Blood Flow Restriction Exercise as a Novel Conservative Standard in Patients with Knee Osteoarthritis—A Narrative Review
Abstract
1. Introduction
2. Methodological Considerations
3. Results
3.1. Effect of BFRT in KOA
3.2. Mechanisms of BFRT
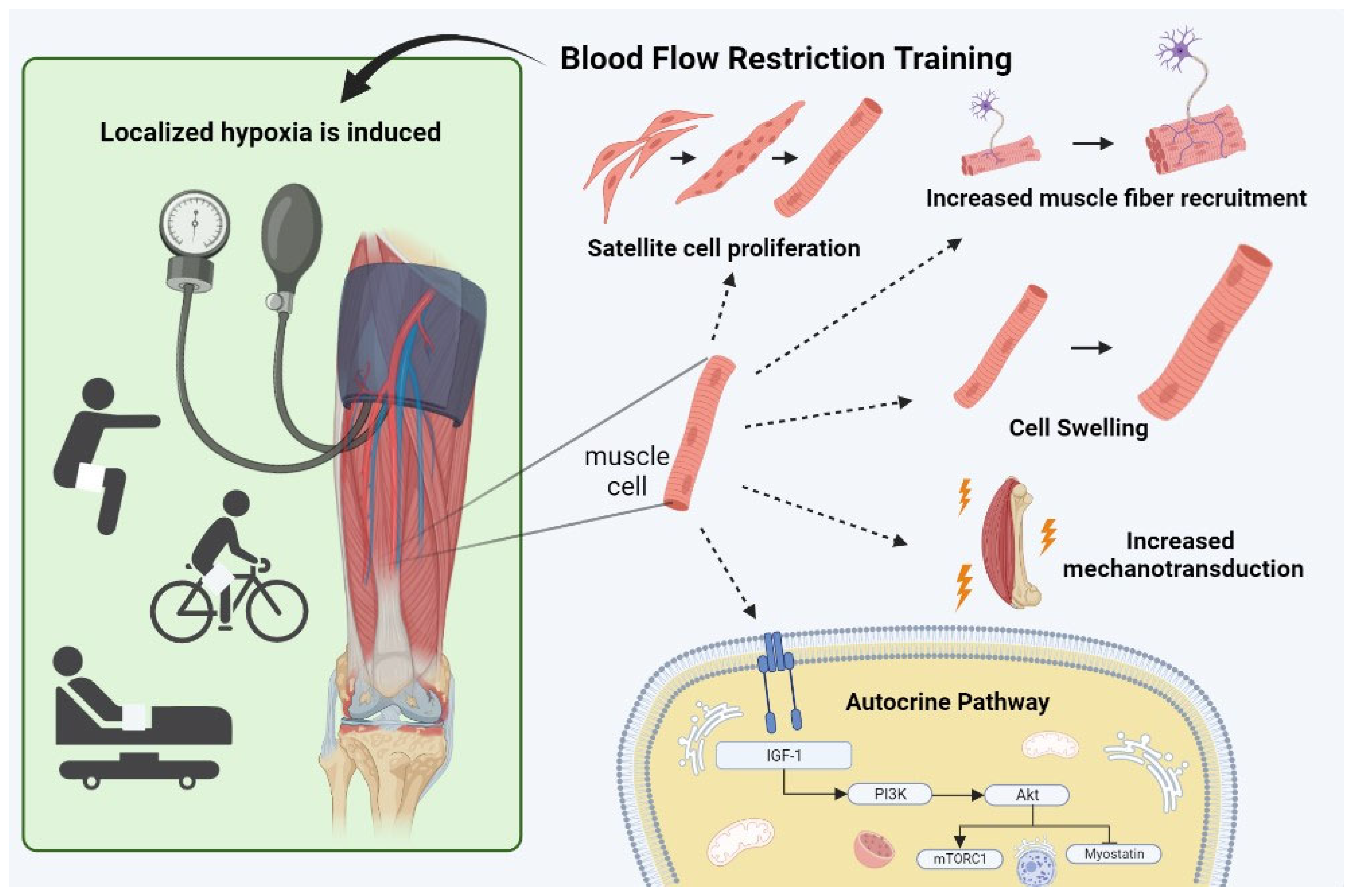
3.2.1. Hypertrophy and Strength
3.2.2. Muscle Fiber Recruitment
3.2.3. Mechanotransduction
3.2.4. Cell Swelling
3.2.5. Muscle Damage
3.2.6. Autocrine Pathway
3.2.7. Pain
3.3. Safety of Blood Flow Restriction
3.3.1. Risk for Venous Thromboembolism
3.3.2. Excessive Cardiovascular Response
3.3.3. Rhabdomyolysis
4. Practical Guidelines to Enhance Safety and Optimize Training Effectiveness
5. Practical Implementation
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Cui, A.; Li, H.; Wang, D.; Zhong, J.; Chen, Y.; Lu, H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine 2020, 29, 100587. [Google Scholar] [CrossRef] [PubMed]
- Sharma, L. Osteoarthritis of the Knee. N. Engl. J. Med. 2021, 384, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.K.; Goyal, N.; Deirmengian, G.; Rangavajulla, A.; Parvizi, J.; Austin, M.S. Revision total knee arthroplasty in the young patient: Is there trouble on the horizon? J. Bone Jt. Surg. 2014, 96, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Vince, K.G. You can do arthroplasty in a young patient, but…: Commentary on articles by John P. Meehan, MD; et al.: “Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty,” and Vinay K. Aggarwal; et al.: “Revision total knee arthroplasty in the young patient: Is there trouble on the horizon?”. J. Bone Jt. Surg. 2014, 96, e58. [Google Scholar] [CrossRef]
- Carr, A.J.; Robertsson, O.; Graves, S.; Price, A.J.; Arden, N.K.; Judge, A.; Beard, D.J. Knee replacement. Lancet 2012, 379, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. 2020, 72, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Skou, S.T.; Roos, E.M. Physical therapy for patients with knee and hip osteoarthritis: Supervised, active treatment is current best practice. Clin. Exp. Rheumatol. 2019, 37 (Suppl. S120), 112–117. [Google Scholar]
- Fisher, N.M.; Pendergast, D.R.; Gresham, G.E.; Calkins, E. Muscle rehabilitation: Its effect on muscular and functional performance of patients with knee osteoarthritis. Arch. Phys. Med. Rehabil. 1991, 72, 367–374. [Google Scholar]
- Schilke, J.M.; Johnson, G.O.; Housh, T.J.; O’Dell, J.R. Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nurs. Res. 1996, 45, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Wilson, J.M.; Lowery, R.P.; Krieger, J.W. Muscular adaptations in low- versus high-load resistance training: A meta-analysis. Eur. J. Sport Sci. 2016, 16, 1–10. [Google Scholar] [CrossRef]
- American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2009, 41, 687–708. [Google Scholar] [CrossRef]
- Hu, C.; Zhu, B.; Wang, Y.; Yang, F.; Zhang, J.; Zhong, W.; Lu, S.; Luo, C. Effectiveness of blood flow restriction versus traditional weight-bearing training in rehabilitation of knee osteoarthritis patients with MASLD: A multicenter randomized controlled trial. Front. Endocrinol. 2023, 14, 1220758. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.W.; Man, G.C.; Choi, B.C.; Yeung, Y.M.; Qiu, J.H.; Lu, X.M.; Ong, M.T.; Yung, P.S. The predictors to self-reported and performance-based physical function in knee osteoarthritis patients: A cross-sectional study. Front. Cell Dev. Biol. 2024, 12, 1406830. [Google Scholar] [CrossRef]
