The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Details about the GMB Process
3. Results
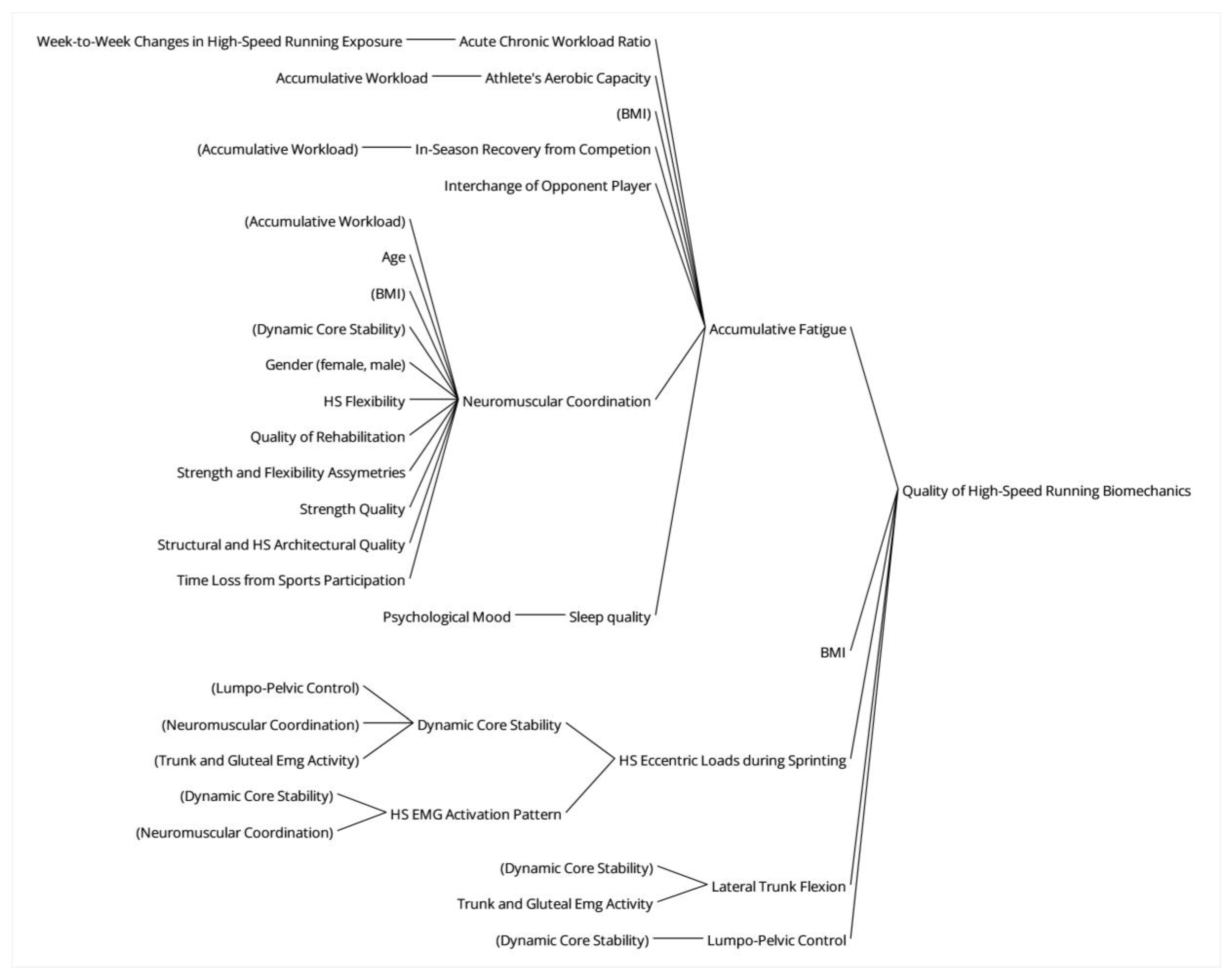
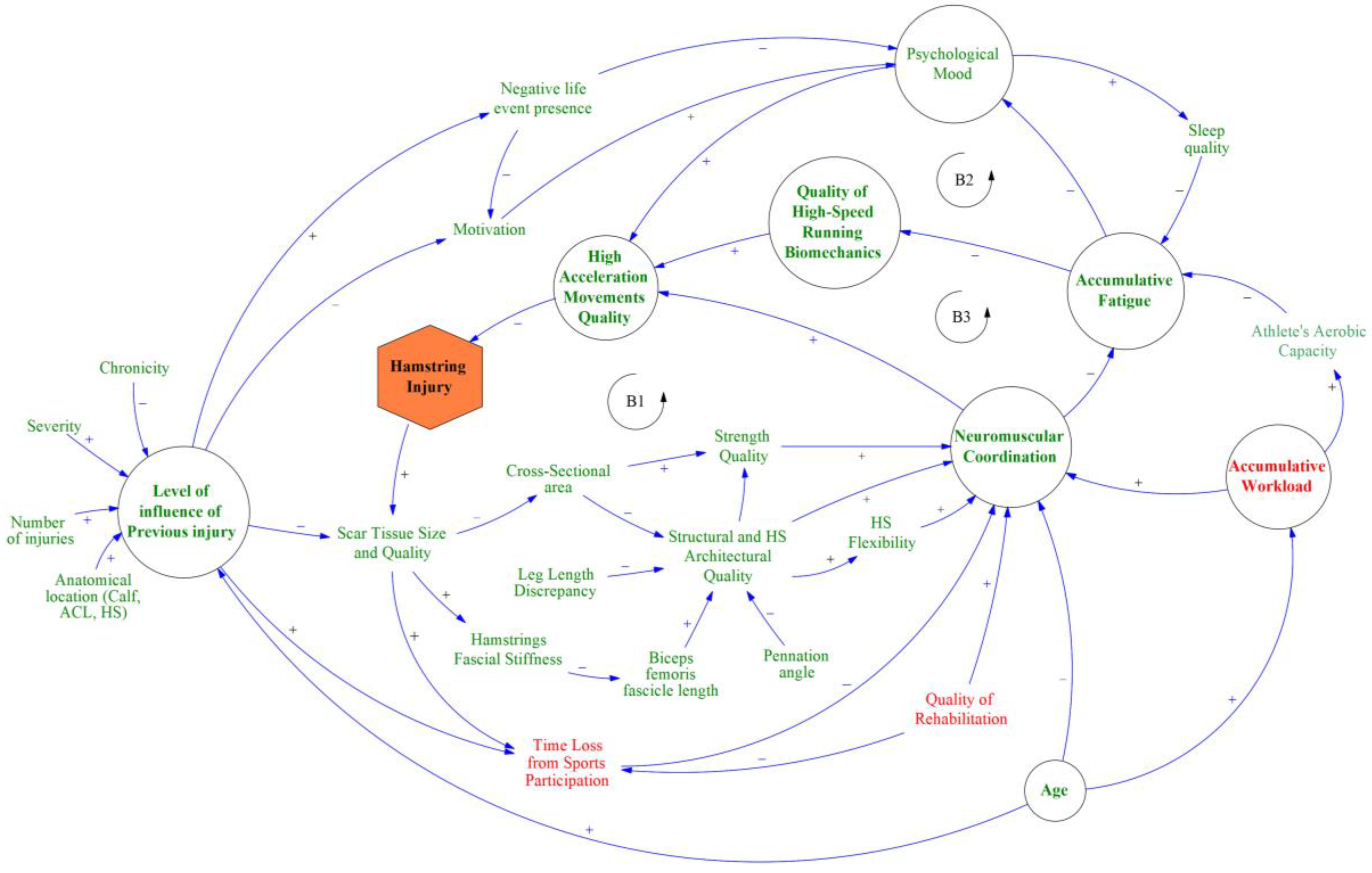
3.1. Impact of Neuromuscular Coordination on the Quality of High-Speed Running Biomechanics and High-Accelerated Movements Quality That Affect Risk for HI
3.2. Interaction of Previous Injury Characteristics, Age, and Psychological Mood with the Athlete’s Neuromuscular Coordination That Affect Risk for HI
3.3. Effect of Workload and Fatigue on Neuromuscular Coordination and High Accelerated Movements That Affect Risk for HI
3.4. Effect of Local and National Policies and Team Staff’s Cooperation in the Total Strategies for Injury Management and Prevention That Affect Risk for HI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maniar, N.; Carmichael, D.S.; Hickey, J.T.; Timmins, R.G.; Jose, A.J.S.; Dickson, J.; Opar, D. Incidence and Prevalence of Hamstring Injuries in Field-Based Team Sports: A Systematic Review and Meta-Analysis of 5952 Injuries from over 7 Million Exposure Hours. Br. J. Sports Med. 2023, 57, 109–116. [Google Scholar] [CrossRef]
- Hägglund, M.; Waldén, M.; Magnusson, H.; Kristenson, K.; Bengtsson, H.; Ekstrand, J. Injuries Affect Team Performance Negatively in Professional Football: An 11-Year Follow-up of the UEFA Champions League Injury Study. Br. J. Sports Med. 2013, 47, 738–742. [Google Scholar] [CrossRef]
- Hickey, J.; Shield, A.J.; Williams, M.D.; Opar, D.A. The Financial Cost of Hamstring Strain Injuries in the Australian Football League. Br. J. Sports Med. 2014, 48, 729–730. [Google Scholar] [CrossRef]
- Ekstrand, J.; Bengtsson, H.; Waldén, M.; Davison, M.; Khan, K.M.; Hägglund, M. Hamstring Injury Rates Have Increased during Recent Seasons and Now Constitute 24% of All Injuries in Men’s Professional Football: The UEFA Elite Club Injury Study from 2001/02 to 2021/22. Br. J. Sports Med. 2023, 57, 292–298. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; van Dyk, N.; Pizzari, T. Recalibrating the Risk of Hamstring Strain Injury (HSI): A 2020 Systematic Review and Meta-Analysis of Risk Factors for Index and Recurrent Hamstring Strain Injury in Sport. Br. J. Sports Med. 2020, 54, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Carling, C.; McCall, A.; Le Gall, F.; Dupont, G. The Impact of Short Periods of Match Congestion on Injury Risk and Patterns in an Elite Football Club. Br. J. Sports Med. 2016, 50, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Ruddy, J.D.; Pietsch, S.; Maniar, N.; Cormack, S.J.; Timmins, R.G.; Williams, M.D.; Carey, D.L.; Opar, D.A. Session Availability as a Result of Prior Injury Impacts the Risk of Subsequent Non-Contact Lower Limb Injury in Elite Male Australian Footballers. Front. Physiol. 2019, 10, 737. [Google Scholar] [CrossRef] [PubMed]
- Schuermans, J.; Van Tiggelen, D.; Palmans, T.; Danneels, L.; Witvrouw, E. Deviating Running Kinematics and Hamstring Injury Susceptibility in Male Soccer Players: Cause or Consequence? Gait Posture 2017, 57, 270–277. [Google Scholar] [CrossRef]
- Schuermans, J.; Danneels, L.; Van Tiggelen, D.; Palmans, T.; Witvrouw, E. Proximal Neuromuscular Control Protects Against Hamstring Injuries in Male Soccer Players: A Prospective Study with Electromyography Time-Series Analysis during Maximal Sprinting. Am. J. Sports Med. 2017, 45, 1315–1325. [Google Scholar] [CrossRef]
