Abstract
Little is known about whether the depth of the vestibular fornix influences people’s ability to access their teeth to remove plaque during oral hygiene measures at home. This study aimed to investigate the association between vestibular fornix depth and periodontal health. The study included 100 adults in good periodontal health, with a plaque index (PI) ≤15%, bleeding on probing (BOP) ≤10%, and a pocket probing depth (PPD) ≤3 mm. Using a periodontal probe and a digital caliper, we measured PI, BOP, PPD, gum phenotype, gum recession, the width of keratinized gingiva, and the vestibular fornix depth. Adjustment for multiple testing was performed using the Benjamini-Hochberg procedure. Results: Vestibular fornix depth was associated with width of keratinized gingiva (ρ 0.60, p < 0.0001). Median BOP was 1.39% in participants with a vestibular fornix depth ≥7 mm, and 0.00% in those with a vestibular fornix depth <7 mm (p = 0.62). Vestibular fornix depth and the width of keratinized gingiva did not seem to be associated with the level of periodontal health. Participants with a shallower vestibular fornix depth should be given advice on how best to ensure good oral hygiene at home.
1. Introduction
In the oral cavity, the vestibule is the space between the dental arches and the inside of the lips and cheeks. In resting conditions, with the dental arches in occlusion, the vestibule forms a horseshoe shaped fissure extending posteriorly to the retromolar trigones, and anteriorly along the whole inner surface of the lips and cheeks. The upper and lower margins of the fornix correspond to the fold in the mucosa of the lips and cheeks over the alveolar processes. On a level with this fold, the lining of the oral cavity—called the alveolar mucosa—forms part of the gums starting from the coronal third of the alveolar process. The walls of the vestibule can stretch, enabling the dental practitioner’s exploration of the oral cavity and the patients’ use of oral hygiene tools at home [1].
In the latest classification of periodontal diseases published in 2017, a correlation was suspected between soft tissue inflammation and a shallower than normal vestibular fornix, which could make it more difficult to access the teeth and ensure an effective oral hygiene [2]. Ward was the first to investigate the relationship between these two parameters in a population of individuals in good periodontal health in 1976 [3]. The results of their research showed that periodontal health can be maintained even in the presence of a shallow mandibular fornix in the anterior sectors of the oral cavity. There was also no significant correlation between the amount of attached gingiva and the level of oral hygiene, indicating that good periodontal health is not more difficult to achieve in individuals with a more limited amount of attached gingiva. Similar considerations were reported by Padmini et al. in 2018 [4], who also considered the fornix in the anterior sectors of the upper jaw, confirming that a shallower fornix did not correlate with negative periodontal health parameters; there was only a weak negative correlation between a shallow fornix and gum recession in the lower jaw. On the other hand, vestibular fornix depth seems to be an important factor for the long-term success of dental implants. The retrospective study conducted by Halperin-Sternfeld et al. was the first, and remains the only investigation published to date, that assessed the correlation between the fornix depth at peri-implant sites and oral hygiene parameters [5]. Their results showed that a shallow fornix correlated with gum recession and there was a consequent loss of clinical attachment at the peri-implant sites. There was also a limited amount of keratinized gingiva in these areas, a factor influencing plaque control and the success of an implant [6,7]. In the literature to date, there have been no other articles investigating the influence of the vestibular fornix depth on parameters of periodontal and peri-implant health. Establishing a minimum adequate fornix depth could be useful for the purposes of a patient-centered treatment and to enhance better oral hygiene at home, especially in young patients [8]. The main goal of the present study was to establish whether an association exists between vestibular fornix depth, width of keratinized gingiva, and periodontal health. We also examined whether it was possible to maintain normal levels of periodontal health even in the presence of a shallow fornix (<7 mm).
