Abstract
Objective: The purpose of this study was to assess the impact of photopolymer resin type, arch location, and post-processing techniques on the trueness and precision of three-dimensionally printed (3DP) full-arch surgical implant guides. Methods: Stereolithography reference images of an upper and lower surgical guide with six drill holes from a full-mouth rehabilitation clinical case were used. The files were imported into the Asiga MAX UV slicing software (Asiga Composer) where build orientation, print resolution, and support structures were added. A digital light processing 3D printer (MAX UV, Asiga Max) was used for printing the samples. The samples assessed were printed using two different, manufacturer-validated resins, DentaGuide (n = 35) and DentaClear (n = 20). The samples were subdivided and measured based on the post-processing technique used: handwashing (n = 20), sonication (n = 25), a mix of handwashing and sonication (n = 10), and post-curing using 385 nm UVA light with nitrogen (n = 50) or without nitrogen (n = 5). The diameter of each drill hole per guide was measured using a coordinate measuring machine (Absolute Arm 7-Axis, Hexagon) and compared with the reference STL to calculate each sample’s trueness (median error) and precision (interquartile range). The Mann–Whitney and Kruskal–Wallis tests were used for statistical analyses. Results: All samples demonstrated a dimensional error of <70 µm. No significant differences (p > 0.05) were observed between upper and lower arches and between post-processing techniques using nitrogen, irrespective of the use of hand- or ultrasonic washing. In contrast, DentaClear resin was significantly (p < 0.001) more accurate with a trueness of 26 µm and precision of 12 to 34 µm versus the DentaGuide at −31 µm and −54 to −17 µm, respectively. The samples post-cured without nitrogen were significantly (p < 0.05) the least accurate of all surgical guides, with a trueness of −42 µm and precision of −68 to −39 µm. Conclusion: The resin type and nitrogen post-processing are parameters that can significantly impact the accuracy of surgical guides. The tolerance of 3DP surgical guides needs to account for the dimensional changes occurring during the manufacturing process to minimise implant positioning errors.
1. Introduction
In dentistry, digital workflow is becoming a prevalent approach for fabricating implant surgical guides [1]. This workflow involves using three-dimensionally printed technology (3DP) for various uses in addition to implant surgical guides, including fixed and removable prostheses and orthodontic aligners [2]. Three-dimensionally printed has several advantages when compared to the subtractive method (milled technology) with regard to sustainability and resource consumption [3]. The three common systems of additive technology employed in dentistry are digital light processing (DLP), stereolithography apparatus (SLA) [4], and fused deposition modelling (FDP) [5].
Implant surgical guides can be fabricated through either subtractive (milling) or additive manufacturing (printing). Abduo and Lau [6] compared milled implant surgical guides with commercial and bench-printed guides. Milled surgical guides proved to be significantly more accurate with the lowest error of 0.21 ± 0.03 mm versus 0.28 ± 0.06 mm for bench-printed guides (p = 0.04). Despite these findings, the use of 3D printing technology for SLA and DLP remains the most common method for the in-office production of implant surgical guides [7] due to its improved affordability and accessibility. The DLP system employs a projector light guided by micromirrors to simultaneously polymerise the monomer in all three axes, thus reducing build time [8,9]. Nonetheless, there are several factors that influence the accuracy of DLP printing of surgical guides that warrant further investigation, especially with regard to full-arch implant surgical guides, as most literature investigates partially edentulous arches. A systematic review comparing the accuracy of partially edentulous arches to fully edentulous arches showed significant differences and suggested a 2 mm safety margin should be applied to ensure that the static computer-aided implant surgery (s-CAIS) approach is within the clinically acceptable range of results [10]. However, Rouzé l’Alzit et al. [11] found that the size of the implant surgical guide can affect trueness and precision. The larger extent guides with fewer supporting teeth were less accurate and had root mean square (RMS) values of 93.12 ± 13.22 μm, compared to 67.75 ± 10.63 μm for smaller extent guides with more supporting teeth, irrespective of the printing technology used.
Furthermore, the DLP system has been used in conjunction with the s-CAIS approach to fabricate full-arch implant surgical guides [12]. The s-CAIS approach proves advantageous in terms of accuracy and accessibility for clinicians as it offers a more affordable and convenient alternative to a traditional workflow [12] and a dynamic computer-assisted guidance approach [13]. It was also noted that by using a navigation-guided procedure such as s-CAIS or dynamic computer-assisted guidance for implant placement, an error of <1 mm of mean linear deviation and angular deviation of <4° is achievable [14]. Regarding the accuracy of s-CAIS, a horizontal error of approximately 1 mm at the entry point and 1.6 mm at the apex, 0.5 mm in height, and with a 5–6° axis is evident in the literature [15,16].