- Kenneally-Dabrowski, C.; Brown, N.A.T.; Warmenhoven, J.; Serpell, B.G.; Perriman, D.; Lai, A.K.M.; Spratford, W. Late Swing Running Mechanics Influence Hamstring Injury Susceptibility in Elite Rugby Athletes: A Prospective Exploratory Analysis. J. Biomech. 2019, 92, 112–119. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Alentorn-Geli, E.; Brughelli, M. Hamstring Strain Injuries: Are We Heading in the Right Direction? Br. J. Sports Med. 2012, 46, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Freckleton, G.; Pizzari, T. Risk Factors for Hamstring Muscle Strain Injury in Sport: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2013, 47, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Fousekis, K.; Tsepis, E.; Poulmedis, P.; Athanasopoulos, S.; Vagenas, G. Intrinsic Risk Factors of Non-Contact Quadriceps and Hamstring Strains in Soccer: A Prospective Study of 100 Professional Players. Br. J. Sports Med. 2011, 45, 709–714. [Google Scholar] [CrossRef] [PubMed]
- van Dyk, N.; Bahr, R.; Whiteley, R.; Tol, J.L.; Kumar, B.D.; Hamilton, B.; Farooq, A.; Witvrouw, E. Hamstring and Quadriceps Isokinetic Strength Deficits Are Weak Risk Factors for Hamstring Strain Injuries: A 4-Year Cohort Study. Am. J. Sports Med. 2016, 44, 1789–1795. [Google Scholar] [CrossRef] [PubMed]
- van Dyk, N.; Farooq, A.; Bahr, R.; Witvrouw, E. Hamstring and Ankle Flexibility Deficits Are Weak Risk Factors for Hamstring Injury in Professional Soccer Players: A Prospective Cohort Study of 438 Players Including 78 Injuries. Am. J. Sports Med. 2018, 46, 2203–2210. [Google Scholar] [CrossRef] [PubMed]
- Bowen, L.; Gross, A.S.; Gimpel, M.; Bruce-Low, S.; Li, F.-X. Spikes in Acute:Chronic Workload Ratio (ACWR) Associated with a 5–7 Times Greater Injury Rate in English Premier League Football Players: A Comprehensive 3-Year Study. Br. J. Sports Med. 2020, 54, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Ruddy, J.D.; Pollard, C.W.; Timmins, R.G.; Williams, M.D.; Shield, A.J.; Opar, D.A. Running Exposure Is Associated with the Risk of Hamstring Strain Injury in Elite Australian Footballers. Br. J. Sports Med. 2018, 52, 919–928. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, J.; Ueblacker, P.; Van Zoest, W.; Verheijen, R.; Vanhecke, B.; Van Wijk, M.; Bengtsson, H. Risk Factors for Hamstring Muscle Injury in Male Elite Football: Medical Expert Experience and Conclusions from 15 European Champions League Clubs. BMJ Open Sport Exerc. Med. 2023, 9, e001461. [Google Scholar] [CrossRef]
- Shalaj, I.; Gjaka, M.; Bachl, N.; Wessner, B.; Tschan, H.; Tishukaj, F. Potential Prognostic Factors for Hamstring Muscle Injury in Elite Male Soccer Players: A Prospective Study. PLoS ONE 2020, 15, e0241127. [Google Scholar] [CrossRef]
- Bolling, C.; van Mechelen, W.; Pasman, H.R.; Verhagen, E. Context Matters: Revisiting the First Step of the ‘Sequence of Prevention’ of Sports Injuries. Sports Med. 2018, 48, 2227–2234. [Google Scholar] [CrossRef]
- Ayala, F.; López-Valenciano, A.; Gámez Martín, J.A.; De Ste Croix, M.; Vera-Garcia, F.J.; García-Vaquero, M.D.P.; Ruiz-Pérez, I.; Myer, G.D. A Preventive Model for Hamstring Injuries in Professional Soccer: Learning Algorithms. Int. J. Sports Med. 2019, 40, 344–353. [Google Scholar] [CrossRef] [PubMed]
- López-Valenciano, A.; Ayala, F.; Puerta, J.M.; De Ste Croix, M.B.A.; Vera-Garcia, F.J.; Hernandez-Sanchez, S.; Ruiz-Perez, I.; Myer, G.D. A Preventive Model for Muscle Injuries: A Novel Approach Based on Learning Algorithms. Med. Sci. Sports Exerc. 2018, 50, 915–927. [Google Scholar] [CrossRef] [PubMed]
- Ruddy, J.D.; Shield, A.J.; Maniar, N.; Williams, M.D.; Duhig, S.; Timmins, R.G.; Hickey, J.; Bourne, M.N.; Opar, D.A. Predictive Modeling of Hamstring Strain Injuries in Elite Australian Footballers. Med. Sci. Sports Exerc. 2018, 50, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, R.O.; Bertelsen, M.L.; Ramskov, D.; Møller, M.; Hulme, A.; Theisen, D.; Finch, C.F.; Fortington, L.V.; Mansournia, M.A.; Parner, E.T. Time-to-Event Analysis for Sports Injury Research Part 2: Time-Varying Outcomes. Br. J. Sports Med. 2019, 53, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Liveris, N.I.; Papageorgiou, G.; Tsepis, E.; Fousekis, K.; Tsarbou, C.; Xergia, S.A. Towards the Development of a System Dynamics Model for the Prediction of Lower Extremity Injuries. Int. J. Exerc. Sci. 2023, 16, 1052–1065. [Google Scholar] [PubMed]