- Zeng, C.Y.; Zhang, Z.R.; Tang, Z.M.; Hua, F.Z. Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Front. Physiol. 2021, 12, 794062. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.; Paton, B.; Rosenblatt, B.; Gissane, C.; Patterson, S.D. Blood flow restriction training in clinical musculoskeletal rehabilitation: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1003–1011. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Kang, S.H.; Kim, N.; Choi, J.; Kang, S. Short-Term Impact of Low-Intensity Exercise with Blood Flow Restriction on Mild Knee Osteoarthritis in Older Adults: A Pilot Study. Healthcare 2024, 12, 308. [Google Scholar] [CrossRef] [PubMed]
- Lixandrao, M.E.; Ugrinowitsch, C.; Berton, R.; Vechin, F.C.; Conceicao, M.S.; Damas, F.; Libardi, C.A.; Roschel, H. Magnitude of Muscle Strength and Mass Adaptations Between High-Load Resistance Training Versus Low-Load Resistance Training Associated with Blood-Flow Restriction: A Systematic Review and Meta-Analysis. Sports Med. 2018, 48, 361–378. [Google Scholar] [CrossRef]
- Abe, T.; Sakamaki, M.; Fujita, S.; Ozaki, H.; Sugaya, M.; Sato, Y.; Nakajima, T. Effects of low-intensity walk training with restricted leg blood flow on muscle strength and aerobic capacity in older adults. J. Geriatr. Phys. Ther. 2010, 33, 34–40. [Google Scholar]
- Abe, T.; Fujita, S.; Nakajima, T.; Sakamaki, M.; Ozaki, H.; Ogasawara, R.; Sugaya, M.; Kudo, M.; Kurano, M.; Yasuda, T.; et al. Effects of Low-Intensity Cycle Training with Restricted Leg Blood Flow on Thigh Muscle Volume and VO2MAX in Young Men. J. Sports Sci. Med. 2010, 9, 452–458. [Google Scholar] [PubMed]
- Held, S.; Behringer, M.; Donath, L. Low intensity rowing with blood flow restriction over 5 weeks increases VO2max in elite rowers: A randomized controlled trial. J. Sci. Med. Sport 2020, 23, 304–308. [Google Scholar] [CrossRef]
- Ferraz, R.B.; Gualano, B.; Rodrigues, R.; Kurimori, C.O.; Fuller, R.; Lima, F.R.; Ana Lúcia, D.S.-P.; Roschel, H. Benefits of Resistance Training with Blood Flow Restriction in Knee Osteoarthritis. Med. Sci. Sports Exerc. 2018, 50, 897–905. [Google Scholar] [CrossRef]
- Bryk, F.F.; Dos Reis, A.C.; Fingerhut, D.; Araujo, T.; Schutzer, M.; Cury Rde, P.; Duarte, A., Jr.; Fukuda, T.Y. Exercises with partial vascular occlusion in patients with knee osteoarthritis: A randomized clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1580–1586. [Google Scholar] [CrossRef]
- Pearson, S.J.; Hussain, S.R. A review on the mechanisms of blood-flow restriction resistance training-induced muscle hypertrophy. Sports Med. 2015, 45, 187–200. [Google Scholar] [CrossRef]
- Freitas, E.D.S.; Karabulut, M.; Bemben, M.G. The Evolution of Blood Flow Restricted Exercise. Front. Physiol. 2021, 12, 747759. [Google Scholar] [CrossRef] [PubMed]
- Patterson, S.D.; Hughes, L.; Warmington, S.; Burr, J.; Scott, B.R.; Owens, J.; Abe, T.; Nielsen, J.L.; Libardi, C.A.; Laurentino, G.; et al. Blood Flow Restriction Exercise: Considerations of Methodology, Application, and Safety. Front. Physiol. 2019, 10, 533. [Google Scholar] [CrossRef]
- Loenneke, J.P.; Fahs, C.A.; Wilson, J.M.; Bemben, M.G. Blood flow restriction: The metabolite/volume threshold theory. Med. Hypotheses 2011, 77, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Green, H.; Goreham, C.; Ouyang, J.; Ball-Burnett, M.; Ranney, D. Regulation of fiber size, oxidative potential, and capillarization in human muscle by resistance exercise. Am. J. Physiol. 1999, 276, R591–R596. [Google Scholar] [CrossRef]