2. Materials and Methods
The present study is an anatomical and clinical study with a descriptive purpose on the association between vestibular fornix depth, width of keratinized gingiva, and periodontal health. The present research adopted the same investigation approach as previous studies [3,4]. From October 2020 to May 2021, we enrolled a convenient sample of 100 volunteers from among the undergraduates and postgraduates attending courses in dental hygiene, dentistry, and dental prosthetics at the School of Dentistry of the University of Padua (Italy). Since there was no a priori formal hypothesis that could be the basis for a sample size calculation, the sample size could not be calculated with mathematical methods and a convenient sample of 100 subjects was considered adequate to obtain reliable results and allow for a sound statistical analysis. The study was conducted in accordance with the principles of the Declaration of Helsinki and all participants gave their consent. The study was approved by the local Ethical Committee (No. 84/2022). The inclusion criteria were:
- aged over 18 years;
- complete upper and lower anterior dentition (teeth from 1.5 to 2.5, and from 3.5 to 4.5);
- no incongruous anterior restorative crowns coming into contact with the gum margin;
- an absence of macroscopically evident skeletal malocclusions;
- no diabetes or pregnancy; no use of anticonvulsants, calcium antagonists, or immune-modulating drugs;
- periodontal tissues in good health with a plaque index (PI) ≤15%; bleeding on probing (BOP) ≤10%; and a pocket probing depth (PPD) ≤3 mm.
We also recorded participants’ smoking habits and smoking frequency, whether they had previously undergone any orthodontic treatments, and whether female participants used oral contraceptives. Each participant was fitted with a bilateral mouth-opener and the following measurements were taken:
Pocket probing depth (PPD)—recorded with the millimetric PCP UNC 15 periodontal probe (Hu-Friedy, Chicago, IL, USA) on the vestibular surface of each front tooth (from 1.3 to 2.3, and from 3.3 to 4.3), coinciding with the medial point of the gum margin. The measurements were rounded up or down to the nearest millimeter (Figure 1);
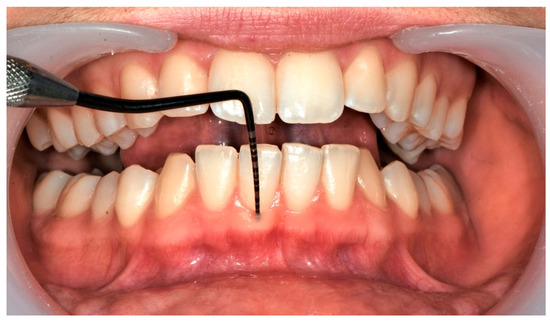
Figure 1.
Clinical measurement of probing depth (PPD).
The O’Larey plaque index (PI) and bleeding on probing (BOP)—recorded at a total of 6 sites (3 vestibular and 3 palatal/lingual) for each anterior tooth in the upper and lower jaws, using a graduated periodontal probe (bleeding was assessed within 10 s of removing the probe);
Gum phenotype—recorded in accordance with previously published reports [9]; the measurement was taken by inserting the probe in the vestibular sulcus in a direction parallel to the long axis of the tooth. If the probe was clearly visible through the gingival tissues, participants were assigned to the group with a thin gum phenotype; if not, their gum phenotype was classified as thick (Figure 2);
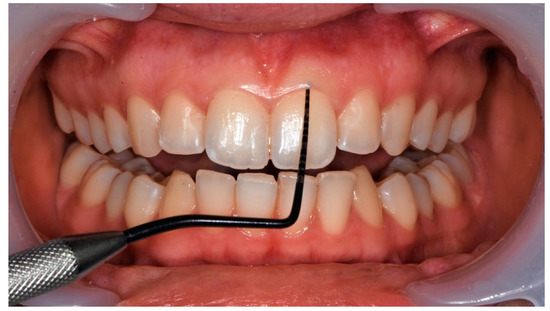
Figure 2.
Measurement of gum phenotype according to De Rouck T. et al. [9].
Gum recession—calculated at the point of greatest concavity along the gum margin or at the medial vestibular point, measuring the distance between the cemento-enamel junction and the gum margin with the PCP UNC 15 periodontal probe (Hu-Friedy, Chicago, IL, USA);
Width of keratinized gingiva—as described elsewhere in the literature, a PCP UNC 15 probe was first placed horizontally on the alveolar mucosa, perpendicular to the long axis of the tooth, then moved coronally, dragging the soft tissue towards the keratinized gingiva to locate the muco-gingival junction precisely [10]. The distance from the medial point of the vestibular gum margin to the muco-gingival junction was recorded (Figure 3 and Figure 4);

Figure 3.
Measurement of width of keratinized gingiva.
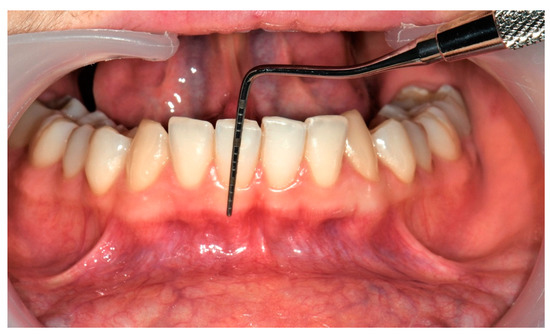
Figure 4.
