Unsupervised Detection of Multiple Sleep Stages Using a Single FMCW Radar
Abstract
1. Introduction
2. FMCW Radar Signal Processing
3. Sleep Stage Detection
3.1. Physiological Characteristics of the Sleep Stages
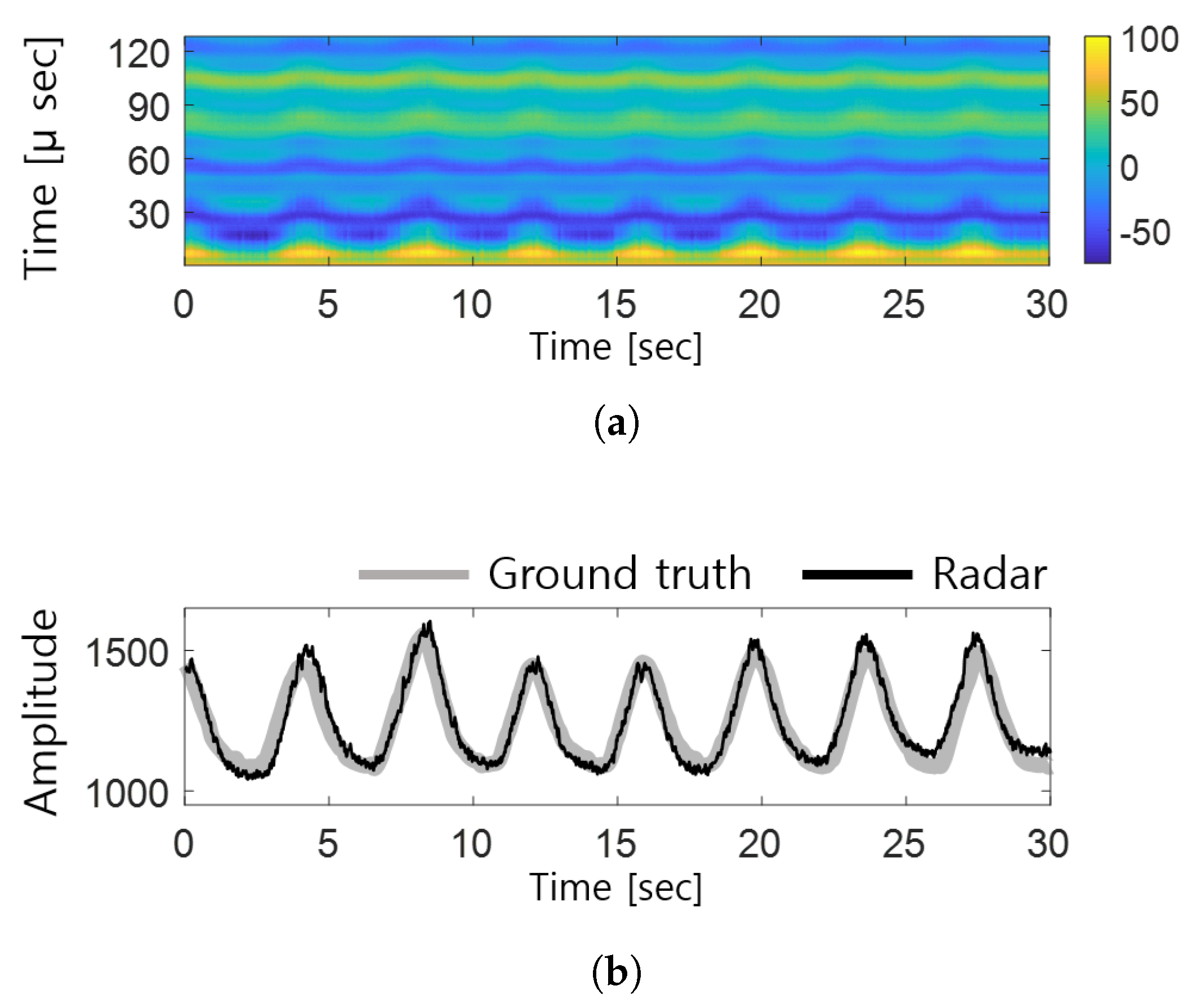
3.2. Bio-Signal Detection
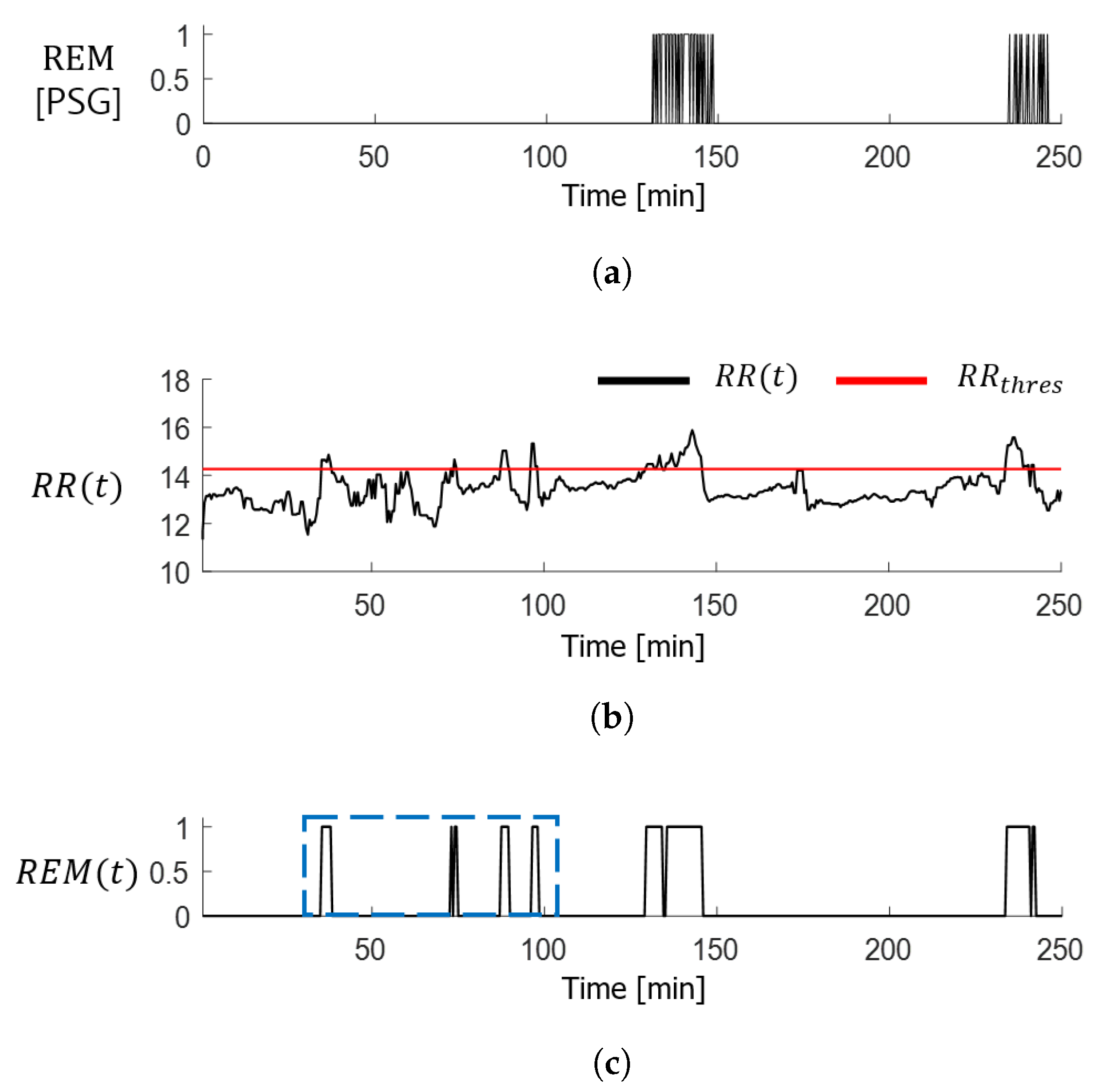
3.3. Detection of REM Sleep Stage
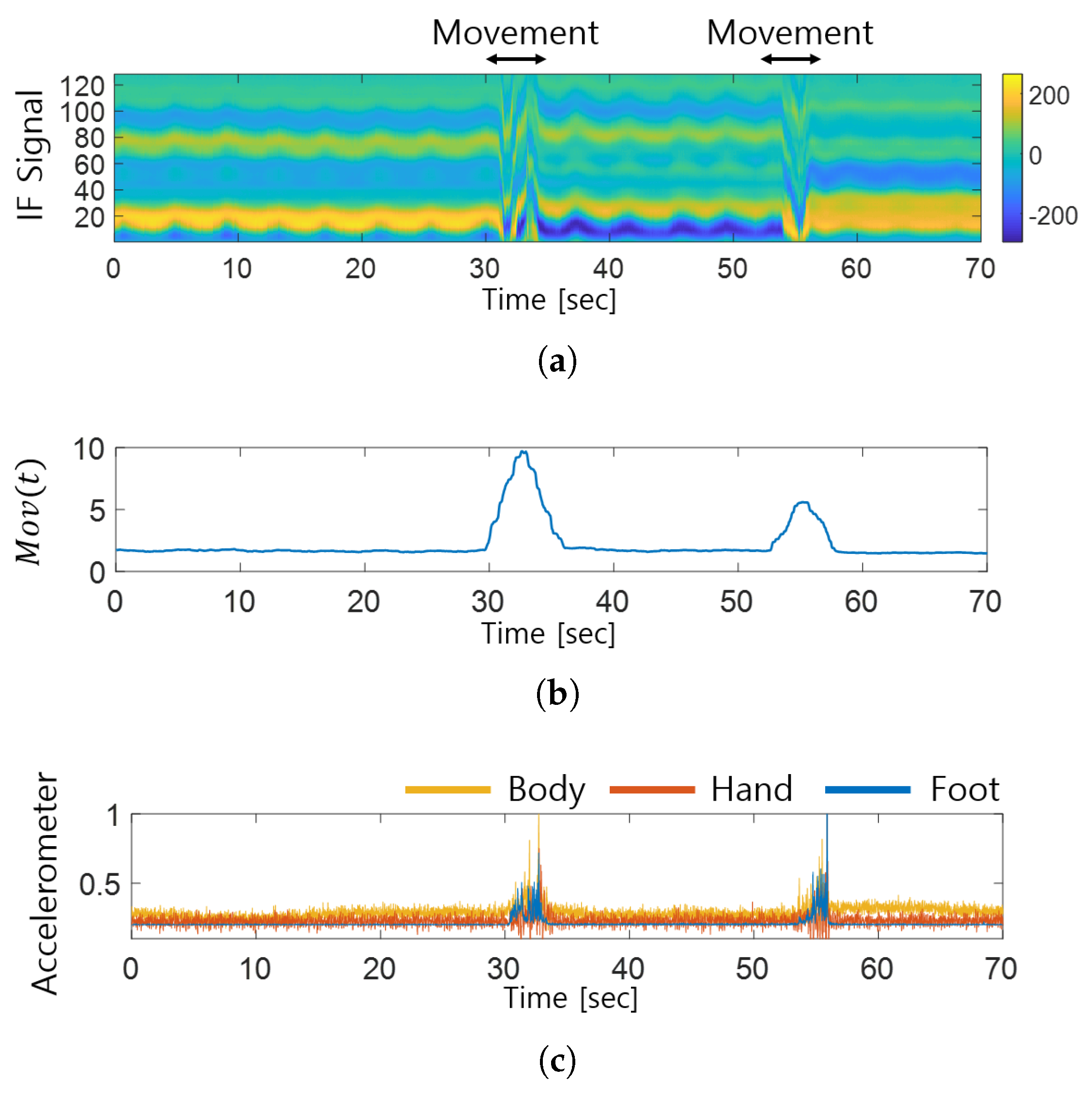