- Fry, A.C. The role of resistance exercise intensity on muscle fibre adaptations. Sports Med. 2004, 34, 663–679. [Google Scholar] [CrossRef]
- Takarada, Y.; Takazawa, H.; Sato, Y.; Takebayashi, S.; Tanaka, Y.; Ishii, N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J. Appl. Physiol. 2000, 88, 2097–2106. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.R.; Burgomaster, K.A.; Schofield, L.M.; Gibala, M.J.; Sale, D.G.; Phillips, S.M. Neuromuscular adaptations in human muscle following low intensity resistance training with vascular occlusion. Eur. J. Appl. Physiol. 2004, 92, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, T.; Brechue, W.F.; Fujita, T.; Shirakawa, J.; Sato, Y.; Abe, T. Muscle activation during low-intensity muscle contractions with restricted blood flow. J. Sports Sci. 2009, 27, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Zou, K.; Meador, B.M.; Johnson, B.; Huntsman, H.D.; Mahmassani, Z.; Valero, M.C.; Huey, K.A.; Boppart, M.D. The alpha(7)beta(1)-integrin increases muscle hypertrophy following multiple bouts of eccentric exercise. J. Appl. Physiol. 2011, 111, 1134–1141. [Google Scholar] [CrossRef] [PubMed]
- Schiaffino, S.; Reggiani, C.; Akimoto, T.; Blaauw, B. Molecular Mechanisms of Skeletal Muscle Hypertrophy. J. Neuromuscul. Dis. 2021, 8, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Fry, C.S.; Glynn, E.L.; Drummond, M.J.; Timmerman, K.L.; Fujita, S.; Abe, T.; Dhanani, S.; Volpi, E.; Rasmussen, B.B. Blood flow restriction exercise stimulates mTORC1 signaling and muscle protein synthesis in older men. J. Appl. Physiol. 2010, 108, 1199–1209. [Google Scholar] [CrossRef]
- Fujita, S.; Abe, T.; Drummond, M.J.; Cadenas, J.G.; Dreyer, H.C.; Sato, Y.; Volpi, E.; Rasmussen, B.B. Blood flow restriction during low-intensity resistance exercise increases S6K1 phosphorylation and muscle protein synthesis. J. Appl. Physiol. 2007, 103, 903–910. [Google Scholar] [CrossRef] [PubMed]
- Lang, F.; Busch, G.L.; Ritter, M.; Volkl, H.; Waldegger, S.; Gulbins, E.; Haussinger, D. Functional significance of cell volume regulatory mechanisms. Physiol. Rev. 1998, 78, 247–306. [Google Scholar] [CrossRef] [PubMed]
- Loenneke, J.P.; Fahs, C.A.; Rossow, L.M.; Abe, T.; Bemben, M.G. The anabolic benefits of venous blood flow restriction training may be induced by muscle cell swelling. Med. Hypotheses 2012, 78, 151–154. [Google Scholar] [CrossRef]
- Takarada, Y.; Takazawa, H.; Ishii, N. Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med. Sci. Sports Exerc. 2000, 32, 2035–2039. [Google Scholar] [CrossRef]
- Kubota, A.; Sakuraba, K.; Sawaki, K.; Sumide, T.; Tamura, Y. Prevention of disuse muscular weakness by restriction of blood flow. Med. Sci. Sports Exerc. 2008, 40, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Nyakayiru, J.; Fuchs, C.J.; Trommelen, J.; Smeets, J.S.J.; Senden, J.M.; Gijsen, A.P.; Zorenc, A.H.; LJC, V.A.N.L.; Verdijk, L.B. Blood Flow Restriction Only Increases Myofibrillar Protein Synthesis with Exercise. Med. Sci. Sports Exerc. 2019, 51, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Proske, U.; Morgan, D.L. Muscle damage from eccentric exercise: Mechanism, mechanical signs, adaptation and clinical applications. J. Physiol. 2001, 537, 333–345. [Google Scholar] [CrossRef] [PubMed]
