1. Introduction
Severe malocclusions and facial deformities of skeletal origin can be treated with a combined orthodontic and surgical approach. Orthognathic surgery (OGS) aims to achieve normal occlusion with optimal dental and facial aesthetics and requires a multidisciplinary team approach with the collaboration of oral and maxillofacial surgeons, orthodontists, restorative dentists, and psychologists. Typically, definitive surgical planning is performed once the teeth are moved to their ideal positions in relation to the skeletal bases, in a pre-surgical orthodontic phase.
Depending on the aetiology of the malocclusion, OGS may involve one or both jaws and it can be performed with either a single-splint or double-splint technique. An orthognathic surgical splint (OSS) is used by the operating surgeon intra-operatively to assist in the positioning of the segments of the jaw(s) in their corrected position following osteotomy. Usually, a single jaw surgery requires a single splint to position the jaw in need of surgical correction, whereas double jaw (bimaxillary) surgery requires an intermediate splint first, in order to first position the maxillary or mandibular segment, followed by application of the final splint to position the remaining osteotomised segment. The accuracy of the fabricated OSS plays an important role in achieving the pre-operatively planned surgical movements during OGS, and this, in turn, influences the overall surgical outcome.
1.1. Treatment Planning in Orthognathic Surgery
1.1.1. Traditional Surgical Planning
Traditionally, surgical planning for OGS has been based on the findings from clinical examination in conjunction with two-dimensional (2D) cephalometric analysis. However, there are many limitations with the traditional method, which include: errors associated with landmark identification and linear and angular measurement errors when using the 2D cephalometric analysis [
1,
2], particularly in the presence of facial asymmetries [
3,
4]; inaccuracies associated with facebow record transfers and bite registration [
5]; and lack of precise control over rotational and translational movements of the plaster casts during the model surgery [
6]. In addition, traditional methods also require technicians to have a firm understanding of the properties of the dental materials used. These issues mean that the dimensions of the final fabricated OSS may be affected by errors accumulated along sequential stages of production.
1.1.2. Virtual Surgical Planning
The introduction of 3D imaging and computer-aided design (CAD) has led to the development of computer-assisted 3D virtual surgical planning (VSP) in OGS, through which a detailed representation of the craniofacial anatomy and enhanced analysis of surgical planning became available. Three-dimensional VSP has been shown to improve the predictability of surgical outcomes [
7,
8,
9,
10], and it certainly is becoming popular within the field [
11].
Three-dimensional VSP starts with the acquisition of intra-oral optical light scans of the dental arches and a cone beam computed tomography (CBCT) scan of the facial bones. A voxel size of 1.0 mm or less is normally required for the CBCT scan, and the acquired CBCT data are extracted in the Digital Imaging and Communications in Medicine (DICOM) format for alignment and fusion with the dental arch scans [
12]. This process creates a virtual patient model that can be segmented and osteotomised for simulation of the planned surgical movements. The maxilla-first approach is most commonly practised as it has been shown to be more predictable than the mandible-first approach unless there is an anti-clockwise rotation of the maxilla and mandible [
13].
A virtual OSS is then created by either inserting a virtual object between the upper and lower teeth and making an indentation of the occlusal surfaces of the upper and lower teeth or virtual filling in of the void between the upper and lower dental models in the new position. The final design of the virtual OSS is then extracted in Standard Tessellation Language (STL) file format and fabricated using a 3D printer [
14]. The OSSs fabricated in this manner have been shown to be highly accurate [
15,
16,
17].
1.2. Definition of Accuracy and Precision in 3D Printing
Three-dimensional printing is an additive manufacturing technique that refers to a process where a 3D object is fabricated by laying down one layer at a time with each successive layer bonding to the preceding layer, and each of these layers can be seen as a thinly sliced cross-section of the object. The main advantages of this technique include its ability to create undercuts, overhangs, and other highly detailed and complex geometry with less material waste.
Accuracy, or trueness, refers to how close the measurements are to the true value, and it is assessed by measuring the degree of deviation in a measurement of the printed object from the actual dimensions of the virtual object [
18]. A printer with a higher accuracy indicates the printer that delivers a result that is closer or equal to the actual dimensions of the digital 3D object. In contrast, precision refers to how close the repeated measurements are to each other and indicates repeatability. A printer with a higher precision correlates to one that produces a more repeatable and consistent print.