3.4. FMCW Radar-Based Movement Detection
3.5. Reducing the False Detection of REM Sleep Stage
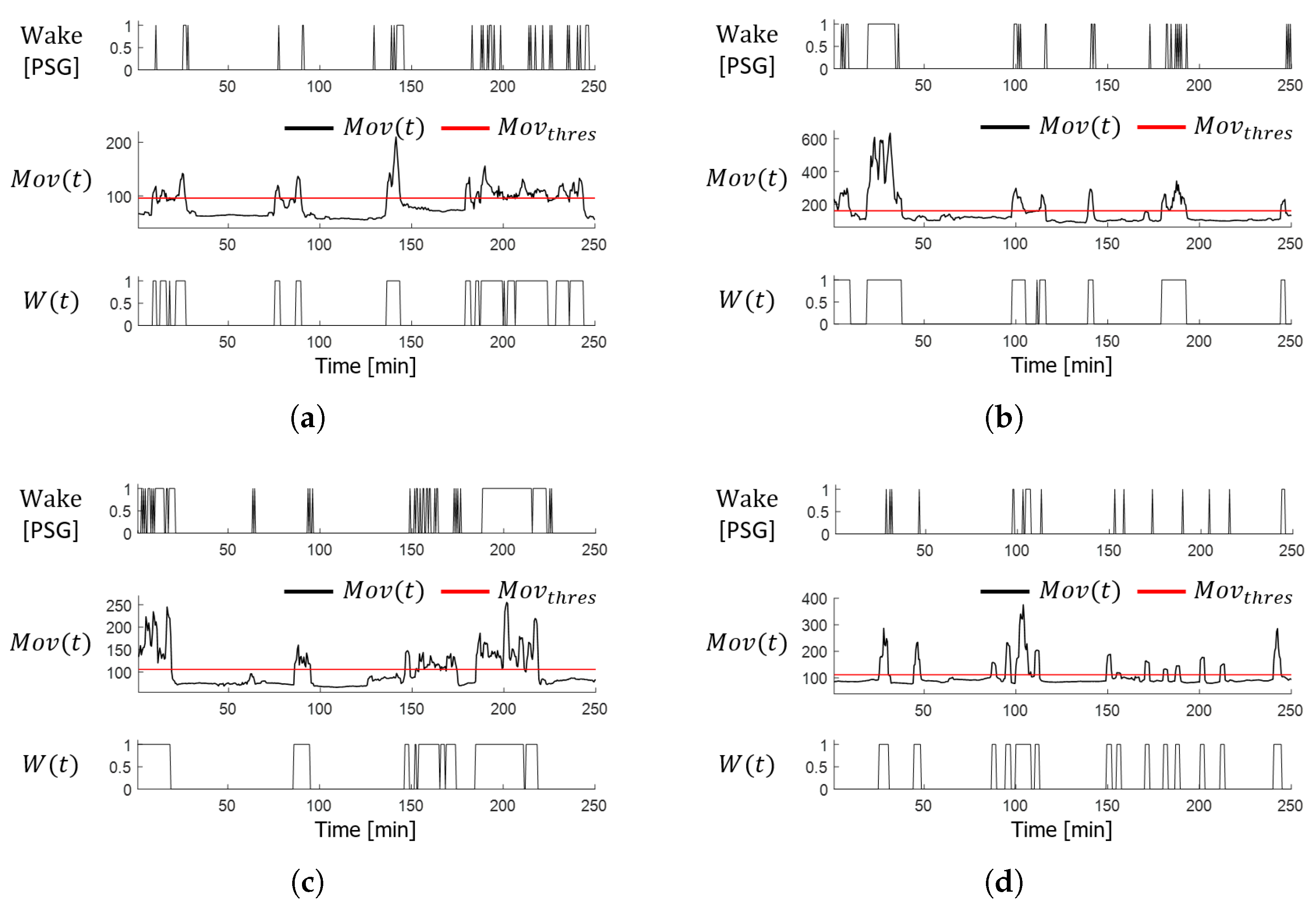
3.6. Wake State Detection
4. Experimental Results
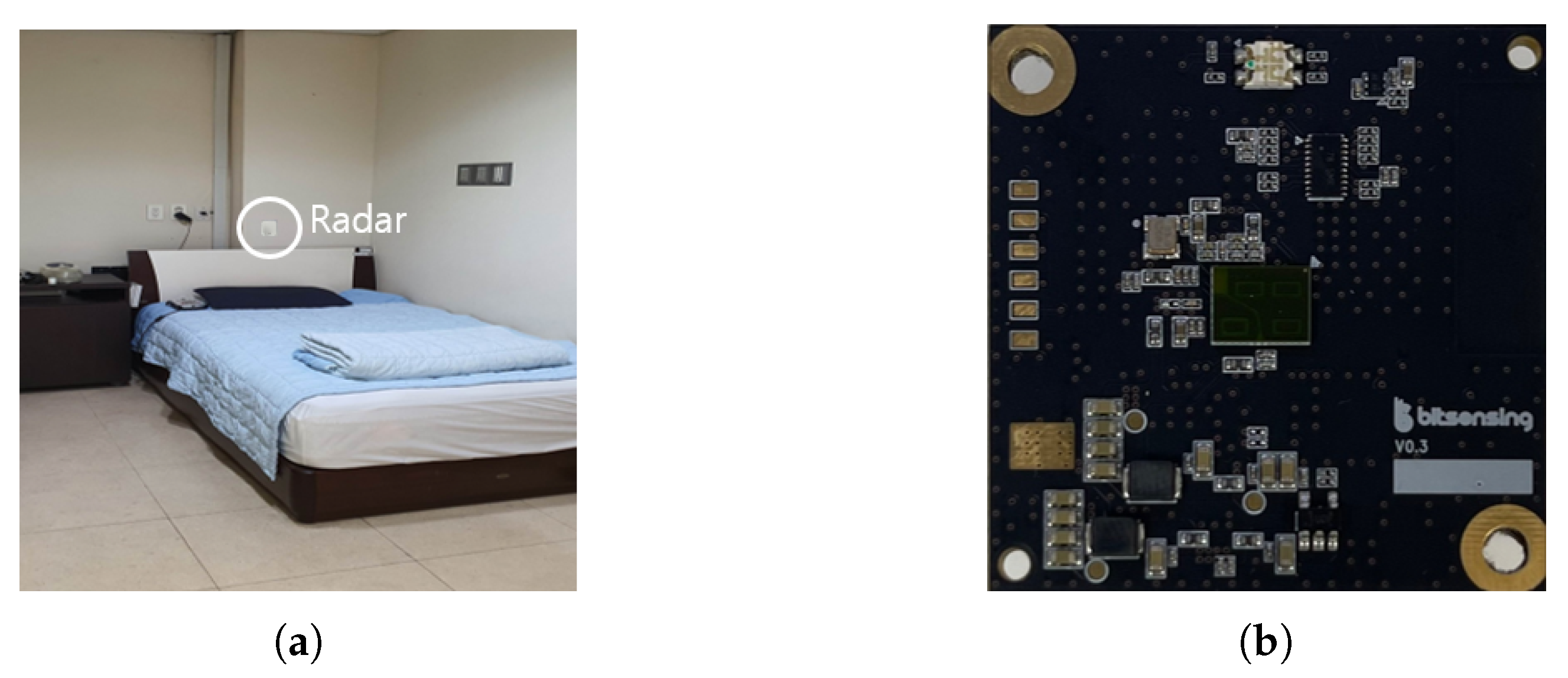
