Abstract
The following paper focuses on the topic of mandibular unilateral condyle hyperplasia (UCH). This form of mandibular asymmetry (MA) is one of the less common but still known pathologies that requires detailed surgical and orthodontic planning and treatment. Since this pathology is mostly related to a high number of individual dental, bone, and overgrowth factors, until now the treatment methods were individually driven. It seems that the scope of surgical intervention is greatly dependent on the degree of bone overgrowth and the occurrence of asymmetry. Many treatment modalities and possible surgical perspectives are known, yet, so far, no adequate detailed guidelines are known. This detailed review of this type of mandibular asymmetry will focus on diagnostics and treatment plans and outcomes. The following paper underlines the authors’ own clinical experiences in MA and UCH treatment, which are compared with the literature review. The authors intend to investigate what has changed in the treatment and diagnostics of one-sided mandibular condyle and bone overgrowth.
1. Introduction
Unilateral condylar hyperplasia (UCH) is a pathology most commonly present in one side of the mandible, characterized by an abnormal condylar process of progressive overgrowth in time, causing visible changes in the anatomy, shape, and size of condylar head and neck elongation, along with visible facial asymmetry features [1,2,3,4,5].
Each mandibular asymmetry (MA) case should be carefully evaluated. UCH remains a challenge for surgeons since each case might be different. This situation is related to the volume of overgrowth, the duration of growth and its intensity, the scope of symptoms, and the formation of both dentoalveolar and skeletal disturbances, and many possible algorithms that could be used to treat it are known [6,7,8,9,10].
Clinically, the visible central incisor dental midline and/or upper/lower lips’ frenulum deviate from the central midline of the body, along with disproportions in the symmetry of the cupid’s bow, the lips’ angle exposure, and lip position. Skeletal, dental, and soft/hard tissue disproportions might occur, which are related to maxillary bone tilting and the scope of asymmetry, mainly impacted by time and the intensity of pathological growth [1,2]. Present bone and teeth discrepancies influence facial contour and balance, which influence facial appearance aspects, such as lip contour and symmetry, the angle of the lips, chin position, subnasal and sublabial balance, zygomaticomalar area prominence, and others [5,6,7,8,9,10,11,12].
The presented pathology might start early, at 9–12 years of age (±2 years), and can have various forms of intensity and growth activity, and even have a natural cessation period and self-limiting over time [6,7,8,9,10,11]. In most cases, mandibular asymmetry should be carefully examined and established, especially in young, growing patients. Growing children and young adults are most affected by this condition, and a higher female predominance (F:M ratio) is noted and estimated at 2:1 or 3:1 [11,12,13,14,15]. On the other hand, some authors emphasize no sex-related occurrence of this pathological condition, while others underline a higher occurrence rate in the left condyle area [11,12]. Raijmakers et al.’s meta-analysis study in 2012 explored 10 studies with 275 patients with UCH [12]. The presented results indicated a female predominance, along with a higher occurrence rate on the left side of the mandible, which has also been confirmed in other studies [13]. A study on two Indian families by Mahajan suggests a possible Y-linked or autosomal dominant etiology of UCH [14]. Both mother- and son-related genetics need further genetic evaluation. A similar rare genetic link was reported by Yang et al. in two siblings with mirror image UCH [15]. The role of potential etiological factors is still not fully known; however, some endocrine and hormone-related factors are also taken into consideration [11,12,13,14,15,16]. Possible etiological factors may be various since no evidence-based relationship has so far been noted in the literature. Some literature reviews suggest the following factors: trauma-related, metabolic hyperactivity, endocrinal distortions (growth factors, insulin growth factors (IGF), hormonal estrogen–progesterone related, and others), arthrosis, genetic factors, hereditary or acquired factors, or others [15,16,17,18,19].
The timing of early diagnostics greatly influences the types of possible treatment modalities that can be used. Moreover, the scope of each asymmetry is different for individual dentoalveolar discrepancies and teeth relations; therefore, the presented narrative review underlines only the selected special cases of UCH from the literature where active asymmetrical growth affected the condyle and those which became self-limiting over time, causing visible mandibular asymmetry, but where the pathological growth is inactive, has ceased, or is not present at all. The presented photos are from the authors’ collection of patients.
2. Mandibular Asymmetries Differentiation
An important topic is the differentiation between UCH and any other forms of mandibular asymmetries (MA), which can be related to different scopes of etiological factors, including: trauma, inflammation, TMJ abnormalities, condyle/head anatomical variations, benign/malignant TMJ tumors, cases with syndromic/non-syndromic genetic syndromes, or others. Mandibular asymmetries can be related to various factors. Anatomically, asymmetry can be described as the under- or over-development of one side of the mandible (ramus, angle, body, symphysis, or condyles) from various factors. Chia et al. underline some key factors that might divide MA into developmental (hemimandibular hyperplasia (HH), hemimandibular elongation (HE), hemifacial microsomia, Parry-Romberg), pathological (cysts, tumors, idiopathic condylar resorption, infections), traumatic (condylar fracture), and functional once (mandibular displacements, luxations, and others) [3]. Other developmental or genetic-related factors co-existing with mandibular asymmetry might include changes in the eye socket, external/internal ear area, temporomandibular area joint structural morphology, zygomatic and maxillary bones, or facial nerve functioning [4,5,6,7,8,9,10,17,18,19].
Other classifications of MA with recognition of dental, skeletal, and occlusal asymmetries features include Bishara et al.’s studies [7]. The mentioned asymmetry has been divided into dental, skeletal, muscular, functional, and a combination of all. On the other hand, a study by Reyeneke et al. divided MA into congenital, developmental, post-traumatic, and pathology-related categories [8]. Other classifications are also known [9,10].
Concerning the temporomandibular joint (TMJ), one of its components is the mandibular condyle (MC), along with its head and neck. Its position in the glenoid fossa of the temporal bone is limited anteriorly by the articular eminence. During growth and maturation, appropriate condyle growth ensures its adequate shape, size, and position. When some growth disturbances or abnormalities occur, various forms of condylar disfigurement might be present. Growth disturbances in the first trimester might result in condyle aplasia, hypoplasia, or related disorders. An understanding of the anatomy of the MC within the glenoid fossa can help in any surgery planning in UCH cases [15,16,17,18,19,20].
3. Classifications
Some types of mandibular asymmetry (MA), named mandibular condyle hyperplasia (CH) or unilateral condyle hyperplasia (UCH), are related to one-sided pathological growth in one of the affected condyles of an unknown origin. The presence of MA might start early in puberty and last even until the patient is fully grown, or the pathological growth might become self-limiting over time, in either way causing visible mandible asymmetry and lack of facial balance with the presence of various dentoalveolar discrepancies [2]. In 1986, Obwegeser and Makek used the first classification to distinguish hemimandibular hyperplasia (HH), an abnormal self-limiting condylar growth, resulting in pathologic one-sided bone overgrowth of the entire mandible on the affected side (Figure 1), as well as other forms such as hemimandibular elongation (HE) and a mixed, rare form HH-HE [1]. Currently, a different classification presented by Wolford et al., which includes some temporomandibular joint manifestations, is also known [6]. Types IA (the most common) and IB have excessive growth in the horizontal vector, while IIA and IIB have excessive growth in the vertical vector. Type III is caused by benign tumors (e.g., chondroma, osteoma), while type IV (the rarest) is caused by malignant tumors (e.g., chondrosarcoma, osteosarcoma) in the TMJ area [6].

Figure 1.
Typical facial appearance of UCH. A notable elongation and overgrowth of the right side of the face with chin asymmetry is visible. Changes in proportions of mouth angles are clearly visible along with the different positions of mandibular gonial diameters.
After the MA etiology and scope of changes within the mandibular body are evaluated, it is quite easy to identify UCH and schedule the necessary proceedings (Table 1).

Table 1.
Authors’ proposal on the scope of approaches. Each of the presented cases should be scheduled for orthodontic treatment because of various scopes of dentoalveolar discrepancies. (1) Case A: asymmetry (MA) without pathological growth and no UCH symptoms: scheduled for orthodontic or surgical camouflage or solely bone remodeling if no dentoalveolar discrepancies are present. (2) Case B–C: rapid or slowly progressive in time FA with MA asymmetry and pathological growth still present in the affected condyle confirmed in SPECT and during clinical examination: mandatory condylectomy followed by orthodontic treatment. After 3–6 months the scope of asymmetry, degree of maxillary tilting, and patient’s willingness to undergo total symmetry correction decide the final approaches. If the scope of mandibular overgrowth is extensive some surgical camouflage or bone remodeling procedures can be chosen. (3) Case D: low growth in SPECT with a tendency to decrease in time: early orthodontics followed by patient monitoring. If the orthodontics is sufficient, then the treatment is finalized. On the other hand, when growth has caused asymmetrical bone discrepancies and orthodontics alone is not sufficient a decision on either BSSO/Lefort I or surgical camouflage could be used. (4) Case E: growth became limited over time: orthodontics is sufficient to prevent MA and FA. In some difficult cases, either BIMAX, BSSO, Lefort I, or another approach can be scheduled based on each individual case. Abbreviations: BIMAX—includes BSSO and Lefort I procedures performed simultanously; ORT—orthodontic treatement.
4. Signs and Symptoms
A close, detailed patient evaluation might be made according to clinical and radiological signs and symptoms. Facial and/or mandibular asymmetry can cause various co-existing problems related to facial appearance, chewing, bite, occlusion, TMJ function, and in some cases even breathing and an unbalanced proper posture [20,21,22,23,24].
To begin with, the scope of mandibular asymmetry should be closely evaluated since its intensity and occurrence and changes in patients’ skeletal appearance are greatly correlated with the excess of growth pathology [1,2,3,4,5,6,7,8,9,10]. Some typical signs and symptoms can be addressed according to the Obwegeser, Wolford, or Kaban classifications of asymmetries, in detailed relation to the type of mandibular and skeletal asymmetry [1,2,3,4,5,6,7,8,9,10,20,21]. First of all, a detailed evaluation of any pain-related TMJ joint symptoms should be performed since, in some cases, patients’ TMJ pain in UCH might be present and result in condyle volume enlargement and its possible dysfunction. An enlarged condyle head might have a different shape and size with exophytic growth present on its surface or even some osteosclerosis or increased bone density [19,20,21,22,23,24]. The shape and size of the affected side are also age- and growth-related. It is worth noting that growth finishes earlier in females than males, at approximately 18 ± 1 year of age in females and up until 21 years of age in males [7,15,22]. Because of different pathological growth factors and the timing of its occurrence in UCH, the scope of mandibular overgrowth might greatly impact not only the shape, size, and position of the mandible. Secondary bone asymmetry, deviation, or lack of balance might also be present in the maxillary bone and might influence the maxillary sinus volume, along with the nasal septum. The degree of dentoalveolar discrepancy has an impact on proper chewing, bite, and occlusion, along with disrupted facial balance [3,8,12].
