Featured Application
Gait smoothness assessment, particularly concerning age-related changes, could offer a valuable clinical tool. The findings indicate the potential utility of gait smoothness estimation in aiding clinicians in identifying and evaluating age-related impairments in gait.
Abstract
The goal of this study is to compare gait smoothness using different metrics. Methodologically, harmonic ratio (HR), spectral arc length (SPARC) and log dimensionless jerk (LDLJ) metrics were applied to acceleration and angular velocity data collected during gait using a wearable inertial sensor placed on the trunk. Sixteen healthy elderly (68.3 ± 4.4 years) and sixteen young (22.6 ± 1.1 years) participants volunteered for the analysis. They were requested to walk at self-selected normal and fast velocities. The results obtained with the three metrics showed variations in smoothness within and between groups. Notably, the older group exhibited contradictory smoothness trends compared to prior studies, presenting a smoother gait than the younger cohort, except for specific directional accelerations. Contradictory outcomes arose between metrics, challenging the influence of age on gait smoothness. Despite concerns about LDLJ’s susceptibility to disturbances, it emerged as the most robust metric. Conversely, HR exhibited alignment with the existing literature on specific acceleration directions. The differences observed in gait smoothness between the two age groups while walking at different speeds suggest that pace might affect smoothness evaluation. The study posits that aging may have a less pronounced impact on gait smoothness compared to cognitive impairment, implying potential clinical utility in discerning age-related gait changes. These findings highlighted the importance of a comprehensive approach to estimating gait smoothness, integrating different metrics and considering several walking speeds, crucial for understanding age-related gait alterations and their clinical implications.
1. Introduction
Human mobility is one of the fundamental skills that impact various aspects of daily life. It affects not only the quality of life but also independence and social engagement. The importance of mobility becomes particularly evident in the context of aging [1]. Among daily motor activities, gait occupies a unique status, being the fundamental and simplest form of human movement, and it is the most widely studied motor task when exploring the impact of cognitive decline [2]. Issues commonly observed in the gait in the elderly, including incorrect posture, altered postural reflexes, muscle function impairments and challenges in neuro-muscular coordination, lead to a disruption in gait smoothness [3]. Movement fluidity encompasses several features related to human movement, resulting from the combination of kinematics, dynamics and neuro-control [4]. Defined by a regular uninterrupted pattern, a ‘smooth’ movement contrasts with an ‘unsmooth’ movement, which exhibits irregularities marked by peaks and results in a less uniform trend characterized by frequent accelerations and decelerations [5]. Metrics to estimate smoothness estimation have been implemented in several fields to objectively evaluate human movement quality. In the medical context, physical impairments have been assessed through smoothness evaluation on people after stroke [6,7,8], Parkinson’s disease individuals [9,10] and cerebellar-ataxia-affected subjects [11]. Furthermore, it has been exploited in the sports field to improve the coordination classification protocol of para-swimmer athletes [12] and, more generally, to assess motor skills in activities of daily living (ADLs) in both open chain [13,14] and closed chain [15].
Smoothness metrics should possess dimensionless attributes, ensuring independence from movement amplitude and duration while demonstrating a consistent response within the physiological range [13]. Several metrics have been proposed to evaluate gait smoothness, including jerk-based measures such as jerk peak inflections [8], jerk root mean square (RMS) [14], log dimensionless jerk (LDLJ) [11,15,16] or the estimation of movement’s frequency spectrum like the harmonic ratio (HR) [2,3,11,17] and spectral arc length (SPARC) [9,10,18,19]. The latter, proposed by Balasubramanian et al. [13], is claimed as reliable, independent from duration and amplitude and not influenced by noise and hence able to outstand other existing metrics that were not robust enough.
Several studies evaluated smoothness in balance, gait and stability, mainly in the clinical context. Blok et al. quantified through the linear jerk root mean square (RMS) metric the smoothness for assessing the trunk balance control in healthy infants [14], while linear jerk inflection counting was implemented by Chandler et al. to determine any differences regarding motion fluidity in sit-to-stand, sit-to-walk and walking in people who had suffered a stroke [8]. Individuals in two different post-stroke phases were also evaluated in terms of body center of mass (CoM) smoothness by comparing LDLJ and SPARC on CoM velocity, finding that LDLJ is more responsive and reliable than SPARC in differentiating gait of both classes [15]. Garcia et al. applied SPARC to the gait velocity patterns in the three directions of post-stroke and control groups, obtaining controversial results [20]. SPARC was utilized also in two studies realized by Figueiredo et al. on trunk accelerations and angular velocities and also by Zucchelli et al. on acceleration RMS to describe walking smoothness exhibited by elderly persons with and without a history of falling, with the aim of investigating a possible fall prevention strategy, since smoothness worsening had been detected [18,19,21]. With regard to aging, the HR metric has been applied to trunk accelerations in three directions to assess gait smoothness, particularly focusing on stability, involving an elderly population with cognitive impairment [2], healthy children and adolescents [17], as well as healthy young and elderly subjects [3]. Although the HR metric has the potential to detect cognitive impairment onset and assess its severity, criticism has emerged regarding its reliability [2].