4.1. Experimental Setup
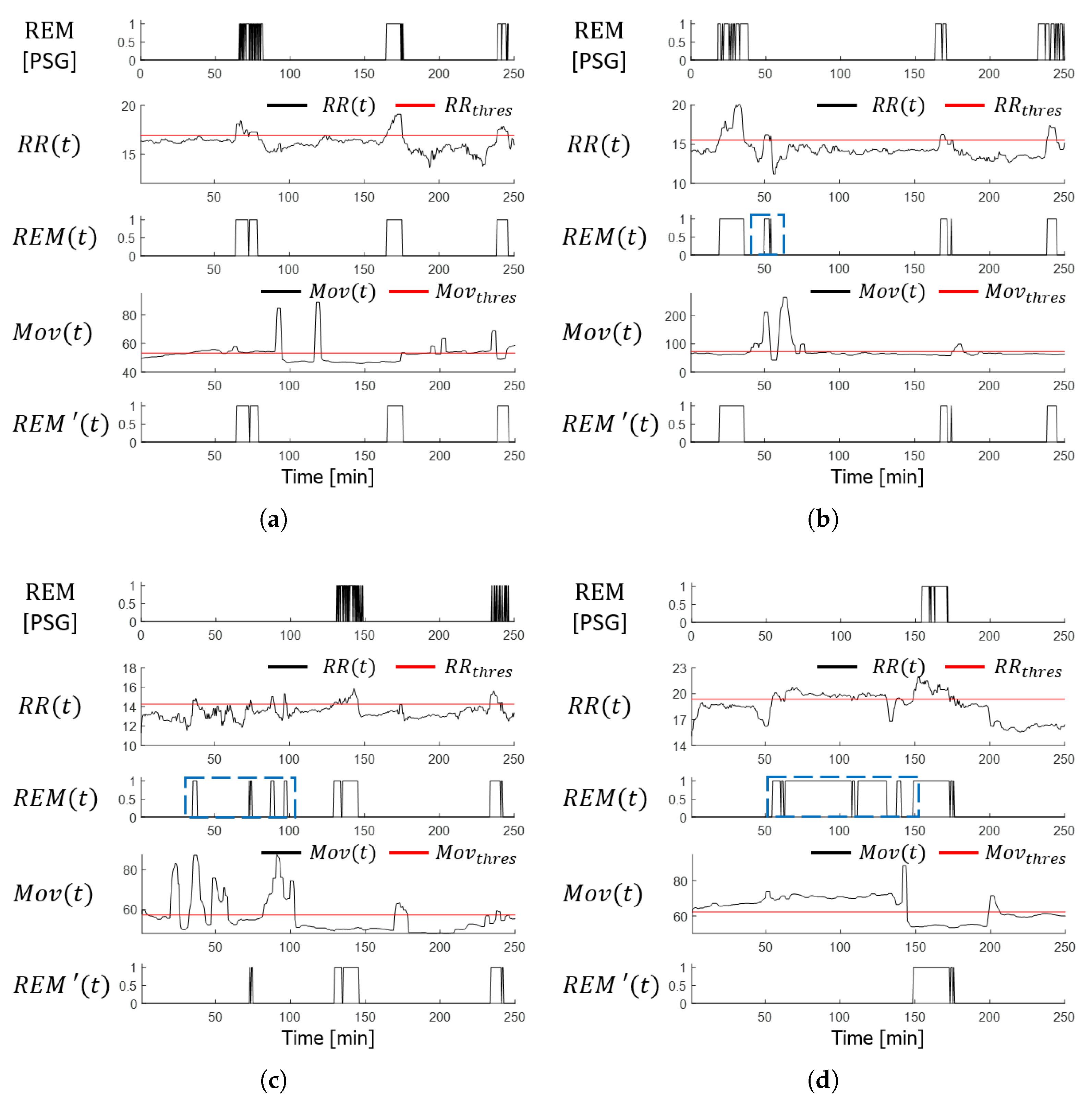
4.2. Sleep-Stage Detection Results
4.3. Accuracy Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- eMD Medical News. ‘Sleep Disorder’, Which Makes You Tired Even If You Sleep, the First Step to Overcome Disease Awareness. Available online: http://mdon.co.kr/news/article.html?no=32331 (accessed on 6 March 2023).