Measurement of width of keratinized gingiva.
Fornix depth—we measured the distance from the medial point, or point of maximum concavity, of the gum margin to the mucobuccal fold. A digital caliper was used to obtain an accurate measurement, which was rounded up or down to the nearest millimeter. The dental arches were kept in gentle occlusion, and the mouth-opener in the frontal position to maximize the depth of the fornix (Figure 5). Each instrument used for measurements was sterilized after each patient, according to the hospital sterilization protocol. This method draws on those described by Halperin in 2016, and by Padmini in 2018 [4,5].
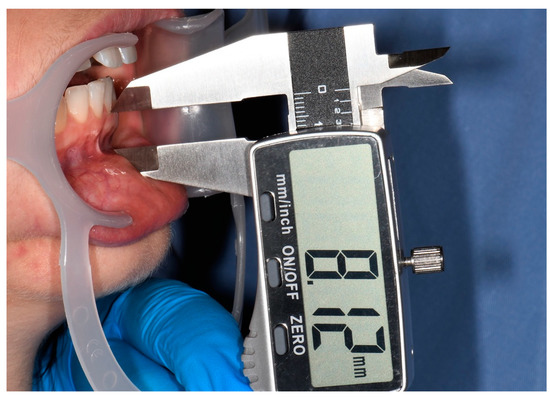
Figure 5.
Measurement of depth of vestibular fornix.
The width of attached gingiva was calculated indirectly by subtracting the probing depth from the width of keratinized gingiva. Based on the data collected, participants were grouped by fornix depth, considering a cut-off of 7 mm. This depth was chosen arbitrarily as it was judged to represent the minimum amount of space needed to maneuver an electric or manual toothbrush comfortably using the modified Bass method, with brushes measuring approximately 10–11 mm in height. All clinical measurements were taken by the same operator (AV). To test their reproducibility and reliability, 10 measurements were obtained from 10 different individuals by two different operators, and their inter-rater reliability was assessed with the intraclass correlation coefficient (ICC) for the keratinized gingiva and fornix, and with Cohen’s Kappa for the phenotype and PPD. Statistics are reported with 95% confidence intervals (CI).
Statistical Analysis
Continuous data were summarized as means and standard deviations (SD), or medians and interquartile ranges (IQR). Categorical data were summarized as frequencies and percentages. Comparisons between two groups were performed using the Student’s t-test, the Mann-Whitney test, and the chi-squared test, as appropriate. Quantile-quantile plots were used to check for normality. Correlations between continuous variables were assessed using Pearson’s or Spearman’s correlation coefficients. All tests were two-sided, and a p-value of less than 0.05 was considered statistically significant. Adjustment for multiple testing was performed using the Benjamini-Hochberg procedure. The statistical analysis was performed using R 4.1 (R Foundation for Statistical Computing, Vienna, Austria) [11].
3. Results
The analysis concerned all 100 participants (36 males and 64 females; median age 25 years, IQR 22–27). Inter-rater reliability was very good for the keratinized gingiva (ICC 0.92, 95% CI 0.88 to 0.94), fornix (ICC 0.93, 95% CI 0.90 to 0.95), and phenotype (Cohen’s Kappa 0.99, 95% CI 0.99 to 0.99), while it was moderate for the PPD (Cohen’s Kappa 0.60, 95% CI 0.44 to 0.77).
Sixty-nine participants (69%) had previously had orthodontic treatments; 18 participants (18%) were smokers (<10 cigarettes/day); and 16/64 females (25%) used oral contraceptives. Overall, the PI was 0.00% (IQR 0.00–1.40%), and the median BOP was 1.39% (IQR 0.00–2.78%). The gum phenotype was thick in 42 participants (42%), and thin in 58 (58%).
The median BOP was 1.39% (IQR 0.00–2.78%) in males, and 1.39% (0.00–2.78%) in females (p = 0.68). The median PI was 0.70% (IQR 0.00–2.78%) in males, and 0.00% (0.00–1.39%) in females (p = 0.33). The median BOP was 1.39% (IQR 0.00–2.78%) in smokers, and 1.39% (0.00–2.78%) in non-smokers (p = 0.68). The median PI was 1.39% (IQR 0.00–3.82%) in smokers, and 0.00% (0.00–1.39%) in non-smokers (p = 0.30). The median BOP was 0.00% (IQR 0.00–2.78%) in females who were using oral contraceptives, and 1.39% (0.00–2.78%) in those who were not (p = 0.68). The median PI was 0.00% (IQR 0.00–1.39%) in both subgroups of females, regardless of any use of oral contraceptives (p = 0.94).