- Hulme, A.; McLean, S.; Salmon, P.M.; Thompson, J.; Lane, B.R.; Nielsen, R.O. Computational Methods to Model Complex Systems in Sports Injury Research: Agent-Based Modelling (ABM) and Systems Dynamics (SD) Modelling. Br. J. Sports Med. 2019, 53, 1507–1510. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.; Kerhervé, H.A.; Stevens, N.; Salmon, P.M. A Systems Analysis Critique of Sport-Science Research. Int. J. Sports Physiol. Perform. 2021, 16, 1385–1392. [Google Scholar] [CrossRef] [PubMed]
- Kenzie, E.S.; Parks, E.L.; Bigler, E.D.; Wright, D.W.; Lim, M.M.; Chesnutt, J.C.; Hawryluk, G.W.J.; Gordon, W.; Wakeland, W. The Dynamics of Concussion: Mapping Pathophysiology, Persistence, and Recovery with Causal-Loop Diagramming. Front. Neurol. 2018, 9, 203. [Google Scholar] [CrossRef]
- Allender, S.; Owen, B.; Kuhlberg, J.; Lowe, J.; Nagorcka-Smith, P.; Whelan, J.; Bell, C. A Community Based Systems Diagram of Obesity Causes. PLoS ONE 2015, 10, e0129683. [Google Scholar] [CrossRef]
- Fonseca, S.T.; Souza, T.R.; Verhagen, E.; van Emmerik, R.; Bittencourt, N.F.N.; Mendonça, L.D.M.; Andrade, A.G.P.; Resende, R.A.; Ocarino, J.M. Sports Injury Forecasting and Complexity: A Synergetic Approach. Sports Med. 2020, 50, 1757–1770. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex Systems Approach for Sports Injuries: Moving from Risk Factor Identification to Injury Pattern Recognition—Narrative Review and New Concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- van Beijsterveldt, A.M.C.; van de Port, I.G.L.; Vereijken, A.J.; Backx, F.J.G. Risk Factors for Hamstring Injuries in Male Soccer Players: A Systematic Review of Prospective Studies. Scand. J. Med. Sci. Sports 2013, 23, 253–262. [Google Scholar] [CrossRef] [PubMed]
- De Visser, H.M.; Reijman, M.; Heijboer, M.P.; Bos, P.K. Risk Factors of Recurrent Hamstring Injuries: A Systematic Review. Br. J. Sports Med. 2012, 46, 124–130. [Google Scholar] [CrossRef]
- Green, B.; Bourne, M.N.; Pizzari, T. Isokinetic Strength Assessment Offers Limited Predictive Validity for Detecting Risk of Future Hamstring Strain in Sport: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2018, 52, 329–336. [Google Scholar] [CrossRef] [PubMed]
- Van Heumen, M.; Tol, J.L.; De Vos, R.J.; Moen, M.H.; Weir, A.; Orchard, J.; Reurink, G. The Prognostic Value of MRI in Determining Reinjury Risk Following Acute Hamstring Injury: A Systematic Review. Br. J. Sports Med. 2017, 51, 1355–1363. [Google Scholar] [CrossRef] [PubMed]
- Chavarro-Nieto, C.; Beaven, M.; Gill, N.; Hébert-Losier, K. Hamstrings Injury Incidence, Risk Factors, and Prevention in Rugby Union Players: A Systematic Review. Phys. Sportsmed. 2023, 51, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Hovmand, P.S.; Andersen, D.F.; Rouwette, E.; Richardson, G.P.; Rux, K.; Calhoun, A. Group Model-Building ‘Scripts’ as a Collaborative Planning Tool. Syst. Res. Behav. Sci. 2012, 29, 179–193. [Google Scholar] [CrossRef]
- Bérard, C. Group Model Building Using System Dynamics: An Analysis of Methodological Frameworks. Electron. J. Bus. Res. Methods 2010, 8, 35–46. [Google Scholar]
- Hovmand, P.; Rouwette, E.; Andersen, D.; Richardson, G.; Calhoun, A.; Rux, K.; Hower, T. Scriptapedia: A Handbook of Scripts for Developing Structured Group Model Building Sessions. In Proceedings of the 29th International Conference of the System Dynamics Society 2011, Washington, DC, USA, 24–28 July 2011; pp. 1476–1491. [Google Scholar]
- Hovmand, P.S.; Rouwette, E.; Andersen, D.F.; Richardson, G.P. Scriptapedia. Available online: https://en.wikibooks.org/wiki/Scriptapedia (accessed on 25 December 2021).
