Abstract
Diabetic foot is a prevalent chronic complication of diabetes and increases the risk of lower limb amputation, leading to both an economic and a major societal problem. By detecting the risk of developing diabetic foot sufficiently early, it can be prevented or at least postponed. Using artificial intelligence, delayed diagnosis can be prevented, leading to more intensive preventive treatment of patients. Based on a systematic literature review, we analyzed 14 articles that included the use of artificial intelligence to predict the risk of developing diabetic foot. The articles were highly heterogeneous in terms of data use and showed varying degrees of sensitivity, specificity, and accuracy. The most used machine learning techniques were support vector machine (SVM) (n = 6) and K-Nearest Neighbor (KNN) (n = 5). Future research is recommended on larger samples of participants using different techniques to determine the most effective one.
1. Introduction
Diabetes mellitus (DM) is a chronic disease that requires constant monitoring and management, not just blood glucose control. Worldwide, around 422 million people have diabetes, most of them in low- and middle-income countries, and 1.5 million deaths a year are directly related to diabetes [1]. The disease causes several chronic complications that can have a significant impact on the quality of life of patients, burden the healthcare system through hospitalizations and contribute to an increase in mortality [2]. Many people with diabetes are expected to develop diabetic foot ulcers (DFU) [3], which causes a high rate of amputations in diabetic patients [4], usually due to poor glycemic control, underlying neuropathy, peripheral vascular disease, or poor foot care. DFU can occur at any age but are most common in diabetic patients aged 45 and over [5]. Mortality rates associated with the development of diabetic foot are estimated at 5% in the first 12 months and 42% at 5 years [6]. The annual incidence of diabetic foot ulcers worldwide is between 9.1 and 26.1 million [5,7].
The characteristics of a DFU, such as anatomical location, depth of the wound, infection, and ischemia of the foot lesion at presentation, as well as glycemic control, influence the outcome [8,9,10]. People at the highest risk of ulcers can be identified by a clinical examination of the feet [11]. Therefore, prevention strategies, including annual diabetic foot examinations, have been implemented to enable early identification of diabetic patients at high risk of diabetic foot complications [12]. Predicting who will develop an ulcer means that preventive therapies can be targeted appropriately [13]. Grading the severity of the ulcer is crucial in the care of patients with DFU and has been reported to have a greater impact on the ultimate success of treatment than the site of the ulcer [8,14].
Artificial intelligence (AI) includes a description of the use of computers and technology to simulate intelligent behavior and critical thinking [15]. Different methods cope with different and increasing amounts of health data, allowing for greater patient autonomy and personalized treatment [16]. Some research has been carried out to diagnose and predict diabetic mellitus and its complications, such as diabetic foot [17]. The automation of healthcare management has led to a transformation in the field by introduction of artificial intelligence-based solutions, due to the ease of mass data collection and powerful computational processing. It has the potential to prevent delayed diagnosis and identify preventive treatments [18]. Clinical practice can use these predictive models to better determine which high-risk people with diabetes should be monitored more closely and treated more intensively [19]. Thermography is also one of the non-invasive methods that can be used to predict risk, as temperature differences in the foot can indicate problems associated with diabetic foot [20].
The aim of this rapid review is to answer the research question: which AI techniques are most effective in predicting the risk of developing diabetic foot?
