Effects of a Home-Based Foot–Ankle Exercise Program with Educational Booklet for Foot Dysfunctions in People with Diabetic Neuropathy: Results of the FOCA-II Randomized Controlled Clinical Trial
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Participants and Recruitment
2.3. Blinding, Randomization, and Allocation
2.4. Treatment Arms
2.5. Outcome Measures
2.6. Sample Size and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global Estimates of the Need for Rehabilitation Based on the Global Burden of Disease Study 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Andersen, H.; Gjerstad, M.D.; Jakoben, J. Atrophy of Foot Muscles A Measure of Diabetic Neuropathy. Diabetes Care 2004, 27, 2382–2385. [Google Scholar] [CrossRef] [PubMed]
- Boulton, A.J.M. The Diabetic Foot: From Art to Science. Diabetologia 2004, 47, 1343–1353. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; Yang, Q.X.; Wang, J.H.; Smith, M.B.; Wunderlich, R.; Cavanagh, P.R. Intrinsic Muscle Atrophy and Toe Deformity in the Diabetic Neuropathic Foot. Diabetes Care 2002, 25, 1444–1450. [Google Scholar] [CrossRef] [PubMed]
- Ijzerman, T.H.; Schaper, N.C.; Melai, T.; Meijer, K.; Willems, P.J.B.; Savelberg, H.H.C.M. Lower Extremity Muscle Strength Is Reduced in People with Type 2 Diabetes, with and without Polyneuropathy, and Is Associated with Impaired Mobility and Reduced Quality of Life. Diabetes Res. Clin. Pract. 2011, 95, 345–351. [Google Scholar] [CrossRef]
- Martinelli, A.R.; Montavani, A.M.; Nozabieli, A.J.L.; Ferreira, D.M.A.; Barela, J.A.; Camargo, M.R.; Fregonesi, C.E.P.T. The Foot Muscle Strength and Ankle Mobility for the Gait Parameters in Diabetic Neuropathies. Foot 2013, 23, 17–21. [Google Scholar] [CrossRef]
- Sacco, I.C.N.; Picon, A.P.; Macedo, D.O.; Butugan, M.K.; Watari, R.; Sartor, C.D. Alterations in the Lower Limb Joint Moments Precede the Peripheral Neuropathy Diagnosis in Diabetes Patients. Diabetes Technol. Ther. 2015, 17, 405–412. [Google Scholar] [CrossRef]
- Sawacha, Z.; Guarneri, G.; Avogaro, A.; Cobelli, C. A New Classification of Diabetic Gait Pattern Based on Cluster Analysis of Biomechanical Data. J. Diabetes Sci. Technol. 2010, 4, 1127–1138. [Google Scholar] [CrossRef]
- Watari, R.; Sartor, C.; Picon, A.; Butugan, M.; Amorim, C.; Ortega, N.; Sacco, I. Effect of Diabetic Neuropathy Severity Classified by a Fuzzy Model in Muscle Dynamics during Gait. J. Neuroeng. Rehabil. 2014, 11, 11. [Google Scholar] [CrossRef]
- Williams, D.S.B.; Brunt, D.; Tanenberg, R.J. Diabetic Neuropathy Is Related to Joint Stiffness during Late Stance Phase. J. Appl. Biomech. 2007, 23, 251–260. [Google Scholar] [CrossRef]
- Zhang, Y.; Lazzarini, P.A.; McPhail, S.M.; van Netten, J.J.; Armstrong, D.G.; Pacella, R.E. Global Disability Burdens of Diabetes-Related Lower-Extremity Complications in 1990 and 2016. Diabetes Care 2020, 43, 964–974. [Google Scholar] [CrossRef]
- Selvarajah, D.; Kar, D.; Khunti, K.; Davies, M.J.; Scott, A.R.; Walker, J.; Tesfaye, S. Diabetic Peripheral Neuropathy: Advances in Diagnosis and Strategies for Screening and Early Intervention. Lancet Diabetes Endocrinol. 2019, 7, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Van Netten, J.J.; Sacco, I.C.N.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Raspovic, A.; Bus, S.A. Treatment of Modifiable Risk Factors for Foot Ulceration in Persons with Diabetes: A Systematic Review. Diabetes Metab. Res. Rev. 2020, 36, e3271. [Google Scholar] [CrossRef] [PubMed]
- Allet, L.; Armand, S.; Aminian, K.; Pataky, Z.; Golay, A.; de Bie, R.A.; de Bruin, E.D. An Exercise Intervention to Improve Diabetic Patients’ Gait in a Real-Life Environment. Gait Posture 2010, 32, 185–190. [Google Scholar] [CrossRef]
- Cruvinel Júnior, R.H.; Ferreira, J.S.S.P.; Beteli, R.I.; Silva, É.Q.; Veríssimo, J.L.; Monteiro, R.L.; Suda, E.Y.; Sacco, I.C.N. Foot-Ankle Functional Outcomes of Using the Diabetic Foot Guidance System (SOPeD) for People with Diabetic Neuropathy: A Feasibility Study for the Single-Blind Randomized Controlled FOotCAre (FOCA) Trial I. Pilot Feasibility Stud. 2021, 7. [Google Scholar] [CrossRef]