1.3. Variables in 3D Printing
1.3.1. Print Orientation
The alignment of an object within the space of the build volume may influence the accuracy and precision of the final 3D-printed product. It is recommended that large, flat surfaces are orientated at an angle between 10° to 20° to reduce the surface area of each layer and the amount of force applied to the print as the build platform elevates after building each layer [
19].
In addition, any objects with two parts of the object that eventually merge together, like an OSS which is horseshoe-shaped, should be orientated in such a way that a shared base is formed first before the layers branch into individual paths. Theoretically, this helps to prevent any cracks or splits forming at the intersection.
All objects should ideally be oriented to self-support themselves with no or minimal amount of overhang where possible. The risk of dimensional changes during post-processing can be reduced by eliminating, or minimising, the number of support structures required.
1.3.2. Print Layer Height
Print layer height refers to the thickness of each layer of material added during the printing process, and it corresponds to the vertical resolution in the Z-axis. Although some CAD/CAM software allows the users to enter free values, the majority offer a couple of print layer height options that are pre-determined according to the manufacturer’s recommendations.
Despite the early suggestions that printing in thinner layers (or higher Z-resolution) would produce more accurate prints, several studies have concluded that there is no difference in the measurements between the objects 3D-printed in 25, 50, and 100 μm layer heights [
20,
21]. The overall printing speed and time taken for each print job are predominantly determined by the number of layers required to create an object, and therefore, it must be selected carefully.
1.3.3. Post-Processing
The objects printed with an SLA printer require washing, drying, and post-curing. These post-processing steps may result in dimensional changes and affect the overall accuracy and precision of the printed objects. The examples of the sources of error include: surface material loss during washing in propan-2-ol, more commonly known as isopropyl alcohol (IPA) [
22,
23]; over-drying leading to the formation of cracks; and curing time and method, which affects the degree of polymerisation shrinkage during the post-curing stage. Whilst some of these can be easy to account for during design and print preparation, others can vary from print to print.
1.3.4. Printing Materials
The choice of printing material is primarily determined by the type of 3D printing technology used. An SLA printer is a type of vat photopolymerisation that uses liquid photopolymers such as acrylates and epoxides, similar to material jetting printers. Material extrusion printers, on the other hand, use polylactic acid or acrylonitrile butadiene styrene, and powder bed fusion printers use polyamides or thermoplastic polyurethanes in powder form.
Over the years, manufacturers have developed many different formulas with varying compositions to enhance certain physical and mechanical properties. The use of different resin materials is one of many factors that may influence the accuracy and precision of 3D-printed OSSs, but currently, there is limited published evidence in the literature evaluating the relationship between them.
1.4. Aims and Objectives
The aim of this study was to assess the accuracy and precision of OSSs 3D-printed in three different resin materials using an SLA printer.
2. Materials and Methods
2.1. Splint Design and Fabrication
A set of typodont models with a full adult dentition (except for third molars) in good alignment and without any spacing was used to represent the dentition of a pre-surgical OGS patient. The upper and lower models were scanned using a laboratory scanner (E3, 3Shape, Copenhagen, Denmark), and a single 3D virtual OSS was designed digitally using the ‘Splint Construction’ function of an orthodontic CAD software, OrthoAnalyzer 1,9, (3Shape, Copenhagen, Denmark). This was then further modified by adding a small loop on the lateral aspect of the virtual splint in the right molar region to allow identification tags to be tied onto the splint. The STL file of the 3D virtual OSS was imported into PreForm software (Formlabs, Somerville, MA, USA,
https://formlabs.com/software/preform/ accessed on 1 July 2024) and was prepared for 3D printing. There were 10 splints per batch, all orientated vertically at 270° with the posterior section directed away from the build platform, as shown in
Figure 1. The supporting structures were generated using the automatic generation function of the software, ensuring that none of these were positioned on the fitting surface.