In the dental aspect, an open bite with the presence of various dentoalveolar discrepancies is found. Often, an open bite on the affected side is present, followed by a crossbite on the contralateral side. Dental balance is always disturbed. Along with mandibular asymmetrical growth, teeth position might result in various forms of open bites and crossbites on the affected side, along with others. The incisor midline may be deviated and shifted towards the healthy side with one of the possible variances in the volume of the increased anteroposterior and mediolateral dimensions of the right side upper and lower dental arches. Incisor tilting towards the affected side is common. Both dental, skeletal, and even labial frenulum symmetry lines can deviate. The types of open bite and molar contact are mostly dependable on the value of UCH condyle growth. Growth in vertical or horizontal aspects might lead to features of a skeletal class III or skeletal open bite (class II is very rarely seen). In slow-growing cases, the maxillary molars are capable of maintaining some contact with the mandibular molars. An open bite with a posterior crossbite might occur. In HH/HE cases, similar features of mandibular prognathism with malocclusion class III according to angle are quite common [3,7,8,15,22].
Skeletal manifestations with visible mandibular asymmetry consisted in most cases of the mandibular ramus’s vertical height being enlarged, followed by a typical antegonial notch, which can be less or more visible on CT/panx [5]. Secondly, the chin position might deviate towards the healthy side, be slightly protruded, or be a combination of the two. The body and mandibular ramus on the affected side may be elongated with an increased anteroposterior thickness of the mandibular body, and the characteristic shape of the gonial angle with a low-settled mandibular canal towards the inferior mandibular border is most commonly found [23,24,25,26,27]. The lateral aspect of the mandibular base can also be enlarged and curved. The chin position might be protruded and deviated in a skeletal class III-like matter. The aspect of increased cortical thickness in the overgrowth bone might be more visible in the affected condyle area. In some situations, the increased volume of the head might decrease mouth opening and some mandibular movements and cause a more visible open bite over time or have a continuous small growth causing simultaneous down growth of the maxillary bone on the affected side.
Some atypical bone features might include asymmetrical growth of the maxillary bones, changes in the volume and size of maxillary sinuses, an increased horizontal volume of the maxillary dental process on the affected side, or other case-specified situations. Some authors also conclude incidence of changes in the shape of the anterior nares, deviation in the nasal septum, and palatal cant. These could also be related to disrupted nasal breathing because of the scope of skeletal malocclusion [16,27,28,29,30].
Soft tissues are characteristics for chin asymmetry, sloping rima oris, lips asymmetry, deviation of the mandibular angle, and convex profile on the affected side, which, in some cases, is also related to alleged eye asymmetry, which is related to head lining for patients’ subconscious adjustment for asymmetry (Figure 2). A study by Fariña et al. with detailed measurements on 20 patients’ vertically increased mandibular ramus concluded that the mandibular lingula is the lowest and most stable reference point for any measurements, while the sigmoidal notch is neither a suitable nor a stable reference point [29,30]. On the other hand, a study by Olate et al., which measured various reference lines between the condylar head and midline, suggests that UCH always influences facial transversal asymmetry [30].

Figure 2.
Visible lack of balance in lip contour with deviated maxillary bite plane and open bite present on the affected right side. The degree of maxillary deviation is related to the degree and volume of abnormal growth in the affected condyle over time. Open bite suggests an increased volume of pathological growth and low compensatory maxillary downward rotation. In the following cases, orthodontic treatment has its limitations, even after a condylectomy.
5. Imaging Tests for Diagnosis
There are two possible methods for distinguishing mandibular condylar hyperplasia (MCH). The first and more basic one is focused on a detailed facial evaluation and anatomical examination. The second, more accurate, and comprehensive method requires one of the following radiological steps, consisting of routine panoramic radiography, mandibular AP/PA radiography to estimate the overgrowth volume, and bone scintigraphy or single-photon emission computed tomography (SPECT). Further diagnostics consist of: mandibular/head cephalometric radiography, cone beam computed tomography (CBCT), low dose computed tomography (LDCT), and magnetic resonance imaging (MRI) or positron emission tomography (PET) is also advised by some authors [31,32,33,34,35,36,37].
5.1. Panoramic Radiographs and Computed Tomography
First of all, the evaluation of routine panoramic radiographs can be essential for establishing the type and scope of other, more advanced diagnostics [37]. The shape and size of the mandibular ramus and condylar process in any case of mandibular asymmetry should be carefully evaluated for typical and atypical signs of condylar hyperplasia; however, the estimation of any asymmetry via classic radiographs has its limitations and should be used with special consideration [38]. Nevertheless, routine radiographs are fast and cheap diagnostic tools that are helpful in surgical planning, especially if they are compared and evaluated with cone beam/low-dose computed tomography studies (CBCT/LDCT) (Figure 3 and Figure 4). As suggested by some authors, after evaluation of routine panoramic radiographs, those radiographs can be useful only for screening as a “first glimpse of an eye diagnostics” [39]. When evaluated, symptoms such as the presence of a clear antegonial notch, the occurrence of an open bite on the affected site (canine/premolar area), a low downward position of the maxillary bone with tilting, an asymmetrical chin position towards the healthy side, a low-positioned mandibular canal and increased vertical ramus height, and other atypical ones are the most common ones for unilateral condylar hyperplasia’s quick and easy identification on routine panoramic radiographs as a basic screening procedure [37,38,39,40]. A similar study compared the usage of 3D cone beam computed tomography (CBCT) and routine panoramic radiographs in hemifacial microsomia (HFM/HCMF) and established that CT is superior to a classic radiograph, but both diagnostic methods are necessary for each case and the combination of the two is very important [38,40,41]. Nolte et al.’s study on the usage of panoramic radiographs in UCH indicated that the following diagnostic method is not sufficient for routine diagnostics and follow-up and should be used for the screening and evaluation of some of the atypical anatomies of the herein-mentioned UCH cases [41,42].
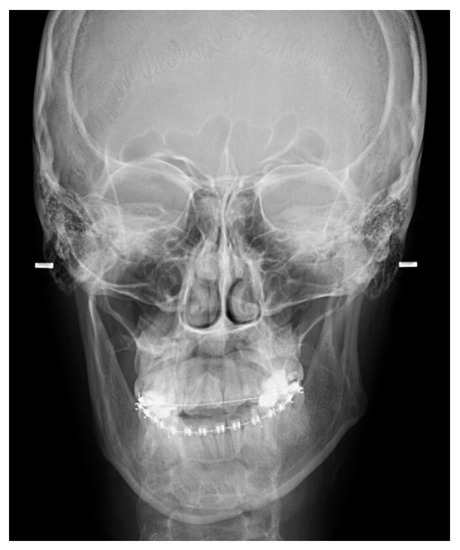
Figure 3.
A classical P-A mandible radiograph.

Figure 4.
LDCT coronal view on the condylar head. Notable bone osteosclerosis and right condyle head enlargement with ramus elongation are present.
Computed tomography (CT) is quite good and accurate enough to estimate the degree of mandibular asymmetry and condylar head shape and size, further improving diagnostics. Nowadays considered a gold standard, CT should always be evaluated with basic routine radiographs, which have many limitations. Furthermore, in CT, additional BD (bone density) and bone structure components might be measured and evaluated in 3D (Figure 4). Nolte et al.’s study on 37 UCH patients underlines that CBCT is the best method for surgical planning, objective patient monitoring, and evaluating the degree and scope of asymmetry, especially when the height of the mandibular ramus is comparable to the condylar and body segments of the affected side of the mandible [41,42]. Close measurements of the scope of mandibular overgrowth are essential for proper condylectomy planning and later orthognathic surgery, or the estimation of any definitive correction of mandibular asymmetry if still present after surgeries. A study by Sun et al. estimated how important CBCT is in the evaluation and estimation of mandibular condylar (MC)-related pathologies [43]. A comparison study on condylar hyperplasia, unilateral condylar hyperplasia (UCH), hemimandibular elongation (HE), solitary condylar hyperplasia (SCH), simple mandibular asymmetry (SMA), and condylar osteoma or osteochondroma (COS) indicated an increased volume of the ramus and mandibular body height and estimated that the two most accurate and specific symptoms in CBCT characteristic for UCH are the inferior convexity of the lower mandibular border and the inferiorly displaced mandibular canal [34,43,44]. It seems that the role of CBCT is crucial not only for surgical planning but also for the evaluation of MC head anatomy. Direct changes and appearances in the bone shape, size, and surface of the MC might also correspond with joint arthritis [44,45,46]. On the other hand, a close evaluation of the condyle head and entire asymmetric mandible in 3D CBCT also enables 3D printing and stereolithographic models and 3D-guided planning for any surgical intervention [31,45,46,47].
5.2. Scintigraphy and Growth Activity
When the first symptoms of asymmetry start to occur, detailed diagnostics should be used. Bone activity is measured in scintigraphy and/or single-photon emission computed tomography (SPECT studies), especially with the use of 99mTc-MDP because it enables the estimation of the accumulation of calcium components and bone hydroxyapatites [6,7]. Nuclear studies determine if the growth is still present (active bone growth,—AG+) or if the growth is not present or has ceased growing (growth lack and/or cessation,—GC−) (Figure 5). The difference in uptake levels might vary in each condyle and also be related to patients’ age, UCH growth, and even the occurrence of other factors, such as inflammations, tumors/pseudotumors, or surgery in close proximity to the condyle, which might lead to study inaccuracy. Some authors, such as Hodder et al. and Yang et al., suggest that differences of 10% in radionuclide uptake between both mandibular condyle heads indicate a bone pathology and signs of UCH [48,49]. Most importantly, at least two growth measurements should be taken before any other approach within a time frame of 6–12 months to estimate any changes in bone activity. The values of sensitivity and specificity vary greatly. Liu et al.’s study on SPECT accuracy in UCH in 249 retrospective cases indicated that the sensitivity of SPECT was 55.3% and the specificity was 48.6%, which is not very good [35]. These results underline that SPECT has major limitations and should not be used alone without any CT/CBCT/RTG, since 3D anatomical and morphological studies in MC and patients’ facial appearances are also very important [12,13,20,50,51]. Therefore, SPECT in UCH examinations has its limitations and should never be used alone as the main indicator for surgery, so additional diagnostics are mandatory. As suggested in the literature, a very advisable approach of “watch and wait” is reasonable enough for the estimation and prediction of this type of atypical and unpredictable bone disease, which UCH clearly is [31,32,33,34,35,48,49,50,51,52].
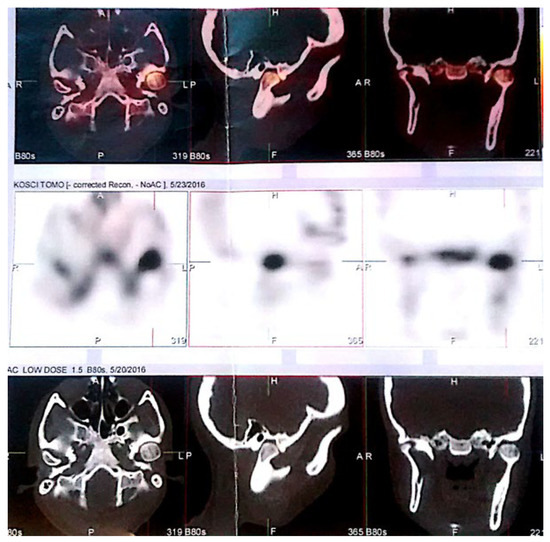
Figure 5.
SPECT evaluation of left side UCH. Presence of enlarged left condylar head with osteosclerosis, typical decrease in glenoid fossa space, and enlarged left ramus of the mandible. Abbreviations: L—left, R—right, H—head/up; F—foot/down, A—anterior, P—posterior.