However, it is evident that 3DP surgical guides can significantly aid in preventing errors associated with manufacturing factors and virtual plans and aid in overall implant positioning [7] compared to conventional implant positioning methods. Specifically, s-CAIS allows for the option of the immediate loading of implants [12,13] and aids in reducing patient discomfort, chair time, and iatrogenic damage to anatomic structures such as the inferior alveolar nerve, thus resulting in fewer surgical complications. Therefore, this is leading to a shift away from conventional implant positioning techniques to one using 3DP surgical guides to improve patient outcomes [7]. Thus, investigating the accuracy of 3DP surgical guides is essential given their increased use as a part of the digital workflow in implantology.
Post-processing 3DP implant surgical guides is essential in ensuring the accuracy of the implant surgical guides fabricated, affecting the accuracy in terms of positive, negative, intaglio, and cameo surface discrepancies. One of the primary sources of error identified is excessive alcohol washing and insufficient removal of uncured resin [17]. Literature looking at single-implant tooth surgical guides comparing the automated method (solely ultrasonic washing) to handwashing along with ultrasonics found that the latter resulted in higher accuracy, with handwashing demonstrating discrepancy values that were consistently higher than the automated group. This trend was seen for all surface accuracy measurements in a similar study comparing post-processing methods [18]. Ammoun et al. [18] reported that handwashing and ultrasonic cleaning had a positive discrepancy, whereas the automated group had a greater negative error. The errors for both, however, were <0.18 mm, and hence deemed clinically acceptable [18]. Nonetheless, previous studies investigated single-implant guides with little evidence supporting specific post-processing recommendations for full-arch surgical guides.
Post-curing in a nitrogen atmosphere has also been reported to affect the properties of 3D printing. Two studies, Mayer et al. [19] and Reymus et al. [20], identified that curing in a nitrogen-rich atmosphere prevents the formation of an oxygen-inhibited layer, ensures complete surface polymerisation, and improves monomers’ conversion. Similarly, Wada et al. [21] looked at 3D-printed occlusal splints with different printers and post-curing techniques, and reported that stroboscopic post-curing with nitrogen improved the mechanical properties. When using Asiga printers, the double bond conversion of monomers (%) was 75.4 ± 4.5 with nitrogen compared to 56.7 ± 6.2 without (p < 0.001), and in terms of the Vickers hardness number (VHN), post-curing with nitrogen was 13.3 ± 0.5 compared to 11.8 ± 0.6 without (p < 0.001). Thus, curing in the presence of nitrogen is proven to have better mechanical properties. Nonetheless, and as previously identified with washing techniques, the effect of nitrogen for post-curing full-arch surgical guides remains to be explored.
This study aims to address the gap in the existing literature on the accuracy of full-arch surgical implant guides, as previous studies focused on single-implant surgical guides. The objective of this study is to assess the impact of photopolymer resin type, location of the arch, and post-processing techniques on the trueness and precision of full-arch 3DP surgical implant guides prior to implant placement.
2. Materials and Methods
2.1. Reference Images and Measurement Set-Up
Reference standard tessellation language (STL) files for a full-arch implant rehabilitation clinical case (All-on-6) consisting of an upper and lower implant surgical guide, each with six surgical holes of approximately 6.5 mm diameter, were used as reference images (Figure 1). The scans were acquired using an intraoral scanner (Trios 3, 3Shape, Copenhagen, Denmark). PolyWorks Inspector software (Innovmetric, QC, Canada) confirmed the individual diameter of each surgical hole and generated the reference data (Table 1).
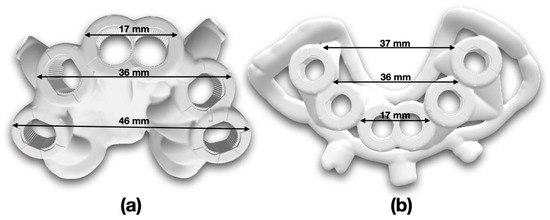
Figure 1.
Stereolithography reference images with indicative length measurements in millimetres (.stl) of implant surgical guides. (a) Upper; (b) lower.

Table 1.
Reference measurements for diameter of each plane hole based on reference STL files. All fifty-five samples were compared to the upper and lower reference measurements to determine error in diameter.
2.2. Manufacturing of 3D-Printed Implant Surgical Guides
This study utilised a DLP printer, an Asiga MAX UV (385 nm ultraviolet laser; Asiga, Alexandria, New South Wales, Australia), and a desktop 3D consumer-level printer [1,22]. The reference STL images of the implant surgical guides were imported into the Asiga MAX UV slicing software (Asiga Composer, Asiga, Alexandria, New South Wales, Australia). Asiga Composer-Build Wizard (Software Version 1.3.6-2) allows for the preparation of builds with multiple parts. The software was also used to orientate the models on the build platform at 0° horizontally and to design base plates for attaching the surgical guides to the build platform (Figure 2). A shadow type, 2 mm base plate thickness, was used underneath each guide. The z-axis resolution was set to 100 µm and was standardised across all samples. Support structures were added to all models before printing (Figure 3). The use of a minimum sample size of 5 samples was a convenience sample. This sample size has been utilised in both the ISO standardised testing protocols as well as in similar studies investigating surgical guide accuracy [23,24]. After printing completion, the models were retrieved from the platform, post-processing was completed, and the support structures were removed.