To quantify smoothness using these metrics, it is necessary to collect gait data. In the clinical field, stereophotogrammetric systems are considered the golden standard for recording gait kinematics of the CoM [8,15]. Over the past decade, however, interest in adopting inertial measurement systems (IMUs) to assess gait kinematics has grown [22,23], and results point to their suitability to assess gait characteristics. For example, a single unit placed on the lumbar zone has been used to investigate gait speed sensitivity [24] and evaluate spatiotemporal parameters and COM kinematics [2]. Several clinical research studies computed, through an IMU positioned on the lumbar zone, SPARC on both linear accelerations and angular velocities across the three directions (anteroposterior, AP; mediolateral, ML; and vertical, V) [9,10,21] or on angular velocities [18,20]. In addition, Pau’s and Leban’s research groups applied HR to linear accelerations in two different populations (elderly and children) to investigate the correlation of smoothness with cognitive impairment in the former case and to characterize gait development during childhood and early adolescence in the latter [2,17]. Beyond clinical contexts, HR was employed on linear acceleration signals gathered via an IMU to investigate its ability to assess smoothness [3,25]. These evaluations encompassed comparing different walking tasks realized by both a cohort of healthy young individuals and a group of healthy aged individuals. Moreover, Brach’s research was conducted with a sample comprising over 70% women, potentially introducing bias into the study.
However, Leban et al. [17] suggested that HR should more properly be used only to quantify gait symmetry because of its lack of consistency in calculating smoothness, in partial agreement with what Pau et al. [2] observed regarding its reliability. Dixon et al. employed the LDLJ and SPARC metrics, to assess both task- and age-related disparities in head and body CoM patterns recorded through an optical system. Their study involved walking and stair ascent and descent in both healthy elderly and young adults [16]. A major limitation of this study is in the process of deriving velocities, accelerations and jerk signals of the CoM by performing up to three subsequent derivatives from the position data acquired using a stereophotogrammetric capture system. This derivative-based procedure can potentially introduce noise, affecting the calculation of smoothness.
In light of the limitations identified in the existing literature concerning the evaluation of smoothness and the exploration of aging effects, this paper aims to apply HR, LDLJ and SPARC metrics to acceleration and angular velocity signals collected during walking by means of an IMU placed on the lumbar region. A comparison is made between a healthy elderly population and a healthy young population. Therefore, the objective is to investigate the metrics’ reliability and robustness, discerning potential differences among them, and establish whether any or all of these metrics can serve as reliable benchmarks in assessing variations in smoothness between younger and elderly individuals during walking.
2. Materials and Methods
2.1. Participants
Regarding the elderly population, gait data collected in a previous study were used. Sixteen healthy elderly subjects (68.3 ± 4.4 years, range 65–79 years) were recruited [26]. Parallel to the previous study, using the same protocol and test conditions, data were also collected from a young population, consisting of 16 subjects (22.6 ± 1.1 years, range 20–24 years). Both groups adhered to two shared inclusion criteria: (i) absence of reported neurological disorders and (ii) no history of musculoskeletal diseases within the past 5 years. In addition to these criteria, the elderly needed to meet two specific requirements: (a) aged over 65 years and (b) absence of prostheses. The gender distribution was balanced within each category, ensuring an equal representation of males and females in both groups. Anthropometric characteristics of both populations are reported in Table 1. Approval from the respective Local Institutional Review Board was obtained for both studies, and all procedures were conducted in accordance with the Helsinki Declaration.

Table 1.
Anthropometric characteristics of young and older people involved in the study.
2.2. Instruments
A single-unit IMU (Xsens, Enschede, The Netherlands) was used. It includes a tri-axial accelerometer (±5 G), a tri-axial gyroscope (±1200 dps) and a tri-axial magnetometer (±75 µT). The manufacturer specifies a noise density of 0.002 m/s2/√Hz for the accelerometer and 0.05 deg/s2/√Hz for the gyroscope [27].
IMU was positioned on the trunk, at T12-L1 vertebral level, and fixed with Xsens elastic bands, emulating the location utilized for gathering gait data in previous work [2,3,16]. The sensor was oriented with the vertical V-axis pointing downward, the mediolateral ML-axis directed to the right side of participants and the anterior-posterior AP-axis pointing in the opposite direction of the gait (Figure 1). Linear accelerations (anteroposterior Acc-AP, mediolateral Acc-ML and vertical Acc-V) and angular velocities (anteroposterior axis Gyr-AP, mediolateral axis Gyr-ML and vertical axis Gyr-V) of the body were measured. The IMU was connected via Bluetooth to the PC through the control system called Xbus Master. Data were acquired through the Xsens proprietary software MT Manager 2018 (Xsens, Enschede, The Netherlands) with a sampling frequency of 50 Hz.
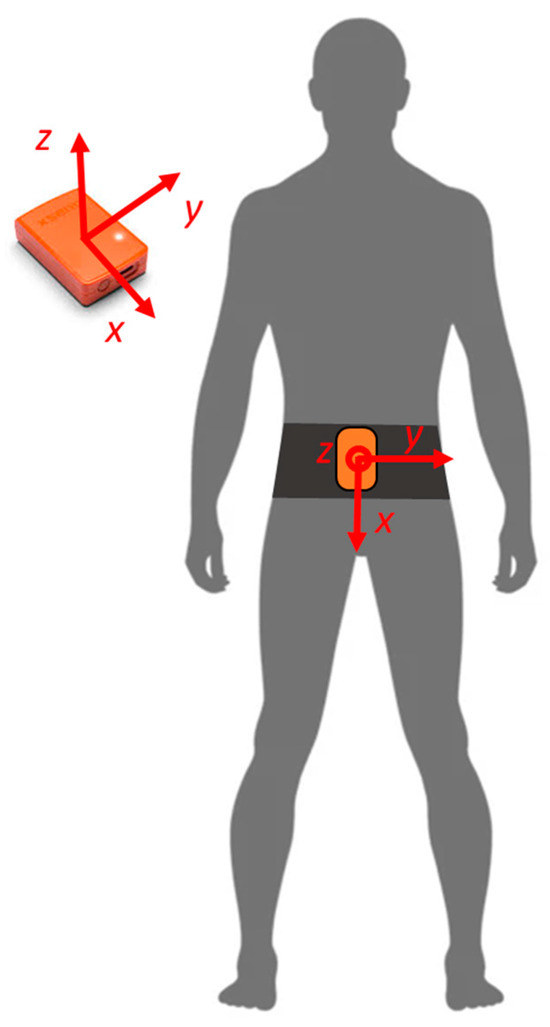
Figure 1.