Saridin et al.’s study established that bone scintigraphy and SPECT are important in condylar hyperplasia evaluation and diagnostics [53]. They are also burdened with a high amount of false positive results, especially in trauma cases or in the overloading of the joint, as mentioned by Pripatnanont et al. [51]. Since this pathology is mostly case-related, it is worth noting that several situations might be present (Table 1): (1) typical hemimandibular hyperplasia/unilateral condylar hyperplasia case with active/rapid pathological growth starting from childhood or young maturing adults; (2) a form which is self-limiting and ceases growth cessation over time (resulting in visible mandibular and facial asymmetry); (3) a case of slowly progressive growth over time with no limitation of age; (4) condyle head cases of rare benign/malignant tumors (described by Wolford et al.); (5) normal growth in the affected condyle, with the contralateral condyle hypoplastic with a lack of inappropriate growth; (6) other related condyle pathologies [30,54,55,56,57,58]. It seems that CT imaging is not only superior to a classical RTG, but it also has more value in surgical planning, while SPECT is helpful in the estimation of the presence of any pathological growth component affecting the condyle.
6. Dental Treatment
First of all, a detailed orthodontic evaluation is mandatory. Before any surgical intervention, the patient should have a dental check-up to decrease any potential sources of inflammation within the oral cavity [40,41,44]. When wisdom teeth ought to be removed and a SPECT evaluation is scheduled, it is mandatory to avoid any surgical interventions before nuclear imaging because of the risk of false positive results. Therefore, some authors decide to remove wisdom teeth when a condylectomy is scheduled or only after they are assured that no abnormal pathological growth is present. In some rare cases, when UCH becomes self-limiting over time, pathological growth is not present, and mandibular asymmetry is acceptable to the patient when confirming growth cessation, a detailed planned orthodontic approach can be used [1,2,3,4,5,6,7,8,9,10,36,37,38,59]. Scheduled dental treatment should focus on the teeth lining and the correction of the occlusion. Dental alignment, arch coordination, and incisor decompensation are important factors in post-condylectomy settings to prepare each patient for additional orthognathic surgery. Some surgeons prefer early orthodontics and, 1–2 months afterward, orthognathic surgery-first approach, while others prefer a classic orthodontic approach after the condylectomy which can last for 1–1.5 years (max 24 months), to ensure that after orthognathic surgery the best possible teeth alignment is secured. Last, but not least, after orthognathic surgery, final orthodontics might last for 6–8 months or even longer. In some cases, when orthodontic treatment is limited, a surgery-first approach is advisable. Long-lasting orthodontic preparation is related to poorer esthetics and a decrease in functional and morphological factors while waiting for orthognathic surgery [46,60,61,62,63].
Most clinicians prefer the standard concept of orthodontic treatment combined with later orthognathic surgery. In some cases, orthodontic treatment with condylectomy alone could also be sufficient for treating UCH. One of the recent papers by Luther et al. [64] presents a detailed three-step approach consisting of the following: (1) pre-surgery orthodontics for dental alignment, incisor decompensation, and arch coordination, (2) orthognathic surgery with splints and rigid fixation to correct the skeletal discrepancies, and (3) post-surgery orthodontics to set the occlusion [63,64,65]. This standard approach might last for a long period of time, while “surgery first” has more to offer in a shorter period of time, however, it also has some limitations. Some of them are related to unstable occlusion, inaccurate teeth alignment, longer periods of orthodontic treatment, and, in some cases, the necessity of teeth polishing and dental filling alignment/polishing to ensure a more stable occlusion after a surgery-first approach (Figure 6). An early surgery and orthodontics approach might have a good impact because of its fast results; however, this approach should not be considered in all cases, which also confirms that UCH is unpredictable in its outcomes of dentoalveolar discrepancies changes (Figure 7). A shorter time before early surgery and then orthognathic is a wise approach, especially in young patients where facial appearances are quite important for good interpersonal contacts, especially in schools [45,46,61,62,63,66].
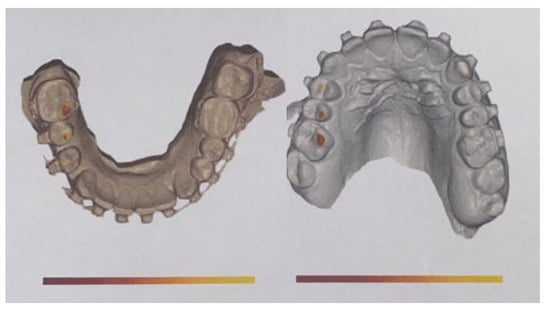
Figure 6.
During preparation for surgery, premature or incorrect dental contacts in 3D planned models are easily highlighted and can be adjusted during surgery with diamond burrs to improve the occlusion and the final result. Some occlusal collisions can be easily removed before the surgery, while others require better correction intraoperatively.
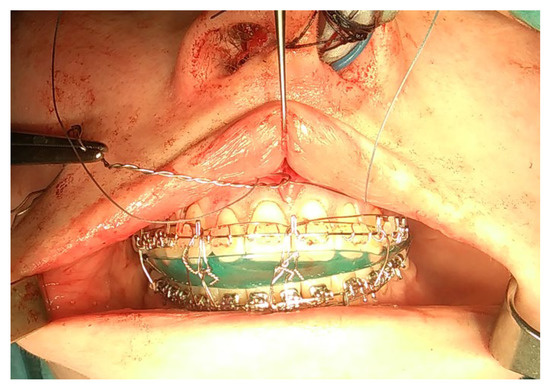
Figure 7.
An intraoperative view of occlusion. Because of maxillary plane deviation, at first, it was necessary to secure a good and proper symmetrical position of the maxillary bone. A proper alignment of dental arches enables good final preparation for orthognathic surgery. The time of wisdom teeth removal should be scheduled for at least 6 months before the main procedure, which is necessary for bone healing and enables good preparation for the final procedure. An acrylic surgical plate guide is necessary to establish a good final occlusion during any orthognathic surgery.
A study by El Mozen et al. compared two groups studied directly after a condylectomy in UCH, consisting of those who used postsurgical orthodontic therapy just after surgery and those who did not undergo orthodontic therapy. The authors conclude that orthodontics helped in restoring the midline symmetry line, promoted alveolar and condylar remodeling, and more directly influenced proper occlusion correction than spontaneous in situ remodeling without orthodontics [65]. Li et al.’s retrospective study on 47 patients described a new method of UCH treatment with the combination of additional miniscrews implanted the infrazygomatic crest and hard palate to intrude the affected side of maxillary molars and apply intermaxillary traction for contralateral molars. This step was measured in CBCT and resulted in a great outcome in reducing the chin deviation, canting of the mandibular-maxillary occlusal plane, and improving molar torque [67]. As described herein, the orthodontic approach was suitable for UCH vertical-type and a combination of vertical–horizontal type, but not sufficient in the orthodontic approach for the horizontal-type UCH.
7. Treatment from Surgeons’ Perspective
Before any surgery is taken into consideration, it is necessary to remember that each case is individual and has various factors that might affect surgical planning. First of all is the necessity of additional orthodontic or dental treatment, and second is the patient’s willingness to undergo the full scope of treatment or just a conservative camouflage approach [8,19,28,29,30,38,50,57,58,65,68,68,69,70,71,72]. The degree and scope of surgical interventions are related to the facial changes present in UCH patients [73]. In cases of active UCH or its inactive forms, there are a lot of possible surgical approaches that could be used. Before any surgical or conservative treatments are scheduled, the patient’s willingness to undergo an extensive surgical approach is mandatory. In cases where patients’ symmetry and lack of facial balance are acceptable to patients, conservative orthodontic treatment can be scheduled. In cases with troublesome asymmetries resulting in a lack of facial balance, decreased speech, and masticatory and bite functions, the non-conservative approach should be taken. The time of full surgical intervention should include fully grown patients; however, the condylectomy can be performed at any age of the patient, even those still growing, since condylectomy is a treatment of choice [26,27,28,29,30,50,57,58,68,69,70,71,72,74,75,76].
7.1. Condylectomy
A condylectomy procedure can be performed using various methods. It is the first and most important surgical approach in cases of active pathological growth in the affected condyle. After achieving a good result within the affected joint, other methods and possibilities for treatment might vary greatly [17,63,75,77]. After a condylectomy, the bony stump can be left in situ or smoothed and resutured with the pterygoid muscles. Various techniques exist. Other factors concern the response to a serious question: whether the bony stump with sharp edges should be smoothed or left intact to reorganize itself [63,75]. In both articles, condylar remodeling was observed and manifested by the smoothening of the condylar surface and the return of the condyle to its normal position in the glenoid fossa. It was concluded that high condylectomy in the treatment of active CH of TMJ improved the functional occlusion and facial aesthetic. Each method should be included in patients’ treatment when the condyle abnormality is stable and controlled [30,32,78].
In almost all cases, there is only one accurate method for the total removal of the pathological growth in the affected condyle. A condylectomy performed in one of the possible approaches is the method of choice. The removal of the most superior part of the condyle head with parts of the surrounding cartilage attached to the bone is widely performed. Other growth-arresting procedures in this type of pathology are not found or known, especially since condylectomy is a well-known, widespread, and well-described technique. A second approach in each MA related to UCH is well-defined monitoring of the growth (SPECT, RTG-PANX, CBCT/LDCT) every 6–12 months to establish if the growth is still present, active, or perhaps is in an ending decreased phase.
The condylectomy procedure, performed in one of the known modalities, might lead to various outcomes (Table 1): (1) the condylectomy removes the pathological growth, and the patient is scheduled for a second surgical procedure for corrective/orthognathic surgery (two-step); (2) the condylectomy is one surgery combined with orthognathic surgery; (3) the condylectomy results in total symmetry correction and patient’s bite/occlusion is not a problem for the patient; (4) the condylectomy results in total symmetry correction but patient still requires additional orthodontics or orthognathic surgery; (5) the condylectomy is performed first with early orthodontics to remove pathological growth in cases of severe asymmetry with maxillary deviated bite plane and secondary asymmetry; (6) condylectomy enables some type of rotation of the mandible towards the overgrowth resected area which causes the mandible to rotate in skeletal class II or class III features; (7) the condylectomy with surgery first approach is performed to improve the time of treatment, especially in young patients with visible lack of facial esthetics; (8) an increased necessity for a corrective genioplasty or other known techniques for definitive mandibular asymmetry correction (Table 1) [79].
After one of the condylectomy procedures is chosen as preferable for a unilateral condylar hyperplasia case, detailed diagnostics are necessary. First of all, establish if the pathology is condylar hyperplasia, or perhaps is a different pathology, such as osteochondroma (OC), osteoma, chondroma, and osteoblastoma, or if any other possible malignant (chondrosarcoma and osteosarcoma) or metastatic co-existing features are present [19,43,79].
Based on the following diagnostic approaches, one of the types of condylectomy approaches can be used. There are a few known and used condylectomy techniques worth remembering and understanding:
- (1)
- High condylectomy, Lippold et al.: excision of 4–5 mm of bone from the superior condyle pole is enough when this amount of bone is cut vertically from the lateral to medial pole [80,81,82]. High condylectomy as a sole operative treatment might be sufficient in some cases of UCH. The use of orthodontic treatment is suitable for some small or mild cases of overgrowth. The problem remains crucial when there are differences in the ramus vertical height and maxillary asymmetry with their own growth on the affected side of UCH [83,84,85].