A medical-grade professional SLA 3D printer (Form 3+, Formlabs, Herning, Denmark) was used to print a total of 90 splints with 30 splints in each of the 3 different resin materials selected: Surgical Guide (SG), Dental LT V2 (DLTV2), and Biomed Clear (BMC) (Formlabs, Somerville, MA, USA). The smallest print layer height available was selected for each resin material to provide the best resolution. Three batches were printed per resin material giving a total of 90 splints. The printed splints were then washed in IPA using FormWash (Formlabs, Somerville, MA, USA), dried, and post-cured using FormCure (Formlabs, Somerville, MA, USA) as per the manufacturer’s specifications. A visual inspection was carried out for any obvious defects or errors, and all splints appeared to fit the teeth on the typodont models passively without the application of additional force for seating.
2.2. Data Collection
The following linear measurements were taken from the upper arch by a single operator using a digital caliper (Preciva Vernier Caliper, Preciva, Portland, OR, USA):
Intercanine width (ICW): The distance between the deepest point of indentation of the right and left canine cusps in the surgical splint
Intermolar width (IMW): The distance between the deepest point indentation of the mesiobuccal cusps of the right and left first molars in the surgical splint
Arch length (AL): The length of a line drawn from a point between the labial surfaces of the central incisors to the mid-point of a line connecting the mesiobuccal cusps of the first molar teeth.
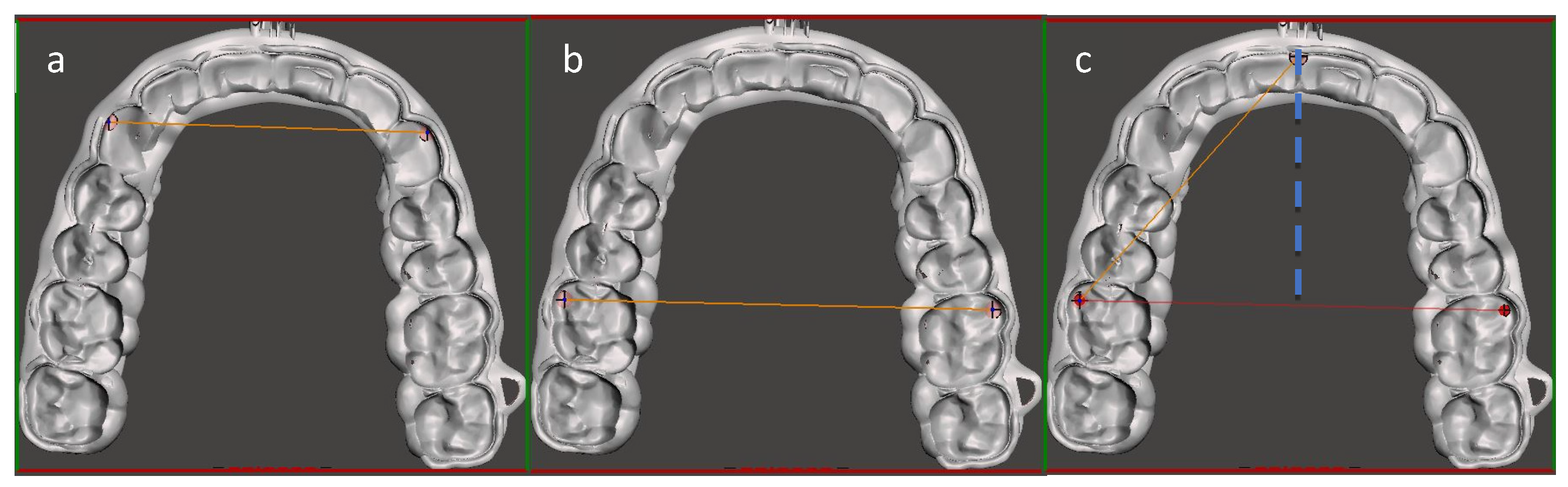
The reference values for upper ICW and IMW were taken virtually from the master STL file of the virtual OSS, using 3D modelling software (Meshmixer, Autodesk Inc., San Francisco, CA, USA,
https://meshmixer.com/), as shown in
Figure 2. The AL of the upper arch was calculated according to Pythagoras’ theorem, using: (1) the distance between a point between the labial surfaces of the two central incisors and the most prominent point of the mesiobuccal cusp of the left first permanent molar, and (2) the distance between the midpoint of the line drawn for IMW measurement and the most prominent point of the mesiobuccal cusp of left first permanent molar.