- HiDoc. Gaining Weight, Exploding Irritability…Seven Symptoms of a Person Who Lacks Sleep. Available online: https://www.hidoc.co.kr/healthstory/news/C0000615379 (accessed on 6 March 2023).
- Šušmáková, K. Human sleep and sleep EEG. Meas. Sci. Rev. 2004, 4, 59–74. [Google Scholar]
- Mayoclinic. Polysomnography (Sleep Study). Available online: https://www.mayoclinic.org/tests-procedures/polysomnogr-aphy/about/pac-20394877 (accessed on 6 March 2023).
- Willemen, T.; Deun, D.V.; Verhaert, V.; Vandekerckhove, M.; Exadaktylos, V.; Verbraecken, J.; Huffel, S.V.; Haex, B.; Sloten, J.V. An evaluation of cardiorespiratory and movement features with respect to sleep-stage classification. IEEE J. Biomed. Health Inform. 2013, 18, 661–669. [Google Scholar] [CrossRef]
- Wikipedia. Polysomnography. Available online: https://en.wikipedia.org/wiki/Polysomnography (accessed on 6 March 2023).
- Du, N.; Liu, K.; Ge, L.; Zhang, J. ApneaRadar: A 24 GHz radar-based contactless sleep apnea detection system. In Proceedings of the 2017 2nd International Conference on Frontiers of Sensors Technologies (ICFST), Shenzhen, China, 14–16 April 2017; pp. 372–376. [Google Scholar]
- Choi, S.H.; Yoon, H.; Kim, H.S.; Kim, H.B.; Kwon, H.B.; Oh, S.M.; Le, Y.J.; Park, K.S. Real-time apnea-hypopnea event detection during sleep by convolutional neural networks. Comput. Biol. Med. 2018, 100, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Pharvis Korea. Polysomnography, Cost-Effectiveness Well…It Is Different from Patients’ Existing Sleep Environment, and There Is a Burden of Time and Cost. Available online: http://www.medipharmhealth.co.kr/news/article.html?no=82531 (accessed on 6 March 2023).