- (2)
- Low condylectomy: dedicated to removing a larger volume of MCH with just the far inferior part left alone. On the other hand, Wolford et al.’s study on 37 UCH-2 (osteochondroma of mandibular condylectomy associated with mandibular deformity) patients used a low condylectomy approach in all patients with recontouring of the condylar neck to form a new condyle, repositioning of the articular disc over the condylar stump, and repositioning of the contralateral disc if any symptoms of displacement or malposition might occur, and any indicated orthognathic surgical procedures [6,75,86]. Further, follow-ups concluded that low condylectomy and orthognathic surgery improved not only TMJ function and proper joint movements but reduced any pain or other related symptoms [29,87,88,89].
- (3)
- A total condylectomy procedure (TCP) is rarely used in UCH and is mostly dedicated to condyle tumors, such as osteochondromas (OC). Domingues et al., after total condylectomy for condyle repair, used a costochondral graft and preserved the articular disc with good outcomes. Some authors advise leaving the resected condyle in the joint without reconstruction or suturing with pterygoid muscles only or using other modifications [13,90,91]. The neocondyle condyle might be unstable for quite some time, and patient education on chewing, biting, diet, and other factors is necessary.
- (4)
- Proportional condylectomy is a special technique that compares the head and ramus’s vertical and horizontal diameters to ensure a more balanced result after the procedure, and therefore this amount of condyle is excised. Mouallem et al.’s retrospective study on 73 patients with UCH was divided into vertical (61.6%) and transversal (38.4%) forms of UCH according to Delaire’s classification [92]. Using proportional condylectomy in the authors’ approach, followed by indicated orthognathic techniques, maxilla–mandibular elastic therapy, and rehabilitation, is a good, accurate, and reliable option for treating UCH, regardless of the activity status of the pathology [93].
- (5)
- Condylar head reshaving and modeling with bone drills, chisels, and piezosurgery (the most superior part of the MCH) [94].
- (6)
- Transoral approach. This might include techniques with mandibular coronoid process osteotomy to gain more visibility toward the condyle, as reported by Choung et al. [95]. A similar approach to the intraoral approach was described by Wang et al., which might be combined with coronoid process resection and an IVRO procedure–intraoral vertical ramus osteotomy [96,97]. Approaches with computer-guided/3D navigation techniques can also be useful. The intraoral approach for a condylectomy is challenging and can be used in various technique alternations. Some authors combine it with a coronoidectomy, while others combine it with temporal coronoid process osteosynthesis to improve access to the MC. The presented method by Deng et al. described new insights into accurate and safe intraoral approaches [98]. The endoscopic-assisted transoral approach is a similar approach and technique used for intraoral condyle fracture osteosynthesis after fractures and can also be used with a great deal of success to improve intraoral condylectomy [99,100,101].
- (7)
- Three-dimensional-guided and similar planning guides: Cascone et al. introduced the usage of 3D mandible and skull cast models based on CBCT to establish the best methods of surgical planning on 3D printed models [102]. The herein-mentioned planning on two cases indicates that proportional condylectomy might be used as the sole procedure for UCH treatment when detailed measurements on 3D models, either virtual or printed, are used to improve the surgical outcomes [103,104].
- (8)
- Conservative condylectomy is another type of condylectomy that includes a conservative approach. Kim et al.’s study on five patients concludes that a conservative condylectomy without any additional orthognathic surgery should include the presence of the vertical height of the condylar process [105]. Additional intermaxillary fixation and elastics are necessary to maintain a stable outcome. Additional orthodontic treatment is also reported to be a valuable and accurate method if condylectomy is the sole procedure [86,106,107].
- (9)
- Other perspectives include head shaving, remodeling, and reshaping into desired forms, but these are rarely known or used. On the other hand, the condylar head after condylectomy might be influenced by many remodeling forces, both from inside and outside the joint. A recent article by Rojare et al. evaluated condyles in CT and expressed that condyle shape and size after a condylectomy might vary greatly [108]. Secondly, the authors reported that all operated condyles developed new cortical bone, and some type of visible glenoid fossa thickening was also present. The scope of the removed volume of the condyle is mostly case- and growth-related [109].
Based on the following, condylectomy is necessary (Figure 8). The scope of surgical condyle excision influences later post-surgical outcomes and the treatment that could be implemented. The herein-mentioned modalities and alternatives of condylectomy approaches are usually related to the cases’ and surgeons’ preferences. Nolte et al. [110] point out that, after a condylectomy, a number of cases can be easily treated and finalized with proper orthodontics, without any additional surgeries, which points out the fact that not all patients require orthognathic surgery.

Figure 8.
Intraoperative view on low condylectomy with modified pterygoid muscle re-attachment via a classic preauricular approach.
7.2. Further Surgical Steps
Despite the knowledge of the principles of orthognathic surgery and each modification of the condylectomy procedure, the treatment of each case of UCH can still be performed in various ways. The main aspects involved in selecting the most sufficient method of treatment should address the following topics: (1) scope of dentoalveolar discrepancies; (2) vertical ramus height and their disproportions; (3) degree of maxillary tilting on the affected side; (4) presence of an open bite; (5) patient’s willingness to undergo the full osteotomy protocol or camouflage surgery; (6) if the type of condylectomy procedure is performed as a sole procedure or with the combination of orthognathic surgery; (7) the volume and scope of mandibular overgrowth and the necessity for genioplasty, chin-wing osteotomy, or other future total symmetry correction of the asymmetrical lower mandibular margins; (8) patient’s age and the possibilities of early or late orthodontic treatment; (9) presence and position of retained wisdom teeth and the timing for their removal; (10) what are the main patient’s goals and wishes? To improve esthetics, function, symmetry, quality of life, or other important topics [26,27,28,29,30,68,69,70,75,76,111,112].
The indications for choosing a one-stage treatment are mostly related to the scope of malocclusion and the degree of overgrowth. Simultaneously performed condylectomy and orthognathic surgery has good outcomes; however, the unstable joint syndrome after condylectomy and the necessity for early orthodontics are demanding. Two-stage orthognathic surgery is focused firstly on condylectomy, and later on, orthognathic surgery, when the entire joint is entirely healed and stable, and good orthodontics grants full osteotomy protocol during mostly surgery consisting of Lefort I and BSSO osteotomies [75,76,77,113,114]. In Table 1, the authors’ proposed algorithm is presented (Table 1).
The main goal is to achieve proper symmetry and a balanced profile. This can be achieved in various ways and methods. Most authors focus on the importance of condylectomy as a gold standard. From there, either orthodontic treatment leads to finalizing the treatment or the patient must be prepared for a total osteotomy protocol, namely, orthognathic surgery. Other treatment modalities might consist of one-stage surgery or two-stage surgery.
A condylectomy is one of the possible surgical interventions that can be used simultaneously after a condylectomy or only after major orthodontic treatment to ensure a good, stable occlusion. It is mandatory to perform any surgical intervention only after fully treating the condyle abnormal growth or after ensuring that the growth is not present [75,76,77,113,114].
- (1)
- Mandibular ramus osteotomy on the affected condyle’s side (unilateral osteotomy) suggested by Motamedi, 1996 [114]: this is a simple and accurate method; however, the rotation of the unaffected condyle might become troublesome;
- (2)
- Condylectomy followed by a surgery-first approach after a month (SFA) suggested by Lopez et al., 2017 [115]: when patients benefit from achieving a balanced facial profile faster without any orthodontic approach, which is mostly scheduled after the surgery in a short period of time;
- (3)
- Orthognathic surgery: BSSO or BSSO with Lefort I on severely asymmetric maxillary and mandibular bones with a prognathic profile and open bite [116];
- (4)
- BSSO with Ferguson modification [117]: for achieving a more balanced chin and lower mandibular border symmetry;
- (5)
- Only BSSO or Lefort I, depending on the scope of asymmetry and profile changes after condylectomy [84];
- (6)
- A condylectomy with BSSO and Lefort I simultaneously was described by Wolford in 2002; however, some authors report operated TMJ joint instability, which might be related to the degree of excised bone and poor condyle stabilization with at least lateral pterygoid muscle reattachment or other, perhaps even related with IMF intramaxillary fixation devices to stabilize the occlusion [75] (Figure 9);
- (7)
- Surgical camouflage such as marginectomy, chin shift procedure, bone osteomodeling, or basic orthognathic surgery in cases of UCH growth cessation/growth end [118];
- (8)
- After corrective condylectomy, no approach at all: either due to the patient’s unwillingness to undergo any additional osteotomies or perhaps as there is no need for surgery because the dentoalveolar disproportions are minor [105,118,119,120];
- (9)
- Corrective genioplasty or its modalities [78,121,122,123,124];
- (10)
- A modification of a wing osteotomy, suggested by Wenghoefer et al., describing a chin-wing osteotomy to restore the balance of the inferior border of the mandible [121];
- (11)
- Other definitive procedures for total symmetry correction [117,118].
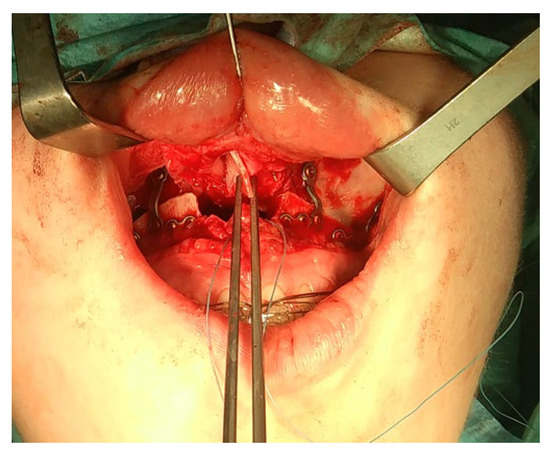
Figure 9.
Intraoperative view after Lefort I stable osteosynthesis and nasal septum positioning after septoplasty and conchoplasty reduction procedure.
In a recently described article on a surgery-first approach (SFA—surgery-first approach) presented by López et al., after a condylectomy procedure, the second step was performed after just one month. In the described case by López, an orthognathic jaw impaction and asymmetric mandibular setback surgery can be used with a high success rate [125]. Later, after 10 days, orthodontic appointments were made and consisted of 14 months of active-phase treatment. The authors reported that after 24 months, good and stable occlusal outcomes were achieved. The main goal of SFA is the early correction of facial asymmetry (a more balanced profile, more symmetrical lips, and improved treatment time), which enables good surgical outcomes; however, later on, extensive orthodontic treatment is necessary. This reduction in treatment reported by López et al. is related to the regional acceleration phenomenon (RAP—rapid bone remodeling and regional loss of bone density) since dental disproportions are partly or mostly corrected after bone surgical osteotomies [125]. Other types of mandibular body or ramus osteotomies are possible but are rarely used.
All of the mentioned surgical procedures require some detailed surgical planning. In order to evaluate facial soft tissue and bone contour and plan for the best possible outcome, a detailed 3D analysis based on CBCT and 3D patient dental scans is necessary. There is a great variety of different software and possible methods for orthognathic planning (Figure 10, Figure 11 and Figure 12). Describing any possible software and types of planning methods exceeds the scope of the following review and will not be presented.
