1. Introduction
Breast lesions classified as lesions of uncertain malignant potential (B3) represent a heterogeneous group of breast abnormalities with a borderline histological spectrum and an increased risk of associated malignancy. In particular, an overall risk for malignancy of 9.9–35.1% after total resection has been estimated [
1]. This B3 group includes various entities such as atypical ductal hyperplasia (ADH), flat epithelial atypia (FEA), classical lobular neoplasia (LN), papillary lesions (PLs), benign phyllodes tumors (PTs) and radial scars (RSs) [
2]. The incidence of B3 lesions varies from 3% up to 17% depending on the setting of breast cancer screening used to detect the lesions [
3,
4]. In the past, open surgical excision has been considered to be the best treatment for all B3 lesions; however, a more conservative management is now preferred for some of these lesions. In fact, over the last decade, some studies have demonstrated that a percutaneous excision using a vacuum-assisted device can remove a large volume of tissue with the same accuracy as open surgery [
5], but with more benefits for patients and reduced costs. Open surgery must be considered for selected high-risk patients [
6]. According to the recommendations from the “Second International Consensus Conference on B3 lesions” that was held in Zurich (Switzerland) in 2018, surgical treatment is strongly recommended in the case of ADH [
2].
There is no consensus on the management of B3 lesions in mutation carrier patients.
Genetic susceptibility explains about 5–10% of all breast cancer cases [
7]. These genes can be divided into three different groups according to their frequency and conferred risk: high-risk (BRCA1, BRCA2, TP53, STIK11, PTEN, CDH1), moderate-risk (ATM, CHEK2, PALB2, BRIP1) and low-risk (RAD51C, RAD51D, Mitochondrial DNA) variants. The most common genes involved in the hereditary predisposition of breast cancer are BRCA1 (BReast CAncer gene one) and BRCA2 (BReast CAncer gene two) [
8,
9]. BRCA1 is located on chromosome 17 while BRCA2 is located on chromosome 13 [
10].
To the best of our knowledge, this is the first study evaluating the incidence, radiological features and clinical impact of B3 lesions in patients with genetic mutations. Thus, the aim of our study is to evaluate the radiological features of B3 lesions in patients with genetic mutations to establish an anatomo-radiological correlation that is potentially useful to guide the therapeutic approach in this specific subgroup of patients.
2. Materials & Methods
The study was performed in accordance with the Declaration of Helsinki and it was approved by the Institutional Review Board of the University Hospital of Campus Bio-Medico in Rome (Code: 90/21 OSS). All patients signed a consent form to use their clinical and imaging data for research purposes.
2.1. Patients
We retrospectively enrolled 227 women with a histological diagnosis at breast biopsy of B3 lesions at the Breast Unit of our Institute, Campus Bio-Medico of Rome, from 2010 to 2021. Among these patients, we identified 21 women with genetic test positivity for high and intermediate penetrance genes associated with breast cancer (BRCA1, BRCA2, and ATM). Buccal swabs or peripheral blood sample from these patients were used for genetic tests using automated DNA extraction and amplification by PCR. The nomenclature used for the sequence variants was established according to the HGVS (Human Genome Variation Society) guidelines (
http://www.varnomen.hgvs.org/), while the interpretation of the clinical significance was in accordance with the pathology reference databases—BRCAExchange (
www.brcaexchange.org), LOVD (
https://www.lovd.nl), and ClinVar (
www.ncbi.nlm.nih.gov/clinvar/)—and with the classification criteria of the ENIGMA consortium (
https://enigmaconsortium.org) all accessed on 10 April 2023.
2.2. Imaging Analysis
For each patient, mammography, breast ultrasound and MRI were performed.