Mean fornix depth was 10.35 mm (SD 0.66) for the upper dental arch (10.69 mm in males, 10.15 mm in females), and 8.39 mm (SD 0.08) for the lower arch (8.71 mm in males, 8.20 mm in females). Vestibular fornix depth ranged between 3 and 17 mm.
The width of keratinized gingiva had a mean of 5.94 mm (SD 0.62) for the upper arch (5.75 mm in males, 6.05 mm in females), and 4.40 mm (SD 0.40) for the lower arch (4.71 mm in males, 4.23 mm in females).
The amount of attached gingiva had a mean of 4.50 mm (SD 0.62) for the upper arch (4.30 mm in males, 4.61 mm in females), and 3.20 mm (SD 0.49) for the lower arch (3.45 mm in males, 3.05 mm in females). The amount of attached gingiva ranged between 1 and 10 mm.
The proportion of the fornix with attached gingiva had a mean of 43.45% for the upper arch (40.17% in males, 45.39% in females), and 38.12% for the lower arch (39.64% in males, 37.22% in females). The proportion of the fornix with attached gingiva ranged from 31% to 50%, while the proportion of the fornix with keratinized gingiva ranged from 48% to 65% (Table 1). A moderate positive correlation emerged between fornix depth and the width of keratinized gingiva at all sites (for each tooth, for the upper and lower arches, and overall) (Table 1).

Table 1.
Analysis of fornix depth, keratinized gingiva, and attached gingiva.
Table 2 shows the correlations between the anatomical parameters (fornix depth, width of keratinized gingiva, and attached gingiva) and the periodontal parameters. No statistically significant correlations came to light between the anatomical and periodontal parameters (Table 2).

Table 2.
Correlations between anatomical parameters (fornix depth, width of keratinized gingiva, and attached gingiva) and periodontal health parameters (BOP and PI).
When participants were compared by overall fornix depth ≥7 vs. <7 mm, we found a median BOP of 1.39% (IQR 0.00–2.78%) in the former, and 0.00% (0.00–1.39%) in the latter (p = 0.62). The median PI was 0.00% (IQR 0.00–1.40%) in participants with an overall fornix depth ≥7 mm, and 0.00% (0.00–0.70%) in those with an overall fornix depth <7 mm (p = 0.66).
The thin gum phenotype was associated with a narrower keratinized gingiva (upper arch, p = 0.0.02; overall, p = 0.0.02) (Table 3).

Table 3.
Associations between clinically relevant parameters and gum phenotype.
Participants who had previously had orthodontic treatments seemed to have less keratinized gingiva in the upper arch, and a shallower fornix depth in the upper arch, and in the fornix as a whole, than participants who had no history of such treatments, but the difference was only close to statistical significance (Table 4).

Table 4.
Associations between anatomical parameters and orthodontic treatments.
4. Discussion
This study investigated periodontal parameters in relation to the depth of the vestibular fornix in individuals in good periodontal health. Our data showed that the anatomical parameters, such as the depth of the fornix, the width of the keratinized gingival, and the width of the attached gingival have absolute values better represented on a level with the upper arch than on the lower one. This observation was also made in the study by Padmini et al., who identified the same difference between the two regions [4].
Our data indicated that the depth of the vestibular fornix could vary considerably from one individual to another, and from one part of the oral cavity to another. In the upper arch, the minimum fornix depths were much the same between pairs of contralateral teeth and amounted to 5 mm in the region of the central incisors, 7 mm on a level with the lateral incisors, and 5 mm in the region of the canine teeth. In the lower arch, they were 3 mm, 4 mm, and 3 mm, respectively. In all regions of the oral cavity, there was at least 1 mm of attached gingiva—a finding consistent with the reports from Bowers et al. and Ward, who demonstrated that 1 mm of attached gingiva sufficed for an adequate periodontal health [3,12].