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Ekstrand, J.; Lundqvist, D.; Davison, M.; D’Hooghe, M.; Pensgaard, A.M. Communication Quality between the Medical Team and the Head Coach/Manager Is Associated with Injury Burden and Player Availability in Elite Football Clubs. Br. J. Sports Med. 2019, 53, 304–308. [Google Scholar] [CrossRef] [PubMed]
- De Vos, R.J.; Reurink, G.; Goudswaard, G.J.; Moen, M.H.; Weir, A.; Tol, J.L. Clinical Findings Just after Return to Play Predict Hamstring Re-Injury, but Baseline MRI Findings Do Not. Br. J. Sports Med. 2014, 48, 1377–1384. [Google Scholar] [CrossRef]
- Järvinen, T.A.H.; Järvinen, M.; Kalimo, H. Regeneration of Injured Skeletal Muscle after the Injury. Muscles Ligaments Tendons J. 2013, 3, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Silder, A.; Heiderscheit, B.C.; Thelen, D.G.; Enright, T.; Tuite, M.J. MR Observations of Long-Term Musculotendon Remodeling Following a Hamstring Strain Injury. Skelet. Radiol. 2008, 37, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, E.; De Ruiter, C.J.; Bastiaansen, B.J.C.; Goedhart, E.A.; Brink, M.S.; Van Der Helm, F.C.T.; Savelsbergh, G.J.P. Associations between Hamstring Fatigue and Sprint Kinematics during a Simulated Football (Soccer) Match. Med. Sci. Sports Exerc. 2021, 53, 2586–2595. [Google Scholar] [CrossRef] [PubMed]
- Goossens, L.; Witvrouw, E.; Vanden Bossche, L.; De Clercq, D. Lower Eccentric Hamstring Strength and Single Leg Hop for Distance Predict Hamstring Injury in PETE Students. Eur. J. Sport Sci. 2015, 15, 436–442. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short Biceps Femoris Fascicles and Eccentric Knee Flexor Weakness Increase the Risk of Hamstring Injury in Elite Football (Soccer): A Prospective Cohort Study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef] [PubMed]
- Duhig, S.; Shield, A.J.; Opar, D.; Gabbett, T.J.; Ferguson, C.; Williams, M. Effect of High-Speed Running on Hamstring Strain Injury Risk. Br. J. Sports Med. 2016, 50, 1536–1540. [Google Scholar] [CrossRef]
- Windt, J.; Gabbett, T.J. How Do Training and Competition Workloads Relate to Injury? The Workload—Injury Aetiology Model. Br. J. Sports Med. 2017, 51, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Gabbett, T.J. The Training-Injury Prevention Paradox: Should Athletes Be Training Smarter and Harder? Br. J. Sports Med. 2016, 50, 273–280. [Google Scholar] [CrossRef]
- Andrade, R.; Wik, E.H.; Rebelo-Marques, A.; Blanch, P.; Whiteley, R.; Espregueira-Mendes, J.; Gabbett, T.J. Is the Acute: Chronic Workload Ratio (ACWR) Associated with Risk of Time-Loss Injury in Professional Team Sports? A Systematic Review of Methodology, Variables and Injury Risk in Practical Situations. Sports Med. 2020, 50, 1613–1635. [Google Scholar] [CrossRef]
- Malone, S.; Roe, M.; Doran, D.A.; Gabbett, T.J.; Collins, K.D. Protection against Spikes in Workload with Aerobic Fitness and Playing Experience: The Role of the Acute: Chronic Workload Ratio on Injury Risk in Elite Gaelic Football. Int. J. Sports Physiol. Perform. 2017, 12, 393–401. [Google Scholar] [CrossRef]
- Gronwald, T.; Klein, C.; Hoenig, T.; Pietzonka, M.; Bloch, H.; Edouard, P.; Hollander, K. Hamstring Injury Patterns in Professional Male Football (Soccer): A Systematic Video Analysis of 52 Cases. Br. J. Sports Med. 2022, 56, 165–171. [Google Scholar] [CrossRef] [PubMed]
- McCall, A.; Carling, C.; Davison, M.; Nedelec, M.; Le Gall, F.; Berthoin, S.; Dupont, G. Injury Risk Factors, Screening Tests and Preventative Strategies: A Systematic Review of the Evidence That Underpins the Perceptions and Practices of 44 Football (Soccer) Teams from Various Premier Leagues. Br. J. Sports Med. 2015, 49, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Bahr, R.; Thorborg, K.; Ekstrand, J. Evidence-Based Hamstring Injury Prevention Is Not Adopted by the Majority of Champions League or Norwegian Premier League Football Teams: The Nordic Hamstring Survey. Br. J. Sports Med. 2015, 49, 1466–1471. [Google Scholar] [CrossRef]
- Freckleton, G.; Cook, J.; Pizzari, T. The Predictive Validity of a Single Leg Bridge Test for Hamstring Injuries in Australian Rules Football Players. Br. J. Sports Med. 2014, 48, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Schuermans, J.; Van Tiggelen, D.; Witvrouw, E. Prone Hip Extension Muscle Recruitment Is Associated with Hamstring Injury Risk in Amateur Soccer. Int. J. Sports Med. 2017, 38, 696–706. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schuermans, J.; Van Tiggelen, D.; Danneels, L.; Witvrouw, E. Susceptibility to Hamstring Injuries in Soccer: A Prospective Study Using Muscle Functional Magnetic Resonance Imaging. Am. J. Sports Med. 2016, 44, 1276–1285. [Google Scholar] [CrossRef]
- Eliakim, E.; Morgulev, E.; Lidor, R.; Meckel, Y. Estimation of Injury Costs: Financial Damage of English Premier League Teams’ Underachievement Due to Injuries. BMJ Open Sport Exerc. Med. 2020, 6, e000675. [Google Scholar] [CrossRef] [PubMed]
- Ekstrand, J.; Van Zoest, W.; Gauffin, H. Changes in Head Staff Members in Male Elite-Level Football Teams Are Associated with Increased Hamstring Injury Burden for That Season: The UEFA Elite Club Injury Study. BMJ Open Sport Exerc. Med. 2023, 9, 1640. [Google Scholar] [CrossRef]
- Ivarsson, A.; Johnson, U.; Andersen, M.B.; Tranaeus, U.; Stenling, A.; Lindwall, M. Psychosocial Factors and Sport Injuries: Meta-Analyses for Prediction and Prevention. Sports Med. 2017, 47, 353–365. [Google Scholar] [CrossRef]
- Kiliç, Ö.; Aoki, H.; Goedhart, E.; Hägglund, M.; Kerkhoffs, G.M.M.J.; Kuijer, P.P.F.M.; Waldén, M.; Gouttebarge, V. Severe Musculoskeletal Time-Loss Injuries and Symptoms of Common Mental Disorders in Professional Soccer: A Longitudinal Analysis of 12-Month Follow-up Data. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 946–954. [Google Scholar] [CrossRef]
- Kawai, T.; Takamoto, K.; Bito, I. Previous Hamstring Muscle Strain Injury Alters Passive Tissue Stiffness and Vibration Sense. J. Bodyw. Mov. Ther. 2021, 27, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Watsford, M.L.M.L.; Murphy, A.J.A.J.; McLachlan, K.A.K.A.; Bryant, A.L.A.L.; Cameron, M.L.M.L.; Crossley, K.M.K.M.; Makdissi, M. A Prospective Study of the Relationship between Lower Body Stiffness and Hamstring Injury in Professional Australian Rules Footballers. Am. J. Sports Med. 2010, 38, 2058–2064. [Google Scholar] [CrossRef] [PubMed]
- Nuñez, F.J.; Ritzmann, R.; Hernandez-Abad, F.; Martinez, J.C.; Suarez-Arrones, L. Muscle Architecture, Morphology, and Mechanical and Functional Properties of Biceps Femoris Long Head in Professional Soccer Players with a Prior Healed Injured Hamstring. J. Clin. Med. 2022, 11, 7222. [Google Scholar] [CrossRef] [PubMed]
- Ivarsson, A.; Johnson, U.; Podlog, L. Psychological Predictors of Injury Occurrence: A Prospective Investigation of Professional Swedish Soccer Players. J. Sport Rehabil. 2013, 22, 19–26. [Google Scholar] [CrossRef]
- Diemer, W.M.; Winters, M.; Tol, J.L.; Pas, H.I.M.F.L.; Moen, M.H. Incidence of Acute Hamstring Injuries in Soccer: A Systematic Review of 13 Studies Involving More than 3800 Athletes with 2 Million Sport Exposure Hours. J. Orthop. Sports Phys. Ther. 2021, 51, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Gudelis, M.; Pruna, R.; Trujillano, J.; Lundblad, M.; Khodaee, M. Epidemiology of Hamstring Injuries in 538 Cases from an FC Barcelona Multi Sports Club. Phys. Sportsmed. 2024, 52, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Bengtsson, H.; Ekstrand, J.; Waldén, M.; Hägglund, M. Muscle Injury Rate in Professional Football Is Higher in Matches Played within 5 Days since the Previous Match: A 14-Year Prospective Study with More than 130 000 Match Observations. Br. J. Sports Med. 2018, 52, 1116–1122. [Google Scholar] [CrossRef] [PubMed]