Mammographic images were obtained in two standard planes [cranio-caudal (CC) and medio-lateral oblique (MLO)] using a full-field digital mammography system MAMMOMAT Inspiration (Siemens Healthcare, Siemens, Erlangen, Germany). In 2019, a single MLO projection by means of a digital breast tomosynthesis system (DBT) was added. Breast sonography was performed using an ultrasound system (PHILIPS HD11 XE) equipped with a linear array L11-5 (5–12 MHz). The MR images were acquired on a 1.5 T system (Siemens Avanto, version Syngo MR B19 and Siemens Aera, version syngo MR E11) using dedicated 4-channel phased array breast coils. The patients were examined in the prone position. Images were acquired using the following pulse sequences on axial planes: T2 short tau inversion recovery, STIR (repetition time, 6210 ms; echo time, 41 ms; slice thickness, 3 mm; field of view, 400 × 362 mm; matrix, 384 × 313 pixels; duration, 2:49 min), T1 flash 3D (repetition time, 7.59 ms; echo time, 4.76 ms; slice thickness, 1.5 mm; field of view, 400 × 334 mm; matrix, 416 × 313 pixels; duration, 1:06 min), T1 flash 3D spectral adiabatic inversion recovery, and SPAIR (repetition time, 4.96 ms; echo time, 2.39 ms; slice thickness, 1.5 mm; field of view, 400 × 350 mm; matrix, 384 × 319 pixels; duration, 0:58 min), obtained before and five times after an intravenous bolus injection of a 0.15 mL/kg body weight dose of paramagnetic contrast medium (gadoteric acid 0.5 mmol/mL) at a rate of 3 mL/s. The imaging protocol included diffusion images with a b-value of 500–1000 s/mm2 (repetition time, 7400 ms; echo time, 66 ms; slice thickness, 3 mm; field of view, 380 × 213 mm; matrix, 164 × 92 pixels; duration, 3:42 min) and apparent diffusion coefficient (ADC) maps. In addition, T1 flash 3D on sagittal planes was performed (repetition time, 4.89 ms; echo time, 1.54 ms; slice thickness, 2 mm; field of view, 280 × 236 mm; matrix, 480 × 365 pixels; duration, 1:51 min). All exams were analyzed by two radiologists experienced in interpreting breast imaging.
Mammographic, sonographic and MRI studies were evaluated according to the 5th edition of BI-RADS lexicon. In particular, in the mammography analysis we evaluated: the presence of a mass and its characteristics such as shape (round, oval or irregular), dimensions (<1 cm and ≥1 cm) and margins (regular or irregular), the presence of microcalcifications and their morphology and distribution, and the presence of any architectural distortion. At the ultrasound exam, we reported the presence of a mass and its features (i.e., shape, dimensions and margins) and echo pattern (anechoic, hyperechoic, complex cystic and solid, hypoechoic, isoechoic or heterogeneous).
The features reported in MRI were the “background parenchymal enhancement” (minimal, mild, moderate or marked) and its distribution (symmetric or asymmetric), the presence of a mass enhancement (with its shape, dimensions, margins and pattern of enhancement according to intensity/time curves of type I, II and III) or a non-mass enhancement (focal, linear, segmental, regional, multiple regions or diffuse).
All these radiological features were reported for each patient and a correlation between these characteristics, the type of genetic mutation, the type of B3 lesions identified at breast biopsy (both core needle biopsy and VAB) and the definitive histological diagnosis was performed.
2.3. Statistical Analysis
Statistical analysis was performed using the chi-squared or Fisher’s exact tests to test for stochastic independency. Correlation of the different variables (patient age, risk anamnesis, lesion size, lesion morphology and histology) with the malignancy rate was determined using a cross table with calculations of the 95% confidence intervals. A correlation was considered significant if p ≤ 0.05. The analyses were performed using a statistical program (SPSS 27.0; SPSS, Chicago, IL, USA).
3. Results
The median age was 55.8 years (range 45–72 years). Out of 21 breast lesions classified as B3 at breast biopsy, 9 (42.8%) were diagnosed as ADH, 6 (28.6%) as LN (3 as atypical lobular neoplasias and 3 lobular carcinomas in situ), 3 (14.3%) as FEA, and 3 (14.3%) as RSs.