2. Materials and Methods
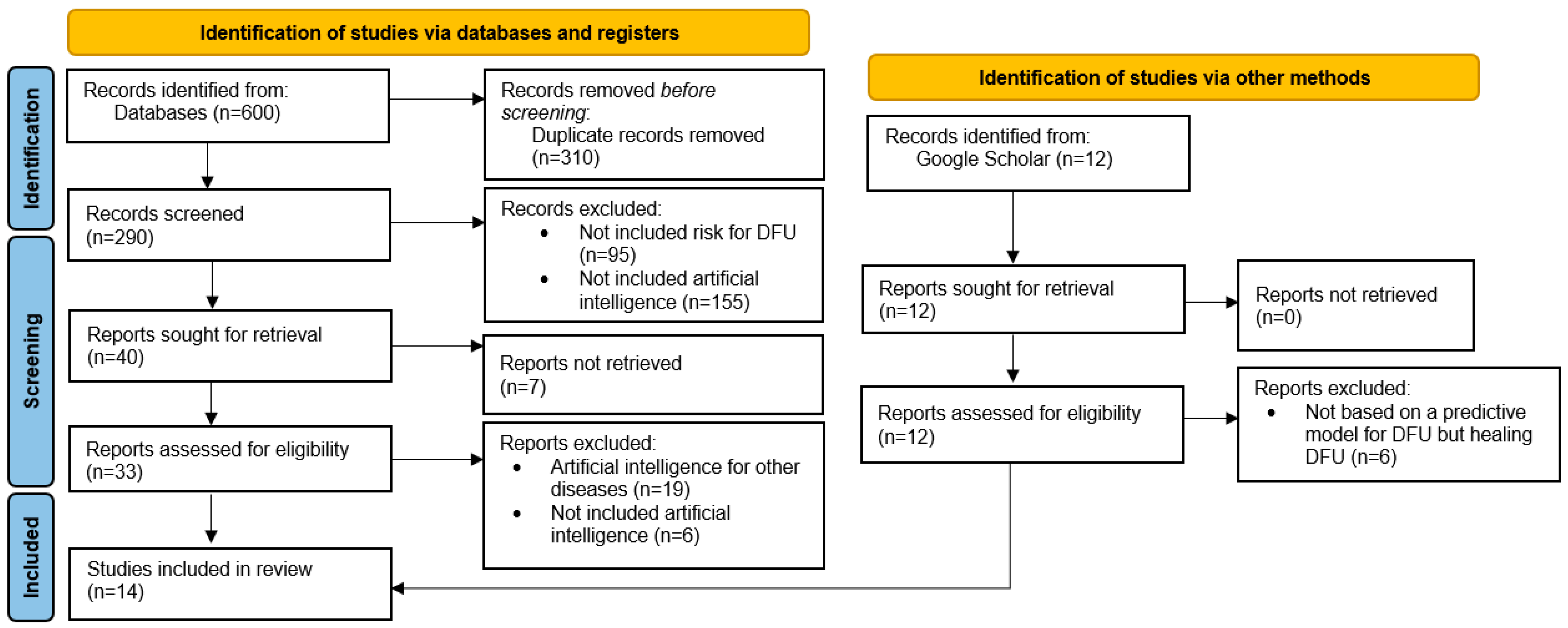
A literature review [21,22] was used to describe the current AI based approaches to diabetes and diabetic foot prediction. The first step included a review of the scientific literature on predictive models for diabetic foot ulcer risk using the keywords and synonyms diabetic foot ulcers, prediction model, and artificial intelligence. The full search string was (“diabetic foot” OR “diabetic foot ulcers”) AND (“artificial intelligence” OR AI OR “predictive models” OR “predictive modeling” OR “prediction model”). Based on the keywords and the search string, a systematic literature review was performed in the following databases: PubMed, CINAHL/MEDLINE, Web of Science, Scopus, and SAGE. We also reviewed the relevant research in Google Scholar. In the next step, two reviewers independently screened the titles and abstracts and analyzed them according to the inclusion/exclusion criteria. All types of research articles in English were included. We excluded duplicates, commentaries, books, protocols, editorials, etc. The articles that were included in the follow-up were downloaded in full and screened.
The analyzed articles were presented using a characteristics table (author, year, study aim, sample, data collection strategies, techniques, main findings, and limitations). Based on the content of the articles, we divided them into two groups: articles for predicting diabetic foot risk based on a prediction model and articles for predicting diabetic foot risk based on thermography. Based on a literature review and an analysis of articles, we have presented a graphical representation of the most frequently used AI techniques.
3. Results
Based on the search string and considering the search limitations, the following hits were extracted from the databases (Table 1): PubMed (n = 152), CINAHL/MEDLINE (n = 134), Scopus (n = 118), SAGE (n = 75), and Web of Science (n = 121).

Table 1.
Searches in the database.
After an additional Google Scholar search, we added 12 more reports. Then, we used the Rayyan, computational tool to remove duplicates (n = 310). We screened the remaining articles (n = 290) and excluded articles that were not predicted DFU, that were full-text available, were not included artificial intelligence, and papers written in other languages. Finally, 14 studies were included in the analysis (Figure 1).
Figure 1.