The width of attached gingiva in our sample had a mean 4.5 mm (min 1.0 mm, max 10.0 mm) for the upper arch, and 3.2 mm (min 1.0 mm max 9.0 mm) for the lower arch. This wide range of values is in accordance with the wide anatomical variability of the healthy periodontium and is in agreement with previous anatomical studies [1,13]. These values also corroborate Ward’s findings for the attached gingiva (min 1.0 mm, max 7.0 mm): Ward considered only the lower jaw and found the attached gingiva narrowest on a level with the canines [3].
The percentage of the fornix with keratinized gingiva was relatively similar from canine to canine, with a mean of 54% in the lower arch and 58% in the upper arch. For both dental arches, the percentage of the fornix occupied by keratinized gingiva tended to diminish from the central incisors to the canine. As for the lower arch, these findings on the relationship between gingiva and the fornix again confirm the findings of Ward [3].
There was evidence of a positive correlation between fornix depth and the width of keratinized gingiva. This would suggest that the fornix has an important role and is probably capable of influencing the width of keratinized gingiva that comes to form around the teeth. No published studies appear to have considered this relationship yet.
Judging from our data, however, fornix depth might not affect periodontal health parameters. This tends to confirm what Padmini et al. reported in their article, as they found no association between fornix depth and oral hygiene or gingival health indicators [4]. The literature review conducted by Mehta also concluded that the width of attached gingiva has no influence on the periodontal health of individuals achieving adequate oral hygiene [14].
The most interesting finding that emerged from our study is that a shallower fornix does not prevent the maintenance of good periodontal health. In our opinion, it is important to bear this in mind when communicating with patients. A shallower fornix would nonetheless warrant appropriate patient training on the most suitable methods and tools for ensuring proper oral hygiene.
As for our participants’ smoking habits, we found that smokers had more plaque than non-smokers. These results confirm the findings of previous experimental studies on the oral health of smokers versus non-smokers [15,16]. A recent systematic review also confirmed this association, reaching the conclusion that periodontal health parameters (PI included) were worse in smokers, of both conventional and electronic cigarettes, than in non-smokers [17].
As for gum phenotype, there might be a correlation with the width of keratinized gingiva. In our sample, participants with the thin gum phenotype had narrower keratinized gingiva than those with the thick phenotype, in both the upper and the lower dental arches. However, the difference was only close to statistical significance, hence caution is suggested. The mean difference was 0.7 mm, which can be considered clinically relevant. To support this result, a recent systematic review identified a positive correlation between gum phenotype and the width of keratinized gingiva among individuals in good periodontal health [18]. We can, therefore, speculate that a thicker gum coincides with a greater apical-coronal dimension of the keratinized mucosa.
One of the main limitations of the present study is the presence of multiple possible confounding factors (age, smoking habits, and orthodontic treatment history). Another limitation of the present study lies in that it only included individuals with intact dentition and good periodontal health indicators. We chose this approach because examining individuals in less healthy conditions would have given rise to false measurements due to periodontal disease, poor oral hygiene, and/or dietary or other modifying factors. Another limitation concerns us having considered gum phenotype, which is difficult to establish objectively. As there is still no method available for it to be rapidly identified and recorded in an easily-reproducible and widely-acknowledged manner, the reliability of any results regarding gum phenotype is debatable [19]. We were also unable to investigate the influence of fornix depth on gum recession and the consequent loss of clinical attachment at peri-implant sites because none of our participants had dental implants. Finally, the study design prevented us from seeking any causal associations between the variables of interest. It would be worth conducting studies that include the posterior sectors of the oral cavity as well, and testing whether the present findings obtained for natural teeth also apply to single implants in the same sectors.
5. Conclusions
The present study identified significant anatomical differences between the two jaws, with a generally deeper vestibular fornix and wider keratinized gingiva in the upper arch. We also found a correlation between these two parameters, although neither vestibular fornix depth nor width of keratinized gingiva revealed any significant influence on the efficacy of participants’ oral hygiene at home. We can, therefore, conclude that the depth of the vestibular fornix has no influence on periodontal health in the young healthy population (<30 years).
Author Contributions
Conceptualization, L.S. and E.S.; methodology, L.S.; investigation, A.V. and M.C.; data curation, F.C.; writing—original draft preparation, A.V.; writing—review and editing, M.C.; supervision, L.S., F.C. and E.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the local Ethical Committee (No. 84/2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon request to the corresponding author.