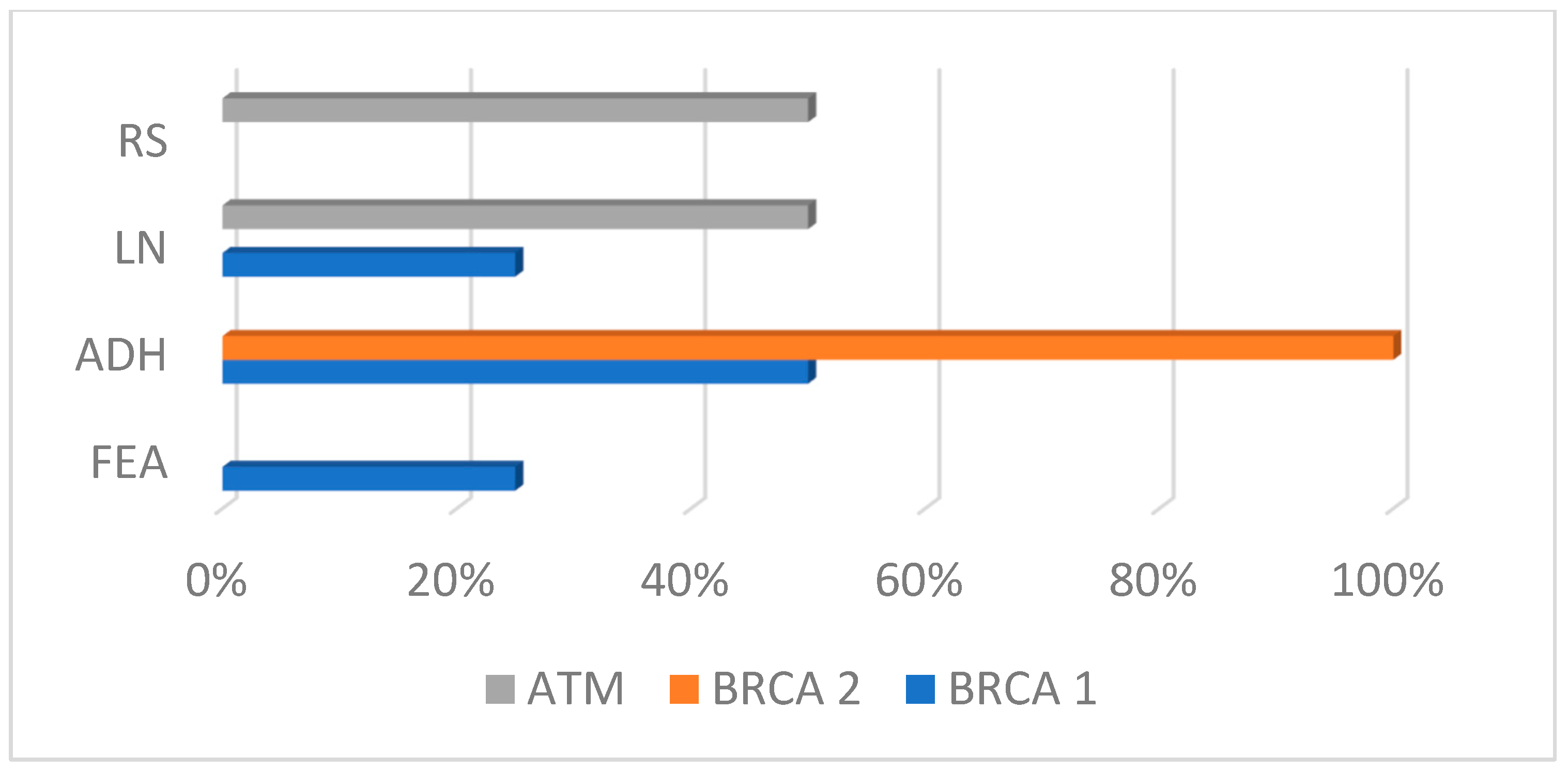
In the ATM group, 50% of lesions were LN and 50% RS; in the BRCA1 group, 25% were FEA, 50% ADH and 25% LN; and in the BRCA2 group, 100% were ADH (
Scheme 1).