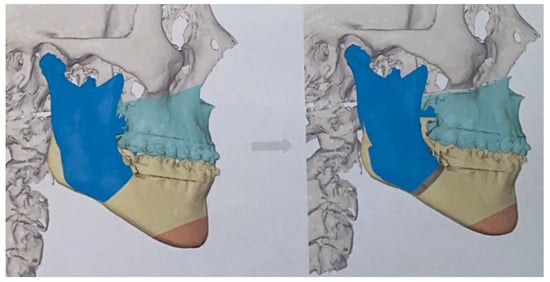
Figure 10.
Virtual planning in orthognathic surgery for UCH patients based on IPS CaseDesigner® (KLS Martin Group, KLS Martin, Tuttlingen, Germany).
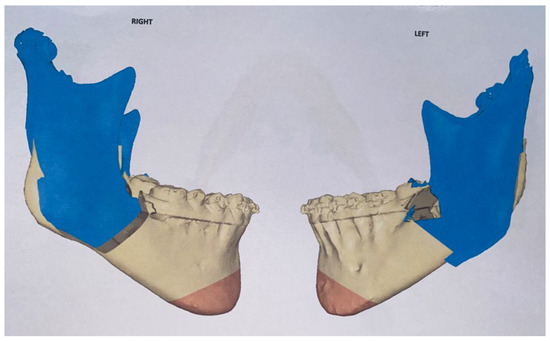
Figure 11.
Virtual planning for BSSO approach.
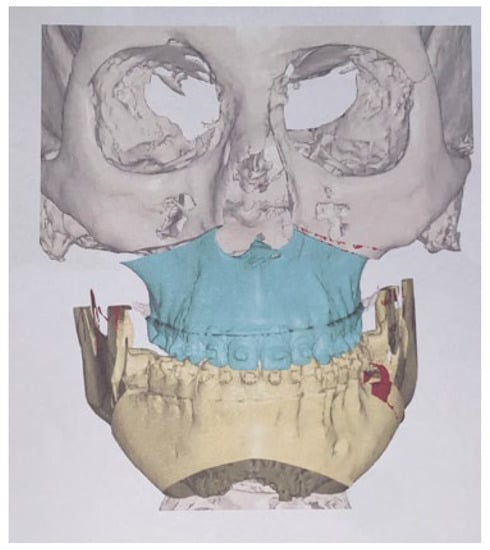
Figure 12.
Virtual 3D model and a surgical guide.
8. Clinical Outcome
In order to maintain a safe patient follow-up routine, radiological and clinical evaluations are necessary. Before any surgical intervention, at least two scintigraphic measurements are necessary. For condylectomy, not only a SPECT/CT but also a CT/CBCT-3D with a panoramic radiograph is necessary. After a condylectomy, either a low-dose CT or panoramic radiograph can be used for MC evaluation closely after surgery. The scope and timing of orthodontics can be estimated as an early approach at one month after surgery or late orthodontics after gaining proper joint movement and an accurately healed TMJ. CBCT remains a quick and accurate radiological approach to establishing 3D remodeling of the affected MC after a condylectomy, which is also confirmed by Verhelst et al.’s study, especially if two CBCTs from before and after surgery are overlapped and closely evaluated together for surface modeling [126]. Clinically, a good, stable condylar head position with sustained lateral excursions and protrusion movements is considered a good outcome. Secondly, improved occlusion, bite, and symmetry are also necessary. In some cases of extensive osteotomies, careful patient monitoring grants a suitable visualization of the final outcomes. In some cases of severe bone discrepancies, a final procedure consisting of definitive correction of the chin, mandibular base, and angular regions can be used. The following procedure should be performed six months after orthognathic surgery and combined with plate removal after orthognathic surgery. The main goal of such a definitive procedure should focus on restoring the harmony of the lower mandibular basis, vertical ramus height, and chin symmetry. In some cases, when patients are satisfied with the results after orthognathic surgery, their lack of symmetry and balance is not an issue for them.
The monitoring and assessment of patients should consist of surgical checkups every 3–6 months and orthodontic evaluations each month in the first year of the surgery, followed by a 3-month time frame to ensure a good final outcome and avoid any unnecessary complications, wound inflammation, or bone instability [39,118,127].
First, the most important issue is related to the restoration of a symmetrical and balanced facial appearance. In some cases of severe overgrowth and asymmetry, a condylectomy and orthognathic surgery might not be enough. Therefore, in some rare cases, an additional third surgery can also be used. It is appropriate to correlate the third surgery with the titanium plate removal and combine it with a total asymmetry correction protocol. This might include various camouflage surgeries to reduce the overgrowth of mandibular bones and reshape the facial contour (Figure 13) (Table 1).

Figure 13.
Some results could be still unsatisfactory because of the lack of chin and lower border of the mandible harmony. In those cases, during plate removal after orthognathic surgery, it is relatively easy to combine a definitive mandibular correction procedure with titanium miniplate removal.
The second serious issue concerns stability after the surgery. These results can be related to factors concerning the orthodontic camouflage treatment, maintaining adequate occlusion, good temporomandibular joint stability after condylectomy, and orthognathic surgery outcomes concerning proper bone alignment and symmetry. All of the following require detailed case evaluations and will be presented in future studies.
9. Conclusions
The final outcomes from a combined surgical and orthodontic approach to condylar hyperplasia are relatively good. The overall success rate is greatly related not only to the scope and degree of asymmetry but also to the use of surgical protocols and the timing of orthodontics. The main indications for one of the used approaches should include: the patient’s age, the vertical ramus height, the occurrence of an open bite, and the lack of facial balance. The choice of surgery-first, one-step surgery, or two-step surgery procedures is mostly individually set. Condylectomy is necessary in the majority of cases. A high condylectomy of the far superior part of the affected condyle followed by elastic wires remains a good approach. For now, it is impossible to establish a classification for MCH because there are many variables affecting each patient. It should be highlighted that SPECT should always be compared with CBCT/LDCT for the estimation of the affected condylar head bony structure. It seems that we did not find any adequate algorithm that corresponds to the patients’ age, dentoalveolar discrepancies, growth ratio in the affected condyle, and scope of maxilla-mandibular bite plane deviations. Yet, so far, condylar hyperplasia remains within the scope of many studies because of its impact on each patient’s facial characteristics. The two most important issues requiring further study are a protocol for total asymmetry correction and the description of a method for evaluating good stability and outcomes from the presented combined orthodontic–surgical approach.
Author Contributions
Conceptualization, K.N.; methodology, K.N. and K.Ł.; software, M.J.; validation, K.N., E.P. and W.P.; formal analysis, K.N.; investigation, K.N.; resources, K.Ł. and M.M.-K.; data curation, M.J. and M.D.; writing—original draft preparation, K.N., K.Ł., B.B. and T.B.; writing—review and editing, W.P. and M.M.-K.; visualization, K.N.; supervision, K.Ł.; project administration, M.J., M.D. and E.P.; funding acquisition, M.J., E.P. and M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financed by a subsidy from Wroclaw Medical University, number SUBZ.B180.23.054.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and the approval for studies UMW 616/2016.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study.
Data Availability Statement
The datasets used in the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Obwegeser, H.L.; Makek, M.S. Hemimandibular Hyperplasia—Hemimandibular Elongation. J. Maxillofac. Surg. 1986, 14, 183–208. [Google Scholar] [CrossRef]
- Rodrigues, D.B.; Castro, V. Condylar Hyperplasia of the Temporomandibular Joint: Types, Treatment, and Surgical Implications. Oral Maxillofac. Surg. Clin. N. Am. 2015, 27, 155–167. [Google Scholar] [CrossRef]
- Chia, M.S.; Naini, F.B.; Gill, D.S. The Aetiology, Diagnosis and Management of Mandibular Asymmetry. Orthod. Updat. 2008, 1, 44–52. [Google Scholar] [CrossRef]
- Madrid, J.R.P.; Montealegre, G.; Gomez, V. A New Classification Based on the Kaban’s Modification for Surgical Management of Craniofacial Microsomia. Craniomaxillofac. Trauma. Reconstr. 2010, 3, 1–7. [Google Scholar] [CrossRef]
- Wink, J.D.; Goldstein, J.A.; Paliga, J.T.; Taylor, J.A.; Bartlett, S.P. The Mandibular Deformity in Hemifacial Microsomia: A Reassessment of the Pruzansky and Kaban Classification. Plast. Reconstr. Surg. 2014, 133, 174e–181e. [Google Scholar] [CrossRef]
- Wolford, L.M.; Movahed, R.; Perez, D.E. A Classification System for Conditions Causing Condylar Hyperplasia. J. Oral Maxillofac. Surg. 2014, 72, 567–595. [Google Scholar] [CrossRef]
- Bishara, S.E.; Burkey, P.S.; Kharouf, J.G. Dental and Facial Asymmetries: A Review. Angle Orthod. 1994, 64, 89–98. [Google Scholar] [CrossRef]
- Reyneke, J.P. Orthognathic Essentials of Surgery: Second Edition; Quintessence Books: Chandler Drive, IL, USA, 2010. [Google Scholar]
- Iyer, J.; Hariharan, A.; Cao, U.M.N.; Tran, S.D. Acquired Facial, Maxillofacial, and Oral Asymmetries—A Review Highlighting Diagnosis and Management. Symmetry 2021, 13, 1661. [Google Scholar] [CrossRef]
- Andrade, N.N.; Mathai, P.; Aggarwal, N. Facial Asymmetry. In Oral and Maxillofacial Surgery for the Clinician; Bonanthaya, K., Panneerselvam, E., Manuel, S., Kumar, V.V., Rai, A., Eds.; Springer Nature: Singapore, 2021; pp. 1549–1576. ISBN 9789811513466. [Google Scholar]
- Almeida, L.E.; Zacharias, J.; Pierce, S. Condylar Hyperplasia: An Updated Review of the Literature. Korean J. Orthod. 2015, 45, 333–340. [Google Scholar] [CrossRef]
- Raijmakers, P.G.; Karssemakers, L.H.E.; Tuinzing, D.B. Female Predominance and Effect of Gender on Unilateral Condylar Hyperplasia: A Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2012, 70, e72–e76. [Google Scholar] [CrossRef]
- Nelke, K.H.; Pawlak, W.; Morawska-Kochman, M.; Łuczak, K. Ten Years of Observations and Demographics of Hemimandibular Hyperplasia and Elongation. J. Craniomaxillofac. Surg. 2018, 46, 979–986. [Google Scholar] [CrossRef]
- Mahajan, M. Unilateral Condylar Hyperplasia—A Genetic Link? Case Reports. Natl. J. Maxillofac. Surg. 2017, 8, 58–63. [Google Scholar] [CrossRef]
- Yang, J.; Lignelli, J.L.; Ruprecht, A. Mirror Image Condylar Hyperplasia in Two Siblings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2004, 97, 281–285. [Google Scholar] [CrossRef]
- Portelli, M.; Gatto, E.; Matarese, G.; Militi, A.; Catalfamo, L.; Gherlone, E.; Lucchese, A. Unilateral Condylar Hyperplasia: Diagnosis, Clinical Aspects and Operative Treatment. A Case Report. Eur. J. Paediatr. Dent. 2015, 16, 99–102. [Google Scholar]
- Mehrotra, D.; Dhasmana, S.; Kamboj, M.; Gambhir, G. Condylar Hyperplasia and Facial Asymmetry: Report of Five Cases. J. Maxillofac. Oral Surg. 2011, 10, 50–56. [Google Scholar] [CrossRef]