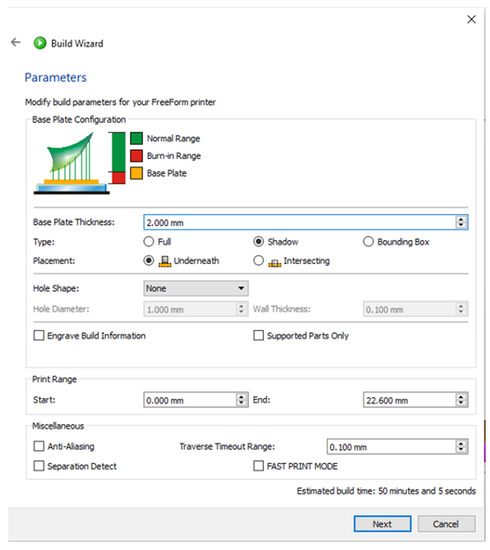
Figure 2.
Asiga Composer—selected parameters for printing on the Build Wizard 3D printing software.
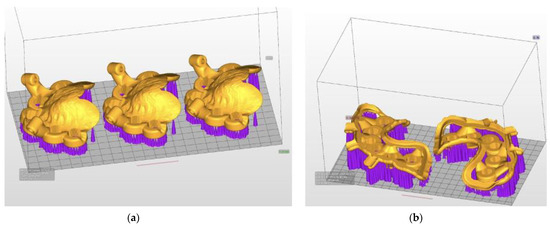
Figure 3.
STL reference images in ASIGA MAX UV slicing software containing implant surgical guides with support structures in place. (a) Upper; (b) lower.
2.3. Post-Processing of the 3DP Implant Surgical Guides
The 3DP of the reference surgical guides was subdivided into groups depending on their location (upper versus lower arch), resin type, and post-processing (washing and curing method). Two different resin types were utilised, the Asiga DentaCLEAR 385 nm resin (Asiga, Alexandria, New South Wales, Australia. Lot number MO/08427) (n = 20), and the Asiga DentaGUIDE (Asiga, Alexandria, New South Wales, Australia. Lot number MO/10567) (n = 35), to print both lower n = 10 and upper n = 45 arches of implant surgical guides. Both resins were agitated thoroughly for one minute in the resin bottle before pouring them into a material tray. This was to ensure colour deviation was avoided and print success was achieved.
All guides were post-processed through washing and post-curing. Five different post-processing methods were performed, with all washes, including pre- and post-washes, using 99.5% isopropanol (Thermo Fisher Scientific Australia, Victoria, Australia) with either hand wash or ultrasonic bath wash in dedicated baths for each resin (Table 2). For handwashing (n = 20), the guides were placed in a plastic bag with 99.5% isopropanol and agitated by the same operator. For the ultrasonic bath, the guides were placed in a beaker with 99.5% isopropanol in the ultrasonic bath (BioSonic UC300 Ultrasonic Cleaner) (n = 10). A combination of hand wash and ultrasonic bath was also used (n = 25).

Table 2.
Breakdown of specific post-processing techniques used for resin and arch type per group.
Before post-curing, the samples were dried thoroughly using compressed air to ensure the printed parts were free of any alcohol residue. Lastly, post-curing with nitrogen (n = 50) or without nitrogen (n = 5) was performed using the same UV curing unit (Otoflash G171, 280–700 nm, Puretone 3D, Kent, United Kingdom). Each sample required a total of 4000 flashes (2 × 2000 flashes), flipping the samples after 2000 flashes in the post-curing box and allowing them to cool for 5 min prior to repeating for a total of 4000 flashes.
After post-processing, the supports were removed and trimmed with caution using pliers. All samples were stored until they were measured by the same operator using the coordinate measuring machine within two weeks post-printing.