The results showed a statistically significant difference between the B3 lesion distributions in the three subgroups of mutations (p = 0.011).
The median lesion size was 15.4 mm (range 5–22 mm).
Out of the 21 surgically excised lesions, the final histopathologic diagnosis showed malignant tumors in 15 lesions: 5 DCISs (2 FEA, 3ADHs), 7 ductal invasive carcinomas (1 RS, 1 FEA, 3 ADHs, 2 LNs), and 3 invasive lobular carcinomas (3 LNs). The underestimation rate of malignancy at breast biopsy based on the total number of lesions at the final follow-up was 71% (15/21) (
Table 1).
The remaining 6 lesions turned out to be B3 at the final histology analysis (2 RS, 3 ADHs and 1 LN), and were followed up by means of mammography and US after 6 months and by MRI at 1 year and every year thereafter.
LNs and FEA showed the higher malignancy correlations, with a PPV of 83% and 100%, respectively; ADHs and RSs had a PPV of 66.7% and 33.3%, respectively.
In the ATM group, 50% (3/6) of lesions turned out to be malignant; in the BRCA1 group, 83.3% of the lesions were found to be malignant (10/12); and in the BRCA2 group, 33.3% (1/3) were malignant. No statistically significant difference was found between the mutation group subtype and the histological results.
Considering the risk anamnesis of the patients, in two patients (9.5%) with recently diagnosed carcinomas in the contralateral breast, the suspicious B3 lesion turned out to be malignant. In 42.8% of the patients with a history of breast cancer and in 9.5% of patients without history of breast cancer the outcome was malignant. Risk anamnesis was a factor that significant influenced the malignancy rate (
p = 0.038) (
Scheme 2).
The patients were divided into two subgroups based on their age: patients between 45 and 55 years (12/21) and patients > 55 years (9/21). The first group (45–55 years) was found to have the worst outcome: 11 out of 21 B3 lesions were malignant (52.4%). In the group > 55 years, 19% of the lesions had a malignant final histology (4/21) (
Table 2).
The patient’s age was a significant factor influencing the malignancy rate (p = 0.03).
Imaging Findings
By mammography, 19/21 (90.5%) lesions were detected; 12 (63%) in the BRCA1 group, 2 (10.5%) in the BRCA2 group and 5 (26.3%) in the ATM group. Two cases, one was a BRCA2 mutation carrier and the other was a ATM mutation carrier, were negative at mammography.
In the BRCA1 group, 10 of the 12 detected lesions (83.3%) appeared as microcalcifications, and 2 (16.7%) as a mass. In the BRCA2 group, 100% of lesions appeared as a mass.
In the ATM group 1, 20% of lesions appeared as a distortion, and 4 (80%) as a mass (
Table 3,
Scheme 3).
The Fisher’s exact test showed a statistically significant difference between the mammographic appearance of B3 lesions in the three groups (p = 0.03). No significant difference was found between the microcalcification morphologies in the three subgroups (p = 0.821)
ADHs, FEA and LNs were more frequently associated with the presence of microcalcifications, with values of 15.8% and 10.5%, respectively. RSs appear as a mass, mass + microcalcification and distortion + microcalcifications with the same frequencies (5.3%). No significative difference was found between mammographic features and the histological results of the preoperative breast biopsy (p = 0.86).
By ultrasound, 13/21 (61.9%) lesions were detected. In the BRCA1 group, 7 lesions (58%) were not detectable; in the BRCA2 group, 2/3 (66.7%) lesions were recognizable; and in the ATM group, in all cases a typical finding was recognizable. The most frequent finding was a hypoechoic lesion with an irregular shape, non-circumscribed margins, and a parallel orientation in each group.
In 7/9 cases (77.8%) of ADH at core biopsy sampling, any finding was discovered using ultrasound, while the remaining 2 cases appeared as irregular and hypoechoic masses.
LNs and RSs were frequently associated with a single mass with posterior acoustic enhancement at ultrasound, with values of 83.3% and 100%, respectively. One case of FEA was discovered by US, appearing as an irregular nodule with obscured margins.