- Kosmadopoulos, A.; Sargent, C.; Darwent, D.; Zhou, X.; Roach, G.D. Alternatives to polysomnography (PSG): A validation of wrist actigraphy and a partial-PSG system. Behav. Res. Methods 2014, 46, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Marino, M.; Li, Y.; Rueschman, M.N.; Winkelman, J.W.; Ellenbogen, J.M.; Solet, J.M.; Dulin, H.; Berkman, L.F.; Buxton, O.M. Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep 2013, 36, 1747–1755. [Google Scholar] [CrossRef]
- Pollak, C.P.; Tryon, W.W.; Nagaraja, H.; Dzwonczyk, R. How accurately does wrist actigraphy identify the states of sleep and wakefulness? Sleep 2001, 24, 957–965. [Google Scholar] [CrossRef]
- Long, X.; Otte, R.; Sanden, E.V.D.; Werth, J.; Tan, T. Video-based actigraphy for monitoring wake and sleep in healthy infants: A Laboratory Study. Sensors 2019, 19, 1075. [Google Scholar] [CrossRef]
- De Chazal, P.; Fox, N.; O’Hare, E.; Heneghan, C.; Zaffaroni, A.; Boyle, P.; Smith, S.; O’Connell, C.; McNicholas, W.T. Sleep/wake measurement using a non-contact biomotion sensor. J. Sleep Res. 2011, 20, 356–366. [Google Scholar] [CrossRef]
- Choi, B.H.; Seo, J.W.; Choi, J.M.; Shin, H.B.; Lee, J.Y.; Jeong, D.U.; Park, K.S. Non-constraining sleep/wake monitoring system using bed actigraphy. Med. Biol. Eng. Comput. 2007, 45, 107–114. [Google Scholar] [CrossRef]
- Walsh, L.; McLoone, S.; Ronda, J.; Duffy, J.F.; Czeisler, C.A. Noncontact pressure-based sleep/wake discrimination. IEEE Trans. Biomed. Eng. 2016, 64, 1750–1760. [Google Scholar] [CrossRef]
- Dafna, E.; Tarasiuk, A.; Zigel, Y. Sleep-wake evaluation from whole-night non-contact audio recordings of breathing sounds. PLoS ONE 2015, 10, e0117382. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xiong, J.; Zhao, H.; Hong, H.; Zhu, X.; Li, C. Sleep stages classification by CW Doppler radar using bagged trees algorithm. In Proceedings of the 2017 IEEE Radar Conference (RadarConf), Seattle, WA, USA, 8–12 May 2017; pp. 788–791. [Google Scholar]
- Hong, H.; Zhang, L.; Gu, C.; Li, Y.; Zhou, G.; Zhu, X. Noncontact sleep stage estimation using a CW Doppler radar. IEEE J. Emerg. Sel. Top. Circuits Syst. 2018, 8, 260–270. [Google Scholar] [CrossRef]
- Hong, H.; Zhang, L.; Zhao, H.; Chu, H.; Gu, C.; Brown, M.; Zhu, X.; Li, C. Microwave sensing and sleep: Noncontact sleep-monitoring technology with microwave biomedical radar. IEEE Microw. Mag. 2019, 20, 18–29. [Google Scholar] [CrossRef]
- Rahman, T.; Adams, A.T.; Ravichandran, R.V.; Zhang, M.; Patel, S.N.; Kientz, J.A.; Choudhury, T. Dopplesleep: A contactless unobtrusive sleep sensing system using short-range doppler radar. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp’15), Osaka, Japan, 7–11 September 2015; pp. 39–50. [Google Scholar]
- Jiang, J.; Jiang, Y.; Qiu, X.; Li, B.; Wang, P. Noncontact Sleep Stage Classification Based on Multi-sensor Feature Level Fusion. In Proceedings of the 2019 IEEE 19th International Conference on Communication Technology (ICCT), Xi’an, China, 16–19 October 2019; pp. 1453–1457. [Google Scholar]
- Kwon, H.B.; Choi, S.H.; Lee, D.; Son, D.; Yoon, H.; Lee, M.H.; Lee, Y.J.; Park, K.S. Attention-based lstm for non-contact sleep stage classification using ir-uwb radar. IEEE J. Biomed. Health Inform. 2021, 25, 3844–3853. [Google Scholar] [CrossRef]
- de Goederen, R.; Pu, S.; Viu, M.S.; Doan, D.; Overeem, S.; Serdijn, W.A.; Joosten, K.F.M.; Dudink, J. Radar-based sleep stage classification in children undergoing polysomnography: A pilot-study. Sleep Med. 2021, 82, 1–8. [Google Scholar] [CrossRef]
- Kagawa, M.; Sasaki, N.; Suzumura, K.; Matsui, T. Sleep stage classification by body movement index and respiratory interval indices using multiple radar sensors. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 7606–7609. [Google Scholar]
- Kagawa, M.; Suzumura, K.; Matsui, T. Sleep stage classification by non-contact vital signs indices using Doppler radar sensors. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 4913–4916. [Google Scholar] [CrossRef]