2.4. Assessment of Accuracy
Each implant surgical guide comprised six surgical drill holes. Fifty-five surgical guides were printed using the MAX UV (385 nm ultraviolet laser; Asiga, Alexandria, New South Wales, Australia) to assess the accuracy using trueness (median error) and precision (IQR) using the data comparing the difference in diameter from the reference STL files. A coordinate measuring machine (CMM, Absolute Arm 7-Axis, Hexagon, Cobham, UK) with a 50 mm long probe and 3 mm ruby tip was used to assess the guides. The CMM Absolute Arm 7-Axis, Hexagon was calibrated according to ISO 10360-12 with a confirmed error of 0.005 mm. The measurement set-up is shown in Figure 4. The CMM measurements began by outlining the base of the model to establish an area in space on PolyWorks Inspector (Innovmetric, QC, Canada) using the six plane holes circumferentially around the surgical implant guide. The plane holes were then measured using hole 1 as the datum (surface of the guide plane around hole 1), where X, Y, and Z are all zero (Figure 4), and X is defined along the line centre to centre for holes 1–6 for consistency. The sequence of measurements of the plane holes was from holes 1 to 6 and the line vector from hole 1 to hole 6 to create a cartesian axis located in the measured centre of hole 1. The diameter of the holes was then calculated using the sphere function on PolyWorks Inspector. All guides were stored and measured in a temperature-controlled room (24 °C, 1013 hPa), with the same operator completing all measurements. The 3D-printed models were stored in the same conditions in a dark storage compartment devoid of light and sent to assess the dimensional stability of the 3D-printed models. The diameter of the holes was used to assess the trueness and precision of the printed guides.
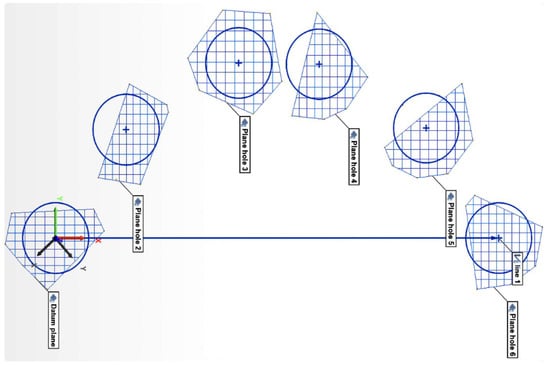
Figure 4.
Measurement set-up using the coordinate measuring machine (CMM). Hole 1 is the datum where X, Y, and Z will be zero. X-axis is defined along the line centre to centre of hole 1–6 for consistency. Datum plane is defined as the surface of the guide around hole 1, describing the X–Y plane.
2.5. Statistical Analysis
The median error was used to determine the trueness, whilst the interquartile range (IQR) was used to assess the precision. The Mann–Whitney U test (Table 3) and Kruskal–Wallis test (Table 4) were used to compare dimensional error for arch location, resin type, and washing technique. All statistical analysis was performed using IBM SPSS statistics software (Version 24; IBM, Armonk, NY, USA) with a significance level of 0.05. This allowed for a comparison of the parameters of resin type, use of nitrogen, and post-processing technique.

Table 3.
Results from Mann–Whitney U test for median (trueness) and interquartile range (IQR) (precision) of arch and resin type compared to the STL reference image measurements. All measurements are in millimetres.

Table 4.
Results from Kruskal–Wallis test for pairwise comparisons using median (trueness) and interquartile range (IQR) (precision) for various processing types. All measurements are in millimetres.
3. Results
It was observed that the dimensional error in terms of trueness and precision was <70 µm for all post-processing groups tested. This study found that there was no statistically significant difference (p > 0.05) when comparing arch location (upper vs. lower) nor between the post-processing techniques of hand or ultrasonic washing in the presence of nitrogen gas. However, a significant error was noted when nitrogen gas was not used.
When comparing the resin type between DentaClear and DentaGuide, the trueness and precision demonstrated a significant difference (p < 0.001). DentaClear was more accurate, with a trueness value of 26 µm compared to a value of −31 µm for DentaGuide. In terms of precision, DentaClear was also more accurate, with IQR values of 12 to 34 µm compared to DentaGuide at −54 to −17 µm. The arch location, however, did not affect accuracy as the upper had a trueness value of −19 µm. In comparison, lower had a value of −23 µm, as well as precision values of −44 µm to 19 µm for upper and −25 µm to −15 µm for lower, with no statistically significant difference noted (p = 0.300).
Lastly, samples post-cured without nitrogen were significantly (p < 0.05) the least accurate of all the printed guides, with a trueness of −42 µm and precision of −68 to −39 µm (Table 3 and Table 4 and Figure 5).
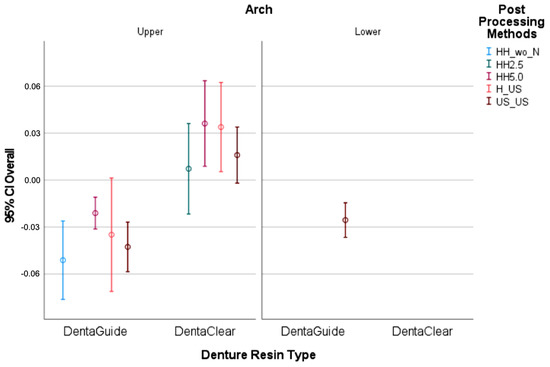
Figure 5.