2.3. Intra-Rater Reliability
Intra-rater reliability was assessed by analysing the data from 2 time points, measured by the same operator at a 2-week interval. The measurements were taken from 10 OSSs printed in SG, and a paired samples
t-test was performed using data analysis software (Minitab LLC, State College, PA, USA,
https://www.minitab.com/). When analysing the data, a
p-value level of
p < 0.05 was assumed to be statistically significant.
2.4. Data Analysis
The collected data were analysed using SPSS (SPSS Statistics Premium 29, IBM, New York, NY, USA) and Minitab v19 (Minitab LLC, State College, PA, USA) for assessment of the accuracy and precision. Consistency with a normal distribution was assessed using the Ryan–Joiner test in Minitab to address if data should be analysed with parametric or non-parametric methods. To assess the accuracy, the mean values for each dataset were compared against the corresponding reference value obtained digitally from the master STL by performing a one-sample
t-test. In addition, the magnitude of error for each dataset was also investigated using the absolute value of the difference between the reference value and each measurement. To assess the precision, the coefficient of variance (CoV) was calculated using the formula below.
(
σ = standard deviation,
μ = mean).
The overall study design is summarised in
Figure 3.
3. Results
3.1. Assessment of Intra-Rater Reliability
The absolute difference between measurements on the two occasions had a median (minimum to maximum) of 0.04 (0.00 to 0.08) mm for ICW, 0.06 (0.01 to 0.11) mm for IMW, and 0.09 (0.02 to 0.19) mm for AL. Thus, in each case, the maximum difference was less than 0.50 mm.
3.2. Assessment of Accuracy and Precision
The mean, standard deviation, and
p-value from one sample
t-test for each parameter of the 3 study groups are shown in
Table 1. The one sample
t-tests were carried out with respect to the respective reference values. It also shows the mean and maximum deviation, which indicates the magnitude of error, as well as the CoV.
All measurements were statistically different from the reference values, except for the ICW and AL in the SG group and the IMW in the BMC group. All mean deviation values were within the clinically acceptable range, which was set at <0.500 mm; the SG group demonstrated the smallest mean deviation for all 3 measurements with 0.088 mm for ICW, 0.126 mm for IMW, and 0.170 mm for AL, and the greatest mean deviation was observed in AL measurements for all 3 materials with 0.170 mm for SG, 0.307 mm for DLTV2, and 0.303 mm for BMC. However, the maximum deviation values for IMW in DLTV2 and BMC groups and AL for all 3 materials were greater than the clinically acceptable deviation, indicating that some of these splints were unacceptable for clinical use.
The CoV values for the 3 resin materials varied depending on the parameter and they were in the ranges of 0.284–0.504% for ICW, 0.227–0.515% for IMW, and 0.709–0.802% for AL. Although the CoV values of the ICWs and IMWs were comparable, those of ALs were much higher than the other two for all 3 resin materials, with the highest value of 0.802% in the DLTV2 group. In terms of overall precision, the SG group had the lowest CoV values for all 3 parameters, indicating that it was more precise than the other resin materials.
3.3. Tolerance of the Printer vs. Clinically Acceptable Deviation
Tolerance is the amount of random deviation or variation permitted for a given dimension, and it reflects the ability of a 3D printer to produce a consistent print that is as close to the master STL as possible. The tolerance limit of a typical SLA printer quoted by the manufacturer was ‘±0.2% with a lower limit of ±0.1 mm’ [
18]; the tolerance limit was set to ±0.1 mm for this analysis as 0.2% of reference values were smaller than 0.1 mm for all measurements. The proportion of OSSs that were within the tolerance limit was in the range of 60.0–96.7% for ICW, 40.0–83.3% for IMW, and 33.3–66.7% for AL, as shown in
Table 2, highlighting that the printer did not meet the tolerance limit quoted by the manufacturer.
A clinically acceptable deviation, on the other hand, refers to the amount of deviation that is permitted without causing a significant impact on the clinical outcome. The clinically acceptable deviation (distance error) was set at ± 0.5 mm. The proportion of splints that were within the clinically acceptable range for each measurement is shown in
Table 3.