Position of the IMU on the trunk and IMU reference system.
2.3. Protocol
The experimental test took place indoors, beginning with the marking of a 6 m linear walking path on the floor.
To calibrate the sensor position, participants were instructed to stand still for 10 s before beginning the walking trial. Then, they were asked to walk barefoot along the marked path at two self-selected speeds: normal and fast. Each speed condition involved participants completing 26 back-and-forth transitions along the path to ensure a minimum of 30 valid gait cycles. The order of the speed conditions was randomized for each subject.
2.4. Signal Processing
The IMU-acquired signals were filtered using a low-pass second-order Butterworth filter, with a cut-off frequency of 20 Hz. This choice was determined by the human gait movement frequencies typically ranging from 0.1 to 15 Hz [28] and the 20 Hz theoretical maximum frequency outlined in the formula for SPARC analysis of the FFT spectrum [13]. The root mean square (RMS) values for both acceleration and angular velocity were then computed. Specifically, the analysis focused on the gait phase while excluding the turning phase within each transition. The intervals delineated by the peaks observed in the angular velocity signal along the V direction, indicative of turns made by the subject along the walk, were identified, and all the signals were then segmented according to these markers. Afterward, the peaks in the AP linear acceleration were detected and utilized to segment the signal between two consecutive peaks, delineating it as a step within the gait phase. Gait phases displaying abnormal walking patterns were omitted from the analysis. The minimum number of steps realized considering all the gait phases of each participant was seven. Consequently, the gait segment starting from the first and ending at the eighth step within each gait phase for all individuals was selected for evaluating smoothness. Subsequently, smoothness was assessed by applying SPARC, LDLJ and HR metrics to the chosen gait segment and then averaged for each participant. Statistical analysis was performed to compare data among smoothness assessment between diverse groups and velocity tasks. Customized MATLAB R2023b© routines were developed to execute all signal processing and to perform statistical analysis.
2.5. Smoothness Metrics
The smoothness was evaluated according to the three metrics LDLJ [29], SPARC [13] and HR [30,31,32] on linear accelerations in the three directions (Acc-AP, Acc-ML and Acc-V) and on the angular velocities (Gyr-AP, Gyr-ML and Gyr-V).
HR indices were computed according to the algorithm proposed by Smidt et al. [30], while Balasubramanian procedures were followed to calculate LDLJ and SPARC [29]. Equation (1) outlines the formulation of the LDLJ , utilizing and as the start and end instants of the movement, respectively. Here, denotes the acceleration profile, and corresponds to the maximum acceleration peak between and [29]. Equation (2) defines the calculation of the SPARC index , where represents the fast Fourier transform (FFT) of the temporal signal profile , normalized with respect to its maximum, and is the specified cut-off frequency [13]. Moving to the HR index, the process begins by transforming the signal into the frequency domain using a finite Fourier series. Equation (3) demonstrates the calculation of HR for AP and V directions ( and , respectively) [30]. This involves evaluating the ratio between the sum of amplitudes from the first ten even harmonics (representing in-phase components of the signal) and the sum of amplitudes from the first ten odd harmonics (related to out-of-phase components). Decreased values of the latter indicate improved gait symmetry. Equation (4) details the HR formulation for the mediolateral (ML) direction. By dividing the sum of amplitudes of odd harmonics by the sum of amplitudes of even harmonics, this index captures the dominance of the first harmonic and subsequent odd harmonics, considering the acceleration pattern typically displaying one peak per stride.
The mentioned equations, initially introduced in a theoretical format as in [13,29,30], were modified for practical application with discrete signals during the post-processing stage. Specifically, SPARC metrics involve fast Fourier transform (FFT) calculations, revealing power dispersion around the primary frequency when applied to finite-time sinusoidal signals. To address this, the utilization of the Chebyshev window [33] was introduced. This windowing technique serves to diminish the amplitude and enhance the attenuation rate of secondary lobes within the FFT. The HR metric ranges from 0 to positive infinity, with zero representing complete unsmoothness. Conversely, LDLJ and SPARC metrics generate values within a negative range from negative infinity to −1, where −1 signifies the smoothest movement. In any case, consistently for all the metrics, an increase in the index values indicates an improvement in smoothness.
2.6. Statistical Analysis
The normality of each metric/signal combination was assessed utilizing the Shapiro–Wilk test, revealing non-normal distributions. Consequently, nonparametric tests were employed for further analyses. To evaluate the discriminant validity of the three metrics, comparisons were made between the young and older groups using the Mann–Whitney U test. Additionally, within each group, comparisons between different walking velocities were performed using the Wilcoxon signed rank test. A significance threshold of p-value < 0.05 was applied for all analyses.