- Umbel, J.D.; Hoffman, R.L.; Dearth, D.J.; Chleboun, G.S.; Manini, T.M.; Clark, B.C. Delayed-onset muscle soreness induced by low-load blood flow-restricted exercise. Eur. J. Appl. Physiol. 2009, 107, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Allen, D.G.; Whitehead, N.P.; Yeung, E.W. Mechanisms of stretch-induced muscle damage in normal and dystrophic muscle: Role of ionic changes. J. Physiol. 2005, 567, 723–735. [Google Scholar] [CrossRef] [PubMed]
- Yeung, E.W.; Whitehead, N.P.; Suchyna, T.M.; Gottlieb, P.A.; Sachs, F.; Allen, D.G. Effects of stretch-activated channel blockers on [Ca2+]i and muscle damage in the mdx mouse. J. Physiol. 2005, 562, 367–380. [Google Scholar] [CrossRef]
- Thiebaud, R.S.; Loenneke, J.P.; Fahs, C.A.; Kim, D.; Ye, X.; Abe, T.; Nosaka, K.; Bemben, M.G. Muscle damage after low-intensity eccentric contractions with blood flow restriction. Acta Physiol. Hung. 2014, 101, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Thiebaud, R.S.; Yasuda, T.; Loenneke, J.P.; Abe, T. Effects of low-intensity concentric and eccentric exercise combined with blood flow restriction on indices of exercise-induced muscle damage. Interv. Med. Appl. Sci. 2013, 5, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Takarada, Y.; Nakamura, Y.; Aruga, S.; Onda, T.; Miyazaki, S.; Ishii, N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J. Appl. Physiol. 2000, 88, 61–65. [Google Scholar] [CrossRef]
- Sieljacks, P.; Matzon, A.; Wernbom, M.; Ringgaard, S.; Vissing, K.; Overgaard, K. Muscle damage and repeated bout effect following blood flow restricted exercise. Eur. J. Appl. Physiol. 2016, 116, 513–525. [Google Scholar] [CrossRef]
- De Queiros, V.S.; Dantas, M.; Neto, G.R.; da Silva, L.F.; Assis, M.G.; Almeida-Neto, P.F.; Dantas, P.M.S.; Cabral, B. Application and side effects of blood flow restriction technique: A cross-sectional questionnaire survey of professionals. Medicine 2021, 100, e25794. [Google Scholar] [CrossRef]
- De Queiros, V.S.; Dos Santos, I.K.; Almeida-Neto, P.F.; Dantas, M.; de Franca, I.M.; Vieira, W.H.B.; Neto, G.R.; Dantas, P.M.S.; Cabral, B. Effect of resistance training with blood flow restriction on muscle damage markers in adults: A systematic review. PLoS ONE 2021, 16, e0253521. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Wang, H.; Hu, P. Stem cell activation in skeletal muscle regeneration. Cell. Mol. Life Sci. CMLS 2015, 72, 1663–1677. [Google Scholar] [CrossRef]
- Wernbom, M.; Apro, W.; Paulsen, G.; Nilsen, T.S.; Blomstrand, E.; Raastad, T. Acute low-load resistance exercise with and without blood flow restriction increased protein signalling and number of satellite cells in human skeletal muscle. Eur. J. Appl. Physiol. 2013, 113, 2953–2965. [Google Scholar] [CrossRef]
- Nielsen, J.L.; Aagaard, P.; Bech, R.D.; Nygaard, T.; Hvid, L.G.; Wernbom, M.; Suetta, C.; Frandsen, U. Proliferation of myogenic stem cells in human skeletal muscle in response to low-load resistance training with blood flow restriction. J. Physiol. 2012, 590, 4351–4361. [Google Scholar] [CrossRef] [PubMed]
- Wozniak, A.C.; Anderson, J.E. Nitric oxide-dependence of satellite stem cell activation and quiescence on normal skeletal muscle fibers. Dev. Dyn. Off. Publ. Am. Assoc. Anat. 2007, 236, 240–250. [Google Scholar] [CrossRef]
- Yoshida, T.; Delafontaine, P. Mechanisms of IGF-1-Mediated Regulation of Skeletal Muscle Hypertrophy and Atrophy. Cells 2020, 9, 1970. [Google Scholar] [CrossRef]
- Trendelenburg, A.U.; Meyer, A.; Rohner, D.; Boyle, J.; Hatakeyama, S.; Glass, D.J. Myostatin reduces Akt/TORC1/p70S6K signaling, inhibiting myoblast differentiation and myotube size. Am. J. Physiol. Cell Physiol. 2009, 296, C1258–C1270. [Google Scholar] [CrossRef] [PubMed]