- Timmins, R.G.; Shield, A.J.; Williams, M.D.; Opar, D.A. Is There Evidence to Support the Use of the Angle of Peak Torque as a Marker of Hamstring Injury and Re-Injury Risk? Sports Med. 2016, 46, 7–13. [Google Scholar] [CrossRef]
- Timmins, R.G.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Biceps Femoris Long Head Architecture: A Reliability and Retrospective Injury Study. Med. Sci. Sports Exerc. 2015, 47, 905–913. [Google Scholar] [CrossRef]
- Orchard, J.W.; Kountouris, A.; Sims, K. Risk Factors for Hamstring Injuries in Australian Male Professional Cricket Players. J. Sport Health Sci. 2017, 6, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.W.; Driscoll, T.; Seward, H.; Orchard, J.J. Relationship between Interchange Usage and Risk of Hamstring Injuries in the Australian Football League. J. Sci. Med. Sport 2012, 15, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Larruskain, J.; Celorrio, D.; Barrio, I.; Odriozola, A.; Gil, S.M.S.M.; Fernandez-Lopez, J.R.J.R.; Nozal, R.; Ortuzar, I.; Lekue, J.A.J.A.; Aznar, J.M.J.M. Genetic Variants and Hamstring Injury in Soccer: An Association and Validation Study. Med. Sci. Sports Exerc. 2018, 50, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.C.C.W.; Zarins, B.; Powell, J.W.; Kenyon, C.D. Hamstring Muscle Strains in Professional Football Players: A 10-Year Review. Am. J. Sports Med. 2011, 39, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Bramah, C.; Mendiguchia, J.; Dos’Santos, T.; Morin, J.B. Exploring the Role of Sprint Biomechanics in Hamstring Strain Injuries: A Current Opinion on Existing Concepts and Evidence. Sports Med. 2023, 54, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Wiese-Bjornstal, D.M. Psychology and Socioculture Affect Injury Risk, Response, and Recovery in High-Intensity Athletes: A Consensus Statement. Scand. J. Med. Sci. Sports 2010, 20, 103–111. [Google Scholar] [CrossRef]
- McCall, A.; Dupont, G.; Ekstrand, J. Injury Prevention Strategies, Coach Compliance and Player Adherence of 33 of the UEFA Elite Club Injury Study Teams: A Survey of Teams’ Head Medical Officers. Br. J. Sports Med. 2016, 50, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Dönmez, G.; Kudaş, S.; Yörübulut, M.; Yildirim, M.; Babayeva, N.; Torgutalp, Ş.Ş. Evaluation of Muscle Injuries in Professional Football Players: Does Coach Replacement Affect the Injury Rate? Clin. J. Sport Med. 2020, 30, 478–483. [Google Scholar] [CrossRef]
- Tee, J.C.; McLaren, S.J.; Jones, B. Sports Injury Prevention Is Complex: We Need to Invest in Better Processes, Not Singular Solutions. Sports Med. 2020, 50, 689–702. [Google Scholar] [CrossRef]
- Lievens, E.; Van Vossel, K.; Van de Casteele, F.; Wezenbeek, E.; Deprez, D.; Matthys, S.; De Winne, B.; McNally, S.; De Graaf, W.; Murdoch, J.B.; et al. Muscle Fibre Typology as a Novel Risk Factor for Hamstring Strain Injuries in Professional Football (Soccer): A Prospective Cohort Study. Sports Med. 2022, 52, 177–185. [Google Scholar] [CrossRef]
- Jokela, A.; Valle, X.; Kosola, J.; Rodas, G.; Til, L.; Burova, M.; Pleshkov, P.; Andersson, H.; Pasta, G.; Manetti, P.; et al. Mechanisms of Hamstring Injury in Professional Soccer Players: Video Analysis and Magnetic Resonance Imaging Findings. Clin. J. Sport Med. 2023, 33, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Kalema, R.N.; Duhig, S.J.; Williams, M.D.; Donaldson, A.; Shield, A.J. Sprinting Technique and Hamstring Strain Injuries: A Concept Mapping Study. J. Sci. Med. Sport 2022, 25, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Buckthorpe, M.; Wright, S.; Bruce-Low, S.; Nanni, G.; Sturdy, T.; Gross, A.S.; Bowen, L.; Styles, B.; Della Villa, S.; Davison, M.; et al. Recommendations for Hamstring Injury Prevention in Elite Football: Translating Research into Practice. Br. J. Sports Med. 2019, 53, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, D.M.; de Lima-e-Silva, F.X.; Aimi, M.; Vaz, M.A.; Baroni, B.M. Do Athletes with Hamstring Strain Injury Have Shorter Muscle Fascicles in the Injured Limb? J. Bodyw. Mov. Ther. 2024, 38, 269–273. [Google Scholar] [CrossRef]
- Opar, D.A.; Ruddy, J.D.; Williams, M.D.; Maniar, N.; Hickey, J.T.; Bourne, M.N.; Pizzari, T.; Timmins, R.G. Screening Hamstring Injury Risk Factors Multiple Times in a Season Does Not Improve the Identification of Future Injury Risk. Med. Sci. Sports Exerc. 2022, 54, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Takahashi, M.; Takamoto, K.; Bito, I. Hamstring Strains in Professional Rugby Players Result in Increased Fascial Stiffness without Muscle Quality Changes as Assessed Using Shear Wave Elastography. J. Bodyw. Mov. Ther. 2021, 27, 34–41. [Google Scholar] [CrossRef]
- Jansen, P.; Lehmann, J.; Fellner, B.; Huppertz, G.; Loose, O.; Achenbach, L.; Krutsch, W. Relation of Injuries and Psychological Symptoms in Amateur Soccer Players. BMJ Open Sport Exerc. Med. 2019, 5, e000522. [Google Scholar] [CrossRef]
- Smith, N.A.; Franettovich Smith, M.M.; Bourne, M.N.; Barrett, R.S.; Hides, J.A. A Prospective Study of Risk Factors for Hamstring Injury in Australian Football League Players. J. Sports Sci. 2021, 39, 1395–1401. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Perez, V.; Paredes, V.; Pastor, D.; Garrosa, F.N.; Vielcazat, S.J.; Del Coso, J.; Mendez-Villanueva, A. Under-Exposure to Official Matches Is Associated with Muscle Injury Incidence in Professional Footballers. Biol. Sport 2021, 38, 563–571. [Google Scholar] [CrossRef]
- Edouard, P.; Lahti, J.; Nagahara, R.; Samozino, P.; Navarro, L.; Guex, K.; Rossi, J.; Brughelli, M.; Mendiguchia, J.; Morin, J.B. Low Horizontal Force Production Capacity during Sprinting as a Potential Risk Factor of Hamstring Injury in Football. Int. J. Environ. Res. Public Health 2021, 18, 7827. [Google Scholar] [CrossRef]
- Edouard, P.; Mendiguchia, J.; Guex, K.; Lathi, J.; Samozino, P.; Morin, J.B. Sprinting: A Potential Vaccine for Hamstring Injury? Sport Perform. Sci. Rep. 2019, 1, 1–2. [Google Scholar]
- Lahti, J.; Mendiguchia, J.; Edouard, P.; Morin, J.B. A Novel Multifactorial Hamstring Screening Protocol: Association with Hamstring Muscle Injuries in Professional Football (Soccer)—A Prospective Cohort Study. Biol. Sport 2022, 39, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Malone, S.; Roe, M.; Doran, D.A.; Gabbett, T.J.; Collins, K. High Chronic Training Loads and Exposure to Bouts of Maximal Velocity Running Reduce Injury Risk in Elite Gaelic Football. J. Sci. Med. Sport 2017, 20, 250–254. [Google Scholar] [CrossRef]
- Wadey, R.; Day, M.; Cavallerio, F.; Martinelli, L. Multilevel Model of Sport Injury (MMSI). In Professional Advances in Sports Coaching; Thelwell, R., Dicks, M., Eds.; Routledge: London, UK, 2018; pp. 336–357. [Google Scholar]
- O’Brien, J.; Finch, C.F.; Pruna, R.; McCall, A. A New Model for Injury Prevention in Team Sports: The Team-Sport Injury Prevention (TIP) Cycle. Sci. Med. Footb. 2019, 3, 77–80. [Google Scholar] [CrossRef]