3. Results
The average walking velocities observed within the older group displayed minimal variance between self-selected normal walking speed and the instructed faster pace. Specifically, during normal walking, the mean velocity recorded for the older individuals was 0.78 ± 0.10 m/s, whereas the average speed increased marginally to 0.97 ± 0.16 m/s during the faster walking condition. Conversely, among the younger individuals, there was a considerable contrast in velocities between the two gait conditions. The average speed during normal walking registered at 1.41 ± 0.28 m/s, contrasting notably with the faster gait condition where the mean speed increased to 1.96 ± 0.24 m/s. This marked discrepancy underscores the substantial difference in velocities exhibited by the younger cohort between the two walking tasks. The velocities of the two walking tasks for both groups are collected in Table 2.

Table 2.
Averaged gait speed for young and older groups. Values are expressed as mean (standard deviation).
The comparison of smoothness data between young and older subjects at different walking speeds is presented in Table 3, Table 4 and Table 5. Table 3 outlines the smoothness values computed using the LDLJ metric and provides insights into statistical differences. It includes p-values depicting comparisons between young and older individuals (row-wise) as well as between different walking velocities within each group (column-wise) for every analyzed signal. Similarly, Table 4 showcases analogous comparisons concerning the SPARC metric, while Table 5 focuses on the HR metric. These tables offer a comprehensive overview of the significant differences observed across age groups and walking velocities for each smoothness metric.

Table 3.
Smoothness of gait calculated through LDLJ for the two age groups at two different speeds with the respective statistical difference p-values. p-values reported below the group column refer to intra-group comparison, while p-values reported on the right column refer to inter-group comparison. Values are expressed as mean (standard deviation).

Table 4.
Smoothness of gait calculated through SPARC for the two age groups at two different speeds with the respective statistical difference p-values. p-values reported below the group column refer to intra-group comparison, while p-values reported on the right column refer to inter-group comparison. Values are expressed as mean (standard deviation).

Table 5.
Smoothness of gait calculated through HR for the two age groups at two different speeds with the respective statistical difference p-values. p-values reported below the group column refer to intra-group comparison, while p-values reported on the right column refer to inter-group comparison. Values are expressed as mean (standard deviation).
Figure 2 and Figure 3 present bar diagrams illustrating the comparison of smoothness values derived from the application of the LDLJ, SPARC and HR metrics on the acceleration and angular velocity signals, respectively. Each of these bar diagrams corresponds to the smoothness values calculated for the normal gait task, showcasing comparisons between the younger (orange) and elderly (blue) participant groups. In further detail, the four pairs of bars represent the analyzed signals across three directional components (V, ML and AP), along with the corresponding root mean square (RMS) values derived from these signals. Similarly, Figure 4 and Figure 5 provide visual representations of the same comparison but specifically associated with the fast-walking task. These figures delineate the differences in smoothness between the age groups for both gait conditions. Conversely, Figure 6, Figure 7, Figure 8 and Figure 9 detail the variations in smoothness behavior within the same groups of subjects based on the velocities of the walking task. Figure 6 and Figure 8 exhibit smoothness values for accelerations during the normal gait task (depicted in blue) and the fast-walking task (depicted in orange) using the three metrics. In contrast, Figure 7 and Figure 9 represent angular velocities, illustrating the respective smoothness values during the normal and fast-walking tasks for the same age groups. The symbol * above the two compared bars denotes a difference between the compared values.
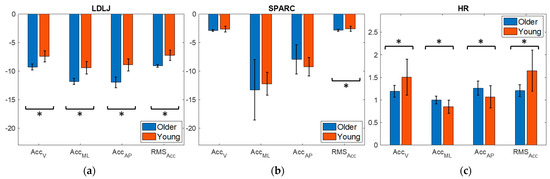
Figure 2.
Smoothness of the acceleration signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and acceleration RMS during the self-selected normal speed gait task. (a) Older vs. young implemented with LDLJ; (b) older vs. young implemented with SPARC; (c) older vs. young implemented with HR. * Specifies statistical difference in the comparison.
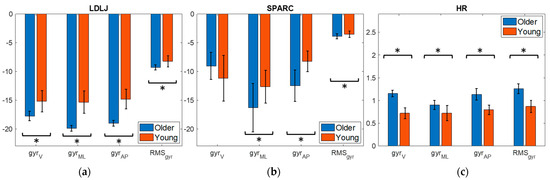
Figure 3.
Smoothness of the angular velocity signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and angular velocity RMS during the self-selected normal speed gait task. (a) Older vs. young implemented with LDLJ; (b) older vs. young implemented with SPARC; (c) older vs. young implemented with HR. * Specifies statistical difference in the comparison.
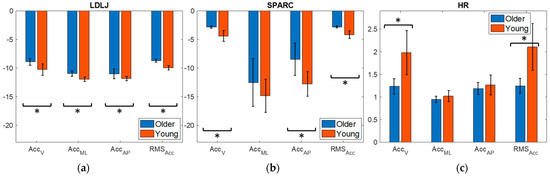
Figure 4.
Smoothness of the acceleration signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and acceleration RMS during the self-selected fast speed gait task. (a) Older vs. young implemented with LDLJ; (b) older vs. young implemented with SPARC; (c) older vs. young implemented with HR. * Specifies statistical difference in the comparison.