3.4. Illustration of the Results
Scatter plots have been drawn for each parameter to illustrate the results as shown in
Figure 4.
4. Discussion
4.1. Z-Resolution
In this study, the OSSs were oriented vertically at 270° and the AL measurements represented the accuracy and precision in the
Z- (or vertical) axis. The greatest magnitude of error and CoV values were observed in AL measurements, and the proportion of splints that were within the clinically acceptable range was considerably lower when compared with the ICW and IMW. This indicates that the greatest inaccuracy and variation was seen in the
Z-axis, which is similar to the findings from other studies that also reported on variation in the
Z-direction being more pronounced than in the
X- or
Y-direction [
17]. Another study conducted by Boyer et al. demonstrated that orthodontic aligners printed vertically at 90° to the build platform were the most accurate, with this being the only group that printed within the clinically acceptable tolerance ranges in comparison to the 7 other orientation groups in this study [
24].
One possible source of the greatest variation in the Z-axis is the motorised stepper motor controlling the print platform height of the 3D printer, which elevates the build plate as each layer is laid. Given that the greatest inaccuracy and variation were seen in the Z-direction, it may be prudent to advise that the splints are printed flat relative to the printer base plate, ensuring that the supports are clear of the fit surface, in order to minimise the effect of the Z-axis variation found.
4.2. Design of Dental Base
The results of this study demonstrate that the IMW is one of the two measurements that showed lower accuracy and precision than ICW for all 3 material groups. Orthognathic surgical splints are designed to engage the occlusal contours of the maxillary and mandibular teeth and have a fitting surface on both sides. For this reason, the splints were designed and printed in a horseshoe shape without any bases. However, horseshoe-shaped models are at greater risk of distortion particularly towards the posterior end. A study conducted by Camardella et al. reported that models with horseshoe-shaped bases print less accurately than other types of dental bases such as the American Board of Orthodontics base design or a horseshoe design with a posterior connection, both of which were shown to be accurate [
25]. An addition of a structure that connects the left and right sides of the posterior ends of the virtual OSS at the designing stage may help to improve the accuracy and precision of the 3D-printed splints. This additional support structure will need to be removed prior to the OGS, as it would interfere with the position of the tongue and prevent the OSS from being seated properly.
4.3. Post-Processing Protocols
This study has been conducted by following the post-processing protocols recommended by the manufacturer. However, there are alternative protocols that have been reported to be more successful in enhancing the degree of conversion, which refers to the extent of monomer-to-polymer conversion during curing, and mechanical properties, thus minimising the dimensional inaccuracies occurring during the printing process.
Oxygen is reported to have adverse effects on the polymerisation process and studies have been conducted to evaluate the effect of oxygen shielding and temperature on the degree of conversion and mechanical properties of 3D-printed photopolymer products. Lim et al. reported that the highest degree of conversion and flexural modulus was observed for specimens post-cured while immersed in glycerin for oxygen shielding when compared with those post-cured in a medium-low vacuum chamber at 5 × 10
−2 Torr or no additional conditioning [
26]. In addition, increasing the temperature to 80 °C further enhanced this effect.
Another study conducted by Simunovic had similar findings, emphasising the importance of oxygen shielding to maximise the degree of conversion and flexural modulus [
27]. This study revealed that the washing protocol also influences the mechanical properties of the 3D-printed products; washing in IPA showed increased resistance to wear in comparison to the centrifuge and ethanol rinse treatments, whereas centrifugation followed by nitrogen polymerisation exhibited the highest flexural modulus.
4.4. Indirect, Calculated Method of Determining Arch Length
The 3D imaging software used to measure reference values from the STL file of the virtual OSS required two points, between which the measurement is taken, to be defined on the virtual object for any linear measurements to be taken. This meant that arch length could not be measured directly using the digital method, and it had to be calculated indirectly using Pythagoras’ theorem.
The addition of a posterior connection to the master model of the OSS, as described in
Section 4.2, may enable the reference AL to be taken virtually from the STL file of the virtual OSS rather than using the indirect, calculated method used in this study. This would also allow all measurements to be taken virtually once the 3D-printed splints have been scanned with a laboratory optical scanner.