Confidence interval and mean demonstrating trueness (mean) and precision (IQR) in a box plot. Note: handwashing without nitrogen (HH wo N), handwashing for 2.5 min (HH 2.5), handwashing for 5 min (HH 5.0), handwashing and sonication (H_US), sonication (US_US). All measurements are in millimetres.
4. Discussion
This study focused on determining a suitable methodology for assessing trueness and precision by considering the error in the diameter of 3DP full-arch surgical guides. The diameters of each plane hole and their accuracy are crucial for implant placement to avoid damage to any anatomical structures such as the maxillary sinus and inferior alveolar nerve [25].
A strength of this study was the method to measure error; to ensure accurate measurement, a CMM with direct profilometric measurements was acquired and analysed using inspection software to compare the measurements to the reference STL files. This approach minimises the measurement errors arising from optic scanning. It is followed by iterative closest point superimposition (best-fit alignment or registration) used by other studies that tend to over- or under-estimate measurement deviation [1,26,27]. Moreover, to minimise printing errors, a high-accuracy DLP printer was selected for manufacturing the surgical guides with a reported accuracy of −16 µm [8].
Additionally, the choice of the controlled variables of print orientation and print layer thickness in this study having been determined based on existing evidence proved to be a strength, as the print orientation affects dimensional and mechanical properties [22]. A study [28] investigated the fracture toughness for additive layer manufacturing (ALM) techniques similar to the DLP used in this study, and found that printing of composite double cantilever beams in a vertical direction had a 217% increased toughness compared to a horizontal direction for the same configuration. However, in terms of print orientation used for dental implications, a horizontal (0°) build angle is most commonly used with proven superior accuracy, although a 45° inclination has also been reported to have a high fit rate [6,11]. Nevertheless, Rubayo et al. [7] reported that a 0° build angle required the shortest printing time of (hour: minute) 1.26 ± 0.03 (p < 0.001) and had a reported accuracy of 0.048 mm ± 0.007, whilst a 90° build angle required the longest printing time of 2.52 ± 0.06 (p < 0.001) and had a 0.097 mm ± 0.017 accuracy. Another study looking at additive manufacturing 3DP [29] assessed the effect of print orientation on strength in terms of elastic modulus and tensile strength. It was found that a print orientation of 0° had higher strengths than those at 90°. As a result of the aforementioned literature, this study utilised a horizontal 0° build angle for all prints. The layer thickness can equally influence the accuracy of the implant surgical guide. Sherman et al. [30] and Zhang et al. [31] assessed layer thickness for DLP printers, and demonstrated that the range of 25 to 150 µm layer thickness achieved clinically acceptable results. Similarly, Etemad-Shahidi et al. [8] reported that a layer thickness of 100 µm proved optimal to ensure accuracy and reduce printing time, compared to 25 and 50 µm thicknesses.
In this study, varying parameters were investigated, including resin type, arch location, and post-processing methods. Regarding the type of resin, both tested resins were propriety, validated, and photosensitive polymer resins from the 3D printer’s manufacturer (Asiga) and indicated for implant surgical guides’ manufacturing. As a result of this, it was appropriate for this study to print implant surgical guides. However, it is important to note that this resin is not intended for long-term use in the oral cavity, and this was an important factor to consider as per the manufacturer’s instructions to optimise the mechanical properties of the guides, which are only used during the surgical placement of the implants. Nonetheless, their accuracy varied significantly, with the DentaClear resin demonstrating improved dimensional accuracy compared to the DentaGuide, which consistently produced undersized surgical guides. Both resins, as per the manufacturer’s specifications, are composed of 7,7,9(or 7,9,9)-trimethyl-4,13-dioxo-3,14-dioxa-5,12-diazahexadecane-1,16-diylbismethacrylate and tetrahydrofurfuryl methacrylate polymer resins, with Diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide as a photoinitiator. Despite their identical composition, the DentaClear produced translucent surgical guides, while the DentaGuide produced significantly more opaque ones (Figure 6). The difference in opacity, and consequent light penetration, polymerisation, and degree of conversion between these otherwise identical resins may account for the detected variation in accuracy. Whilst the maxillary surgical guide was larger in size than the mandibular one, it was evident that the size difference was insufficient to produce any significant errors.