- Meeuwisse, W.H.; Tyreman, H.; Hagel, B.; Emery, C. A Dynamic Model of Etiology in Sport Injury: The Recursive Nature of Risk and Causation. Clin. J. Sport Med. 2007, 17, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Goode, A.P.; Reiman, M.P.; Harris, L.; DeLisa, L.; Kauffman, A.; Beltramo, D.; Poole, C.; Ledbetter, L.; Taylor, A.B. Eccentric Training for Prevention of Hamstring Injuries May Depend on Intervention Compliance: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2015, 49, 349–356. [Google Scholar] [CrossRef]
- McCall, A.; Jones, M.; Gelis, L.; Duncan, C.; Ehrmann, F.; Dupont, G.; Duffield, R. Monitoring Loads and Non-Contact Injury during the Transition from Club to National Team Prior to an International Football Tournament: A Case Study of the 2014 FIFA World Cup and 2015 Asia Cup. J. Sci. Med. Sport 2018, 21, 800–804. [Google Scholar] [CrossRef]
- Pol, R.; Hristovski, R.; Medina, D.; Balague, N. From Microscopic to Macroscopic Sports Injuries. Applying the Complex Dynamic Systems Approach to Sports Medicine: A Narrative Review. Br. J. Sports Med. 2019, 53, 1214–1220. [Google Scholar] [CrossRef]
- Stern, B.D.; Hegedus, E.J.; Lai, Y.C. Injury Prediction as a Non-Linear System. Phys. Ther. Sport 2020, 41, 43–48. [Google Scholar] [CrossRef]
- Tsarbou, C.; Liveris, N.I.; Xergia, S.A.; Tsekoura, M.; Fousekis, K.; Tsepis, E. Pre-Season ACL Risk Classification of Professional and Semi-Professional Football Players, via a Proof-of-Concept Test Battery. Appl. Sci. 2023, 13, 7780. [Google Scholar] [CrossRef]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Vanden Bossche, L.; Danneels, L.; Roosen, P. Impaired Core Stability as a Risk Factor for the Development of Lower Extremity Overuse Injuries: A Prospective Cohort Study. Am. J. Sports Med. 2019, 47, 1713–1721. [Google Scholar] [CrossRef] [PubMed]


| Steps | Task’s Purpose | Time | Script from Scriptapedia | Actions | Participants |
|---|---|---|---|---|---|
| A. | Review the main risk factors for acute hamstring injury (HI) from systematic reviews and relevant literature | - | - | Create a list of HI risk factors for further discussion in the group model building workshops. | Two members of the modeling Team |
| B | Group Model Building Workshops | ||||
| B1 | Discuss list of risk factors for acute HI | 120’ | Variable elicitation | Participants discuss the variables and remove or add variables. | Modeling team and two members of the stakeholders’ team |
| B1.1 | Create a CLD for acute HI (HI-CLD) based on literature and the discussion during the previous GMB session | - | - | Formulation of an initial perspective of HI risk factors interaction. | One member of the modeling team |
| B2 | Discuss and review the HI-CLD with the modeling team | 120’ | 1. Causal Mapping with Seed Structure, 2. Model Review 3. Next Steps and Closing | Review the HI-CLD and propose corrections. | Modeling team |
| B3 | Review HI-CLD with the modeling team | 60’ | 1. Model Review, 2. Next Steps and Closing | Review the HI-CLD after the corrections and prepare the following steps. | Modeling team |
| B4 | Presentation of CLD to stakeholders and incorporation of their point of view | 120’ | 1 Modeling Project Community Presentation, 2. Model Review | Presentation of HI-CLD to stakeholders. Discussion about the HI-CLD and the included variables. | Modeling team and all members of the Stakeholders’ team |
| B5 | Review the HI-CLD and incorporation of stakeholders’ points of view | 90’ | Initiating and elaborating a “Causal Loop Diagram” or “Stock and Flow” Model, 2. Model Review | Summarizing the inputs from stakeholders. | Modeling team |
| Model’s Factors | Stakeholders’ Viewpoint and Supporting Literature Evidence for Each Factor Included | Scoring (1–10) | |
|---|---|---|---|
| 1 | Level of influence of previous injury | Higher Order Factor that is a compound of simpler measures of previous injury characteristics [5,12,36]. Stakeholders agreed that is probably the most significant risk factor that affects soft tissue quality and the ability of muscle to generate appropriate functionality. | 9.20 |
| 2 | Quality of rehabilitation | Quick return to play without appropriate soft tissue reconditioning and insufficient ability of HS to tolerate the sport’s load demand increase the risk for re-injury. Evidence-based and sport-specific rehabilitation reduces the re-injury rate [5,18,33,36]. | 8.86 |
| 3 | Severity of previous injury | Severity of the first injury increases the risk for recurrence. The new injury tends to result in more days lost [5,12,33,36]. | 8.71 |
| 4 | Coache’s compliance with medical instruction | The coach is a critical person in injury prevention. Teams that their coaches have a more democratic style, better compliance, and communication with medical staff report fewer HIs [18,42]. Stakeholders agreed a coach with concentrate leadership style increases the (re)injuries likelihood. | 8.71 |
| 5 | Number of previous injuries | The number of previous HIs affects the soft tissue quality leading to future injuries [5,43]. | 8.57 |
| 6 | Scar Tissue Size and Quality | The size and the quality (elasticity, collagen quality) of scar tissue depend on the severity of previous HI and the quality of early mobility intervention. Scar tissue quality may has an impact on the athletes neuromuscular coordination affecting the re-injury rate [44,45]. | 8.57 |
| 7 | External or internal pressure on athlete to return to play after an injury | Coaches with a less democratic leadership style may puss athletes, with not properly healing injuries, to return to play or not consider the minor discomforts/injuries mentioned by the athletes [18,42]. | 8.57 |
| 8 | Accumulative fatigue | Fatigue during football games affects the HS muscle’s ability to decelerate the lower leg in the late swing phase of high-speed running. After fatigue, there is a decline in knee extension peak angles and total angles during running, affecting all running kinematics [18,46]. | 8.50 |
| 9 | Age | Older age athletes (>25) are at increased risk. This associated with a grater injury history, grater workload, and decline in soft tissue quality [5,12]. | 8.29 |
| 10 | Hamstring eccentric strength | Lower HS eccentric strength has been associated with HI and re-injury [43,47,48]. | 8.29 |
| 11 | Week-to-week changes in running exposure | Sudden changes in running exposure affect injury likelihood. More than the two-yearly average amount of high-speed running (>24 km/h) in the 4 weeks before HS injury and more significantly in the last week (OR = 6.44) impact the occurrence of HI [49]. Weekly distance covered above 24 km/h (RR = 3.4), and absolute week-to-week change in distance covered above 24 km/hour (RR = 3.3) had a significant impact on the risk of HI in the following week [17]. | 8.29 |
| 12 | Anatomical location | Previous HI increases the risk for new injury. History of HI (Risk Ratio (RR) = 2.7), previous ACL injury (RR = 1.7), and previous calf strain injury (RR = 1.5) significantly increase the risk for HI [5]. | 8.14 |
| 13 | Acute chronic workload ratio (ACWR) | Sudden changes in workload increase the fatigue and the risk for injury. ACWR within the range of 0.8–1.3 could be considered an appropriate level. ACWR ≥ 1.5 represents the ‘danger zone,’ and ACWR > 2.0 has been associated with a greater risk for injury relative to moderate or low ACWR (RR = 3.7–3.9) [16,50,51,52]. | 8.14 |
| 14 | Communication between medical staff and coaching staff | Lack of communication between the Medical and the coaching staff has been linked with a higher rate of HIs. It affects factors such as prevention strategies, rehabilitation, and load management in at-risk payers [18,42]. | 8.00 |