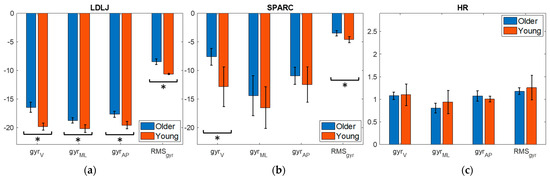
Figure 5.
Smoothness of the angular velocity signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and angular velocity RMS during the self-selected fast speed gait task. (a) Older vs. young implemented with LDLJ; (b) older vs. young implemented with SPARC; (c) older vs. young implemented with HR. * Specifies statistical difference in the comparison.
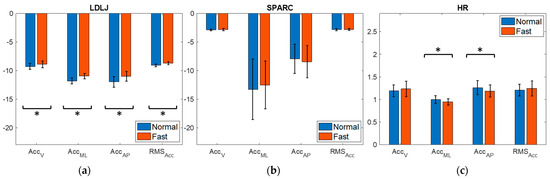
Figure 6.
Smoothness of the acceleration signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and acceleration RMS on the gait task performed by older group. (a) Normal vs. fast task implemented with LDLJ; (b) normal vs. fast task implemented with SPARC; (c) normal vs. fast task implemented with HR. * Specifies statistical difference in the comparison.
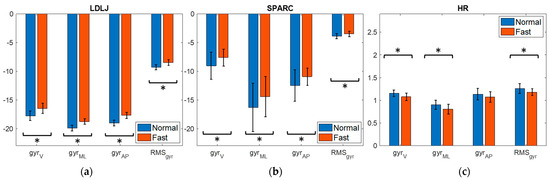
Figure 7.
Smoothness of the angular velocity signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and angular velocity RMS on the gait task performed by older group. (a) Normal vs. fast task implemented with LDLJ; (b) normal vs. fast task implemented with SPARC; (c) normal vs. fast task implemented with HR. * Specifies statistical difference in the comparison.
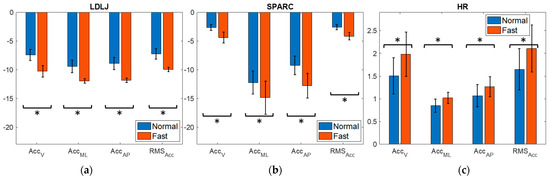
Figure 8.
Smoothness of the acceleration signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and acceleration RMS on the gait task performed by young group. (a) Normal vs. fast task implemented with LDLJ; (b) normal vs. fast task implemented with SPARC; (c) normal vs. fast task implemented with HR. * Specifies statistical difference in the comparison.
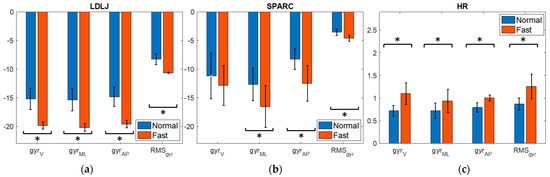
Figure 9.
Smoothness of the angular velocity signals along vertical (V), mediolateral (ML) and anteroposterior (AP) directions and angular velocity RMS on the gait task performed by young group. (a) Normal vs. fast task implemented with LDLJ; (b) normal vs. fast task implemented with SPARC; (c) normal vs. fast task implemented with HR. * Specifies statistical difference in the comparison.
4. Discussion
4.1. Age Group Comparison
The HR metric has been previously utilized in clinical studies to compare smoothness between healthy older adults and those experiencing cognitive decline [2]. Pau et al. observed significant differences in the AP and V directions among tested groups. Individuals with cognitive impairment displayed lower HR values compared to healthy controls, suggesting that notable changes in HR are discernible even in the early stages of cognitive decline. The authors stated that monitoring trunk accelerations may facilitate the early detection of HR changes preceding alterations in walking speed. Brach et al. similarly employed HR to assess smoothness in healthy individuals across two different age groups [3]. Their study revealed that younger individuals walked smoother than older counterparts, showing statistical differences in HR along the AP axis. This finding contradicts Menz et al. [25], where no significant differences were observed. Moreover, the study concluded that age did not differentiate smoothness at varying walking speeds, affirming that younger individuals consistently exhibited smoother gaits than older individuals across all conditions.
This study aimed to replicate Brach et al.’s research and complement Pau et al.’s findings by comparing young and older individuals, regardless of any disorders, to clarify whether aging alone affects smoothness, independent of cognitive impairment. Surprisingly, the results of this work concerning HR metrics during normal gait are characterized by controversial trends. Contrary to previous studies, the older individuals demonstrated smoother gait than the younger group across all signals analyzed, except for acceleration along the V direction and acceleration RMS, which align with prior research findings. According to this, during fast walking, statistical significance was only found in acceleration along the V axis and acceleration RMS, with outcomes in line with the literature. In this scenario, younger individuals exhibited smoother gait compared to older adults, consistent with previous findings. All in all, the HR index did not indicate a direct association suggesting that age affects gait smoothness similar to the onset of cognitive impairment at the moment; however, HR calculated on acceleration along the V direction and acceleration RMS may deserve further investigation.