- Singh, V.; Verma, A.; Attresh, G.; Batra, J. Ortho-Surgical Management of Condylar Hyperplasia: Rare Case Reports. Natl. J. Maxillofac. Surg. 2014, 5, 54–59. [Google Scholar] [CrossRef]
- Ma, X.; Wang, H.; Zhang, X. [Orthognathic surgery in the treatment of condylar osteochondroma]. Hua Xi Kou Qiang Yi Xue Za Zhi 2014, 32, 150–152. [Google Scholar] [CrossRef]
- Fisch, A.W.; Espinosa, C.I.; Quezada, S.R. Facial Asymmetry Secondary to Mandibular Condylar Hyperplasia. A Case Report. Rev. Odontol. Mex. 2011, 15, 251–256. [Google Scholar]
- Brionne, C.; Cadre, B.; Laroche, Y.; Lhotellier, J.; Maze, M.; Raffre, A.; Sorel, O. The Diagnosis of Mandibular Assymmetries. J. Dentofac. Anom. Orthod. 2013, 16. [Google Scholar] [CrossRef]
- Alyamani, A.; Abuzinada, S. Management of Patients with Condylar Hyperplasia: A Diverse Experience with 18 Patients. Ann. Maxillofac. Surg. 2012, 2, 17–23. [Google Scholar] [CrossRef]
- Arora, K.S.; Bansal, R.; Mohapatra, S.; Pareek, S. Review and Classification Update: Unilateral Condylar Hyperplasia. BMJ Case Rep. 2019, 12, e227569. [Google Scholar] [CrossRef]
- Nitzan, D.W.; Katsnelson, A.; Bermanis, I.; Brin, I.; Casap, N. The Clinical Characteristics of Condylar Hyperplasia: Experience with 61 Patients. J. Oral Maxillofac. Surg. 2008, 66, 312–318. [Google Scholar] [CrossRef]
- Khawaja, S.N.; Crow, H.; Gonzalez, Y. Goldenhar Syndrome and Pain-Related Temporomandibular Disorders. A Case Report. N. Y. State Dent. J. 2016, 82, 21–24. [Google Scholar]
- GN, S.; Sharma, M.L.; JK, D.R.; Goel, S.; Srivastava, S. Facial Asymmetry in Young Adults with Condylar Hyperplasia-Unusual Changes in the Facial Bones. J. Clin. Diagn. Res. 2015, 9, ZD21–ZD23. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, H.K.; Kim, S.S.; Jarrahy, R.; Bradley, J.P. Differential Diagnosis of the Idiopathic Laterally Deviated Mandible. Plast. Reconstr. Surg. 2009, 124, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- De Stefano, A.A.; Di Chicco, A.; Alessandra, I.; Emanuela, S.; Guercio-Mónaco, E.; Galluccio, G. Unilateral Condylar Hyperplasia: A Thee-Dimensional CBCT Morphometric and Volumetric Evaluation of Mandibular Condyle by Open-Source Softwares. Int. J. Morphol. 2021, 39. [Google Scholar] [CrossRef]
- Fariña, R.; Bravo, R.; Villanueva, R.; Valladares, S.; Hinojosa, A.; Martinez, B. Measuring the Condylar Unit in Condylar Hyperplasia: From the Sigmoid Notch or from the Mandibular Lingula? Int. J. Oral Maxillofac. Surg. 2017, 46, 857–860. [Google Scholar] [CrossRef]
- Olate, S.; Cantín, M.; Alister, J.P.; Uribe, F.; Navarro, P.; Olate, G.; de Moraes, M. Relationship Between Condylar Size and Transverse Facial Asymmetry in Subject with Condylar Hyperplasia. Int. J. Morphol. 2013, 31, 937–941. [Google Scholar] [CrossRef]
- Saridin, C.P.; Raijmakers, P.; Becking, A.G. Quantitative Analysis of Planar Bone Scintigraphy in Patients with Unilateral Condylar Hyperplasia. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, 259–263. [Google Scholar] [CrossRef]
- Olate, S.; Netto, H.D.; Rodriguez-Chessa, J.; Alister, J.P.; de Albergaria-Barbosa, J.; de Moraes, M. Mandible Condylar Hyperplasia: A Review of Diagnosis and Treatment Protocol. Int. J. Clin. Exp. Med. 2013, 6, 727. [Google Scholar]
- Di Luzio, C.; Caputo, M.; Favale, M.L.; Bellisario, A.; Squillace, F. Spect Bone Scintigraphy in the Diagnosis of Unilateral Condylar Hyperplasia: A Systematic Review. 2017. Available online: https://www.webmedcentral.com/article_view/5377 (accessed on 12 November 2022).
- Saridin, C.P.; Raijmakers, P.G.; Tuinzing, D.B.; Becking, A.G. Bone Scintigraphy as a Diagnostic Method in Unilateral Hyperactivity of the Mandibular Condyles: A Review and Meta-Analysis of the Literature. Int. J. Oral Maxillofac. Surg. 2011, 40, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Shi, J. Growth Trends Analysis of Unilateral Condylar Hyperplasia Followed up with Planar Scintigraphy. Medicine 2021, 100, e28226. [Google Scholar] [CrossRef] [PubMed]
- Higginson, J.A.; Bartram, A.C.; Banks, R.J.; Keith, D.J.W. Condylar Hyperplasia: Current Thinking. Br. J. Oral Maxillofac. Surg. 2018, 56, 655–662. [Google Scholar] [CrossRef]
- Kambylafkas, P.; Murdock, E.; Gilda, E.; Tallents, R.H.; Kyrkanides, S. Validity of Panoramic Radiographs for Measuring Mandibular Asymmetry. Angle Orthod. 2006, 76, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Van Elslande, D.C.; Russett, S.J.; Major, P.W.; Flores-Mir, C. Mandibular Asymmetry Diagnosis with Panoramic Imaging. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 183–192. [Google Scholar] [CrossRef]
- Nelke, K.; Łuczak, K.; Janeczek, M.; Pasicka, E.; Barnaś, S.; Dobrzyński, M. What Features on Routine Panoramic Radiographs Could Help Orthodontists to Estimate the Occurrence of Condylar Hyperplasia from Other Mandibular Asymmetries—Retrospective Analysis Study. Symmetry 2022, 14, 1287. [Google Scholar] [CrossRef]
- Takahashi-Ichikawa, N.; Susami, T.; Nagahama, K.; Ohkubo, K.; Okayasu, M.; Uchino, N.; Uwatoko, K.; Saijo, H.; Mori, Y.; Takato, T. Evaluation of Mandibular Hypoplasia in Patients with Hemifacial Microsomia: A Comparison between Panoramic Radiography and Three-Dimensional Computed Tomography. Cleft Palate Craniofac. J. 2013, 50, 381–387. [Google Scholar] [CrossRef]
- Nolte, J.W.; Karssemakers, L.H.E.; Grootendorst, D.C.; Tuinzing, D.B.; Becking, A.G. Panoramic Imaging Is Not Suitable for Quantitative Evaluation, Classification, and Follow up in Unilateral Condylar Hyperplasia. Br. J. Oral Maxillofac. Surg. 2015, 53, 446–450. [Google Scholar] [CrossRef]
- Nolte, J.W.; Verhoeven, T.J.; Schreurs, R.; Bergé, S.J.; Karssemakers, L.H.E.; Becking, A.G.; Maal, T.J.J. 3-Dimensional CBCT Analysis of Mandibular Asymmetry in Unilateral Condylar Hyperplasia. J. Craniomaxillofac. Surg. 2016, 44, 1970–1976. [Google Scholar] [CrossRef]
- Sun, R.; Sun, L.; Sun, Z.; Li, G.; Zhao, Y.; Ma, X.; Sun, C. A Three-Dimensional Study of Hemimandibular Hyperplasia, Hemimandibular Elongation, Solitary Condylar Hyperplasia, Simple Mandibular Asymmetry and Condylar Osteoma or Osteochondroma. J. Craniomaxillofac. Surg. 2019, 47, 1665–1675. [Google Scholar] [CrossRef]
- Cavagnetto, D.; Abate, A.; Caprioglio, A.; Cressoni, P.; Maspero, C. Three-Dimensional Volumetric Evaluation of the Different Mandibular Segments Using CBCT in Patients Affected by Juvenile Idiopathic Arthritis: A Cross-Sectional Study. Prog. Orthod. 2021, 22, 32. [Google Scholar] [CrossRef] [PubMed]
- Hatamleh, M.M.; Yeung, E.; Osher, J.; Huppa, C. Novel Treatment Planning of Hemimandibular Hyperplasia by the Use of Three-Dimensional Computer-Aided-Design and Computer-Aided-Manufacturing Technologies. J. Craniofac. Surg. 2017, 28, 764–767. [Google Scholar] [CrossRef] [PubMed]
- Rizwana, A.; Mohan, N.; Kumar, P.T.R.; Karthik, R.; Gokulraj, S. Panoramic Radiograph and CBCT in Unilateral Mandibular Condylar Hyperplasia—A Case Report. Indian J. Radiol. Imaging 2021, 31, 1070–1074. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, E.; Kansu, Ö.; Özgen, B.; Akçiçek, G.; Kansu, H. Radiographic Manifestations of the Temporomandibular Joint in a Case of Proteus Syndrome. Dentomaxillofac. Radiol. 2013, 42, 58444855. [Google Scholar] [CrossRef]
- Hodder, S.C.; Rees, J.I.; Oliver, T.B.; Facey, P.E.; Sugar, A.W. SPECT Bone Scintigraphy in the Diagnosis and Management of Mandibular Condylar Hyperplasia. Br. J. Oral Maxillofac. Surg. 2000, 38, 87–93. [Google Scholar] [CrossRef]
- Yang, Z.; Reed, T.; Longino, B.H. Bone Scintigraphy SPECT/CT Evaluation of Mandibular Condylar Hyperplasia. J. Nucl. Med. Technol. 2016, 44, 49–51. [Google Scholar] [CrossRef]
- Buitrago, D.F.L.; Botero, J.R. Asymmetry of Glenoid Fossa as Differential Diagnosis for Hemimandibular Elongation. Rev. Mex. De Ortod. 2017, 5, 221–230. [Google Scholar]
- López, B.D.F.; Corral, S.C.M. Comparison of Planar Bone Scintigraphy and Single Photon Emission Computed Tomography for Diagnosis of Active Condylar Hyperplasia. J. Craniomaxillofac. Surg. 2016, 44, 70–74. [Google Scholar] [CrossRef]
- Wen, B.; Shen, Y.; Wang, C.-Y. Clinical Value of 99Tcm-MDP SPECT Bone Scintigraphy in the Diagnosis of Unilateral Condylar Hyperplasia. Sci. World J. 2014, 2014, 1–6. [Google Scholar]
- DeLone, D.R.; Brown, W.D.; Gentry, L.R. Proteus Syndrome: Craniofacial and Cerebral MRI. Neuroradiology 1999, 41, 840–843. [Google Scholar] [CrossRef]
- Pripatnanont, P.; Vittayakittipong, P.; Markmanee, U.; Thongmak, S.; Yipintsoi, T. The Use of SPECT to Evaluate Growth Cessation of the Mandible in Unilateral Condylar Hyperplasia. Int. J. Oral Maxillofac. Surg. 2005, 34, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Saridin, C.P.; Raijmakers, P.G.; Slootweg, P.J.; Tuinzing, D.B.; Becking, A.G.; van der Waal, I. Unilateral Condylar Hyperactivity: A Histopathologic Analysis of 47 Patients. J. Oral Maxillofac. Surg. 2010, 68, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Saridin, C.P.; Raijmakers, P.; Al Shamma, S.; Tuinzing, D.B.; Becking, A.G. Comparison of Different Analytical Methods Used for Analyzing SPECT Scans of Patients with Unilateral Condylar Hyperactivity. Int. J. Oral Maxillofac. Surg. 2009, 38, 942–946. [Google Scholar] [CrossRef] [PubMed]
- Warhekar, A.M.; Wanjari, P.V.; Phulambrikar, T. Unilateral Trifid Mandibular Condyle: A Case Report. Cranio 2011, 29, 80–84. [Google Scholar] [CrossRef]
- Katti, G.; Najmuddin, M.; Fatima, S.; Unnithan, J. Bifid Mandibular Condyle. BMJ Case Rep. 2012, 2012, bcr-2012-007051. [Google Scholar] [CrossRef]
- John, L.; Yin, Y.Y.; David, Y.W.C.; Kwong, C.L. Planar Scintigraphy in Assessment of Mandibular Asymmetry: Unilateral Condylar Hyperplasia vs. Asymmetric Mandibular Hyperplasia. 2012. Available online: https://www.scirp.org/journal/paperinformation.aspx?paperid=26244 (accessed on 12 November 2022).