| 15 | Chronicity | Previous HI in the same season significantly increases the risk for re-injury (RR = 4.8) [5]. | 7.86 |
| 16 | Accumulative workload | Higher chronic training loads with a balanced ACWR protect athletes by producing positive neuromuscular adaptations. It is measured: Internal loads: RPE, External loads: GPS, accelerometer [50,51,53]. | 7.86 |
| 17 | Quality of high-speed running biomechanics | Higher order factor that is a compound of various measure kinematic and kinetic variables during high-speed running, mainly assessed by 3D kinematic evaluation | 7.81 |
| 18 | Quality of high acceleration movements | The primary mechanism leading to HI [54]. | 7.80 |
| 19 | Neuromuscular coordination | Higher Order Factor that is a compound of simpler measures about the neuromuscular condition. | 7.75 |
| 20 | Strength and flexibility asymmetries | High strength and flexibility asymmetries are proposed as potential risk factors. High interlimb asymmetries are associated with asymmetrical imposed loads on athletes [5]. | 7.71 |
| 21 | Structural and HS architectural quality | A collective variable that describes the quality of structural and architectural characteristics | 7.71 |
| 22 | Hamstring eccentric load during sprinting | Large extension moments in hip and knee power absorption during the swing phase of running would place competing demands on the HIs [8,10]. | 7.71 |
| 23 | Injury prevention strategies | Evidence-based overall prevention strategies applied by the teams are essential for HI prevention [55,56]. | 7.71 |
| 24 | Strength quality | A collective factor that describes the quality of the whole strength characteristics. It is measured by isokinetic dynamometer (ID), hand-held dynamometer (HHD), Nordic hamstring device [5]. | 7.57 |
| 25 | Hamstring strength endurance | A decline in eccentric hamstring endurance may be associated with changes in the intermuscular recruitment pattern, increasing the risk of injury [57]. | 7.57 |
| 26 | Hamstring flexibility | Conflicted evidence for the linear association of hamstring flexibility and injury. Reducing hamstring flexibility after return to play is associated with re-injury. It is measured by passive single leg raise (SLR), active knee extension (AKE), and passive knee extension (PKE) [5,43]. | 7.57 |
| 27 | In-season recovery from competition | Medical experts of high-level football teams have highlighted the strategies as a significant risk factor. lack of in-season recovery may increase the workload and accumulative fatigue [18]. | 7.57 |
| 28 | Hamstring EMG activation pattern/intermuscular interplay/intermuscular hierarchy | Athletes whose HIs activated after the lumbar erector spinae were eight times more likely to sustain a hamstring injury [58]. The overactivation of the biceps femoris and the decline of the semitendinosus activation during eccentric exercise have been connected to HI [59]. | 7.43 |
| 29 | High-speed running exposure during training | Lack of regular exposure to high-speed football during training sessions may make athletes unprepared to cope with demanding situations during sports participation. Exposures to maximal velocity running during training reduce the HI risk [18,53]. | 7.43 |
| 30 | Permanent medical staff in the team | The existence of adequate and permanent medical staff within the team is important for appropriate injury prevention [60,61]. | 7.43 |
| 31 | Psychological mood | A collective higher-order factor that composes the quality of multiple measure factors of athlete psychological characteristics (daily hassles, anxiety, negative life events, common mental disorders (CMD)). It is assessed by the use of various questionnaires. Included studies assess all sports injuries, non-specific studies for HI risk [55,62,63]. | 7.33 |
| 32 | Hamstring: quadriceps strength ratio | Conflicted evidence about the linear relationship of hamstring to quadriceps ratio and HI. It is proposed that an increased ratio increases the risk for HI [5,34]. This factor affects the overall strength quality and performance. | 7.29 |
| 33 | Hamstrings fascial stiffness | Increased passive stiffness of fascial tissues is observed in the leg with a previous history of HI [64]. Hamstring stiffness is defined as the resistance to a particular external force that changes the muscle’s shape and is determined from the mechanical oscillation of the leg evaluated by an accelerometer. It is measured by MRI, and shear wave elastography [65]. | 7.29 |
| 34 | Dynamic core stability | Lateral trunk flexion and low electromyography (EMG) activity of trunk muscle during running have been associated with HI. Core stability is considered an important factor for injury prevention and high speed running performance [8,9,10]. Dynamic assessment: 3D kinematic evaluation. Static Assessment: Core endurance tests (maximum time). | 7.29 |
| 35 | Biceps femoris long head (BFlh) fascicle length | Biceps femoris long head length fascicles shorter than 10.56 cm (RR = 4.1) increase the risk for HI [48,66]. | 7.14 |
| 36 | Lateral trunk flexion | Ipsilateral to late swing phase trunk flexion during high-speed running has been associated with HI [8,10]. | 7.14 |
| 37 | Motivation | Sports devaluation and overall burnout symptoms have been linked to HIs. Athlete’s doubts about the benefits gained from the sports may lead to loss of concentration, increasing the risk of injury [21,22]. | 7.14 |
| 38 | Negative life event | Negative life events stress (previous injury, death of a family member, etc.) has been associated with future injuries in football [67]. | 7.14 |
| 39 | Core and gluteal EMG activity during swing phase | Graeter gluteal and trunk muscle electromyographic activation during the swing phase of sprinting were related with a decreased risk of HIs [9]. | 7.00 |
| 40 | Exposure rate to training and competition | Higher exposure to training and matches increases the total workload and the exposure of athletes to high-speed running [50,51]. | 7.00 |
| 41 | Level of competition | Higher levels of competition cause athletes to have increased workloads and are imposed more on external risk factors [68,69]. | 7.00 |
| 42 | Match congestion | Muscle injuries were lower when there were at least 6 days between the matches’ exposure [6,70]. | 7.00 |
| 43 | Angle of peak torque | The angle of peak torque production has been proposed as a potential risk factor for HI and re-injury. Hamstring torque production in the outer range position (near knee extension with hip flexion) is an important measure [71]. | 6.86 |
| 44 | Pennation angle | Pennation angle was significantly greater in injured BFlh than uninjured control at rest and during isometric contraction as measured by ultrasound [72]. | 6.86 |
| 45 | Sleep quality | Lower sleep quality has been associated with HIs [21]. | 6.86 |
| 46 | BMI | Conflicted evidence. Did not significantly increase HI [5,12]. Injured players had significantly higher BMI [19]. | 6.71 |
| 47 | Time loss from sports participation due to injury | The higher time loss is associated with larger soft tissue damage, increasing the possibility of re-injury [33]. | 6.67 |
| 48 | Gender | HS incidence is 0.3 to 0.5 per 1000 h of exposure in women and 0.3 to 1.9 per 1000 h of exposure in men [68]. | 6.57 |
| 49 | Environmental condition | There is no clear evidence. The different environmental conditions in the match’s place may indirectly affect the occurrence of injury [5,73]. | 6.50 |