By breast MRI, 2 of 12 (16.7 %) BRCA1 and 2 of 6 (33.3 %) ATM lesions exhibited negative findings. Moreover, 10/12 (83.3%) BRCA1, 3/3 (100%) BRCA2 and 4/6 (66.7%) ATM lesions were detected via breast MRI. In the BRCA1 group, six (60%) and four (40%) lesions were mass and non-mass lesions, respectively; in the BRCA2 group, two lesions were mass (66.7%) and one (33.3%) non-mass lesions, whereas in the ATM group, three (75%) and one (25%) were mass and non-mass lesions, respectively (
Table 4).
By analyzing the MRI features among the different B3 lesions groups, ADHs appeared more often as a mass lesion, LNs and FEA were associated with mass and non-mass enhancements in the same way, while only a single case of an RS lesion exhibited MRI positive findings with a mass-enhancing lesion with spiculated margins, inhomogeneous contrast enhancement and a positive DWI (
Scheme 4).
No significant difference was observed in the ratio of mass to non-mass lesions among the groups (p = 0.917). For mass lesions, the main features observed in the BRCA1 and ATM groups included an irregular shape; BRCA1 carriers tended to exhibit a more circumscribed margin in comparison with the ATM group, without showing a significant difference (p = 0.427). For non-mass lesions, a segmental distribution and clumped enhancement were the dominant MRI features observed in the groups; no significant difference was observed between the groups.
As for as the kinetic curves, all eight cases (100%) of ADH detected via breast MRI showed a high enhancing curve (type 2–3), as well as the 83.3% of LN lesions and the single RS being recognized by MRI. The two FEA findings showed a type 1 and type 2 curve, respectively. A significant difference was found in regard to the kinetic curves of the B3 lesions (p = 0.009).
By comparing the MRI findings with the final post-operative histological examination, the DWI of the lesions, the mass to non-mass enhancement and MRI margins were significantly correlated with the risk of carcinoma, with a p values of 0.028, 0.034 and 0.002, respectively.
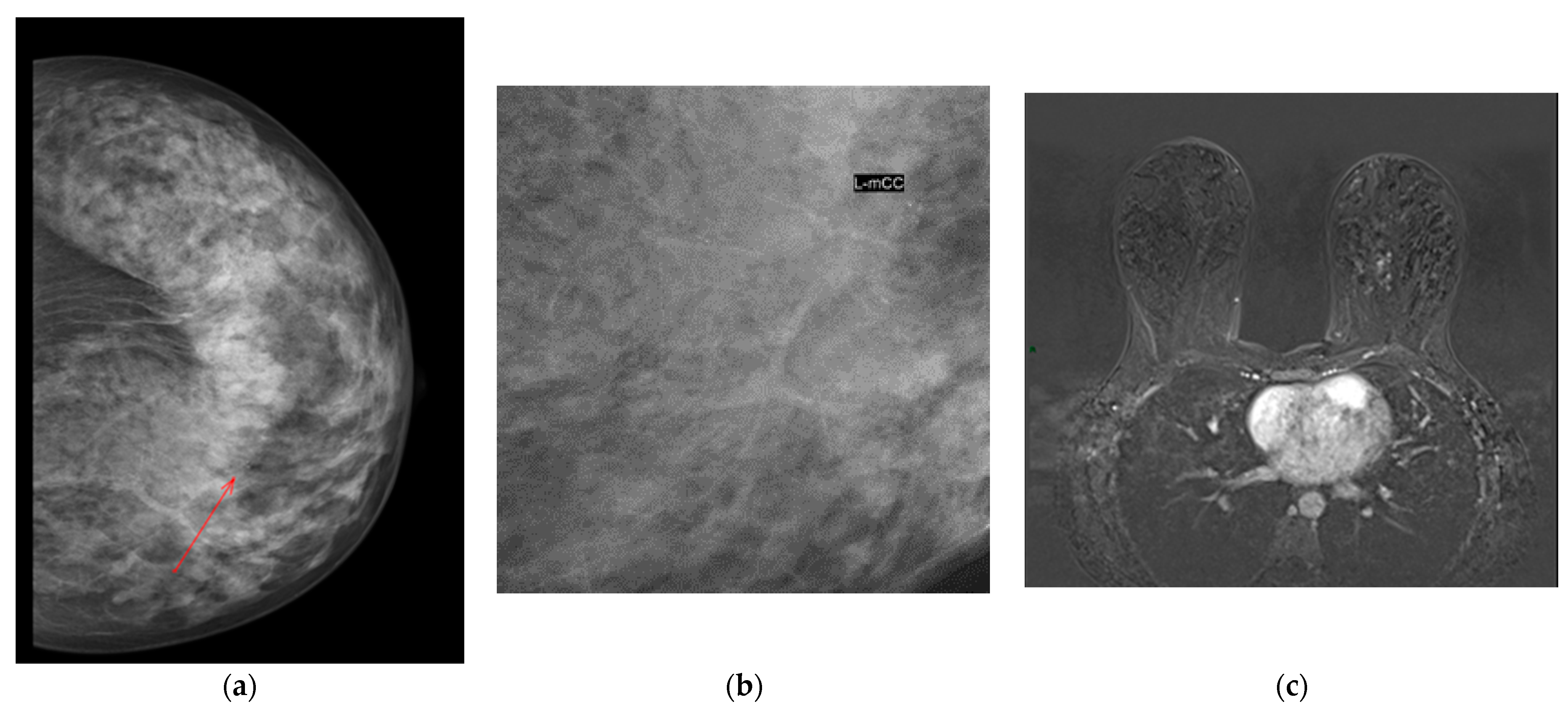
Figure 1 shows an example of an ADH with mammographic evidence of a cluster of pleomorphic calcifications in the internal quadrants of the left breast and an NME on MRI.
4. Discussion
B3 lesions comprise a wide range of findings considered non-obligate precursors of breast cancer; some of these lesions can evolve into DCIS or low-grade invasive tumors after surgical excision with an overall risk of malignancy of 10–35%.