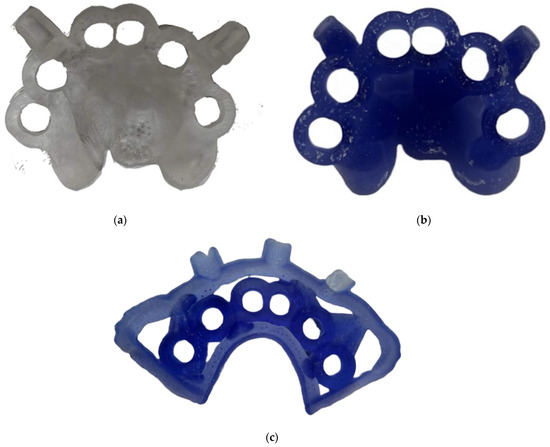
Figure 6.
Upper implant surgical guides in both resins: (a) DentaClear; (b) DentaGuide. (c) Lower surgical guide in DentaGuide resin.
This study followed the manufacturer’s instructions for using both resins in terms of washing and post-processing whilst testing alternative approaches. For the washing of the guides, the DentaClear guides were handwashed for 5 min, instead of 2.5 min, to allow for direct comparison against the DentaGuide guides, which were also washed for 5 min. The results of this study demonstrated no statistically significant difference between handwashing, ultrasonic washing, or a combination of both washing techniques. Thus, it is not likely that the washing method alone can significantly impact the dimensional accuracy of implant surgical guides.
The findings of this study also identified that using nitrogen during the post-curing significantly impacted accuracy, with the guides post-cured with the presence of nitrogen gas in the UV curing unit demonstrating higher dimensional accuracy regardless of the resin type and post-processing washing technique used. Indeed, the manufacturer’s instructions for both DentaClear and DentaGuide resins recommend using nitrogen for post-curing. It was evident from this study that post-curing the surgical guides with nitrogen showed statistically significant results in terms of dimensional accuracy for both precision and trueness. Similar results of improved mechanical properties when using nitrogen for post-curing were also reported by Wada et al. [21], who investigated 3D-printed occlusal splints. Their study showed that splints post-cured with nitrogen had improved monomer conversion and hardness according to Vickers hardness score.
Whilst all samples, irrespective of resin type, location, or post-processing technique, demonstrated a discrepancy, that discrepancy remained <70 µm. Previous studies investigating implant-supported complete dental prostheses or hybrid bridges concluded that a maximum acceptable threshold of fit between the prostheses platform and the dental implants ranges between 59–150 μm. As such, the surgical guides assessed in this study remain within the clinically acceptable threshold for implant placement. It is critical that the surgical drill and the guide hole are a suitable match with minimal tolerance to ensure implant placement in the prosthetically planned location. The placement of a metal sleeve or manual adjustment of the drill hole results in the introduction of errors into the surgical guide. Henceforth, identifying and accounting for any manufacturing errors of surgical splints is important.
The type of cleaning medium can also have an impact on the properties of the resultant print. Two studies, Mayer et al. [19] and Reymus et al. [20], identified that post-washing with different cleaning products can significantly influence dimensional accuracy due to improper removal of uncured resin monomer leading to high surface roughness and a reduced degree of conversion. These studies compared different post-washing solutions and found that the manufacturer’s recommendation did not always provide the highest mechanical properties. Both studies used a DLP printer and a resin containing 7,7,9(or 7,9,9)-trimethyl-4,13-dioxo-3,14-dioxa-5,12-diazahexadecane-1,16-diylbismethacrylate, and found that cleaning with 100% isopropanol (as per the manufacturer’s recommendation) resulted in the second highest degree of conversion (%) of 90.8 ± 4.5, whilst using Yellow Magic 7 cleaner resulted in 93.4 ± 1.6%. Further research should explore using different cleaning media that may veer from the manufacturer’s guidelines to obtain the highest dimensional accuracy.
Some limitations to consider include operator error. In this study, to reduce inter-operator variability and inconsistency, a single operator performed the surgical guide printing and washing, J.K.L., while a second operator performed the surgical guide post-curing, W.L. Hence, while precision in the form of repeatability was assessed, the same cannot be claimed for reproducibility amongst different operators. The operators’ training and experience has been reported to influence post-processing [18]. This study also only investigated the accuracy of the drill holes. The presence of soft and hard tissue interferences, saliva, blood, and patient movement may impact the surgical guide’s seating, site preparation, and implant insertion, factors that have not been investigated in this in vitro study. Moreover, other factors may influence the accuracy of surgical guides and need to be considered that are out of the scope of this study. A limitation of this study is assessing the possible effects of disinfection and sterilisation on the accuracy of 3DP implant surgical guides. The last step of preparing the surgical guides prior to patient use, where there is contact with the oral cavity, is disinfection and sterilisation, as without proper protocols, there is chance of infection [30]. Sterilisation involves the complete removal and destruction of all microbial organisms, whilst disinfection removes any microbial organisms that produce spores [32], and both have been found to significantly impact the properties of surgical guides, with heat sterilisation at 121 and 134 °C modifying the mechanical properties of DLP and SLA 3DP guides, when compared to disinfection with 4% aldehyde-free disinfectant [33].