| 50 | Cross-sectional area (CSA) | Larger CSA is associated with a higher ability of muscle to produce power. It is measured by MRI [48,66]. | 6.43 |
| 51 | Leg length discrepancy | Functional leg length asymmetries (OR = 3.80) have been associated with HI [13]. | 6.43 |
| 52 | Interchange of opponent player | A player who enters to play after a rest on the interchange bench may have short-term protection against HI due to the absence of fatigue. However, his unfatigued condition may contribute to increased average high-speed running for his direct opponent, increasing the fatigue and the risk of injury for the opposition team’s players [5,74]. | 6.43 |
| 53 | Genetic factors | Genetic variants seem to be involved in the multifactorial etiology of HIs, as measured by genotyping [75]. | 6.00 |
| 54 | Player position | The player position that requires more high-speed running actions increases the injury risk [5,36,76]. | 6.00 |
| 55 | Athlete’s aerobic capacity | Higher athlete’s aerobic capacity protects against high workload and ACWR [50,51,53]. | 5.86 |
| 56 | Surface type | HI risk is 1.5-fold higher on grass compared with artificial turf surfaces [1]. | 5.86 |
| 57 | Team financial level | Team’s sports performance is significantly affected by injuries and financial performance. Investment in injury prevention can reduce the injury incidence [60]. | 5.86 |
| 58 | Team financial consistency | Team financial consistency affects the work of the team’s staff and athletes [60]. | 5.71 |
| 59 | Season phase | Season phase impacts the workload characteristics applied to athletes [5,76]. | 5.14 |
| The following variables included after reviewing stakeholders’ discussion and conducting further literature review | |||
| 60 | Lumbo-pelvic control | Anterior pelvic tilt increases tensile forces on HS during running. Lack of appropriate lumbo-pelvic stability may increase the anterior pelvic tilt during high-speed movements [77]. | |
| 61 | Sociocultural stress | The expectation from athletes to be “tough” and participate in sports through pain and injury. Factors such as social pressure mechanisms, organizational stress, and stress in pursuit of high achievement in sports affect the response to injury [78]. | |
| 62 | Compliance of athlete | Lack of player adherence to medical and coach instructions may limit the effects of contemporary injury prevention programs [79]. | |
| 63 | Changes in coaches and medical staff | Replacement of head staff members (coaches, trainers, medical staff) in male elite-level football teams seems associated with increased HI burden during the season [61,80]. | |
| 64 | Local and national injury prevention policies | Investment in injury prevention, national and league characteristics [20,70,80,81]. | |
| 65 | Muscle fiber typology | Athletes with faster typology fibers are 5.3 more likely to sustain a HI. Potential correlation with fatigue [82]. | |
| Loop | Definition |
|---|---|
| B1 | HS re-injury loop |
| B2 | Effect of psychological factors loop |
| B3 | Effect of neuromuscular coordination on fatigue and the total injury risk |
| B4 | Negative workload effect on neuromuscular coordination due to fatigue loop |
| R1 | Positive workload effect on neuromuscular coordination loop |
| 1 | (Re) Evaluation | |
|---|---|---|
| Factors | Measurements | |
| External Workload | Global position system (GPS) data (daily data collection) | |
| Internal Workload (Sence of fatigue) | Borg’s rating of perceived exertion (RPE) (daily data collection) | |
| High-speed running biomechanics | Two-dimensional video analysis or Inertial sensors (weekly or monthly evaluation) | |
| Ballistic function | Triple hop for distance test (weekly or monthly evaluation) | |
| Core muscle strength endurance | Prone Bridging Test, Side Bridging Test, Biering–Sorensen test (weekly or monthly evaluation) | |
| Hamstring strength endurance | Single-leg hamstring bridge (SLHB) (weekly or monthly evaluation) | |
| Hamstring eccentric strength | Hand-held dynamometer (HHD). Brake test at 30° of knee flexion from a prone position (weekly or monthly evaluation) | |
| Hamstring, hip flexors, calf muscle flexibility | Straight leg raise (SLR), modify Thomas, weight-bearing lunge test (WBLT) (weekly or monthly evaluation) | |
| Psychological condition | Athlete Burnout Questionnaire (ABQ) (weekly or monthly evaluation) | |
| 2 | Identification of specific impairments of athletes | |
| 3 | HI preventive strategies and interventions to tackle specific athlete impairments | |
| Impairments | Interventions | |
| Low eccentric strength, isometric to eccentric ratio or increased interlimb asymmetries | HS eccentric strength exercises (e.g., Nordic hamstrings exercise, dead lift) to increase strength and reduce interlimb asymmetries | |
| Low repetitions in SLHB test < 25 repetitions | HS Strength endurance exercises | |
| Decrease flexibility below cut-points and asymmetries in SLR test, modify Thomas test, WBLT. | Hamstring, hip flexors, and soleus flexibility exercises | |
| Exposure to high-speed running during training | Constant exposure to high-speed sports training without high week-to-week changes and maintaining the weekly exposure < 24 kg/h | |
| Core stability and lower limb impairments in running kinematics | Proper running kinematics, preventing later trunk flexion and forward trunk lean | |
| Impairments in core stability observed in running assessment and in specific core muscle strength endurance tests | Core stability exercises | |
| Impairments in core stability and increased anterior pelvic tilt | Lumbopelvic control exercises, preventing anterior pelvic tilt | |
| High values in the specific psychological questionnaire or during interviews with sports psychologists | Psychological interventions to reduce possible psychological symptoms | |
| Increase psychological and physiological fatigue or pain in hamstrings during the evaluation protocol. | Adequate recovery from the competition and specific interventions | |
| Athlete compliance with medical and coaching instructions | Strategies to increase athletes’ adherence to preventive interventions | |
| Communication quality between medical and coaching staff | Proper communication between medical and coaching staff. Frequent medical and coaching staff discussions and meetings about the management of injured athletes and the application of injury prevention strategies | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liveris, N.I.; Tsarbou, C.; Papageorgiou, G.; Tsepis, E.; Fousekis, K.; Kvist, J.; Xergia, S.A. The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach. Appl. Sci. 2024, 14, 6316. https://doi.org/10.3390/app14146316
Liveris NI, Tsarbou C, Papageorgiou G, Tsepis E, Fousekis K, Kvist J, Xergia SA. The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach. Applied Sciences. 2024; 14(14):6316. https://doi.org/10.3390/app14146316
Chicago/Turabian StyleLiveris, Nikolaos I., Charis Tsarbou, George Papageorgiou, Elias Tsepis, Konstantinos Fousekis, Joanna Kvist, and Sofia A. Xergia. 2024. "The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach" Applied Sciences 14, no. 14: 6316. https://doi.org/10.3390/app14146316
APA StyleLiveris, N. I., Tsarbou, C., Papageorgiou, G., Tsepis, E., Fousekis, K., Kvist, J., & Xergia, S. A. (2024). The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach. Applied Sciences, 14(14), 6316. https://doi.org/10.3390/app14146316