PRISMA flow diagram.
Table 2 presents the basic characteristics of the included studies.

Table 2.
Basic characteristics of the included studies.
Tulloch et al., in 2020 [29], reviewed articles that addressed the topic of prevention, diagnostician, and treatment of DFU using ML alone. In the case of our review, we did not limit ourselves to these models. We included seven articles that included variable-based prediction of DFU risk and a prediction model, and seven articles that addressed the possibility of DFU based on thermal images.
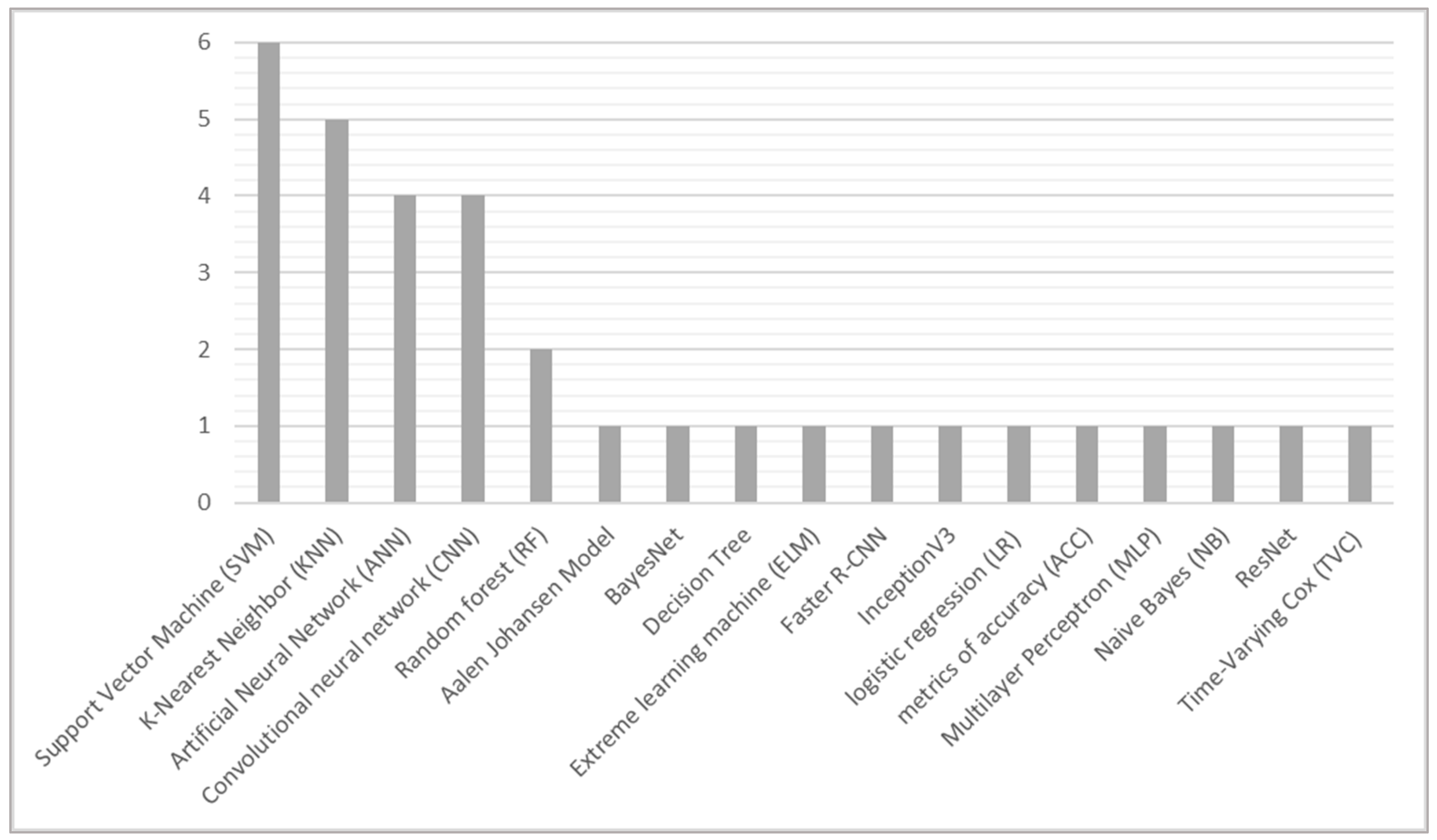
The most frequently used AI models were SVM (n = 6) and KNN (n = 5), followed by ANN and CNN (each n = 4) and RF (n = 2) (Figure 2).