- Laurentino, G.C.; Ugrinowitsch, C.; Roschel, H.; Aoki, M.S.; Soares, A.G.; Neves, M., Jr.; Aihara, A.Y.; Fernandes Ada, R.; Tricoli, V. Strength training with blood flow restriction diminishes myostatin gene expression. Med. Sci. Sports Exerc. 2012, 44, 406–412. [Google Scholar] [CrossRef]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef]
- Da Costa, B.R.; Reichenbach, S.; Keller, N.; Nartey, L.; Wandel, S.; Juni, P.; Trelle, S. Effectiveness of non-steroidal anti-inflammatory drugs for the treatment of pain in knee and hip osteoarthritis: A network meta-analysis. Lancet 2017, 390, e21–e33. [Google Scholar] [CrossRef] [PubMed]
- Zeng, C.; Doherty, M.; Persson, M.S.M.; Yang, Z.; Sarmanova, A.; Zhang, Y.; Wei, J.; Kaur, J.; Li, X.; Lei, G.; et al. Comparative efficacy and safety of acetaminophen, topical and oral non-steroidal anti-inflammatory drugs for knee osteoarthritis: Evidence from a network meta-analysis of randomized controlled trials and real-world data. Osteoarthr. Cartil. 2021, 29, 1242–1251. [Google Scholar] [CrossRef] [PubMed]
- Bannuru, R.R.; Schmid, C.H.; Kent, D.M.; Vaysbrot, E.E.; Wong, J.B.; McAlindon, T.E. Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: A systematic review and network meta-analysis. Ann. Intern. Med. 2015, 162, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Koltyn, K.F.; Arbogast, R.W. Perception of pain after resistance exercise. Br. J. Sports Med. 1998, 32, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.; Patterson, S.D. The effect of blood flow restriction exercise on exercise-induced hypoalgesia and endogenous opioid and endocannabinoid mechanisms of pain modulation. J. Appl. Physiol. 2020, 128, 914–924. [Google Scholar] [CrossRef] [PubMed]
- Korakakis, V.; Whiteley, R.; Giakas, G. Low load resistance training with blood flow restriction decreases anterior knee pain more than resistance training alone. A pilot randomised controlled trial. Phys. Ther. Sport 2018, 34, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Ogrezeanu, D.C.; Lopez-Bueno, L.; Sanchis-Sanchez, E.; Suso-Marti, L.; Lopez-Bueno, R.; Nunez-Cortes, R.; Cruz-Montecinos, C.; Perez-Alenda, S.; Casana, J.; Gargallo, P.; et al. Exercise-induced hypoalgesia with end-stage knee osteoarthritis during different blood flow restriction levels: Sham-controlled crossover study. PM&R 2023, 15, 1565–1573. [Google Scholar] [CrossRef]
- McGuire, D.B. Comprehensive and multidimensional assessment and measurement of pain. J. Pain Symptom Manag. 1992, 7, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Hughes, L.; Patterson, S.D. Low intensity blood flow restriction exercise: Rationale for a hypoalgesia effect. Med. Hypotheses 2019, 132, 109370. [Google Scholar] [CrossRef]
- Gronfeldt, B.M.; Lindberg Nielsen, J.; Mieritz, R.M.; Lund, H.; Aagaard, P. Effect of blood-flow restricted vs heavy-load strength training on muscle strength: Systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 837–848. [Google Scholar] [CrossRef]
- Minniti, M.C.; Statkevich, A.P.; Kelly, R.L.; Rigsby, V.P.; Exline, M.M.; Rhon, D.I.; Clewley, D. The Safety of Blood Flow Restriction Training as a Therapeutic Intervention for Patients With Musculoskeletal Disorders: A Systematic Review. Am. J. Sports Med. 2020, 48, 1773–1785. [Google Scholar] [CrossRef]