5. Conclusions
There were statistically significant differences between the reference dimensions of the virtual splint and the corresponding mean measurements of the 3D-printed splints, and the SG group was found to be superior to the DLTV2 and BMC groups. However, most of the splints demonstrated clinically acceptable accuracy and precision across all study groups.
This study has also highlighted some other important points that need to be addressed. Firstly, the greatest inaccuracy and variation was observed in the AL measurement for all three materials, which relates to the Z-axis of the printer. Secondly, a significant proportion of the splints did not meet the tolerance limit that was quoted by the manufacturer.
Further research assessing the 3D accuracy and precision of 3D-printed OSSs would help to explore the variation found between different resin materials used and confirm the findings of this research. In the meantime, it may be prudent to advise that surgical wafers are printed flat relative to the printer base plate, ensuring that the supports are clear of the fit surface, to minimise the effect of Z-axis variation.
Author Contributions
Methodology and investigation, N.Y.K.; formal analysis, D.W.; writing—original draft preparation, N.Y.K.; writing—review and editing, C.D.D. and F.B.N.; supervision, C.D.D. and F.B.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Dataset available on request from the authors.
Acknowledgments
We would like to thank Shanghyun Park from the 3D Unit at Kingston Hospital for his technical assistance with the CAD/CAM software and the fabrication of the virtual OSS used in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 1. Landmark identification. Am. J. Orthod. 1971, 60, 111–127. [Google Scholar] [CrossRef]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 2. Conventional angular and linear measures. Am. J. Orthod. 1972, 60, 505–517. [Google Scholar] [CrossRef] [PubMed]
- Lonic, D.; Pai, B.C.-J.; Yamaguchi, K.; Chortrakarnkij, P.; Lin, H.-H.; Lo, L.-J. Computer-Assisted Orthognathic Surgery for Patients with Cleft Lip/Palate: From Traditional Planning to Three-Dimensional Surgical Simulation. PLoS ONE 2016, 11, e0152014. [Google Scholar] [CrossRef] [PubMed]
- Lundstrom, A.; Lundstrom, F.; Lebret, L.M.; Moorrees, C.F. Natural head position and natural head orientation: Basic considerations in cephalometric analysis and research. Eur. J. Orthod. 1995, 17, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Zizelmann, C.; Hammer, B.; Gellrich, N.C.; Schwestka-Polly, R.; Rana, M.; Bucher, P. An evaluation of face-bow transfer for the planning of orthognathic surgery. J. Oral Maxillofac. Surg. 2012, 70, 1944–1950. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, R.; Reychler, H. Limitations of orthognathic model surgery: Theoretical and practical implications. Rev. Stomatol. Chir. Maxillo-Faciale 2004, 105, 165–169. [Google Scholar] [CrossRef]
- Awad, D.; Reinert, S.; Kluba, S. Accuracy of Three-Dimensional Soft-Tissue Prediction Considering the Facial Aesthetic Units Using a Virtual Planning System in Orthognathic Surgery. J. Pers. Med. 2022, 12, 1379. [Google Scholar] [CrossRef] [PubMed]
- Bengtsson, M.; Wall, G.; Larsson, P.; Becktor, J.P.; Rasmusson, L. Treatment outcomes and patient-reported quality of life after orthognathic surgery with computer-assisted 2- or 3-dimensional planning: A randomized double-blind active-controlled clinical trial. Am. J. Orthod. Dentofac. Northop 2018, 153, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Hanafy, M.; Akoush, Y.; Abou-ElFetouh, A.; Mounir, R.M. Precision of orthognathic digital plan transfer using patient-specific cutting guides and osteosynthesis versus mixed analogue-digitally planned surgery: A randomized controlled clinical trial. Int. J. Oral Maxillofac. Surg. 2020, 49, 62–68. [Google Scholar] [CrossRef]
- Schneider, D.; Kämmerer, P.W.; Hennig, M.; Schön, G.; Thiem, D.G.E.; Bschorer, R. Customized in bimaxillary orthognathic surgery: A prospective randomized trial. Clin. Oral Investig. 2019, 23, 3115–3122. [Google Scholar] [CrossRef]
- Zoabi, A.; Redenski, I.; Oren, D.; Kasem, A.; Zigron, A.; Daoud, S.; Moskovich, L.; Kablan, F.; Srouji, S. 3D Printing and Virtual Surgical Planning in Oral and Maxillofacial Surgery. J. Clin. Med. 2022, 11, 2385. [Google Scholar] [CrossRef] [PubMed]
- KLS Martin. Available online: https://www.klsmartin.com/mediathek/90-242-02-10_Individual_Patient_Solutions_IPS_Implants.pdf (accessed on 5 June 2024).