Figure 2.
Artificial intelligence prediction techniques for risk of developing diabetic foot.
4. Discussion
Diabetic foot ulcers are costly and debilitating and have serious consequences for people with diabetes [37]. All diabetic patients should be carefully and thoroughly educated about preventive measures and foot care [5]. However, the traditional process of diagnosis of DFU by clinicians and DFU specialists is very expensive and time-consuming. Therefore, deep learning in medical imaging opens corridors for the automatic diagnosis of DFU [38]. Given the complex nature of DFUs, AI methodologies seem well suited to address aspects such as timely screening to identify the risk of foot ulcers (or worse, amputation) based on appropriate sensor technologies [39].
Our review of the papers found that DFUs can be identified in different ways. The most used classifiers in the reviewed papers are SVM and KNN. Nanda et al. [24] found that SVM is better than the other algorithms in point of MCC, which is 0.875, and F-measure, which is 0.938. The performance of KNN and Naive Bayes were comparable to each other. In the study, RF was the most efficient in terms of sensitivity and SVM was the most efficient in terms of highest specificity, which was 93.8%. Reddy et al. [26] included ELM and ANN in the research, in parallel to SVM and KNN. The ELM achieved the highest accuracy, followed by the SVM with 92.31%. The ANN and KNN were comparable, both achieving an accuracy of 84.62%. In a literature review by Tulloch et al. [28], all included models achieved accuracies above 90%. SVM and KNN have also been used for risk prediction based on thermography. In a study by Cruz-Vega [30], although the SVM model obtained satisfactory results, it did so after a feature extraction procedure, which we would like to avoid. Eid et al. [31] found that KNN achieved the highest performance, improving classification accuracy by 4.3% compared to using SVM. Another effective technique for interpreting the learned features of CNN layers is t-distributed stochastic neighborhood embedding (t-SNE) [40], which has been used to visualize clusters of heart rate data with respect to glucose levels. The use of t-SNE can also be generalized to other CNN applications, such as DFU detection, in order to qualitatively analyze the extracted feature maps. In addition, a recent study has also verified the consistency of neural network models with respect to glucose and insulin dynamics [41]. Similar approaches can be used to analyze the performance of DNNs and further improve interpretability [42].
The most common variables included in the prognostic model are age, type of diabetes, body mass index (BMI), and type of diabetes. In the studies by Ferreira et al. [23] and Zhang et al. [29], only ANN models were used. In the first study, they reported a sensitivity of 71%, a specificity of 100%, and an accuracy of 90%. In the second study, they report that the model had a sensitivity of 92.3% and a specificity of 93.5%.
Many authors attempt to classify foot thermograms using asymmetric analysis, which consists of comparing the temperature of the foot with that of the contralateral foot [31]. Several papers report that thermography is useful for detecting changes in sole temperature that could increase the risk of pressure ulcers. Cruz-Vega et al. (2020) discovered that the CNN classifiers require an additional data augmentation step for three structures (GoogLeNet, AlexNet, and DFTNet) [30]. The highest values of sensitivity, specificity, AUC (area under the curve), and accuracy were obtained with classifiers such as SVM and for the CNN structures in almost all pairs of classes compared, especially in the well-separated classes. The best results of DFNet can be attributed to the specific network design for this type of images. Although the GoogLeNet and AlexNet network structures are more complex and supposed to be better classifiers, they were trained with a different type of images. This work presents a comparison of conventional classifiers such as ANN, SVM, and currently important classifiers such as CNN [30]. The works by Muralidhara et al. [35] use techniques that only allow binary classification of thermograms (which corresponds to the first case).
Improving AI-based systems improves the accuracy and efficiency of diagnosis and treatment in different areas [43], and thus, the safety of care [44]. Using AI and data sources also reduces the frequency of errors in different areas of patient care [44].