- Nakajima, T.; Kurano, M.; Iida, H.; Takano, H.; Oonuma, H.; Morita, T.; Meguro, K.; Sato, Y.; Nagata, T. Use and safety of KAATSU training:Results of a national survey. Int. J. KAATSU Train Res. 2006, 2, 5–13. [Google Scholar] [CrossRef]
- Hughes, L.; Rosenblatt, B.; Gissane, C.; Paton, B.; Patterson, S.D. Interface pressure, perceptual, and mean arterial pressure responses to different blood flow restriction systems. Scand. J. Med. Sci. Sports 2018, 28, 1757–1765. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, R.; Kyle, K.; Mikhail, C.S.; Weatherford, B.; Brandner, C. Perceived Barriers to Blood Flow Restriction Training. Front. Physiol. 2021, 8, 697082. [Google Scholar] [CrossRef]
- Bond, C.W.; Hackney, K.J.; Brown, S.L.; Noonan, B.C. Blood Flow Restriction Resistance Exercise as a Rehabilitation Modality Following Orthopaedic Surgery: A Review of Venous Thromboembolism Risk. J. Orthop. Sports Phys. Ther. 2019, 49, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, P.M.; Ritchie, I.K.; Albadran, L.; Glen, S.K.; Bridges, A.B.; Ely, M. Do thigh tourniquets contribute to the formation of intra-operative venous emboli? Acta Orthop. Belg. 2004, 70, 253–259. [Google Scholar]
- Madarame, H.; Kurano, M.; Takano, H.; Iida, H.; Sato, Y.; Ohshima, H.; Abe, T.; Ishii, N.; Morita, T.; Nakajima, T. Effects of low-intensity resistance exercise with blood flow restriction on coagulation system in healthy subjects. Clin. Physiol. Funct. Imaging 2010, 30, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Spranger, M.D.; Krishnan, A.C.; Levy, P.D.; O’Leary, D.S.; Smith, S.A. Blood flow restriction training and the exercise pressor reflex: A call for concern. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H1440–H1452. [Google Scholar] [CrossRef]
- Cristina-Oliveira, M.; Meireles, K.; Spranger, M.D.; O’Leary, D.S.; Roschel, H.; Pecanha, T. Clinical safety of blood flow-restricted training? A comprehensive review of altered muscle metaboreflex in cardiovascular disease during ischemic exercise. Am. J. Physiol. Heart Circ. Physiol. 2020, 318, H90–H109. [Google Scholar] [CrossRef]
- Scott, B.R.; Peiffer, J.J.; Thomas, H.J.; Marston, K.J.; Hill, K.D. Hemodynamic Responses to Low-Load Blood Flow Restriction and Unrestricted High-Load Resistance Exercise in Older Women. Front. Physiol. 2018, 9, 1324. [Google Scholar] [CrossRef]
- Neto, G.R.; Novaes, J.S.; Dias, I.; Brown, A.; Vianna, J.; Cirilo-Sousa, M.S. Effects of resistance training with blood flow restriction on haemodynamics: A systematic review. Clin. Physiol. Funct. Imaging 2017, 37, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Araujo, J.P.; Silva, E.D.; Silva, J.C.; Souza, T.S.; Lima, E.O.; Guerra, I.; Sousa, M.S. The acute effect of resistance exercise with blood flow restriction with hemodynamic variables on hypertensive subjects. J. Hum. Kinet. 2014, 43, 79–85. [Google Scholar] [CrossRef]
- Thompson, K.M.A.; Slysz, J.T.; Burr, J.F. Risks of Exertional Rhabdomyolysis with Blood Flow-Restricted Training: Beyond the Case Report. Clin. J. Sport Med. 2018, 28, 491–492. [Google Scholar] [CrossRef]
- Tabata, S.; Suzuki, Y.; Azuma, K.; Matsumoto, H. Rhabdomyolysis After Performing Blood Flow Restriction Training: A Case Report. J. Strength Cond. Res. 2016, 30, 2064–2068. [Google Scholar] [CrossRef] [PubMed]
- Clark, B.C.; Manini, T.M. Can KAATSU Exercise Cause Rhabdomyolysis? Clin. J. Sport Med. 2017, 27, e1–e2. [Google Scholar] [CrossRef]