- Goulart, D.R.; Muñoz, P.; Cantín López, M.G.; de Moraes, M.; Olate, S. Comparative Evaluation of Condylar Volume between Patients with Unilateral Condylar Hyperplasia and Class III Dentofacial Deformity. J. Oral Maxillofac. Surg. 2017, 75, 180–188. [Google Scholar] [CrossRef]
- Sedano-Balbin, G.; Romero-Tapia, P.; Pérez-Vargas, F.; Alvitez-Temoche, D.; Mayta-Tovalino, F. Three-Dimensional Correlation between Condylar Size and Mandibular Asymmetry with Type 1B Condylar Hyperplasia: A Quasi-Experimental Study from PERU. J. Int. Oral Health 2020, 12, 323. [Google Scholar] [CrossRef]
- Nah, K.-S. Condylar Bony Changes in Patients with Temporomandibular Disorders: A CBCT Study. Imaging Sci. Dent. 2012, 42, 249–253. [Google Scholar] [CrossRef]
- Angiero, F.; Farronato, G.; Benedicenti, S.; Vinci, R.; Farronato, D.; Magistro, S.; Stefani, M. Mandibular Condylar Hyperplasia: Clinical, Histopathological, and Treatment Considerations. Cranio 2009, 27, 24–32. [Google Scholar] [CrossRef]
- Luther, F.; Morris, D.O.; Hart, C. Orthodontic Preparation for Orthognathic Surgery: How Long Does It Take and Why? A Retrospective Study. Br. J. Oral Maxillofac. Surg. 2003, 41, 401–406. [Google Scholar] [CrossRef]
- El Mozen, L.A.; Meng, Q.-G.; Li, Y.-J.; Long, X.; Chen, G.-X. Condylar and Occlusal Changes after High Condylectomy and Orthodontic Treatment for Condylar Hyperplasia. J. Huazhong Univ. Sci. Technol. Med. Sci. 2015, 35, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Goulart, D.R.; Muñoz, P.; Olate, S.; de Moraes, M.; Fariña, R. No Differences in Morphological Characteristics between Hyperplastic Condyle and Class III Condyle. Int. J. Oral Maxillofac. Surg. 2015, 44, 1281–1286. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zheng, Y.; Cai, H.; Meng, Q.; Fang, W.; Ke, J.; Long, X.; Chen, G. Standard Orthodontic Treatment after Condylectomy for Patients with Active Unilateral Condylar Hyperplasia. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 404–415.e1. [Google Scholar] [CrossRef] [PubMed]
- Shivhare, P.; Lata, S.; Balaji, P.; Gupta, A. Non-Syndromic Bilateral Condylar Aplasia: A Rare Case. Indian J. Dent. Res. 2015, 26, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Canger, E.M.; Celenk, P. Aplasia of the Mandibular Condyle Associated with Some Orthopaedic Abnormalities. Dentomaxillofac. Radiol. 2012, 41, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Kaneyama, K.; Segami, N.; Hatta, T. Congenital Deformities and Developmental Abnormalities of the Mandibular Condyle in the Temporomandibular Joint. Congenit. Anom. 2008, 48, 118–125. [Google Scholar] [CrossRef]
- Bertolini, F.; Bianchi, B.; De Riu, G.; Di Blasio, A.; Sesenna, E. Hemimandibular hyperplasia treated by early high condylectomy: A case report. Int. J. Adult Orthod. Orthognath. Surg. 2001, 16, 227–234. [Google Scholar]
- Tun Oo, L.; Miyamoto, J.J.; Takada, J.-I.; Moriyama, K. Correlation between the Position of the Glenoid Fossa and Condylar Translational Movement in Skeletal Class III Mandibular Asymmetry Patients. Eur. J. Orthod. 2022, 44, 294–302. [Google Scholar] [CrossRef]
- Damstra, J.; Fourie, Z.; Ren, Y. Evaluation and comparison of postero-anterior cephalograms and cone-beam computed tomography images for the detection of mandibular asymmetry. Eur. J. Orthod. 2013, 35, 45–50. [Google Scholar] [CrossRef]
- Shivhare, P.; Shankarnarayan, L.; Kumar, M.; Sowbhagya, M.B. Condylar Aplasia and Hypoplasia: A Rare Case. Case Rep. Dent. 2013, 2013, 745602. [Google Scholar] [CrossRef]
- Wolford, L.M.; Mehra, P.; Reiche-Fischel, O.; Morales-Ryan, C.A.; García-Morales, P. Efficacy of High Condylectomy for Management of Condylar Hyperplasia. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 136–150, discussion 150–151. [Google Scholar] [CrossRef] [PubMed]
- Da Costa Araújo, F.A.; de Santana Santos, T.; de Oliveira e Silva, E.D.; Filho, J.R.L. One-Stage Treatment of Hemimandibular Hyperplasia. J. Craniofac. Surg. 2012, 23, e635. [Google Scholar] [CrossRef] [PubMed]
- Xavier, S.P.; Santos, T.D.S.; Silva, E.R.; Faria, A.C.; de Mello Filho, F.V. Two-Stage Treatment of Facial Asymmetry Caused by Unilateral Condylar Hyperplasia. Braz. Dent. J. 2014, 25, 257–260. [Google Scholar] [CrossRef] [PubMed]
- Diniz, J.A.; dos Santos Siqueira, A.; Torres, L.H.S.; Faro, T.F.; Rodrigues, E.D.R.; Laureano Filho, J.R. Virtual Surgical Planning and One-Stage Treatment of Active Hemimandibular Hyperplasia. J. Craniofac. Surg. 2019, 30, e679–e681. [Google Scholar] [CrossRef] [PubMed]
- Ferri, J.; Raoul, G.; Potier, J.; Nicot, R. Temporomandibular Joint (TMJ): Condyle Hyperplasia and Condylectomy. Rev. De Stomatol. De Chir. Maxillo-Faciale Et De Chir. Orale 2016, 117, 259–265. [Google Scholar]
- Lippold, C.; Kruse-Losler, B.; Danesh, G.; Joos, U.; Meyer, U. Treatment of Hemimandibular Hyperplasia: The Biological Basis of Condylectomy. Br. J. Oral Maxillofac. Surg. 2007, 45, 353–360. [Google Scholar] [CrossRef]
- Pereira-Santos, D.; De Melo, W.M.; Souza, F.Á.; De Moura, W.L.; de Paulo Cravinhos, J.C. High Condylectomy Procedure: A Valuable Resource for Surgical Management of the Mandibular Condylar Hyperplasia. J. Craniofac. Surg. 2013, 24, 1451–1453. [Google Scholar] [CrossRef]
- Ghawsi, S.; Aagaard, E.; Thygesen, T.H. High Condylectomy for the Treatment of Mandibular Condylar Hyperplasia: A Systematic Review of the Literature. Int. J. Oral Maxillofac. Surg. 2016, 45, 60–71. [Google Scholar] [CrossRef]
- Muñoz, M.F.; Monje, F.; Goizueta, C.; Rodríguez-Campo, F. Active Condylar Hyperplasia Treated by High Condylectomy: Report of Case. J. Oral Maxillofac. Surg. 1999, 57, 1455–1459. [Google Scholar] [CrossRef]
- Maniskas, S.A.; Ly, C.L.; Pourtaheri, N.; Parsaei, Y.; Steinbacher, D.M. Concurrent High Condylectomy and Orthognathic Surgery for Treatment of Patients With Unilateral Condylar Hyperplasia. J. Craniofac. Surg. 2020, 31, 2217–2221. [Google Scholar] [CrossRef]
- Wu, C.; Meng, Q.; Deng, M.; Cai, H.; Ke, J.; Long, X. Cone–Beam Computed Tomographic Analysis of Maxillary and Mandibular Changes after High Condylectomy Combined with Orthodontic Treatment for Active Unilateral Condylar Hyperplasia. Br. J. Oral Maxillofac. Surg. 2018, 56, 692–697. [Google Scholar] [CrossRef]
- Wolford, L.M.; Movahed, R.; Dhameja, A.; Allen, W.R. Low Condylectomy and Orthognathic Surgery to Treat Mandibular Condylar Osteochondroma: A Retrospective Review of 37 Cases. J. Oral Maxillofac. Surg. 2014, 72, 1704–1728. [Google Scholar] [CrossRef] [PubMed]
- Fariña, R.A.; Becar, M.; Plaza, C.; Espinoza, I.; Franco, M.E. Correlation between Single Photon Emission Computed Tomography, AgNOR Count, and Histomorphologic Features in Patients with Active Mandibular Condylar Hyperplasia. J. Oral Maxillofac. Surg. 2011, 69, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Fariña, R.; Pintor, F.; Pérez, J.; Pantoja, R.; Berner, D. Low Condylectomy as the Sole Treatment for Active Condylar Hyperplasia: Facial, Occlusal and Skeletal Changes. An Observational Study. Int. J. Oral Maxillofac. Surg. 2015, 44, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Alsayegh, H.A.; Alsubaie, Z.A.; Alwayil, A.R.; Alqadhi, M.A.; Alawadh, A.M. Unilateral Condylar Hyperplasia With Active Bony Overgrowth: A Case Report. Cureus 2021, 13, e5840. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, M.; Castillo, J.L.D.; Guerra, M.M.; Sanchez, R.; La Plata, M.M.D. Condylar Osteochondroma Treated with Total Condylectomy and Preservation of the Articular Disc: A Case Report. Craniomaxillofac. Trauma Reconstr. 2015, 8, 136–140. [Google Scholar] [CrossRef]
- De Melo, W.M.; Pereira-Santos, D.; Sonoda, C.K.; De Moura, W.L.; de Paulo-Cravinhos, J.C. Conservative Condylectomy for Management of Osteochondroma of the Mandibular Condyle. J. Craniofac. Surg. 2013, 24, e209–e211. [Google Scholar] [CrossRef]
- Mouallem, G.; Vernex-Boukerma, Z.; Longis, J.; Perrin, J.-P.; Delaire, J.; Mercier, J.-M.; Corre, P. Efficacy of Proportional Condylectomy in a Treatment Protocol for Unilateral Condylar Hyperplasia: A Review of 73 Cases. J. Cranio-Maxillofac. Surg. 2017, 45, 1083–1093. [Google Scholar] [CrossRef]
- Niño-Sandoval, T.C.; Maia, F.P.A.; Vasconcelos, B.C.E. Efficacy of Proportional versus High Condylectomy in Active Condylar Hyperplasia—A Systematic Review. J. Craniomaxillofac. Surg. 2019, 47, 1222–1232. [Google Scholar] [CrossRef]