Previous studies identified a statistically significant difference between SLA and DLP printers, with DLP demonstrating a lower deviation at the entry point of the implants (p = 0.023) and proving to be more accurate [34]. Assessing different types of 3D printers, such as SLA printers, for dimensional stability might be helpful for future studies to account for manufacturing errors arising from the printing system. Further research should also be aimed at assessing dimensional stability in an intra-oral environment as well as the impact of storage time, which are out of the scope of this in vitro study.
5. Conclusions
Within the limitations of this study, the type of resin and use of nitrogen for post-processing are parameters that significantly affected the accuracy of the full-arch surgical guides. Although the guides printed with nitrogen and DentaClear were of greater accuracy, dimensional changes were still seen. This must be considered during manufacturing to avoid positioning errors when placing implants. Further in vivo testing is needed to investigate the impact of additional factors such as sterilisation, disinfection, and storage time for more reproducible and predictable results in guided implantology.
Author Contributions
Conceptualisation, K.E.A.; methodology, R.V., W.L., J.K.L., F.A.-S., D.S., A.G. and K.E.A.; software, F.A.-S., D.S. and A.G.; validation, R.V. and K.E.A.; formal analysis, R.V., W.L. and J.K.L.; investigation, R.V., W.L. and J.K.L.; resources, K.E.A. and F.A.-S.; data curation, R.V., W.L., J.K.L., S.K.T., D.S. and A.G.; writing—original draft preparation, R.V. and K.E.A.; writing—review and editing, R.V., W.L., J.K.L., F.A.-S., G.C. and K.E.A.; visualization, R.V., W.L. and J.K.L.; supervision, K.E.A. and F.A.-S.; project administration, K.E.A.; funding acquisition, F.A.-S. and K.E.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lin, L.H.; Granatelli, J.; Alifui-Segbaya, F.; Drake, L.; Smith, D.; Ahmed, K.E. A Proposed In Vitro Methodology for Assessing the Accuracy of Three-Dimensionally Printed Dental Models and the Impact of Storage on Dimensional Stability. Appl. Sci. 2021, 11, 5994. [Google Scholar] [CrossRef]
- Braian, M.; Jimbo, R.; Wennerberg, A. Production tolerance of additive manufactured polymeric objects for clinical applications. Dent. Mater. 2016, 32, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef] [PubMed]
- Yoshidome, K.; Torii, M.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Trueness and fitting accuracy of maxillary 3D printed complete dentures. J. Prosthodont. Res. 2021, 65, 559–564. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef]
- Abduo, J.; Lau, D. Effect of Manufacturing Technique on the Accuracy of Surgical Guides for Static Computer-Aided Implant Surgery. Int. J. Oral Maxillofac. Implant. 2020, 35, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.-S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef]
- Etemad-Shahidi, Y.; Qallandar, O.B.; Evenden, J.; Alifui-Segbaya, F.; Ahmed, K.E. Accuracy of 3-Dimensionally Printed Full-Arch Dental Models: A Systematic Review. J. Clin. Med. 2020, 9, 3357. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29, 416–435. [Google Scholar] [CrossRef] [PubMed]
- Rouzé l’Alzit, F.; Cade, R.; Naveau, A.; Babilotte, J.; Meglioli, M.; Catros, S. Accuracy of commercial 3D printers for the fabrication of surgical guides in dental implantology. J. Dent. 2022, 117, 103909. [Google Scholar] [CrossRef]
- Wegmüller, L.; Halbeisen, F.; Sharma, N.; Kühl, S.; Thieringer, F.M. Consumer vs. High-End 3D Printers for Guided Implant Surgery—An In Vitro Accuracy Assessment Study of Different 3D Printing Technologies. J. Clin. Med. 2021, 10, 4894. [Google Scholar] [CrossRef]
- D’haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontology 2000 2017, 73, 121–133. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Vindasiute, E.; Linkeviciene, L.; Apse, P. Does residual cement around implant-supported restorations cause peri-implant disease? A retrospective case analysis. Clin. Oral Implant. Res. 2013, 24, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.; Marquardt, P.; Zwahlen, M.; Jung, R.E. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin. Oral Implant. Res. 2009, 20, 73–86. [Google Scholar] [CrossRef]