Their management varies greatly from country to country and from hospital to hospital although, currently, there is a trend toward a more conservative management instead of open surgery, such as vacuum-assisted excision [
11].
BRCA1 and BRCA2 are the most common genetic mutations responsible for breast and ovarian cancer development. These patients have a 3% greater risk of developing breast cancer before the age of 30, and the risk over their lifetime increases to 50–80% by 70 years of age. In particular, some meta-analyses reported a breast cancer risk of 55–70% for BRCA1 carriers and 40–70% for BRCA2 carriers [
12,
13,
14]. The natural history of ATM-related breast cancer is not well defined, although some studies report their tendency to be more aggressive, dedifferentiated and endocrine-positive with respect to the sporadic ones, and with a poor prognosis. Moreover, this mutation is also a contraindication for radiation therapy because it increases radiotherapy toxicity and the risk of developing a second tumor after RT [
15].
To our knowledge, this is the first study evaluating the relationship between the type of mutation and the imaging and pathological findings of B3 lesions.
Our results indicated that ADHs were the most commonly encountered lesion after breast biopsy (42.8%), followed by LNs (28.6%), FEA and RSs (14.3% for both). Their distribution among the three groups of mutations showed a significant difference, with a higher prevalence of ADH in the BRCA1 group.
LNs and FEA showed a higher malignancy correlation, with a PPV of 83% and 100%, respectively; these results are quite different from those observed in general populations, showing a PPV of about 8–60% for LN and 13–67% for FEA [
16]. These results highlight that in mutation carriers, these lesions should always be surgically excised.
ADHs and RSs had a PPV of 66.7% and 33.3%, respectively. The PPV in the general population for ADH is about 60%, quite similar to our results, but still high enough to require surgical excision. The data regarding RSs were higher than that observed in non-mutation carrier patients (between 1.1 and 7%) [
16,
17]. This fact led to open excision in all the cases, although the natural history of this finding is that of a benign lesions requiring therapeutic excision with VAE for those lesions visible at imaging, according to the second International Consensus Conference on B3 lesions, which indicates surgery only in presence of RSs associated with atypia. Nevertheless, our results were still too high to recommend VAE only.