Additionally, Dixon et al. employed LDLJ and SPARC metrics to assess differences between young and older individuals with good health conditions during gait and stair negotiation, collecting gait signals using a stereophotogrammetric system [16]. No between-group differences were noted for walking or stair ascent. However, the LDLJ metric indicated that the older adult group performed stair descent less smoothly than the young adult group in all directions of acceleration. Our study findings demonstrated that during normal speed gait, LDLJ metrics showed differences in smoothness between older (less smooth) and younger individuals (more smooth) across all investigated signals. Similar outcomes were observed for SPARC but with statistical significance in acceleration RMS and all angular velocity signals, with the exception of the angular velocity along the V direction. Conversely, contrasting results emerged from the comparison between the two groups during fast-paced walking using SPARC and LDLJ metrics with respect to the normal one. LDLJ suggested that older individuals exhibited smoother gaits than the younger group across all variables studied, whereas SPARC confirmed these outcomes, except for ML acceleration and angular velocities along ML and AP directions. The discrepancies observed with these metrics when comparing normal and fast gait between older and younger individuals could be attributed to comparable absolute speeds in both normal and fast walking within the older group, while a substantial difference in speed between the two tasks existed in the younger group. This discrepancy aligns with previous findings indicating that self-selected normal speed gait tends to be the smoothest [31].
Dixon’s findings, however, were derived from signals processed by applying two and three derivatives for SPARC and LDLJ calculations, respectively. This methodology might introduce noise and potentially disrupt the accuracy of smoothness evaluation, possibly contributing to the absence of significant differences observed in walking between the two age groups. Implementing smoothness from acceleration and angular velocity signals directly recorded through IMUs can offer greater accuracy and minimize potential errors in the calculations.
In summary, differences in normal gait were observed specifically in the assessment of smoothness using SPARC on the angular velocity along the AP axis, which stands out as the principal axis of motion. As proposed by Dixon et al. and Brach et al., it is suggested to exclude the assessment of smoothness in the remaining directions of motion, since they did not reveal any statistically significant differences. This suggests that, for smoothness assessment, SPARC applied to AP angular velocity could be employed without necessitating application to all other kinematic features. Additionally, significant differences were found across all estimations made using the LDLJ metric. For this reason, despite concerns regarding susceptibility to disturbances and dependency on duration, LDLJ emerges as the most robust metric for calculating gait smoothness.
4.2. Walking Condition Comparisons
To our knowledge, there is no existing literature that has conducted a comparison of smoothness within the same healthy subject groups concerning normal self-selected speed versus fast self-selected speed. Regarding the older subjects in our study, the analysis revealed that LDLJ metrics indicated a smoother gait during the fast-walking task compared to the normal pace. Notably, these results showed significance in statistical terms across the metrics derived from both accelerations and angular velocities. Conversely, when assessing smoothness using LDLJ in the two distinct gait tasks among the younger group, the findings indicate a smoother gait during the normal walking pace compared to the faster walking task.
Similarly, analogous observations arise from the SPARC smoothness calculations for both the younger and older individuals. However, when considering the older group, it is noteworthy that statistical differences were observed solely in the angular velocities.
In the older group, HR-based smoothness analysis revealed statistical differences exclusively for acceleration along ML and AP directions, as well as for all angular velocity calculations except in the AP direction. Interestingly, contrary to the observations made using SPARC and LDLJ, the analysis indicates that the normal walking task is smoother than the fast-paced task. Conversely, in the analysis of the younger group, HR highlighted that the normal gait is smoother than the faster pace with statistical differences across all examined variables. In both group analyses, HR’s observations stand in stark contrast to SPARC and LDLJ trends.
The divergence in smoothness between normal and fast gaits in young individuals could be attributed to the significant change in absolute speed when transitioning from normal to fast walking. Some previous studies have indicated that self-selected normal walking velocity tends to be the smoothest compared to slower and faster paces [3,31]. In this study, both LDLJ and SPARC metrics corroborated the trends observed in prior research, supporting the notion that normal gait exhibits greater smoothness. However, HR presented an opposing viewpoint, which was the metric adopted in these two studies to calculate smoothness. On the other hand, older individuals maintained a comparable velocity during the fast gait, similar to that of the normal task. Consequently, despite some statistical differences observed, the smoothness variations between the two tasks in older individuals could be deemed negligible.
However, determining a singular methodology as a reliable standard for smoothness estimation remains still inconclusive. Investigation involving different metrics is essential to establish consistency in the obtained results.
It is crucial to acknowledge the limitations inherent in our study. The first limitation relates to the relatively short distance covered in the gait analysis. The brevity of the walking path may have implications for the generalizability of our findings, and future studies should consider longer walking distances. Furthermore, our study lacked a comparison with individuals affected by neurological disorders or cognitive impairments. Including individuals with specific pathologies in future research could provide a more robust framework for assessing age-related changes in gait smoothness. Another interesting future investigation can be the implementation of the TUG test in our methodology. The TUG test could offer valuable insights into dynamic balance and overall gait performance, complementing our current findings.
5. Conclusions
In this study, the aim was to investigate the impact of aging and gait velocity on gait smoothness in healthy young and older individuals, utilizing trunk acceleration and angular velocity data collected through a wearable inertial sensor. The results highlighted discernible alterations in gait smoothness when analyzed using HR, SPARC and LDLJ metrics. However, inconsistencies emerged when considering the effect of gait velocity changes within the same subject group, as the metrics showed discrepancies. In the comparison between age groups, HR and SPARC metrics yielded conflicting outcomes and identified statistical differences in a limited and not repeatable set of signals, while LDLJ emerged as a more promising and robust metric for evaluating smoothness. Nevertheless, further exploration of HR on acceleration along the V axis and acceleration RMS is warranted due to their alignment with the existing literature. These findings suggest that the impact of aging on gait smoothness may not be as pronounced as that of cognitive impairment. Furthermore, the results obtained from this analysis provide valuable data for both the elderly and young populations, serving as a reference for control groups of the two ages in evaluating individuals with pathologies.