- Burr, J.F.; Hughes, L.; Warmington, S.; Scott, B.R.; Owens, J.; Abe, T.; Nielsen, J.L.; Libardi, C.A.; Laurentino, G.; Neto, G.R.; et al. Response: Commentary: Can Blood Flow Restricted Exercise Cause Muscle Damage? Commentary on Blood Flow Restriction Exercise: Considerations of Methodology, Application, and Safety. Front. Physiol. 2020, 11, 574633. [Google Scholar] [CrossRef]
- Sauret, J.M.; Marinides, G.; Wang, G.K. Rhabdomyolysis. Am. Fam. Physician 2002, 65, 907–912. [Google Scholar]
- Jacobs, E.; Rolnick, N.; Wezenbeek, E.; Stroobant, L.; Capelleman, R.; Arnout, N.; Witvrouw, E.; Schuermans, J. Investigating the autoregulation of applied blood flow restriction training pressures in healthy, physically active adults: An intervention study evaluating acute training responses and safety. Br. J. Sports Med. 2023, 57, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Segal, N.A.; Williams, G.N.; Davis, M.C.; Wallace, R.B.; Mikesky, A.E. Efficacy of blood flow-restricted, low-load resistance training in women with risk factors for symptomatic knee osteoarthritis. PM&R J. Inj. Funct. Rehabil. 2015, 7, 376–384. [Google Scholar] [CrossRef]
- Segal, N.; Davis, M.D.; Mikesky, A.E. Efficacy of Blood Flow-Restricted Low-Load Resistance Training For Quadriceps Strengthening in Men at Risk of Symptomatic Knee Osteoarthritis. Geriatr. Orthop. Surg. Rehabil. 2015, 6, 160–167. [Google Scholar] [CrossRef]
- Jessee, M.B.; Buckner, S.L.; Mouser, J.G.; Mattocks, K.T.; Loenneke, J.P. Letter to the editor: Applying the blood flow restriction pressure: The elephant in the room. Am. J. Physiol. Heart Circ. Physiol. 2016, 310, H132–H133. [Google Scholar] [CrossRef] [PubMed]
- Lixandrao, M.E.; Ugrinowitsch, C.; Laurentino, G.; Libardi, C.A.; Aihara, A.Y.; Cardoso, F.N.; Tricoli, V.; Roschel, H. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur. J. Appl. Physiol. 2015, 115, 2471–2480. [Google Scholar] [CrossRef] [PubMed]
- Spitz, R.W.; Chatakondi, R.N.; Bell, Z.W.; Wong, V.; Viana, R.B.; Dankel, S.J.; Abe, T.; Yamada, Y.; Loenneke, J.P. Blood Flow Restriction Exercise: Effects of Sex, Cuff Width, and Cuff Pressure on Perceived Lower Body Discomfort. Percept. Mot. Ski. 2021, 128, 353–374. [Google Scholar] [CrossRef] [PubMed]
- Loenneke, J.P.; Wilson, J.M.; Marin, P.J.; Zourdos, M.C.; Bemben, M.G. Low intensity blood flow restriction training: A meta-analysis. Eur. J. Appl. Physiol. 2012, 112, 1849–1859. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.R.; Loenneke, J.P.; Slattery, K.M.; Dascombe, B.J. Exercise with blood flow restriction: An updated evidence-based approach for enhanced muscular development. Sports Med. 2015, 45, 313–325. [Google Scholar] [CrossRef] [PubMed]
- Loenneke, J.P.; Abe, T.; Wilson, J.M.; Thiebaud, R.S.; Fahs, C.A.; Rossow, L.M.; Bemben, M.G. Blood flow restriction: An evidence based progressive model. Acta Physiol. Hung. 2012, 99, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Centner, C.; Wiegel, P.; Gollhofer, A.; Konig, D. Effects of Blood Flow Restriction Training on Muscular Strength and Hypertrophy in Older Individuals: A Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 95–108. [Google Scholar] [CrossRef] [PubMed]
- Slysz, J.; Stultz, J.; Burr, J.F. The efficacy of blood flow restricted exercise: A systematic review & meta-analysis. J. Sci. Med. Sport 2016, 19, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Clarkson, M.J.; Conway, L.; Warmington, S.A. Blood flow restriction walking and physical function in older adults: A randomized control trial. J. Sci. Med. Sport 2017, 20, 1041–1046. [Google Scholar] [CrossRef]