According to the malignancy rate in the three groups of mutations, there was no significant difference among them, although we observed that the majority of patients in the BRCA1 group developed a tumor.
Patient age was a significant factor influencing the malignancy rate, with patients between 45 and 55 years having the worst outcome, with 52.4% developing a breast cancer after surgical excision.
In the current study, the most common mammographic presentation of B3 lesions was microcalcification (36.8%) followed by distortion + microcalcification (15.8%), findings which were more representative in the BRCA1 group, with a significant difference with respect to the other groups. In particular, microcalcifications were more often associated with ADH, FEA and LN, and they were rare in radial scars.
Some studies demonstrated that when calcification was the main radiological abnormality, the lesion diagnosed on breast biopsy was frequently epithelial or lobular neoplasia. Moreover, where microcalcifications were the main radiological abnormality, it was more likely to be associated with malignancy at surgery in 77.8% of the cases, compared to mass lesions or architectural distortions. This result is in line with the current literature in the general population [
18,
19].
These findings enhance the fact that some radiological features help in deciding further management after a B3 needle core biopsy diagnosis in mutation carrier patients.
Parenchymal distortion was present in 28% of lesions, and was more often associated with ADHs and RSs. Among them, 66.7% were upgraded to cancer (three ADHs and one RS), and more specifically, three were BRCA1 mutation carriers and one ATM. BRCA1 mutation carrier patients were most often correlated with cancer evolution by histology.
The ultrasound detected 13/21 lesions. The most common finding of the BRCA1, BRCA2 and ATM groups included hypoechoic masses with an irregular shape, parallel orientation and non-circumscribed margins. These results are in line with the study of Min Ha et al., who described 95 of 99 (96.0%) BRCA1 and 102 of 103 (99.0%) BRCA2 lesions detected at sonography as characterized by hypoechoic lesions with an irregular shape, non-circumscribed margins and a parallel orientation in both groups. In their series, the authors described a higher frequency of posterior acoustic enhancements in the BRCA1 group, a finding not encountered in our sample, as the majority of B3 lesions identified by US were LNs and RSs, with one case of FEA and two cases of ADH only, which did not demonstrate a posterior acoustic shadowing.
According to MRI, there was no significant difference between the three groups in the proportion of mass versus non-mass lesions, mass shapes and non-mass features. In the BRCA1 group, mass lesions tended to exhibit more circumscribed margins compared to the BRCA2 and ATM groups, but without evidence of a significant difference. Additionally, in the study by Min Ha et al., BRCA1 mutation carriers tended to show more regular lesions in comparison to the BRCA2 group [
20].
In our study, the upgrade was more often associated with a mass-like lesions, with a significant correlation with the risk of malignancy; in particular, the upgrade was characterized by ADH and LN lesions. This result is in line with some previous studies in the general population, which found a significant correlation between malignancy and mass-like lesions with a lower risk in the case of non-mass-like lesions [
17,
19].
In all cases appearing as mass lesions, ADHs showed almost regular margins and a positive DWI.
When analyzing the MRI morphologic and functional features among the different B3 lesions groups and when comparing with the final post-operative histological examination, DWI and kinetic curves significantly correlated with the risk of carcinoma, suggesting that in the presence of a mass-like lesion with regular margins and mild enhancement, the functional information given by DWI and contrast enhancement can help in guiding the decision process.
Our study has several limitations. Firstly, the small sample size resulted in only a few conclusions concerning significance. Second, the retrospective study design did not allow evaluation of the variables affecting the management of every single patient. Third, the lack of some B3 findings, such as papillary lesions, prevented a comprehensive evaluation of all B3 lesions and, in the end, the patients did not perform VAE prior to surgery because of the lack of equipment at the time of the examinations.