Currently, based on these findings, the calculation of smoothness could serve as a partial objective tool to aid clinicians in identifying potential impairments linked to age-related changes in gait smoothness, even if a robust and reliable standard methodology has not been well-established yet.
Author Contributions
Conceptualization M.A., E.C. and L.G.; methodology, M.A., E.C. and L.G.; investigation and data collection, M.A. and E.C.; data post-processing, M.A. and E.C.; writing—original draft preparation, M.A.; writing—review and editing, M.A., E.C. and L.G.; supervision, L.G.; funding acquisition, L.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Harada, C.N.; Love, M.C.N.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Mulas, I.; Putzu, V.; Asoni, G.; Viale, D.; Mameli, I.; Leban, B.; Allali, G. Smoothness of gait in healthy and cognitively impaired individuals: A study on Italian elderly using wearable inertial sensor. Sensors 2020, 20, 3577. [Google Scholar] [CrossRef] [PubMed]
- Brach, J.S.; McGurl, D.; Wert, D.; VanSwearingen, J.M.; Perera, S.; Cham, R.; Studenski, S. Validation of a measure of smoothness of walking. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66A, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Vikne, H.; Bakke, E.S.; Liestøl, K.; Sandbæk, G.; Vøllestad, N. The smoothness of unconstrained head movements is velocity-dependent. Hum. Mov. Sci. 2013, 32, 540–554. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, C.; Qin, G.; Zhigang, D.; O’Malley Marcia, K. Intermittency of Slow Arm Movements Increases in Distal Direction. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 10–15 October 2009; IEEE: Piscataway, NJ, USA, 2009. [Google Scholar]
- Rohrer, B.; Fasoli, S.; Krebs, H.I.; Hughes, R.; Volpe, B.; Frontera, W.R.; Stein, J.; Hogan, N. Movement Smoothness Changes during Stroke Recovery. J. Neurosci. 2002, 22, 8297–8304. [Google Scholar] [CrossRef] [PubMed]
- Van Kordelaar, J.; Van Wegen, E.; Kwakkel, G. Impact of time on quality of motor control of the paretic upper limb after stroke. Arch. Phys. Med. Rehabil. 2014, 95, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Chandler, E.A.; Stone, T.; Pomeroy, V.M.; Clark, A.B.; Kerr, A.; Rowe, P.; Ugbolue, U.C.; Smith, J.; Hancock, N.J. Investigating the Relationships Between Three Important Functional Tasks Early After Stroke: Movement Characteristics of Sit-To-Stand, Sit-To-Walk, and Walking. Front. Neurol. 2021, 12, 660383. [Google Scholar] [CrossRef] [PubMed]
- Beck, Y.; Herman, T.; Brozgol, M.; Giladi, N.; Mirelman, A.; Hausdorff, J.M. SPARC: A new approach to quantifying gait smoothness in patients with Parkinson’s disease. J. Neuroeng. Rehabil. 2018, 15, 49. [Google Scholar] [CrossRef]
- Pinto, C.; Schuch, C.P.; Balbinot, G.; Salazar, A.P.; Hennig, E.M.; Kleiner, A.F.R.; Pagnussat, A.S. Movement smoothness during a functional mobility task in subjects with Parkinson’s disease and freezing of gait-An analysis using inertial measurement units. J. Neuroeng. Rehabil. 2019, 16, 110. [Google Scholar] [CrossRef]
- Castiglia, S.F.; Trabassi, D.; Tatarelli, A.; Ranavolo, A.; Varrecchia, T.; Fiori, L.; Di Lenola, D.; Cioffi, E.; Raju, M.; Coppola, G.; et al. Identification of Gait Unbalance and Fallers Among Subjects with Cerebellar Ataxia by a Set of Trunk Acceleration-Derived Indices of Gait. Cerebellum 2023, 22, 46–58. [Google Scholar] [CrossRef]
- Maia, A.C.; Hogarth, L.; Burkett, B.; Payton, C. Improving the objectivity of the current World Para Swimming motor coordination test for swimmers with hypertonia, ataxia and athetosis using measures of movement smoothness, rhythm and accuracy. J. Sports Sci. 2021, 39, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, S.; Melendez-Calderon, A.; Burdet, E. A robust and sensitive metric for quantifying movement smoothness. IEEE Trans. Biomed. Eng. 2012, 59, 2126–2136. [Google Scholar] [CrossRef] [PubMed]
- Blok, J.; Poggensee, K.L.; Lemus, D.; Kok, M.; Pangalila, R.F.; Vallery, H.; Deferme, J.; Toussaint-Duyster, L.C.; Horemans, H. Quantification of the development of trunk control in healthy infants using inertial measurement units. In Proceedings of the 2022 International Conference on Rehabilitation Robotics (ICORR), Rotterdam, The Netherlands, 25–29 July 2022. [Google Scholar]
- Germanotta, M.; Iacovelli, C.; Aprile, I. Evaluation of Gait Smoothness in Patients with Stroke Undergoing Rehabilitation: Comparison between Two Metrics. Int. J. Environ. Res. Public Health 2022, 19, 13440. [Google Scholar] [CrossRef] [PubMed]