The main limitation is the heterogeneity of the research, as we have included different types of research with different prediction models. By using balanced datasets with a significant number of samples, classification models can achieve more accurate predictions. Expanding the dataset should not only mean including more detailed clinical information on the subjects studied, but should also include a wide range of the most common variables included in the prognostic models. The images used in the studies analyzed were usually taken with a smartphone or tablet and did not require the high-tech imaging available only in research and industrial settings. The use of hand-crafted imaging features and raw clinical attributes in the prediction algorithm facilitates better insight for both clinicians and patients. With more samples and research, it is expected that accuracy will increase and that it could be performed in specialized units in daily practice for early DFU, allowing rapid care and avoiding further costs and consequences for the patient. Different Al models have been applied in these areas, achieving better experimental performance than previous conventional machine learning methods. On the other hand, several challenges have been identified in the literature, including data availability, feature processing, and interpretability of models. In the future, there is considerable potential to address these challenges by applying recent advances in deep learning technologies to massive multimodal diabetes treatment data. We expect that deep learning technologies will be widely deployed in clinical settings and will greatly improve the treatment of people living with diabetes. In the discussion, we compared the numerical values of the performance of the models reported in the reviewed papers. The papers did not use the same dataset for training and testing, which could be a serious limitation in some studies. We also limited our search to English articles only, thus leaving open the possibility that we did not include all relevant studies in the review.
Author Contributions
Conceptualization, L.G. and G.S.; methodology, L.G., M.L., A.S. and G.S.; formal analysis, L.G., A.S. and G.S.; writing—original draft preparation, L.G., M.L., A.S. and G.S.; writing—review and editing, L.G. and G.S.; supervision, L.G. and G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Diabetes. Available online: https://www.who.int/health-topics/diabetes#tab=tab_3 (accessed on 21 November 2022).
- Negash, Z.; Yismaw, M. Management practice and contributing risk factors for chronic complications among type 2 diabetes mellitus adult patients in follow-up at a tertiary care teaching hospital. Diabetes Metab. Syndr. Obes. Targets Ther. 2020, 13, 3969. [Google Scholar] [CrossRef] [PubMed]
- Naves, C.C. The diabetic foot: A historical overview and gaps in current treatment. Adv. Wound Care 2016, 5, 191–197. [Google Scholar] [CrossRef]
- Xie, P.; Li, Y.; Deng, B.; Du, C.; Rui, S.; Deng, W.; Wang, M.; Boey, J.; Armstrong, D.G.; Ma, Y.; et al. An explainable machine learning model for predicting in-hospital amputation rate of patients with diabetic foot ulcer. Int. Wound J. 2022, 19, 910–918. [Google Scholar] [CrossRef]
- Oliver, T.I.; Mutluoglu, M. Diabetic foot ulcer. Lancet 2003, 361, 1545–1551. [Google Scholar]
- Everett, E.; Mathioudakis, N. Update on management of diabetic foot ulcers. Ann. N. Y. Acad. Sci. 2018, 1411, 153–165. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Boulton, A.J.; Bus, S.A. Diabetic foot ulcers and their recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Sikhondze, M.M.; Twesigye, D.; Odongo, C.N.; Mutiibwa, D.; Tayebwa, E.; Tibaijuka, L.; Ayana, S.D.; Dreque, C.C. Diabetic foot ulcers: Surgical characteristics, treatment modalities and short-term treatment outcomes at a tertiary hospital in South-Western Uganda. Open Access Surg. 2022, 15, 75–87. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A.; Harkless, L.B. Validation of a diabetic wound classification system: The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998, 21, 855–859. [Google Scholar] [CrossRef]