- Dattani, A.; Heggie, A. Hemifacial Hyperplasia: A Case Series and Review of the Literature. Int. J. Oral Maxillofac. Surg. 2021, 50, 341–348. [Google Scholar] [CrossRef]
- Choung, P.H.; Nam, I.W. An Intraoral Approach to Treatment of Condylar Hyperplasia or High Condylar Process Fractures Using the Intraoral Vertico-Sagittal Ramus Osteotomy. J. Oral Maxillofac. Surg. 1998, 56, 563–570, discussion 571. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Z.; Yi, B.; Liang, C.; Li, Y.; Wang, X. [Preliminary study of condylectomy via intraoral approach]. Zhonghua Kou Qiang Yi Xue Za Zhi 2012, 47, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Z.; Yi, B.; Liang, C.; Tian, K.; Wang, X. [Clinical application of condylectomy via intraoral approach under computer assisted surgical navigation]. Zhonghua Kou Qiang Yi Xue Za Zhi 2013, 48, 350–354. [Google Scholar] [CrossRef] [PubMed]
- Deng, M.; Long, X.; Cheng, A.H.A.; Cheng, Y.; Cai, H. Modified Trans-Oral Approach for Mandibular Condylectomy. Int. J. Oral Maxillofac. Surg. 2009, 38, 374–377. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Sun, H.; Zhang, L.; Wang, X. Simple Way of Facilitating Intraoral Condylectomy and Securing the Excised Condyle: Technical Note. Br. J. Oral Maxillofac. Surg. 2013, 51, e305–e306. [Google Scholar] [CrossRef] [PubMed]
- You, H.-J.; Moon, K.-C.; Yoon, E.-S.; Lee, B.-I.; Park, S.-H. Clinical and Radiological Outcomes of Transoral Endoscope-Assisted Treatment of Mandibular Condylar Fractures. Int. J. Oral Maxillofac. Surg. 2016, 45, 284–291. [Google Scholar] [CrossRef]
- Schmelzeisen, R.; Cienfuegos-Monroy, R.; Schön, R.; Chen, C.-T.; Cunningham Jr, L.; Goldhahn, S. Patient Benefit from Endoscopically Assisted Fixation of Condylar Neck Fractures—A Randomized Controlled Trial. J. Oral Maxillofac. Surg. 2009, 67, 147–158. [Google Scholar] [CrossRef]
- Cascone, P.; Cicero, B.; Ramieri, V.; Germano, F.; Vellone, V. Treatment of Unilateral Condylar Hyperplasia with Proportional Condylectomy and Orthodontic Aligners. J. Clin. Orthod. JCO 2020, 54, 611–619. [Google Scholar]
- Abotaleb, B.; Bi, R.; Telha, W.; Zhao, W.; Li, Y.; Zhu, S. Treatment Measures of Hemimandibular Hyperplasia and Associated Facial Deformities. J. Cranio-Maxillofac. Surg. 2021, 49, 126–134. [Google Scholar] [CrossRef]
- Qi, L.; Cao, N.; Ge, W.; Jiang, T.; Fan, L.; Zhang, L. A New Method for Individual Condylar Osteotomy and Repositioning Guides Used in Patients with Severe Deformity Secondary to Condylar Osteochondroma. Orphanet J. Rare Dis. 2021, 16, 1–11. [Google Scholar] [CrossRef]
- Kim, D.S.; Kim, J.-Y.; Jeong, C.-W.; Park, K.-H.; Huh, J.-K. Conservative Condylectomy Alone for the Correction of Mandibular Asymmetry Caused by Osteochondroma of the Mandibular Condyle: A Report of Five Cases. J. Korean Assoc. Oral Maxillofac. Surg. 2015, 41, 259. [Google Scholar] [CrossRef] [PubMed]
- Wolford, L.M.; Mehra, P.; Franco, P. Use of Conservative Condylectomy for Treatment of Osteochondroma of the Mandibular Condyle. J. Oral Maxillofac. Surg. 2002, 60, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Santos, G.S.; Gomes, J.B.; de Sousa Maia, S.; Bermejo, P.R.; Shinohara, E.H.; Sonoda, C.K.; de Melo, W.M. Using Conservative Condylectomy for Management of a Large Osteochondroma of the Mandibular Condyle with 6-Year Follow-Up. J. Craniofac. Surg. 2014, 25, e102–e104. [Google Scholar] [CrossRef] [PubMed]
- Rojare, C.; Wojcik, T.; Coussens, C.; Ferri, J.; Pertuzon, B.; Raoul, G. Condylar Hyperplasia: Qualitative and Quantitative Study of Temporomandibular Joints Remodeling after Condylectomy. L’Orthodontie Française 2014, 85, 189–200. [Google Scholar] [CrossRef]
- Gc, R.; Muralidoss, H.; Ramaiah, S. Conservative Management of Unilateral Condylar Hyperplasia. Oral Maxillofac. Surg. 2012, 16, 201–205. [Google Scholar] [CrossRef]
- Nolte, J.W.; Schreurs, R.; Karssemakers, L.H.E.; Tuinzing, D.B.; Becking, A.G. Demographic Features in Unilateral Condylar Hyperplasia: An Overview of 309 Asymmetric Cases and Presentation of an Algorithm. J. Cranio-Maxillofac. Surg. 2018, 46, 1484–1492. [Google Scholar] [CrossRef]
- Açikgöz, A. Bilateral Bifid Mandibular Condyle: A Case Report. J. Oral Rehabil. 2006, 33, 784–787. [Google Scholar] [CrossRef]
- Neelakandan, R.S.; Bhargava, D. Bifid hyperplastic mandibular condyle. J. Maxillofac. Oral Surg. 2013, 12, 466–471. [Google Scholar] [CrossRef]
- Butt, F.M.A.; Guthua, S.W.; Nganga, P.; Edalia, M.; Dimba, E.A.O. One-Stage Treatment of Acquired Facial Deformity Caused by Severe Unilateral Condylar Hyperplasia. J. Craniofac. Surg. 2011, 22, 1966–1968. [Google Scholar] [CrossRef]
- Motamedi, M.H. Treatment of Condylar Hyperplasia of the Mandible Using Unilateral Ramus Osteotomies. J. Oral Maxillofac. Surg. 1996, 54, 1161–1169, discussion 1169–1170. [Google Scholar] [CrossRef]
- López, D.F.; Aristizábal, J.F.; Martínez-Smit, R. Condylectomy and “Surgery First” Approach: An Expedited Treatment for Condylar Hyperplasia in a Patient with Facial Asymmetry. Dent. Press J. Orthod. 2017, 22, 86–96. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, A.L.; Ruellas, A.C.D.O.; Benavides, E.; Soki, F.N.; Aronovich, S.; Magraw, C.B.L.; Turvey, T.; Cevidanes, L. Mandibular Condylar Remodeling Characteristics after Simultaneous Condylectomy and Orthognathic Surgery. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.W. Definitive Surgical Correction of the Deformity Resulting from Hemimandibular Hyperplasia. J. Craniomaxillofac. Surg. 2005, 33, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Nelke, K.; Łuczak, K.; Janeczek, M.; Pasicka, E.; Morawska-Kochman, M.; Guziński, M.; Dobrzyński, M. Methods of Definitive Correction of Mandibular Deformity in Hemimandibular Hyperplasia Based on Radiological, Anatomical, and Topographical Measurements—Proposition of Author’s Own Protocol. Int. J. Env. Res. Public Health 2022, 19, 10005. [Google Scholar] [CrossRef]
- Cascone, P.; D’Alessandro, F.; Gallo, E.; Cicero, G.; Vellone, V. The Role of Three-Dimensional Printing Technology as an Additional Tool in Unilateral Condylar Hyperplasia Surgical Planning. J. Craniofac. Surg. 2020, 31, e735–e738. [Google Scholar] [CrossRef]
- Ha, S.-W.; Choi, J.-Y.; Baek, S.-H. Correction of Unilateral Condylar Hyperplasia and Posterior Open Bite with Proportional Condylectomy and Fixed Orthodontic Treatment. Angle Orthod. 2020, 90, 144–158. [Google Scholar] [CrossRef]
- Wenghoefer, M.; Peters, A.; Reich, R.H. Modified Triaca-Style Wing Osteotomy to Correct Facial Asymmetry in a Patient With Horizontal Growth–Type Condylar Hyperplasia. J. Craniofac. Surg. 2013, 24, 1769–1771. [Google Scholar] [CrossRef]
- Nagasaka, H.; Sugawara, J.; Kawamura, H.; Nanda, R. “ Surgery First” Skeletal Class III Correction Using the Skeletal Anchorage System. J. Clin. Orthod. JCO 2009, 43, 97–105. [Google Scholar]
- Janakiraman, N.; Feinberg, M.; Vishwanath, M.; Jayaratne, Y.S.N.; Steinbacher, D.M.; Nanda, R.; Uribe, F. Integration of 3-Dimensional Surgical and Orthodontic Technologies with Orthognathic “Surgery-First” Approach in the Management of Unilateral Condylar Hyperplasia. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 1054–1066. [Google Scholar] [CrossRef]
- Peng, S.P.; Ko, W.-C.E.; Lin, C.-H.; Ho, C.-Y. Hemimandibular Hyperplasia Treated by Orthognathic Surgery and Condylectomy in a Young Woman. Taiwan. J. Orthod. 2021, 33, 5. [Google Scholar] [CrossRef]
- Vernucci, R.A.; Mazzoli, V.; Galluccio, G.; Silvestri, A.; Barbato, E. Unilateral hemimandibular hyperactivity: Clinical features of a population of 128 patients. J. Craniomaxillofac. Surg. 2018, 46, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Verhelst, P.-J.; Shaheen, E.; de Faria Vasconcelos, K.; Van der Cruyssen, F.; Shujaat, S.; Coudyzer, W.; Salmon, B.; Swennen, G.; Politis, C.; Jacobs, R. Validation of a 3D CBCT-Based Protocol for the Follow-up of Mandibular Condyle Remodeling. Dentomaxillofac. Radiol. 2020, 49, 20190364. [Google Scholar] [CrossRef] [PubMed]
- Nelke, K.H.; Morawska-Kochman, M.; Nienartowicz, J.; Grzelak, J.; Staszak, K.; Fraczek, M.; Luczak, K.; Guzinski, M. Anatomical and Clinical Implications in Neocondyle Stability After a Condylectomy. J. Craniofac. Surg. 2020, 31, 241–250. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).