- Dixon, P.C.; Stirling, L.; Xu, X.; Chang, C.C.; Dennerlein, J.T.; Schiffman, J.M. Aging may negatively impact movement smoothness during stair negotiation. Hum. Mov. Sci. 2018, 60, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Leban, B.; Cimolin, V.; Porta, M.; Arippa, F.; Pilloni, G.; Galli, M.; Pau, M. Age-Related Changes in Smoothness of Gait of Healthy Children and Early Adolescents. J. Mot. Behav. 2020, 52, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, A.I.; Balbinot, G.; Brauner, F.O.; Schiavo, A.; de Souza Urbanetto, M.; Mestriner, R.G. History of falls alters movement smoothness and time taken to complete a functional mobility task in the oldest-old: A case-control study. Exp. Gerontol. 2022, 167, 111918. [Google Scholar] [CrossRef]
- Zucchelli, A.; Lucente, D.; Filippini, C.; Marengoni, A.; Lopomo, N.F. Instrumental evaluation of gait smoothness and history of falling in older persons: Results from an exploratory case–control study. Aging Clin. Exp. Res. 2023, 35, 1357–1361. [Google Scholar] [CrossRef]
- do Vale Garcia, F.; da Cunha, M.J.; Schuch, C.P.; Schifino, G.P.; Balbinot, G.; Pagnussat, A.S. Movement smoothness in chronic post-stroke individuals walking in an outdoor environment-A cross-sectional study using IMU sensors. PLoS ONE 2021, 16, e0250100. [Google Scholar] [CrossRef]
- Figueiredo, A.I.; Balbinot, G.; Brauner, F.O.; Schiavo, A.; Baptista, R.R.; Pagnussat, A.S.; Hollands, K.; Mestriner, R.G. SPARC Metrics Provide Mobility Smoothness Assessment in Oldest-Old With and Without a History of Falls: A Case Control Study. Front. Physiol. 2020, 11, 540. [Google Scholar] [CrossRef]
- Digo, E.; Agostini, V.; Pastorelli, S.; Gastaldi, L.; Panero, E. Gait phases detection in elderly using Trunk-MIMU system. In Proceedings of the BIODEVICES 2021-14th International Conference on Biomedical Electronics and Devices; Part of the 14th International Joint Conference on Biomedical Engineering Systems and Technologies, BIOSTEC 2021, Vienna, Austria, 11–13 February 2021; SciTePress: Setúbal, Portugal, 2021; pp. 58–65. [Google Scholar] [CrossRef]
- Digo, E.; Pierro, G.; Pastorelli, S.; Gastaldi, L. Tilt-Twist Method Using Inertial Sensors to Assess Spinal Posture During Gait. In Advances in Intelligent Systems and Computing; Springer: Berlin/Heidelberg, Germany, 2020; pp. 384–392. [Google Scholar] [CrossRef]
- Czech, M.D.; Psaltos, D.; Zhang, H.; Adamusiak, T.; Calicchio, M.; Kelekar, A.; Messere, A.; Van Dijk, K.R.A.; Ramos, V.; Demanuele, C.; et al. Age and environment-related differences in gait in healthy adults using wearables. NPJ Digit. Med. 2020, 3, 127. [Google Scholar] [CrossRef]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Age-related differences in walking stability. Age Ageing 2003, 32, 137–142. Available online: https://academic.oup.com/ageing/article/32/2/137/28914 (accessed on 15 December 2023). [CrossRef] [PubMed]
- Digo, E.; Panero, E.; Agostini, V.; Gastaldi, L. Comparison of IMU set-ups for the estimation of gait spatio-temporal parameters in an elderly population. Proc. Inst. Mech. Eng. H 2023, 237, 61–73. [Google Scholar] [CrossRef] [PubMed]
- “Xsens Website.”. Available online: https://www.movella.com/products/xsens (accessed on 5 January 2024).
- Khusainov, R.; Azzi, D.; Achumba, I.E.; Bersch, S.D. Real-time human ambulation, activity, and physiological monitoring: Taxonomy of issues, techniques, applications, challenges and limitations. Sensors 2013, 13, 12852–12902. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, S.; Melendez-Calderon, A.; Roby-Brami, A.; Burdet, E. On the analysis of movement smoothness. J. Neuroeng. Rehabil. 2015, 12, 112. [Google Scholar] [CrossRef]
- Smidt, G.; Arora, J.S. Accelerographic Analysis of Several Types of Walking. 1972. Available online: https://www.researchgate.net/publication/18026492 (accessed on 14 December 2023).
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Acceleration Patterns of the Head and Pelvis When Walking on Level and Irregular Surfaces. Gait Posture 2003, 18, 35–46. [Google Scholar] [CrossRef]
- Panero, E.; Digo, E.; Dimanico, U.; Artusi, C.A.; Zibetti, M.; Gastaldi, L. Effect of deep brain stimulation frequency on gait symmetry, smoothness and variability using IMU. In Proceedings of the 2021 IEEE International Symposium on Medical Measurements and Applications, MeMeA 2021-Conference Proceedings, Lausanne, Switzerland, 23–25 June 2021; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2021. [Google Scholar] [CrossRef]
- Dolph, C.L. A Current Distribution for Broadside Arrays Which Optimizes the Relationship between Beam Width and Side-Lobe Level. Proc. IRE 1946, 34, 335–348. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).