- Oyibo, S.O.; Jude, E.B.; Tarawneh, I.; Nguyen, H.C.; Armstrong, D.G.; Harkless, L.B.; Boulton, A.J. The effects of ulcer size and site, patient’s age, sex and type and duration of diabetes on the outcome of diabetic foot ulcers. Diabet. Med. 2001, 18, 133–138. [Google Scholar] [CrossRef]
- Boulton, A.J.; Vileikyte, L.; Ragnarson-Tennvall, G.; Apelqvist, J. The global burden of diabetic foot disease. Lancet 2005, 366, 1719–1724. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.Z.; Ng, N.S.; Thomas, C. Prevention and treatment of diabetic foot ulcers. J. R. Soc. Med. 2017, 110, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Chappell, F.M.; Crawford, F.; Horne, M.; Leese, G.P.; Martin, A.; Weller, D.; Boulton, A.J.; Abbott, C.; Monteiro-Soares, M.; Veves, A.; et al. Development and validation of a clinical prediction rule for development of diabetic foot ulceration: An analysis of data from five cohort studies. BMJ Open Diabetes Res. Care 2021, 9, e002150. [Google Scholar] [CrossRef] [PubMed]
- Young, M.; Stang, D. Stay classy: The classification of diabetic foot ulcers and its relevance to management: Part 1. Diabet. Foot J. 2018, 21, 52–55. [Google Scholar]
- Amisha; Malik, P.; Pathania, M.; Rathaur, V.K. Overview of artificial intelligence in medicine. J. Fam. Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar] [CrossRef]
- Briganti, G.; Le Moine, O. Artificial intelligence in medicine: Today and tomorrow. Front. Med. 2020, 7, 27. [Google Scholar] [CrossRef]
- Aboul-Ela, M.M.; Amer, A.A.; Ismail, S.M. Diabetic foot prediction using hybrid artificial intelligent systems. Int. J. Adv. Comput. Technol. (IJACT) 2016, 5, 19–29. [Google Scholar]
- Howard, T.; Ahluwalia, R.; Papanas, N. The advent of artificial intelligence in diabetic foot medicine: A new horizon, a new order, or a false dawn? Int. J. Low. Extrem. Wounds 2021, 15347346211041866. [Google Scholar] [CrossRef] [PubMed]
- Wouter, B.; Schut, M.C.; Abu-Hanna, A.; van Baal, J.G.; van Netten, J.J.; Bus, S.A. Development of a prediction model for foot ulcer recurrence in people with diabetes using easy-to-obtain clinical variables. BMJ Open Diabetes Res. Care 2021, 9, e002257. [Google Scholar]
- Hernandez-Contreras, D.; Peregrina-Barreto, H.; Rangel-Magdaleno, J.; Gonzalez-Bernal, J. Narrative review: Diabetic foot and infrared thermography. Infrared Phys. Technol. 2016, 1, 105–117. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Bujold, M.; Wassef, M. Convergent and sequential synthesis designs: Implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst. Rev. 2017, 6, 1–4. [Google Scholar] [CrossRef]
- Polit, D.; Beck, C.T. Nursing Research Generating and Assessing Evidence for Nursing Practice, 11th ed.; Wolters Kluwer: Alphen, The Netherlands, 2021. [Google Scholar]
- Ferreira, A.C.; Ferreira, D.D.; Oliveira, H.C.; de Resende, I.C.; Anjos, A.; de Moraes Lopes, M.H. Competitive neural layer-based method to identify people with high risk for diabetic foot. Comput. Biol. Med. 2020, 120, 103744. [Google Scholar] [CrossRef]
- Nanda, R.; Nath, A.; Patel, S.; Mohapatra, E. Machine learning algorithm to evaluate risk factors of diabetic foot ulcers and its severity. Med. Biol. Eng. Comput. 2022, 60, 2349–2357. [Google Scholar] [CrossRef]
- Ohura, N.; Mitsuno, R.; Sakisaka, M.; Terabe, Y.; Morishige, Y.; Uchiyama, A.; Okoshi, T.; Shinji, I.; Takushima, A. Convolutional neural networks for wound detection: The role of artificial intelligence in wound care. J. Wound Care 2019, 28, S13–S24. [Google Scholar] [CrossRef]
- Reddy, S.S.; Mahesh, G.; Preethi, N.M. Exploiting machine learning algorithms to diagnose foot ulcers in diabetic patients. EAI Endorsed Trans. Pervasive Health Technol. 2021, 7, e2. [Google Scholar] [CrossRef]