- De Queiros, V.S.; Rolnick, N.; Schoenfeld, B.J.; de França, I.M.; Vieira, J.G.; Sardeli, A.V.; Kamis, O.; Neto, G.R.; Cabral, B.G.D.A.T.; Dantas, P.M.S. Hypertrophic effects of low-load blood flow restriction training with different repetition schemes: A systematic review and meta-analysis. PeerJ 2024, 12, e17195. [Google Scholar] [CrossRef]
| Research Domain | Search Strategy | Hits |
|---|---|---|
| Blood Flow Restriction | (“blood flow restriction training” OR “BFR training” OR “blood flow restriction exercise” OR “BFR exercise” OR “blood flow restriction therapy” OR “BFR therapy” OR “blood-flow restriction” OR BFR OR “occlusion training” OR “occlusion therapy” OR “Blood Flow Restriction Therapy”[Mesh]) | 7277 |
| Knee Osteoarthritis | “knee osteoarthr *” or “KOA” or “gonarthrosis” | 35,349 |
| Resting State BFR Accommodation | Aerobic Training | Low-Load Resistance Training | |
|---|---|---|---|
| Patient Profile | Sedentary patients; Patients starting to rehabilitate after a period of bedrest; Patients with anxiety for BFRT | All KOA patients | All KOA patients |
| LOP | 70–100% LOP | <50% VO2max or HRR | 40–80% LOP (depending on the patient’s training status) |
| Training Frequency | 1–2×/day during supine position | 2–3×/week | 2–3×/week |
| Restriction time | 5 min | 5–20 min per exercise | 5–10 min per exercise |
| Repetitions & Rest Between Sets | 3–5×/5 min, 3–5 min passive recovery | 2–4×/5 min up to 2 × 10 min, 1–2 min active or passive recovery | 60 reps—15/15/15/15, 30–60 s rest |
| Restriction Form | Intermittent | Continuous or intermittent | Continuous or intermittent |
| Type Of Exercise | None; Electrostimulation | Walking; Cycling; rowing |
|
| Expected Training Results | Prevention of muscle atrophy, familiarization with BFR | Optimization of cardiovascular response to aerobic stimuli; muscle volume and strength gains | Muscle volume and strength gains |
| Safety Guidelines | Use individualized LOP and autoregulated BFR devices, guaranteeing safe occlusion pressure levels | Use individualized LOP and autoregulated BFR devices, guaranteeing safe occlusion pressure levels | Use individualized LOP and autoregulated BFR devices, guaranteeing safe occlusion pressure levels |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacobs, E.; Witvrouw, E.; Calders, P.; Stroobant, L.; Victor, J.; Schuermans, J.; Wezenbeek, E. Blood Flow Restriction Exercise as a Novel Conservative Standard in Patients with Knee Osteoarthritis—A Narrative Review. Appl. Sci. 2024, 14, 6150. https://doi.org/10.3390/app14146150
Jacobs E, Witvrouw E, Calders P, Stroobant L, Victor J, Schuermans J, Wezenbeek E. Blood Flow Restriction Exercise as a Novel Conservative Standard in Patients with Knee Osteoarthritis—A Narrative Review. Applied Sciences. 2024; 14(14):6150. https://doi.org/10.3390/app14146150
Chicago/Turabian StyleJacobs, Ewoud, Erik Witvrouw, Patrick Calders, Lenka Stroobant, Jan Victor, Joke Schuermans, and Evi Wezenbeek. 2024. "Blood Flow Restriction Exercise as a Novel Conservative Standard in Patients with Knee Osteoarthritis—A Narrative Review" Applied Sciences 14, no. 14: 6150. https://doi.org/10.3390/app14146150
APA StyleJacobs, E., Witvrouw, E., Calders, P., Stroobant, L., Victor, J., Schuermans, J., & Wezenbeek, E. (2024). Blood Flow Restriction Exercise as a Novel Conservative Standard in Patients with Knee Osteoarthritis—A Narrative Review. Applied Sciences, 14(14), 6150. https://doi.org/10.3390/app14146150