- Kanchanasamut, W.; Pensri, P. Effects of Weight-Bearing Exercise on a Mini-Trampoline on Foot Mobility, Plantar Pressure and Sensation of Diabetic Neuropathic Feet; a Preliminary Study. Diabet Foot Ankle 2017, 8, 1287239. [Google Scholar] [CrossRef] [PubMed]
- Kruse, R.L.; Lemaster, J.W.; Madsen, R.W. Fall and Balance Outcomes after an Intervention to Promote Leg Strength, Balance, and Walking in People with Diabetic Peripheral Neuropathy: “Feet First” Randomized Controlled Trial. Phys. Ther. 2010, 90, 1568–1579. [Google Scholar] [CrossRef]
- Sartor, C.D.; Hasue, R.H.; Cacciari, L.P.; Butugan, M.K.; Watari, R.; Pássaro, A.C.; Giacomozzi, C.; Sacco, I.C. Effects of Strengthening, Stretching and Functional Training on Foot Function in Patients with Diabetic Neuropathy: Results of a Randomized Controlled Trial. BMC Musculoskelet Disord. 2014, 15, 137. [Google Scholar] [CrossRef]
- Win, M.M.T.; Fukai, K.; Nyunt, H.H.; Linn, K.Z. Hand and Foot Exercise for Diabetic Peripheral Neurophaty: A Randomized Controlled Trial. Nurs. Health Sci. 2020, 22, 416–426. [Google Scholar] [CrossRef]
- Cerrahoglu, L.; Koşan, U.; Sirin, T.C.; Ulusoy, A. Range of Motion and Plantar Pressure Evaluation for the Effects of Self-Care Foot Exercises on Diabetic Patients with and Without Neuropathy. J. Am. Podiatr. Med. Assoc. 2016, 106, 189–200. [Google Scholar] [CrossRef]
- Chang, C.-F.; Chang, C.-C.; Hwang, S.-L.; Chen, M.-Y. Effects of Buerger Exercise Combined Health-Promoting Program on Peripheral Neurovasculopathy Among Community Residents at High Risk for Diabetic Foot Ulceration. Worldviews Evid. Based Nurs. 2015, 12, 145–153. [Google Scholar] [CrossRef]
- Fayed, E.E.; Mohamed Badr, N.; Mahmoud, S.; Hakim, S.A. Exercise Therapy Improves Planter Pressure Distribution in Patients with Diabetic Peripheral Neuropathy. Int. J. PharmTech Res. 2016, 9, 151–159. [Google Scholar]
- Francia, P.; Anichini, R.; de Bellis, A.; Seghieri, G.; Lazzeri, R.; Paternostro, F.; Gulisano, M. Diabetic Foot Prevention: The Role of Exercise Therapy in the Treatment of Limited Joint Mobility, Muscle Weakness and Reduced Gait Speed. Ital. J. Anat. Embryol. 2015, 120, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, J.R.; Lidtke, R.H.; Shott, S. The Effects of Range-of-Motion Therapy on the Plantar Pressures of Patients with Diabetes Mellitus. J. Am. Podiatr. Med. Assoc. 2002, 92, 483–490. [Google Scholar] [CrossRef]
- Monteiro, R.L.; Ferreira, J.S.S.P.; Silva, É.Q.; Cruvinel-Júnior, R.H.; Veríssimo, J.L.; Bus, S.A.; Sacco, I.C.N. Foot–Ankle Therapeutic Exercise Program Can Improve Gait Speed in People with Diabetic Neuropathy: A Randomized Controlled Trial. Sci. Rep. 2022, 12, 7561. [Google Scholar] [CrossRef] [PubMed]
- Pataky, Z.; de León Rodriguez, D.; Allet, L.; Golay, A.; Assal, M.; Assal, J.P.; Hauert, C.A. Biofeedback for Foot Offloading in Diabetic Patients with Peripheral Neuropathy. Diabet. Med. 2010, 27, 61–64. [Google Scholar] [CrossRef]
- York, R.M.; Perell-Gerson, K.L.; Barr, M.; Durham, J.; Roper, J.M. Motor Learning of a Gait Pattern to Reduce Forefoot Plantar Pressures in Individuals with Diabetic Peripheral Neuropathy. PM&R 2009, 1, 434–441. [Google Scholar] [CrossRef]
- Schaper, N.C.; van Netten, J.J.; Apelqvist, J.; Bus, S.A.; Hinchliffe, R.J.; Lipsky, B.A. Practical Guidelines on the Prevention and Management of Diabetic Foot Disease (IWGDF 2019 Update). Diabetes Metab. Res. Rev. 2020, 36, e3266. [Google Scholar] [CrossRef]
- Allet, L.; Armand, S.; de Bie, R.A.; Golay, A.; Monnin, D.; Aminian, K.; Staal, J.B.; de Bruin, E.D. The Gait and Balance of Patients with Diabetes Can Be Improved: A Randomised Controlled Trial. Diabetologia 2010, 53, 458–466. [Google Scholar] [CrossRef]
- Silva, É.Q.; Santos, D.P.; Beteli, R.I.; Monteiro, R.L.; Ferreira, J.S.S.P.; Cruvinel-Junior, R.H.; Donini, A.; Verissímo, J.L.; Suda, E.Y.; Sacco, I.C.N. Feasibility of a Home-Based Foot–Ankle Exercise Programme for Musculoskeletal Dysfunctions in People with Diabetes: Randomised Controlled FOotCAre (FOCA) Trial II. Sci. Rep. 2021, 11, 12404. [Google Scholar] [CrossRef]
- Silva, E.Q.; Suda, E.Y.; Santos, D.P.; Veríssimo, J.L.; Ferreira, J.S.S.P.; Cruvinel Júnior, R.H.; Monteiro, R.L.; Sartor, C.D.; