions on a scale from 0 to 5: (1) number of tics, (2) frequency, (3) duration, (4) intensity, and (5) complexity. Each dimension is assessed separately for motor and vocal tics, resulting in subscale scores for both motor and vocal tics (ranging from 0 to 25). These subscales are then combined to provide a total tic severity score (ranging from 0 to 50), with higher scores indicating more severe tics. The YGTSS has demonstrated acceptable internal consistency, as well as convergent and divergent validity [18,32]. This measure was used at both baseline and follow-up in all the studies included in the present systematic review, thus ensuring a high homogeneity across the nine studies reviewed (see the Section 4).
3.2.3. Classification of Interventions
Treatment programs have been examined to identify theoretical foundations, objectives, modalities, and validity. As previously highlighted, studies were highly heterogeneous in the treatments models and modalities (see Table A3), with overall durations ranging from a minimum of three weeks [29] to a maximum of ten weeks [15,19,21,22]. The majority of the studies implemented protocols of eight to ten sessions [15,18,19,20,21,22,31], with each session generally lasting 60–90 min [15,19,30,31]. Interventions were administered by therapists with varying levels of experience, from recent graduates [20,21,30] to clinicians with extensive practice experience [15,18,19,22,29,31].
Notably, all interventions had a behavioral approach [4]. Furthermore, the Comprehensive Behavioral Intervention for Tics (CBIT) emerged as the most widely recognized and validated program for treating children and adults with TS and CTD, demonstrating a significant validity and relevance in the recent literature [15,33].
Among the studies, different treatment approaches for TD symptoms were employed: the majority used the CBIT program [15,18,19,20,31], also in its reduced version, the HRT [30], while others applied the ERP [21,22,29]. In particular, four studies examined an Internet-based adaptation of these interventions [19,20,21,22], others adhered to the traditional face-to-face format [15,29,30,31], and one used both modalities [18]. With the only exception of Heijerman-Holtgrefe and colleagues [29], in all studies, children and adolescents received parental support [15,18,19,20,21,22,30,31]. Three studies investigated a group-based adaptation of these interventions [29,30,31], while the others maintained the original individual administration format [15,18,19,20,21,22].
Despite structure variations, all treatment programs aimed at reducing or mitigating symptoms associated with tic disorders. The following section provides a brief overview of each treatment program
Comprehensive Behavioral Intervention for Tics (CBIT). CBIT is acknowledged as a primary therapeutic approach for managing tics [34]. Evidence supports CBIT’s efficacy and safety in treating tics across pediatric and adult populations. It is a manualized behavioral therapy of eight sessions over ten weeks, with optional booster sessions, including psychoeducation, functional analysis, and relaxation training [15,34]. The success of CBIT is based on the active engagement of patients, involving collaboration with the therapist, completion of assigned homework, and active participation in the sessions.
Internet-based guided self-help Comprehensive Behavioral Intervention for Tics (ICBIT). ICBIT represents an adaptation of CBIT: It is a caregiver-led self-help program with minimal therapist involvement, delivered through telepsychotherapy. The primary goals of this program are to provide both the child and the caregiver with specific behavioral and cognitive strategies for managing tics and to facilitate caregiver support, particularly for those unable to access in-person therapy [20]. ICBIT is commonly administered through an encrypted, purpose-designed online platform. An example included in this systematic review is the Barninternetprojektet (Child Internet Project, BIP) [27]. The intervention consists of nine consecutive joint child-caregiver modules delivered over a nine-week period, with a training duration of 20 to 30 min. The ICBIT incorporates a wide range of techniques, including psychoeducation, functional analysis of interactions, HRT, maintaining gains, and relapse prevention [20]. In addition to these steps, the CBIT-VoIP includes diaphragmatic breathing, progressive muscle relaxation, and behavioral rewards [19].
Habit Reversal Training (HRT). The treatment is based on a structured program of ten chapters (modules) containing age-appropriate textual materials, animations, videos, and exercises over a period of ten weeks. These sessions are facilitated by therapists and by in-person assistants. In HRT, of which CBIT is the extended version, participants are guided to focus on one tic at a time, to enhance their awareness of these tics and prevent their occurrence by employing alternative responses. In eleven videos specifically developed for this purpose, a clinical psychologist shows a wide range of competing responses, corresponding to distinct muscle groups [30].
Exposure and Response prevention Program (ERP). In ERP, participants are asked to engage in exercises aimed at simultaneously suppressing tics (response avoidance) followed by a systematic process of gradually eliciting bodily sensations (premonitory stimuli), also achieved with the involvement of parents, to increase the challenge of tic suppression (exposure). The Internet-delivered ERP includes a built-in stopwatch to facilitate the practice of tic suppression, with children encouraged to extend the duration of tic suppression over time [21].
Tackle your Tics (TYT). It is a four-days group intervention, based on ERP. Similarly to ERP, participants are trained to simultaneously suppress all their tics for an extended period, while focusing on tolerating the preceding sensations (premonitory urges) or ‘tic alarms’. However, unlike ERP, the TYT program involves daily one-hour workshops, which are led by young adult patients and focused on living with and managing tics [29].
3.3. Results of Individual Studies
A summary of the main results of the included studies is provided in the next section (see the Section 3.4). The results of the individual studies included are presented in Table A4 and Table A5.
3.4. Results of Syntheses
The effectiveness of CBIT treatment was specifically investigated in two studies [15,31]. One study [15] reported a significant reduction in the YGTSS Total Tic score after the CBIT intervention with a decrease of 7.6 points in the experimental group from baseline to post-treatment. Instead, the control group showed only a 3.5 points reduction in the YGTSS Total Tic score between the two evaluations.
Conversely, in the second study [31], an initial increase in the YGTSS Total Tic score was observed in both the experimental and the control group at the first assessment post-intervention, followed by a significant decrease at the follow-up (especially in the experimental group). Trends were different for motor tics, vocal tics, and level of impairment: motor tics and level of impairment significantly decreased in the subjects of the group-based CBIT (a reduction of 32% of motor tics was observed immediately after the CBIT and was maintained at the 3-month follow-up), as well as in the control group (the reduction of 42.8% in motor tics after the psychoeducation was followed by an increase of 76.5%). Instead, a significant increase in vocal tics was observed in both the group-based CBIT (+106%), and the control group (+107%) at the first assessment post-intervention, followed by a significant decrease at the follow-up (with vocal tics decreasing by 65.7% in the group-based CBIT and by 74.8% in the EIT group).
Another article [30] investigated the efficacy of Habit Reversal Training (HRT), compared to an educational intervention. The findings indicated a significant improvement in the Motor Tics score for the HRT group, while no improvement was observed in the Vocal Tic Severity subscale. These results suggest that HRT may yield greater improvements in motor tics, compared to the educational intervention [30].
One article examined the efficacy of an intensive Exposure and Response prevention Program (ERP), called “Tackle your Tics” (TYT) [29]. In this study, the intervention group received TYT treatment, while the control group had to wait three months before receiving the same intervention. The YGTSS total tic score showed a reduction of 3.14 points in the TYT group. The waiting-list group exhibited a spontaneous reduction in tic severity during the waiting period, and after receiving the treatment, there was a 2.85 points reduction in the YGTSS total tic score. Furthermore, no significant group differences were found in the mean decrease of motor and vocal tics, with both scores showing significant reductions [29].
The remaining studies [18,19,20,21] investigate the effectiveness of behavioral treatments administered via telehealth or the Internet. These studies examined CBIT delivered via telehealth [18], CBIT provided through Voice over Internet Protocol (VoIP) [19], Internet-based CBIT (ICBT) [20], and Internet-delivered ERP [21]. The findings support the hypothesis that CBIT can be an effective intervention even when administered in an Internet-based way. For telehealth-administered CBIT, the YGTSS Total Tic Severity score decreased by 7.8 points at post-treatment, compared to a 6.5 point reduction following face-to-face CBIT [18]. The slight difference suggests that CBIT can be effectively administered via telehealth without a loss of efficacy. Regarding CBIT-VoIP, a significant difference was found between the Total Tic score at baseline versus post-treatment, with a decrease of 7.25 points at post-treatment, compared to a reduction of only 1.75 points in the control group [19]. This statistically significant difference suggests the effectiveness of CBIT delivered via telematics. The Internet-based CBIT was also effective in treating young people with CTD [20]. This way of delivering CBIT resulted in a significant reduction in the YGTSS Motor Tic and Impairment score. Although there was no immediate improvement in the Vocal Tic Score post-treatment, a significant reduction in phonic tics was observed at follow-up [20].
The Internet-delivered ERP was also associated with improvements. In one study, higher treatment response rates were observed, compared to an online psychoeducation program [21]. In a second study [22], in which the online ERP was compared to the psychoeducation, at the first (12-month) and second (18-month) follow-up with YGTSS-TTSS, decreases of 2.46 points and 2.01 points, respectively, were observed. These results highlight the efficacy of online ERP over online psychoeducation.
Follow-Ups
The majority of the analyzed studies (seven out of nine) conducted follow-up assessments to examine treatment effectiveness over extended periods. These follow-ups were conducted at various intervals, including three [15,20,21,29,31], four [18], six [15,20,22], twelve [22], and eighteen months [22] following treatment administration.
Throughout the follow-up assessments, a significant drop-out of participants was observed, resulting in a substantial reduction in the total number of subjects included. Despite the dropouts, all follow-ups confirmed the effectiveness of the treatments examined: CBIT [15,31], CBIT delivered by telehealth [18], Internet-delivered ERP [21,22], ICBIT [20], and TYT [29].
4. Discussion
The purpose of the present systematic review was to examine extant research investigating the efficacy of nonpharmacological interventions for TDs in children and adolescents. Since the literature lacks of explicit evidence on the potential impact of different types of tics (TS, CTD, and PTD) on treatment efficacy [7], the focus was placed on the therapeutic effects of nonpharmacological interventions on tic severity. The differential treatment effect on motor tics, vocal/phonic tics, and level of impairment was explored.
Overall, findings confirmed the efficacy of psychosocial and behavioral treatments, which could be considered as first-line interventions for pediatric patients with TDs [17,35]. Among the different behavioral interventions, the studies primarily focused on HRT [30], ERP [21,22], an intense form of ERP called TYT [29], and CBIT [15,18,19,20,31]. The effectiveness of HRT [7,11,12,35,36,37,38,39], ERP [7,35,36,37,40], and CBIT [11,12,36,38,41] has been extensively examined and validated in the scientific literature, in both recent and prior studies.
In addition, the present review provided support to the effectiveness of behavioral interventions when administered online [18,19,20,21]. The implementation of telehealth interventions, such as the ICBIT program, has many advantages: not only facilitating a continuous and uninterrupted treatment [20], but also enhancing the accessibility to care [20,21], particularly for children who are unable to access any form of face-to-face therapy for tics [22], and therefore, reaching a broader population of youth [21]. Finally, online behavioral therapies for tics may be optimally effective as a primary interventions with nonresponders or partial responders who can subsequently be treated with more intensive face-to-face therapy [22].
An interesting result was that in six out of nine studies [15,19,20,29,30,31] exploring motor tics, vocal tics, and tic-related impairment, behavioral interventions were generally effective in reducing motor tics, with effect sizes ranging from 0.22 to 1.07. This finding is consistent with a previous review and meta-analysis [42] conducted on adults, which showed that nonpharmacological therapy is effective, compared to the control group, especially for motor tics. The CBIT-VoIP [19] appeared to be the most effective treatment in reducing motor tics (1.07), possibly related to the inclusion of techniques such as diaphragmatic breathing and progressive muscle relaxation in the online version. Conversely, the sole implementation of HRT [30] appears to show only a modest effect on motor tic reduction, in accordance with previous studies conducted on adults [42]. Therefore, it seems that a more comprehensive and multimodal intervention—incorporating a combination of behavioral, educational, and stress management techniques—may be more effective in reducing motor tics. Moreover, group-based CBIT interventions focusing on tic reduction were associated to more lasting effects [31], suggesting a role of social support in motor tics improvement. However, it should also be considered that children with behavioral difficulties such as aggressive and attention problems benefited less from group interventions [29,30,31].
Greater variability in the effectiveness of behavioral treatments has been observed in the reduction of vocal tics, with effect sizes ranging from −0.28 to 1.32. Notably, three studies reported a lower effectiveness on vocal tics when compared to motor tics [19,20,30]. The authors hypothesized that this result could be related to the intervention protocol, focusing on a few tics which were experienced by children as the most distressing [30,43]. Because of this procedure, in fact, the youths often preferred to work on motor tics (e.g., in the study by Zimmerman-Brenner and colleagues [31], where the authors noted that 76.5% of participants primarily chose to focus on their motor tics). Additionally, other authors suggest a delayed impact of the intervention on vocal tics, with more significant improvements observed in follow-up phases [20,31]. Other explanations are related to differences in neurobiological substrate [44] and higher sensitivity of vocal tics to environmental and social conditions [45,46]. It is known, for example, that tics tend to increase with social attention and decrease with isolation [47]: during discussions about tics (“tic-talk”) or in group-based interventions, a higher increase in vocal tics compared to motor tics can be observed [29,30,31,48]. In this case, it could be hypothesized that group settings could contribute to the maintenance of some tics, especially vocal tics [31].
Finally, regarding the type of intervention, as in the case of motor tics, bigger improvements in vocal tics were observed for the Comprehensive Behavioral Intervention for Tics (CBIT), independently of the delivery method used [15,19,20,29,30,31].
Overall, studies [15,19,20,21,22,29,31] have shown that both the CBIT (delivered online or in-person) and the Internet-based ERP were effective in improving tic-related impairments in children and adolescents with TDs. Improvements appeared to be associated with enhancements in quality of life, as well as in emotional and behavioral functioning [29], with results comparable to those observed with other treatments (e.g., [43,49]). Specifically, studies by Zimmerman-Brenner and colleagues [31] and Hollis and colleagues [22] suggested that CBIT and ERP are particularly effective not only in managing tics, but also in reducing comorbid conditions, such as anxiety and behavioral symptoms. These findings are consistent with previous reports highlighting the contribution of behavioral interventions and supportive psychoeducational strategies in addressing anxiety and behavioral problems in youths [49,50]. Similarly, techniques such as relaxation [14,49] may contribute to improvements in emotional and behavioral well-being. Therefore, these interventions offer benefits which goes far beyond tic management, suggesting that an integrated approach, also addressing comorbid conditions and incorporating complementary techniques, might be particularly effective.
This systematic review provides novel insight into the use of behavioral therapies (CBIT, HRT, and ERP) delivered either online or face-to-face, summarizing its effectiveness on motor, vocal tics, and tic-related impairments. Overall, the interventions were associated with high satisfaction levels among children and adolescents. The observed tics reduction and response rates aligned with those reported in previous trials on pharmacological interventions for tic reduction in pediatric populations [51,52], thus confirming the validity of recommending nonpharmacological treatments as first-line alternatives in the management of tic disorders in children and adolescents [7].
In light of the side-effects associated with the use of pharmacological medications for TDs [7], it is of primary importance to explore alternative treatment modalities. Therefore, the results of the present review significantly add to the literature by supporting the efficacy and the use of nonpharmacological treatments for TDs in pediatric populations.
4.1. Limitations
The present systematic review addressed a gap in the scientific literature by including RCT studies, focusing exclusively on children and adolescents, as well investigating both online and face-to-face interventions in all selected studies.
However, it has some limitations which might affect the results and their generalizability. First, a larger number of articles could have provided more robust evidence regarding the effectiveness of nonpharmacological treatments.
Second, an area with a potential knowledge gap (and therefore, the topic of future research) lies in the limited data on the simultaneous use of pharmacological therapies [15]. While information on medication for TDs was collected at the beginning of each study, their potential influence on treatment outcomes was not explored. Furthermore, all studies included samples with comorbid conditions such as ADHD and OCD: these comorbidities were not excluded unless their severity required “immediate treatment”. The inclusion of subjects with other diagnoses or simultaneously treated with drugs may have influenced the treatment outcomes.
Third, the heterogeneity among the studies included represents a significant limitation. The use of different versions of CBIT and ERP, administered individually or in a group-based format, delivered either face-to-face or online, with different treatment duration and number of sessions, raises relevant challenges in drawing clear conclusions about effective interventions. Moreover, the involvement of different professionals with different levels of training may have introduced a bias effect. Specifically, interventions were administered by clinicians or therapists with masters-level or higher education [15,30], clinicians or therapists specialized in CBIT training [18,19,21,31], supervised master degree’s students [20], young adult patients supported by therapists with at least three years of experience [29], or through online expert support [22].
Fourth, the generalizability of the findings is reduced by the characteristics of the studies included in the present review. Primarily, the small sample size across the studies reduces the statistical power to address efficacy [18,19,20,31]. Additionally, all studies relied on self-reported measures, susceptible to potential bias. Notably, youths with minimal or marked impairment were excluded from one study [18].
A fifth limitation concerns the partial lack of assessment of long-term treatment effect. While two studies [19,30] did not include a follow-up assessment, the others showed differences in the follow-up period: at three and six month post-treatment [15,20], after three months [21,29,31], after four months [18], and after six, twelve, and eighteen months [22]. Due to all these reasons, the findings of the present review should be interpreted with caution.
Finally, during the selection process, several articles were unretrievable at the full-text level.
4.2. Future Studies
The present systematic review of the literature provided valuable insights into the efficacy of nonpharmacological treatments for TDs in individuals aged < 18 years, supporting the effectiveness of CBIT, its reduced version, HRT, and ERP treatments for tic reduction, also in samples with children and adolescents [12].
Areas for future studies are also highlighted. Research into the treatment of TDs should continue to evaluate the effectiveness of nonpharmacological interventions (especially on vocal tics), while also identifying those treatment components which are most essential to drive change: these includes, among others, the role of parental involvement [20,30] and stress management techniques. Effectiveness could be further explored by enhancing the understanding of predictors and moderators of response. Interventions’ efficacy should be investigated in different age groups (preschool, school-age, and adolescents) [15,18,19,20,21,29,30,31], as well as in different settings and modalities (individual and group-based). Group interventions, for example, might increase cost-effectiveness, reducing waiting times [30].
Moreover, while clinical and self-reported measures have been valuable in evaluating the efficacy of nonpharmacological interventions, future studies would benefit from incorporating objective, continuous measurement methods to capture the dynamic nature of tic activity. These tools, e.g., electromyography (EMG) or electroencephalography (EEG), would provide a more nuanced understanding of how tics evolve and respond to treatment, offering insights beyond episodic assessments, such as the YGTSS. For instance, EMG has been successfully applied in assessing motor function after stroke [53], and EEG has been widely used in epilepsy research [54]. Incorporating such methodologies into TDs research could enhance the precision of treatment evaluations and broaden the implications for future interventions.
The use of wider samples and rigorous methodologies will enhance the generalizability of results. Future research should aim to enroll larger cohorts, and include both short- and long-term follow-up assessments [19,20,31] to have a better understanding of the maintenance of treatment gains over time and provide clarity on long-term outcomes.
Regarding CBIT-VoIP treatments, it seems reasonable to investigate the relationship between computer- and Internet-related variables, such as access to technology, digital literacy, and treatment outcomes, in order to determine whether these factors influence treatment efficacy [19].
5. Conclusions
TD is a complex condition, frequently co-occurring with other psychological symptoms, such as OCD and ADHD. For tics that do not have a substantial improvement or resolution over time, several nonpharmacological treatment options are available and effective. More robust research in this domain will support the treatment of children and adolescents with TDs, reducing family and individual burden, improving a successful attainment of age-specific developmental tasks, and enhancing long-term wellbeing.
Author Contributions
Conceptualization, M.L., C.A., C.C., M.R. and E.B.; methodology, C.A. and C.C.; investigation, C.A., C.C., M.R. and E.B.; data curation, C.A. and C.C.; writing—original draft preparation, C.A., C.C., M.R. and E.B.; writing—review and editing, C.A., B.F. and C.C.; supervision, B.F., S.S. and M.L.; project administration, B.F. and M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The contributions presented in the study are included in the cited articles; further inquiries can be directed to the corresponding author.
Acknowledgments
The authors would like to thank Kamila Midor for proofreading this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
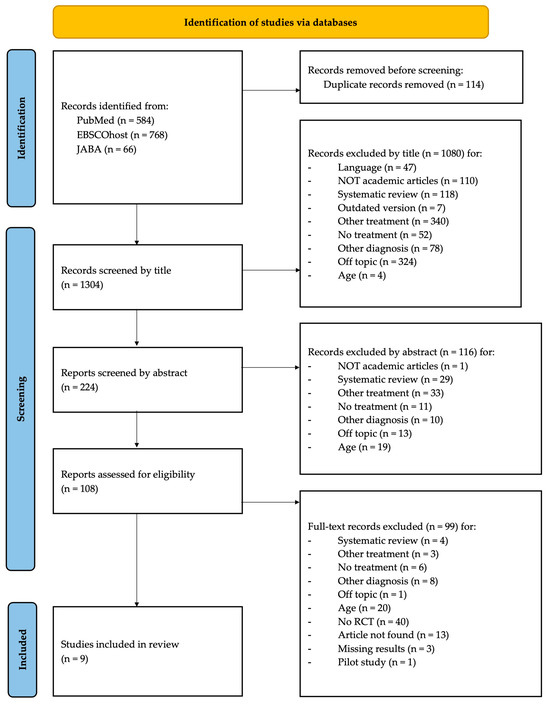
Figure A1.
PRISMA flowchart: study selection.
Figure A1.
PRISMA flowchart: study selection.
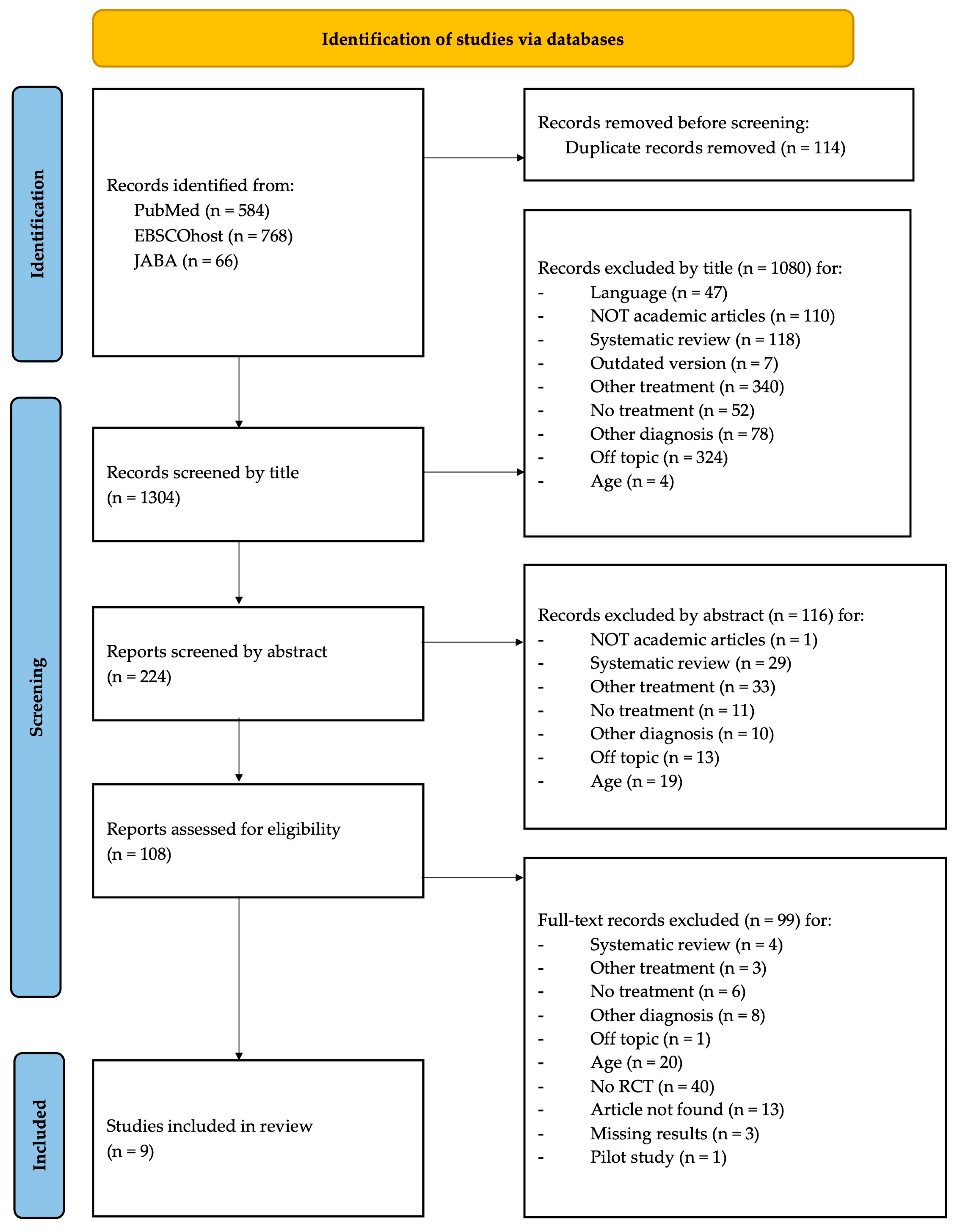

Table A1.
Database and coverage.
Table A1.
Database and coverage.
| Database | Coverage |
|---|---|
| PubMed | 1977 to present |
| EBSCOhost (APA PsycInfo, APA PsycArticles, PSYNDEX Literature with PSYNDEX Tests, ERIC) | 1951 to present |
| JABA | 1968 to present |
Note. The table displays the name, the interface, or the platform through which each consulted database was searched, as well as the dates of coverage.

Table A2.
Characteristics of the selected studies.
Table A2.
Characteristics of the selected studies.
| ID | Study and Year | Country | Sample Size (Male, %) | Age Range M [SD] | Diagnosis | Study Design |
|---|---|---|---|---|---|---|
| 1 | Piacentini et al. (2010) | United States of America | 126 (Male = 99; 79%) | 9–17 years 11.7 [2.30] | TS or CTD | Two-phase, multicenter, RCT |
| 2 | Himle et al. (2012) | - a | 18 (Male = 17; 94%) | 8–17 years 11.6 [2.70] | TS or CTD | Randomized Pilot Trial |
| 3 | Ricketts et al. (2012) | - | 20 (Male = 13; 65%) | 8–16 years 12.16 [2.34] | TS or CTD | Randomized Waitlist-controlled Pilot Trial |
| 4 | Yates et al. (2016) | England | 33 (Male = 25; 76%) | 9–13 years 10.96 [1.45] | TS or CTD | Single-blind RCT |
| 5 | Rachamim et al. (2020) | Israel | 41 (Male = 29; 71%) | 7–18 years 11.26 [1.94] | TS or CTD | RCT |
| 6 | Andrén et al. (2022) | Sweden | 221 (Male = 152; 69%) | 9–17 years 12.1 [2.30] | TS or CTD | Single-masked, parallel group, superiority RCT |
| 7 | Zimmerman-Brenner et al. (2022) | Israel | 55 (Male = 45; 82%) | 8–15 years 10.93 | TS or CTD | RCT |
| 8 | Hollis et al. (2023) | England | 224 (Male = 177; 79%) | 9–17 years | TS or CTD | Superiority parallel-group, single-blind, multicenter RCT |
| 9 | Heijerman-Holtgrefe et al. (2024) | The Netherlands | 106 (Male = 71; 67%) | 9–17 years 12.59 [2.11] | TS or CTD | Investigator-blinded RCT |
Notes. a— = The study does not specify the research location; TS = Tourette syndrome; CTD = chronic tic disorder; RCT = randomized control trial.

Table A3.
Characteristics of interventions.
Table A3.
Characteristics of interventions.
| ID | Study and Year | Intervention | Intervention’s Components | Delivered by | Timing | Follow Up |
|---|---|---|---|---|---|---|
| 1 | Piacentini et al. (2010) | CBIT | HRT (awareness training, competing response training), relaxation training, functional intervention | Therapists with master’s-level or higher education | 8 sessions (60 or 90 min long) during 10 weeks | 3-, 6-months |
| 2 | Himle et al. (2012) | Telehealth- delivered CBIT Face-to-Face- delivered CBIT | Psychoeducation, HRT, FAI, relaxation training | Therapists were level psychologists with extensive CBIT training | 6 weekly sessions + 2 bi-weekly sessions | 4-months |
| 3 | Ricketts et al. (2012) | CBIT-VoIP | HRT, psychoeducation, self-monitoring, FAI, diaphragmatic breathing, progressive muscle relaxation, behavioral rewards | Four master’s level therapists who were trained using the CBIT manual | 2 sessions (1.5 h long) + 6 sessions (1 h long) occurring over a 10-week period | - a |
| 4 | Yates et al. (2016) | HRT | Relaxation training, functional analysis | Five clinicians (three qualified and two in training) | 2 sessions (90 min long) + Other sessions (1 h long) | - |
| 5 | Rachamim et al. (2020) | ICBIT | Psycho-education, awareness training, stress management skills, identifying factors that exacerbate tics, education, maintaining intervention gains and relapse prevention | Students in a master’s degree program in Clinical Psychology, with no previous experience in providing CBIT or ICBIT, supervised by three clinicians | 9 consecutive conjoint child-caregiver modules, delivered over 9 weeks | 3-, 6-months |
| 6 | Andrén et al. (2022) | Internet delivered ERP | Practice tic suppression (response prevention) and gradually provoke premonitory urges to make the tic suppression more challenging (exposure) | Clinical or trainee psychologists with specific training | 10 modules delivered over 10 weeks | 3-, 6-, 12-months |
| 7 | Zimmerman-Brenner et al. (2022) | CBIT EIT | CBIT: psychoeducation, tic awareness, competing response training, functional intervention, relaxation training, rewards EIT: psychoeducation, supportive intervention | Two trained CBT therapists administered intervention sessions | 8 weekly sessions (60 or 90 min long) + 3 additional monthly booster sessions (60 min long) | 3-months |
| 8 | Hollis et al. (2023) | Internet delivered ERP | Online, therapist-supported ERP | Therapist | 10 modules delivered over 10 weeks | 3-, 6-, 12-, 18-months |
| 9 | Heijerman-Holtgrefe et al. (2024) | TYT | Condensed group treatment with evidence-based ERP, Workshops | Treatment: therapists with 3–15 years of experience assisted by co-therapists Workshops: given by experts by experience (young adult patients) | 3 weeks | 3-, 6-months |
Notes. CBIT = Comprehensive Behavioral Intervention for Tics; CBIT-VoIP = Voice over Internet Protocol-delivered CBIT; HRT = Habit Reversal Training; ICBIT = Internet-based CBIT; or-BT = Online Remote Behavior Therapy; ftf-BT = Face-To-Face Behavior Therapy; EIT = Educational Intervention for Tics; TYT = Tackle Your Tics treatment; FAI = Function-based Assessment and Intervention; a— = The study does not specify the presence and/or duration of follow-up.

Table A4.
Results of the selected studies.
Table A4.
Results of the selected studies.
| Yale Global Tic Severity Scale (YGTSS) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | |||||||||||||||||||||||
| Total Tic Score | Total Motor Score | Total Phonic Score | Impairment | Total Tic Score | Total Motor Score | Total Phonic Score | Impairment | |||||||||||||||||
| ID | B | PT | ES | B | PT | ES | B | PT | ES | B | PT | ES | B | PT | ES | B | PT | ES | B | PT | ES | B | PT | ES |
| 1 | 24.70 | 17.10 | 0.68 *** | 14.60 | 10.70 | 0.49 | 10.10 | 6.50 | 0.50 | 25.00 | 12.20 | 0.57 | 24.60 | 21.10 | - a | 14.60 | 12.50 | - | 10.00 | 8.60 | - | 23.40 | 16.40 | - |
| 2 | 23.40 [7.50] | 15.60 [9.80] | 0.54 * | - | - | - | - | - | - | - | - | - | 24.10 [3.90] | 17.60 [6.50] | 0.75 * | - | - | - | - | - | - | - | - | - |
| 3 | 25.75 [8.51] | 18.50 [7.75] | 0.90 *** | 16.33 [3.31] | 12.08 [3.48] | 1.07 ** | 9.42 [6.13] | 6.42 [5.89] | 0.57 * | 31.25 [9.16] | 20.83 [8.08] | 0.94 ** | 22.00 [5.71] | 20.25 [6.21] | 0.39 | 14.13 [1.96] | 13.13 [2.90] | 0.42 | 7.88 [5.33] | 7.13 [4.79] | 0.15 | 31.75 [6.27] | 28.00 [7.11] | 0.67 |
| 4 | - | - | - | 17.65 [4.74] | 15.12 [4.30] | 0.22 * | 12.71 [6.99] | 12.71 [5.61] | −0.28 | - | - | - | - | - | - | 16.31 [3.03] | 15.88 [2.28] | - | 12.63 [5.93] | 11.13 [5.82] | - | - | - | - |
| 5 | 22.72 [6.37] | 16.12 [7.96] | 0.20 ** | 16.48 [4.55] | 11.44 [6.09] | 0.40 *** | 6.24 [5.50] | 4.68 [5.05] | 0.03 | 33.60 [14.86] | 15.22 [12.38] | 0.18 ** | 21.88 [5.03] | 20.94 [7.83] | - | 14.31 [3.82] | 14.75 [3.13] | - | 7.57 [6.00] | 5.63 [6.02] | - | 30.00 [17.51] | 26.88 [16.21] | - |
| 6 | 22.25 [5.60] | 18.53 [5.94] | 0.44 *** | - | - | - | - | - | - | 18.38 [7.08] | 10.65 [8.68] | 1.00 *** | 23.01 [5.92] | 19.27 [7.20] | 0.60 *** | - | - | - | - | - | - | 18.73 [7.79] | 11.52 [9.59] | 1.00 *** |
| 7 | 24.80 [9.30] | 18.40 [11.50] | 0.86 *** | 14.30 [5.10] | 10.90 [6.20] | 0.73 ** | 10.60 [8.00] | 7.40 [6.60] | 1.32 *** | 20.80 [10.40] | 14.30 [12.30] | 0.75 *** | 22.00 [6.00] | 21.80 [9.00] | 1.09 *** | 14.00 [3.50] | 14.10 [4.30] | 0.96 *** | 8.00 [4.60] | 7.70 [5.70] | 1.95 *** | 21.70 [10.30] | 13.50 [13.70] | 0.72 ** |
| 8 | 28.40 [7.70] | 23.90 [8.20] | - | - | - | - | - | - | - | 23.80 [10.30] | 16.70 [10.40] | - | 28.40 [7.10] | 26.80 [7.30] | - | - | - | - | - | - | - | 22.90 [9.90] | 19.10 [10.90] | - |
| 9 | 26.79 [8.30] | 23.65 [7.85] | - | 16.27 [4.30] | 14.80 [3.99] | - | 10.52 [6.68] | 8.84 [6.39] | - | 24.04 [11.59] | 19.41 [13.18] | - | 29.61 [9.23] | 27.93 [10.41] | - | 17.74 [4.18] | 16.63 [4.99] | - | 11.87 [6.72] | 11.30 [6.97] | - | 27.41 [12.16] | 25.56 [12.24] | - |
Notes. B = Baseline. PT = Post Treatment. ES = Effect Size. a—= The study does not specify this data. * p ≤ 0.05, ** p ≤ 0.01, *** p ≤ 0.001.

Table A5.
Results of the follow-ups.
Table A5.
Results of the follow-ups.
| Yale Global Tic Severity Scale (YGTSS)—Total Tic Severity Score | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention Group | Control Group | ||||||||||||||
| ID | Study and Year | Baseline | PT | 3-mth | 4-mth | 6-mth | 12-mth | 18-mth | Baseline | PT | 3-mth | 4-mth | 6-mth | 12-mth | 18-mth |
| 1 | Piacentini et al. (2010) | 18.60 | 13.70 | 13.90 | - | 13.30 | - | - | 18.15 | 13.00 | 9.90 | - | 10.40 | - | - |
| 2 | Himle et al. (2012) | 23.40 | 15.60 | - a | 16.80 | - | - | - | 24.10 | 17.60 | - | 20.10 | - | - | - |
| 5 | Rachamim et al. (2020) | 20.58 | 12.47 | 9.36 | - | 8.72 | - | - | 21.88 | 20.94 | - | - | - | - | - |
| 6 | Andrén et al. (2022) | 22.25 | 18.53 | 16.17 | - | - | - | - | 23.01 | 19.27 | 17.72 | - | - | - | - |
| 7 | Zimmerman-Brenner et al. (2022) | 24.80 | 39.80 | 18.40 | - | - | - | - | 22.00 | 37.10 | 21.80 | - | - | - | - |
| 8 | Hollis et al. (2023) | 28.40 | 23.90 | - | - | 21.50 | 21.70 | 21.50 | 28.40 | 26.80 | - | - | 25.00 | 24.90 | 23.90 |
| 9 | Heijerman-Holtgrefe et al. (2024) | 26.79 | 23.65 | 21.43 | - | - | - | - | 29.61 | 27.93 | 26.76 | - | - | - | - |
Notes. PT = Post treatment. a The study does not specify this data.
References
- American Psychiatric Association. DSM-5: Manuale Diagnostico e Statistico dei Disturbi Mentali; R. Cortina: Milano, Italy, 2014. [Google Scholar]
- Scharf, J.M.; Miller, L.L.; Gauvin, C.A.; Alabiso, J.; Mathews, C.A.; Ben-Shlomo, Y. Population prevalence of Tourette syndrome: A systematic review and meta-analysis: Meta-Analysis of TS Prevalence. Mov. Disord. 2015, 30, 221–228. [Google Scholar] [CrossRef]
- Scahill, L.; Specht, M.; Page, C. The prevalence of tic disorders and clinical characteristics in children. J. Obs.-Compuls. Relat. Disord. 2014, 3, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Knight, T.; Steeves, T.; Day, L.; Lowerison, M.; Jette, N.; Pringsheim, T. Prevalence of Tic Disorders: A Systematic Review and Meta-Analysis. Pediatr. Neurol. 2012, 47, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Ludolph, A.G.; Roessner, V.; Münchau, A.; Müller-Vahl, K. Tourette Syndrome and Other Tic Disorders in Childhood, Adolescence and Adulthood. Dtsch. Ärztebl. Int. 2012, 109, 821. [Google Scholar] [CrossRef] [PubMed]
- Pappert, E.J.; Goetz, C.G.; Louis, E.D.; Blasucci, L.; Leurgans, S. Objective assessments of longitudinal outcome in Gilles de la Tourette’s syndrome. Neurology 2003, 61, 936–940. [Google Scholar] [CrossRef] [PubMed]
- Cook, C.R.; Blacher, J. Evidence-based psychosocial treatments for tic disorders. Clin. Psychol. Sci. Pract. 2007, 14, 252–267. [Google Scholar] [CrossRef]
- Scahill, L.; Erenberg, G.; Berlin, C.M.; Budman, C.; Coffey, B.J.; Jankovic, J.; Kiessling, L.; King, R.A.; Kurlan, R.; Lang, A.; et al. Contemporary assessment and pharmacotherapy of Tourette syndrome. NeuroRX 2006, 3, 192–206. [Google Scholar] [CrossRef]
- Yang, C.; Cheng, X.; Zhang, Q.; Yu, D.; Li, J.; Zhang, L. Interventions for tic disorders: An updated overview of systematic reviews and meta analyses. Psychiatry Res. 2020, 287, 112905. [Google Scholar] [CrossRef]
- Blount, T.H. Intensive outpatient comprehensive behavioral intervention for tics: A case series. World J. Clin. Cases 2014, 2, 569. [Google Scholar] [CrossRef]
- Hollis, C.; Pennant, M.; Cuenca, J.; Glazebrook, C.; Kendall, T.; Whittington, C.; Stockton, S.; Larsson, L.; Bunton, P.; Dobson, S.; et al. Clinical effectiveness and patient perspectives of different treatment strategies for tics in children and adolescents with Tourette syndrome: A systematic review and qualitative analysis. Health Technol. Assess. 2016, 20, 1–450. [Google Scholar] [CrossRef]
- Whittington, C.; Pennant, M.; Kendall, T.; Glazebrook, C.; Trayner, P.; Groom, M.; Hedderly, T.; Heyman, I.; Jackson, G.; Jackson, S.; et al. Practitioner Review: Treatments for Tourette syndrome in children and young people—A systematic review. J. Child Psychol. Psychiatry 2016, 57, 988–1004. [Google Scholar] [CrossRef] [PubMed]
- Flancbaum, M.; Rockmore, L.; Franklin, M.E. Intensive Behavior Therapy for Tics: Implications for Clinical Practice and Overcoming Barriers to Treatment. J. Dev. Phys. Disabil. 2011, 23, 61–69. [Google Scholar] [CrossRef]
- Tilling, F.; Cavanna, A.E. Relaxation therapy as a treatment for tics in patients with Tourette syndrome: A systematic literature review. Neurol. Sci. 2020, 41, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Piacentini, J.; Woods, D.W.; Scahill, L.; Wilhelm, S.; Peterson, A.L.; Chang, S.; Ginsburg, G.S.; Deckersbach, T.; Dziura, J.; Levi-Pearl, S.; et al. Behavior Therapy for Children with Tourette Disorder: A Randomized Controlled Trial. JAMA 2010, 303, 1929. [Google Scholar] [CrossRef] [PubMed]
- Dutta, N.; Cavanna, A.E. The effectiveness of habit reversal therapy in the treatment of Tourette syndrome and other chronic tic disorders: A systematic review. Funct. Neurol. 2013, 28, 7–12. [Google Scholar]
- Wile, D.J.; Pringsheim, T.M. Behavior Therapy for Tourette Syndrome: A Systematic Review and Meta-analysis. Curr. Treat. Options Neurol. 2013, 15, 385–395. [Google Scholar] [CrossRef]
- Himle, M.B.; Freitag, M.; Walther, M.; Franklin, S.A.; Ely, L.; Woods, D.W. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav. Res. Ther. 2012, 50, 565–570. [Google Scholar] [CrossRef]
- Ricketts, E.J.; Goetz, A.R.; Capriotti, M.R.; Bauer, C.C.; Brei, N.G.; Himle, M.B.; Espil, F.M.; Snorrason, Í.; Ran, D.; Woods, D.W. A randomized waitlist-controlled pilot trial of voice over Internet protocol-delivered behavior therapy for youth with chronic tic disorders. J. Telemed. Telecare 2016, 22, 153–162. [Google Scholar] [CrossRef]
- Rachamim, L.; Zimmerman-Brenner, S.; Rachamim, O.; Mualem, H.; Zingboim, N.; Rotstein, M. Internet-based guided self-help comprehensive behavioral intervention for tics (ICBIT) for youth with tic disorders: A feasibility and effectiveness study with 6 month-follow-up. Eur. Child Adolesc. Psychiatry 2020, 31, 275–287. [Google Scholar] [CrossRef]
- Andrén, P.; Holmsved, M.; Ringberg, H.; Wachtmeister, V.; Isomura, K.; Aspvall, K.; Lenhard, F.; Hall, C.L.; Davies, E.B.; Murphy, T.; et al. Therapist-Supported Internet-Delivered Exposure and Response Prevention for Children and Adolescents with Tourette Syndrome: A Randomized Clinical Trial. JAMA Netw. Open 2022, 5, e2225614. [Google Scholar] [CrossRef]
- Hollis, C.; Hall, C.L.; Khan, K.; Jones, R.; Marston, L.; Le Novere, M.; Hunter, R.; Andrén, P.; Bennett, S.D.; Brown, B.J.; et al. Long-term clinical and cost-effectiveness of a therapist-supported online remote behavioural intervention for tics in children and adolescents: Extended 12- and 18-month follow-up of a single-blind randomised controlled trial. J. Child Psychol. Psychiatry 2023, 64, 941–951. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Andrén, P.; de la Cruz, L.F.; Isomura, K.; Lenhard, F.; Hall, C.L.; Davies, E.B.; Murphy, T.; Hollis, C.; Sampaio, F.; Feldman, I.; et al. Efficacy and cost-effectiveness of therapist-guided internet-delivered behaviour therapy for children and adolescents with Tourette syndrome: Study protocol for a single-blind randomised controlled trial. Trials 2021, 22, 669. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.L.; Davies, E.B.; Andrén, P.; Murphy, T.; Bennett, S.; Brown, B.J.; Brown, S.; Chamberlain, L.; Craven, M.P.; Evans, A.; et al. Investigating a therapist-guided, parent-assisted remote digital behavioural intervention for tics in children and adolescents—‘Online Remote Behavioural Intervention for Tics’ (ORBIT) trial: Protocol of an internal pilot study and single-blind randomised controlled trial. BMJ Open 2019, 9, e027583. [Google Scholar] [CrossRef] [PubMed]
- Heijerman-Holtgrefe, A.; Huyser, C.; Verdellen, C.; Van De Griendt, J.; Beljaars, L.; Kan, K.-J.; Lindauer, R.; Cath, D.; Hoekstra, P.; Utens, L. Effectiveness of ‘Tackle Your Tics’, a brief, intensive group-based exposure therapy programme for children with tic disorders: Study protocol of a randomised controlled trial. BMJ Open 2022, 12, e058534. [Google Scholar] [CrossRef]
- Andrén, P.; Aspvall, K.; Fernández de la Cruz, L.; Wiktor, P.; Romano, S.; Andersson, E.; Murphy, T.; Isomura, K.; Serlachius, E.; Mataix-Cols, D. Therapist-guided and parent-guided internet-delivered behaviour therapy for paediatric Tourette’s disorder: A pilot randomised controlled trial with long-term follow-up. BMJ Open 2019, 9, e024685. [Google Scholar] [CrossRef]
- Chen, C.; Wang, H.; Chang, H.; Hsueh, C. Effectiveness of a modified comprehensive behavioral intervention for tics for children and adolescents with tourette’s syndrome: A randomized controlled trial. J. Adv. Nurs. 2020, 76, 903–915. [Google Scholar] [CrossRef]
- Heijerman-Holtgrefe, A.P.; Huyser, C.; Bus, M.; Beljaars, L.P.L.; Van De Griendt, J.M.T.M.; Verdellen, C.W.J.; Kan, K.J.; Zijlstra, B.J.H.; Lindauer, R.J.L.; Cath, D.C.; et al. Tackle your Tics, a brief intensive group-based exposure treatment for young people with tics: Results of a randomised controlled trial. Eur. Child Adolesc. Psychiatry 2024. [Google Scholar] [CrossRef]
- Yates, R.; Edwards, K.; King, J.; Luzon, O.; Evangeli, M.; Stark, D.; McFarlane, F.; Heyman, I.; İnce, B.; Kodric, J.; et al. Habit reversal training and educational group treatments for children with tourette syndrome: A preliminary randomised controlled trial. Behav. Res. Ther. 2016, 80, 43–50. [Google Scholar] [CrossRef]
- Zimmerman-Brenner, S.; Pilowsky-Peleg, T.; Rachamim, L.; Ben-Zvi, A.; Gur, N.; Murphy, T.; Fattal-Valevski, A.; Rotstein, M. Group behavioral interventions for tics and comorbid symptoms in children with chronic tic disorders. Eur. Child Adolesc. Psychiatry 2022, 31, 637–648. [Google Scholar] [CrossRef]
- Storch, E.A.; Murphy, T.K.; Geffken, G.R.; Sajid, M.; Allen, P.; Roberti, J.W.; Goodman, W.K. Reliability and validity of the Yale Global Tic Severity Scale. Psychol. Assess. 2005, 17, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, S.; Peterson, A.L.; Piacentini, J.; Woods, D.W.; Deckersbach, T.; Sukhodolsky, D.G.; Chang, S.; Liu, H.; Dziura, J.; Walkup, J.T.; et al. Randomized Trial of Behavior Therapy for Adults with Tourette Syndrome. Arch. Gen. Psychiatry 2012, 69, 795. [Google Scholar] [CrossRef] [PubMed]
- Haas, M.; Jakubovski, E.; Fremer, C.; Dietrich, A.; Hoekstra, P.J.; Jäger, B.; Müller-Vahl, K.R.; The EMTICS Collaborative Group. Yale Global Tic Severity Scale (YGTSS): Psychometric Quality of the Gold Standard for Tic Assessment Based on the Large-Scale EMTICS Study. Front. Psychiatry 2021, 12, 626459. [Google Scholar] [CrossRef] [PubMed]
- Verdellen, C.; van de Griendt, J.; Hartmann, A.; Murphy, T.; the ESSTS Guidelines Group. European clinical guidelines for Tourette Syndrome and other tic disorders. Part III: Behavioural and psychosocial interventions. Eur. Child Adolesc. Psychiatry 2011, 20, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Essoe, J.K.-Y.; Grados, M.A.; Singer, H.S.; Myers, N.S.; McGuire, J.F. Evidence-based treatment of Tourette’s disorder and chronic tic disorders. Expert Rev. Neurother. 2019, 19, 1103–1115. [Google Scholar] [CrossRef]
- Franklin, S.A.; Walther, M.R.; Woods, D.W. Behavioral Interventions for Tic Disorders. Psychiatr. Clin. N. Am. 2010, 33, 641–655. [Google Scholar] [CrossRef]
- Hwang, G.C.; Tillberg, C.S.; Scahill, L. Habit Reversal Training for Children with Tourette Syndrome: Update and Review: Habit Reversal Training for Children with Tourette Syndrome: Update and Review. J. Child Adolesc. Psychiatr. Nurs. 2012, 25, 178–183. [Google Scholar] [CrossRef]
- Woods, D.W.; Miltenberger, R.G.; Lumley, V.A. Sequential Application of Major Habit-Reversal Components to Treat Motor Tics in Children. J. Appl. Behav. Anal. 1996, 29, 483–493. [Google Scholar] [CrossRef]
- Verdellen, C.W.J.; Keijsers, G.P.J.; Cath, D.C.; Hoogduin, C.A.L. Exposure with response prevention versus habit reversal in Tourettes’s syndrome: A controlled study. Behav. Res. Ther. 2004, 42, 501–511. [Google Scholar] [CrossRef]
- Bennett, S.M.; Capriotti, M.; Bauer, C.; Chang, S.; Keller, A.E.; Walkup, J.; Woods, D.; Piacentini, J. Development and Open Trial of a Psychosocial Intervention for Young Children with Chronic Tics: The CBIT-JR Study. Behav. Ther. 2020, 51, 659–669. [Google Scholar] [CrossRef]
- Shou, S.; Li, Y.; Fan, G.; Zhang, Q.; Yan, Y.; Lv, T.; Wang, J. The Efficacy of Cognitive Behavioral Therapy for Tic Disorder: A Meta-Analysis and a Literature Review. Front. Psychol. 2022, 13, 851250. [Google Scholar] [CrossRef] [PubMed]
- Dabrowski, J.; King, J.; Edwards, K.; Yates, R.; Heyman, I.; Zimmerman-Brenner, S.; Murphy, T. The Long-Term Effects of Group-Based Psychological Interventions for Children with Tourette Syndrome: A Randomized Controlled Trial. Behav. Ther. 2018, 49, 331–343. [Google Scholar] [CrossRef] [PubMed]
- McCairn, K.W.; Nagai, Y.; Hori, Y.; Ninomiya, T.; Kikuchi, E.; Lee, J.-Y.; Suhara, T.; Iriki, A.; Minamimoto, T.; Takada, M.; et al. A Primary Role for Nucleus Accumbens and Related Limbic Network in Vocal Tics. Neuron 2016, 89, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Goldman, K.J.; DeLeon, I.G. A Review on Functional Analyses of Tics. Behav. Modif. 2020, 44, 296–315. [Google Scholar] [CrossRef]
- Silva, R.R.; Munoz, D.M.; Barickman, J.; Friedhoff, A.J. Environmental Factors and Related Fluctuation of Symptoms in Children and Adolescents with Tourette’s Disorder. J. Child Psychol. Psychiatry 1995, 36, 305–312. [Google Scholar] [CrossRef]
- Barnea, M.; Benaroya-Milshtein, N.; Gilboa-Sechtman, E.; Woods, D.W.; Piacentini, J.; Fennig, S.; Apter, A.; Steinberg, T. Subjective versus objective measures of tic severity in Tourette syndrome—The influence of environment. Psychiatry Res. 2016, 242, 204–209. [Google Scholar] [CrossRef]
- Woods, D.W.; Watson, T.S.; Wolfe, E.; Twohig, M.P.; Friman, P.C. Analyzing the Influence of tic-Related Talk on Vocal and Motor Tics in Children with Tourette’s Syndrome. J. Appl. Behav. Anal. 2001, 34, 353–356. [Google Scholar] [CrossRef]
- Woods, D.W.; Piacentini, J.C.; Scahill, L.; Peterson, A.L.; Wilhelm, S.; Chang, S.; Deckersbach, T.; McGuire, J.; Specht, M.; Conelea, C.A.; et al. Behavior Therapy for Tics in Children: Acute and Long-Term Effects on Psychiatric and Psychosocial Functioning. J. Child Neurol. 2011, 26, 858–865. [Google Scholar] [CrossRef]
- Nissen, J.B.; Kaergaard, M.; Laursen, L.; Parner, E.; Thomsen, P.H. Combined habit reversal training and exposure response prevention in a group setting compared to individual training: A randomized controlled clinical trial. Eur. Child Adolesc. Psychiatry 2019, 28, 57–68. [Google Scholar] [CrossRef]
- Scahill, L.; Leckman, J.F.; Schultz, R.T.; Katsovich, L.; Peterson, B.S. A placebo-controlled trial of risperidone in Tourette syndrome. Neurology 2003, 60, 1130–1135. [Google Scholar] [CrossRef]
- Sallee, F.R.; Kurlan, R.; Goetz, C.G.; Singer, H.; Scahill, L.; Law, G.; Dittman, V.M.; Chappell, P.B. Ziprasidone Treatment of Children and Adolescents with Tourette’s Syndrome: A Pilot Study. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, J.Y.; Lee, J.; Jeong, G.H.; Lee, E.; Lee, S.; Lee, K.H.; Kronbichler, A.; Stubbs, B.; Solmi, M.; et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: An umbrella review. Lancet Psychiatry 2020, 7, 955–970. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.J.M. EEG in the diagnosis, classification, and management of patients with epilepsy. J. Neurol. Neurosurg. Psychiatry 2005, 76, ii2–ii7. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