- Van Assche, N.; Vercruyssen, M.; Coucke, W.; Teughels, W.; Jacobs, R.; Quirynen, M. Accuracy of computer-aided implant placement. Clin. Oral Implant. Res. 2012, 23, 112–123. [Google Scholar] [CrossRef]
- Daoud, G.E.; Pezzutti, D.L.; Dolatowski, C.J.; Carrau, R.L.; Pancake, M.; Herderick, E.; VanKoevering, K.K. Establishing a point-of-care additive manufacturing workflow for clinical use. J. Mater. Res. 2021, 36, 3761–3780. [Google Scholar] [CrossRef]
- Ammoun, R.; Dalal, N.; Abdulmajeed, A.; Deeb, G.; Bencharit, S. Effects of two Post-Processing Methods Onto Surface Dimension of in-Office Fabricated Stereolithographic Implant Surgical Guides. J. Prosthodont. 2020, 30, 71–75. [Google Scholar] [CrossRef]
- Mayer, J.; Reymus, M.; Mayinger, F.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Temporary 3D printed fixed dental prosthesis materials: Impact of post printing cleaning methods on degree of conversion as well as surface and mechanical properties. Int. J. Prosthodont. 2021, 34, 784–795. [Google Scholar] [CrossRef]
- Reymus, M.; Liebermann, A.; Diegritz, C.; Keßler, A. Development and evaluation of an interdisciplinary teaching model via 3D printing. Clin. Exp. Dent. Res. 2021, 7, 3–10. [Google Scholar] [CrossRef]
- Wada, J.; Wada, K.; Gibreel, M.; Wakabayashi, N.; Iwamoto, T.; Vallittu, P.K.; Lassila, L. Effect of Nitrogen Gas Post-Curing and Printer Type on the Mechanical Properties of 3D-Printed Hard Occlusal Splint Material. Polymers 2022, 14, 3971. [Google Scholar] [CrossRef]
- Tahir, N.; Abduo, J. An In Vitro Evaluation of the Effect of 3D Printing Orientation on the Accuracy of Implant Surgical Templates Fabricated By Desktop Printer. J. Prosthodont. 2022, 31, 791–798. [Google Scholar] [CrossRef]
- Johansson, C.; Dibes, J.; Rodriguez, L.E.L.; Papia, E. Accuracy of 3D printed polymers intended for models and surgical guides printed with two different 3D printers. Dent. Mater. J. 2021, 40, 339–347. [Google Scholar] [CrossRef]
- Bennett, G.W.; Kim, S.K. Comparison of the fit of surgical guides manufactured with low-cost 3D printers. Gen. Dent. 2022, 70, 18–21. [Google Scholar]
- Lee, J.-H.; Park, J.-M.; Kim, S.-M.; Kim, M.-J.; Lee, J.-H.; Kim, M.-J. An assessment of template-guided implant surgery in terms of accuracy and related factors. J. Adv. Prosthodont. 2013, 5, 440–447. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, Y.-W.; Alshawaf, B.; Kang, K.; Finkelman, M.; Chronopoulos, V.; Weber, H.-P. Digital workflow: In vitro accuracy of 3D printed casts generated from complete-arch digital implant scans. J. Prosthet. Dent. 2020, 124, 589–593. [Google Scholar] [CrossRef]
- Yousef, H.; Harris, B.T.; Elathamna, E.N.; Morton, D.; Lin, W.-S. Effect of additive manufacturing process and storage condition on the dimensional accuracy and stability of 3D-printed dental casts. J. Prosthet. Dent. 2021, 128, 1041–1046. [Google Scholar] [CrossRef]
- Aranda, M.T.; Reinoso, J.; García, I.G. On different 3D printing methods and fracture performance in DCB composite specimens including structured interfaces. Theor. Appl. Fract. Mech. 2022, 122, 103552. [Google Scholar] [CrossRef]
- Khosravani, M.R.; Berto, F.; Ayatollahi, M.R.; Reinicke, T. Characterization of 3D-printed PLA parts with different raster orientations and printing speeds. Sci. Rep. 2022, 12, 1016. [Google Scholar] [CrossRef]
- Sherman, S.L.; Kadioglu, O.; Currier, G.F.; Kierl, J.P.; Li, J. Accuracy of digital light processing printing of 3-dimensional dental models. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 422–428. [Google Scholar] [CrossRef]
- Zhang, Z.-C.; Li, P.-L.; Chu, F.-T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop./Fortschr. Kieferorthopadie 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Available online: https://www.iso.org/standard/66262.html (accessed on 1 February 2022).
- Pop, S.I.; Dudescu, M.; Mihali, S.G.; Păcurar, M.; Bratu, D.C. Effects of Disinfection and Steam Sterilization on the Mechanical Properties of 3D SLA- and DLP-Printed Surgical Guides for Orthodontic Implant Placement. Polymers 2022, 14, 2107. [Google Scholar] [CrossRef] [PubMed]
- Gjelvold, B.; Mahmood, D.J.H.; Wennerberg, A. Accuracy of surgical guides from 2 different desktop 3D printers for computed tomography-guided surgery. J. Prosthet. Dent. 2019, 121, 498–503. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