- Lee, W.H.; Kim, S.H.; Na, J.Y.; Lim, Y.H.; Cho, S.H.; Cho, S.H.; Park, H.K. Non-contact sleep/wake monitoring using impulse-radio ultrawideband radar in neonates. Front. Pediatr. 2021, 9, 782623. [Google Scholar] [CrossRef]
- Wang, S.; Pohl, A.; Jaeschke, T.; Czaplik, M.; Köny, M.; Leonhardt, S.; Pohl, N. A novel ultra-wideband 80 GHz FMCW radar system for contactless monitoring of vital signs. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4978–4981. [Google Scholar]
- Fonseca, P.; van Gilst, M.M.; Radha, M.; Ross, M.; Moreau, A.; Cerny, A.; Anderer, P.; Long, X.; van Dijk, J.P.; Overeem, S. Automatic sleep staging using heart rate variability, body movements, and recurrent neural networks in a sleep disordered population. Sleep 2020, 43, zsaa048. [Google Scholar] [CrossRef]
- Yoo, Y.K.; Shin, H.C. Movement Compensated Driver’s Respiratory Rate Extraction. Appl. Sci. 2022, 12, 2695. [Google Scholar] [CrossRef]
- American Academy of SLEEP MEDICINE. The AASM Manual for the Scoring of Sleep and Associated Events; AASM: Darien, CT, USA, 2020; pp. 23–31. [Google Scholar]
- Choi, H.I.; Song, W.J.; Song, H.; Shin, H.C. Selecting target range with accurate vital sign using spatial phase coherency of FMCW radar. Appl. Sci. 2021, 11, 4514. [Google Scholar] [CrossRef]
- Dugundji, J. Envelopes and pre-envelopes of real waveforms. IRE Trans. Inf. Theory 1958, 4, 53–57. [Google Scholar] [CrossRef]
- Bitsensing. Don’t Wait Let’s Predict from Sleep Scoring to Illness Prediction. Available online: https://bitsensing.com/pdf/bitsen-sing_Wellness_Sensor_mini-H_Introduction.pdf (accessed on 6 March 2023).
- Tataraidze, A.; Anishchenko, L.; Korostovtseva, L.; Kooij, B.J.; Bochkarev, M.; Sviryaev, Y. Sleep stage classification based on bioradiolocation signals. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 362–365. [Google Scholar]
- Lee, Y.J.; Lee, S.J.; Kang, D.J. Clinical and polysomnographic characteristics of REM sleep-dependent obstructive sleep apnea. Sleep Med. Psychophysiol. 2008, 15, 77–81. [Google Scholar]


| Parameters | Value |
|---|---|
| Center Frequency | 60 GHz |
| Chirp duration | 300 μs |
| Sampling Frequency | 1 MHz |
| Scan interval | 100 ms |
| Bandwidth | 3.75 GHz |
| Number of Tx antenna | 1 |
| Number of Rx antenna | 3 |
| Algorithm | Radar in Application | Evaluation Criteria | Number of Stage | Use of Learning-Based Method | Detection Accuracy [%] |
|---|---|---|---|---|---|
| [18] | CW Doppler | Accuracy | 4 | O | W/R/L/D 81.8/85.5/78.6/81.2 |
| [23] | IR UWB | Accuracy | 4 | O | Four-stage Average 82.6 |
| [20] | CW Doppler | Precision Recall F1-Score | 3 | O | W/S-(P)86.0/(R)86.5/(F)86.2 R/NR-(P)75.5/(R)75.4/(F)75.8 |
| [24] | IR UWB | Accuracy | 3 | O | Three-Stage Average 72.93 |
| [35] | Bio | Precision | 3 | O | Three-Stage Average 75.13 |
| [25] | Micro Doppler | Precision | 3 | O | Three-Stage Average 68.10 |
| [26] | Micro Doppler | Accuracy | 3 | O | Three-Stage Average 57.10 |
| [27] | IR UWB | Recall | 2 | X | Three-Stage Average 75.00 |
| Proposed | FMCW | Accuracy | 3 | X | Three-Stage Average 68.91 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, Y.-K.; Jung, C.-W.; Shin, H.-C. Unsupervised Detection of Multiple Sleep Stages Using a Single FMCW Radar. Appl. Sci. 2023, 13, 4468. https://doi.org/10.3390/app13074468
Yoo Y-K, Jung C-W, Shin H-C. Unsupervised Detection of Multiple Sleep Stages Using a Single FMCW Radar. Applied Sciences. 2023; 13(7):4468. https://doi.org/10.3390/app13074468
Chicago/Turabian StyleYoo, Young-Keun, Chae-Won Jung, and Hyun-Chool Shin. 2023. "Unsupervised Detection of Multiple Sleep Stages Using a Single FMCW Radar" Applied Sciences 13, no. 7: 4468. https://doi.org/10.3390/app13074468
APA StyleYoo, Y.-K., Jung, C.-W., & Shin, H.-C. (2023). Unsupervised Detection of Multiple Sleep Stages Using a Single FMCW Radar. Applied Sciences, 13(7), 4468. https://doi.org/10.3390/app13074468