Acknowledgments
The authors would like to thank all the students involved in the present study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Berglundh, T.; Giannobile, W.V.; Lang, N.p.; Sanz, M. Lindhe’s Clinical Periodontology and Implant Dentistry, 7th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2022. [Google Scholar]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A New Classification Scheme for Periodontal and Peri-Implant Diseases and Conditions—Introduction and Key Changes from the 1999 Classification. J. Clin. Periodontol. 2018, 45, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Ward, V.J. The Depth of the Vestibular Fornix in the Mandibular Anterior Region in Health. J. Periodontol. 1976, 47, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Padmini, H.; Raja, K.; Ting, Z. Correlation of Width of Attached Gingiva, Depth of the Vestibule on Gingival Health and Oral Hygiene Maintenance in Malaysian Young Adults. J. Clin. Diagn. Res. 2018, 12, 39–44. [Google Scholar] [CrossRef]
- Halperin-Sternfeld, M.; Zigdon-Giladi, H.; Machtei, E.E. The Association between Shallow Vestibular Depth and Peri-Implant Parameters: A Retrospective 6 Years Longitudinal Study. J. Clin. Periodontol. 2016, 43, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.-H.; Chan, H.-L.; Wang, H.-L. The Significance of Keratinized Mucosa on Implant Health: A Systematic Review. J. Periodontol. 2013, 84, 1755–1767. [Google Scholar] [CrossRef] [PubMed]
- Todisco, M.; Buti, J.; Sbricoli, L.; Esposito, M. On the role of keratinised mucosa at dental implants: A 5-year prospective single-cohort study. Int. J. Oral Implantol. 2019, 12, 13–22. [Google Scholar] [PubMed]
- Sbricoli, L.; Bernardi, L.; Ezeddine, F.; Bacci, C.; Di Fiore, A. Oral Hygiene in Adolescence: A Questionnaire-Based Study. Int. J. Environ. Res. Public Health 2022, 16, 7381. [Google Scholar] [CrossRef] [PubMed]
- De Rouck, T.; Eghbali, R.; Collys, K.; De Bruyn, H.; Cosyn, J. The Gingival Biotype Revisited: Transparency of the Periodontal Probe through the Gingival Margin as a Method to Discriminate Thin from Thick Gingiva. J. Clin. Periodontol. 2009, 36, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Guglielmoni, P.; Promsudthi, A.; Tatakis, D.N.; Trombelli, L. Intra- and Inter-Examiner Reproducibility in Keratinized Tissue Width Assessment with 3 Methods for Mucogingival Junction Determination. J. Periodontol. 2001, 72, 134–139. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Bowers, G.M. A Study of the Width of Attached Gingiva. J. Periodontol. 1963, 34, 201–209. [Google Scholar] [CrossRef]
- Ainamo, J.; Talari, A. The increase with age of the width of attached gingiva. J. Periodontal. Res. 1976, 11, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.; Lim, L.P. The Width of the Attached Gingiva—Much Ado about Nothing? J. Dent. 2010, 38, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Luzzi, L.I.T.; Greghi, S.L.A.; Passanezi, E.; Sant’ana, A.C.P.; Lauris, J.R.P.; Cestari, T.M. Evaluation of clinical periodontal conditions in smokers and non-smokers. J. Appl. Oral Sci. 2007, 15, 512–517. [Google Scholar] [CrossRef] [PubMed]
- Pesce, P.; Menini, M.; Ugo, G.; Bagnasco, F.; Dioguardi, M.; Troiano, G. Evaluation of periodontal indices among non-smokers, tobacco, and e-cigarette smokers: A systematic review and network meta-analysis. Clin. Oral Investig. 2022, 26, 4701–4714. [Google Scholar] [CrossRef] [PubMed]
- Ralho, A.; Coelho, A.; Ribeiro, M.; Paula, A.; Amaro, I.; Sousa, J.; Marto, C.; Ferreira, M.; Carrilho, E. Effects of Electronic Cigarettes on Oral Cavity: A Systematic Review. J. Evid. Based Dent. Pract. 2019, 19, 101318. [Google Scholar] [CrossRef] [PubMed]
- Vlachodimou, E.; Fragkioudakis, I.; Vouros, I. Is There an Association between the Gingival Phenotype and the Width of Keratinized Gingiva? A Systematic Review. Dent. J. 2021, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Alves, P.H.M.; Alves, T.C.L.P.; Pegoraro, T.A.; Costa, Y.M.; Bonfante, E.A.; de Almeida, A.L.P.F. Measurement Properties of Gingival Biotype Evaluation Methods. Clin. Implant Dent. Relat. Res. 2018, 20, 280–284. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).