- Liebregts, J.; Baan, F.; de Koning, M.; Ongkosuwito, E.; Berge, S.; Maal, T.; Xi, T. Achievability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2017, 7, 9314. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.C.; Hohlweg-Majert, B.; Schwarz, U.; Teschner, M.; Hammer, B.; Schmelzeisen, R. Manufacturing splints for orthognathic surgery using a three-dimensional printer. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 105, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, Y.; Kim, S.Y.; Kim, H.J.; Jung, Y.S.; Jung, H.D. Accuracy of modified CAD/CAM generated wafer for orthognathic surgery. PLoS ONE 2019, 14, e0216945. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, E.; Sun, Y.; Jacobs, R.; Politis, C. Three-dimensional printed final occlusal splint for orthognathic surgery: Design and validation. Int. J. Oral Maxillofac. Surg. 2017, 46, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alfaro, F.; Guijarro-Martínez, R. New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study. Int. J. Oral Maxillofac. Surg. 2013, 42, 1547–1556. [Google Scholar] [CrossRef]
- Accuracy and Precision in Measurement Systems—Minitab. Available online: https://support.minitab.com/en-us/minitab/help-and-how-to/quality-and-process-improvement/measurement-system-analysis/supporting-topics/basics/accuracy-and-precision/#:~:text=Not%20accurate%20or%20precise,two%20components%3A%20repeatability%20and%20reproducibility (accessed on 5 June 2024).
- Model Orientation Best Practices for SLA Printing: Tilting a Flat Surface. Available online: https://support.formlabs.com/s/article/Model-Orientation?language=en_US#angle-flat-surfaces (accessed on 20 June 2024).
- Loflin, W.A.; English, J.D.; Borders, C.; Harris, L.M.; Moon, A.; Holland, J.N.; Kasper, F.K. Effect of print layer height on the assessment of 3D-printed models. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 283–289. [Google Scholar] [CrossRef] [PubMed]
- ElShebiny, T.; Matthaios, S.; Menezes, L.M.; Tsolakis, I.A.; Palomo, J.M. Effect of printing technology, layer height, and orientation on assessment of 3D-printed models. J. World Fed. Orthod. 2024; in press. [Google Scholar] [CrossRef]
- Doh, R.-M.; Kim, J.-E.; Nam, N.-E.; Shin, S.-H.; Lim, J.-H.; Shim, J.-S. Evaluation of Dimensional Changes during Postcuring of a Three-Dimensionally Printed Denture Base According to the Curing Time and the Time of Removal of the Support Structure: An In Vitro Study. Appl. Sci. 2021, 11, 10000. [Google Scholar] [CrossRef]
- Mayer, J.; Reymus, M.; Mayinger, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D printed fixed dental prosthesis materials: Impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. 2021, 34, 784–795. [Google Scholar] [CrossRef]
- Boyer, R.A.; Kasper, F.K.; English, J.D.; Jacob, H.B. Effect of print orientation on the dimensional accuracy of orthodontic aligners printed 3-dimensionally. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Camardella, L.T.; de Vasconcellos Vilella, O.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Lee, S.Y.; Gu, H.; Jin, G.; Kim, J.E. Evaluating oxygen shielding effect using glycerin or vacuum with varying temperature on 3D printed photopolymer in post-polymerization. J. Mech. Behav. Biomed. Mater. 2022, 130, 105170. [Google Scholar] [CrossRef] [PubMed]
- Šimunović, L.; Jurela, A.; Sudarević, K.; Bačić, I.; Haramina, T.; Meštrović, S. Influence of Post-Processing on the Degree of Conversion and Mechanical Properties of 3D-Printed Polyurethane Aligners. Polymers 2023, 16, 17. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).