- Schäfer, Z.; Mathisen, A.; Svendsen, K.; Engberg, S.; Rolighed Thomsen, T.; Kirketerp-Møller, K. Toward machine-learning-based decision support in diabetes care: A risk stratification study on diabetic foot ulcer and amputation. Front. Med. 2021, 7, 601602. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, J.; Zamani, R.; Akrami, M. Machine learning in the prevention, diagnosis and management of diabetic foot ulcers: A systematic review. IEEE Access 2020, 8, 198977-9000. [Google Scholar] [CrossRef]
- Zhang, D.; Dong, W.; Guan, H.; Yakupu, A.; Wang, H.; Chen, L.; Lu, S.; Tang, J. CT-Angiography-based outcome prediction on diabetic foot ulcer patients: A statistical learning approach. Diagnostics 2022, 12, 1076. [Google Scholar] [CrossRef]
- Cruz-Vega, I.; Hernandez-Contreras, D.; Peregrina-Barreto, H.; Rangel-Magdaleno, J.D.; Ramirez-Cortes, J.M. Deep learning classification for diabetic foot thermograms. Sensors 2020, 2, 1762. [Google Scholar] [CrossRef]
- Eid, M.M.; Yousef, R.N.; Mohamed, M.A. A proposed automated system to classify diabetic foot from thermography. Int. J. Sci. Eng. Res. 2018, 9, 371–381. [Google Scholar]
- Filipe, V.; Teixeira, P.; Teixeira, A. Automatic classification of foot thermograms using machine learning techniques. Algorithms 2022, 15, 236. [Google Scholar] [CrossRef]
- Goyal, M.; Reeves, N.D.; Davison, A.K.; Rajbhandari, S.; Spragg, J.; Yap, M.H. Dfunet: Convolutional neural networks for diabetic foot ulcer classification. IEEE Trans. Emerg. Top. Comput. Intell. 2018, 4, 728–739. [Google Scholar] [CrossRef]
- Gururajarao, S.B.; Venkatappa, U.; Shivaram, J.M.; Sikkandar, M.Y.; Al Amoudi, A. Infrared thermography and soft computing for diabetic foot assessment. In Machine Learning in Bio-Signal Analysis and Diagnostic Imaging; Academic Press: Cambridge, MA, USA, 2019; pp. 73–97. [Google Scholar]
- Muralidhara, S.; Lucieri, A.; Dengel, A.; Ahmed, S. Holistic multi-class classification & grading of diabetic foot ulcerations from plantar thermal images using deep learning. Health Inf. Sci. Syst. 2022, 10, 1–9. [Google Scholar]
- Vardasca, R.; Vaz, L.; Magalhaes, C.; Seixas, A.; Mendes, J. Towards the diabetic foot ulcers classification with infrared thermal images. In Proceedings of the 14th Quantitative Infrared Thermography Conference, Berlin, Germany, 25–29 June 2018. [Google Scholar]
- Rafiq, M.K.; Kamran, H.; Ayub, A.; Jameel, F. Diabetic foot ulcers: Insights into management and prevention. Pak. J. Med. Health Sci. 2022, 16, 633. [Google Scholar] [CrossRef]
- Das, S.K.; Roy, P.; Mishra, A.K. Pre-trained efficientnet-b0 with adjusted optimizer, learning rate and image size to improve diabetic foot ulcers diagnosis. In Emerging Electronics and Automation; Springer: Singapore, 2022; pp. 317–329. [Google Scholar]
- Chemello, G.; Salvatori, B.; Morettini, M.; Tura, A. Artificial intelligence methodologies applied to technologies for screening, diagnosis and care of the diabetic foot: A narrative review. Biosensors 2022, 12, 985. [Google Scholar] [CrossRef]
- Maaten, L.; Hinton, G. Visualizing data using t-SNE. J. Mach. Learn. Res. 2008, 9, 2579–2605. [Google Scholar]
- Kushner, T.; Sankaranarayanan, S.; Breton, M. Conformance verification for neural network models of glucose-insulin dynamics. In Proceedings of the 23rd International Conference on Hybrid Systems: Computation and Control, Sydney, Australia, 21–24 April 2020; pp. 1–12. [Google Scholar]
- Zhu, T.; Li, K.; Herrero, P.; Georgiou, P. Deep Learning for Diabetes: A Systematic Review. J. Biomed. Health Inform. 2020, 25, 2168–2194. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, A.S. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ 2019, 7, e7702. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Levine, D.; Syrowatka, A.; Kuznetsova, M.; Craig, K.J.; Rui, A.; Jackson, G.P.; Rhee, K. The potential of artificial intelligence to improve patient safety: A scoping review. NPJ Digit. Med. 2021, 4, 1–8. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).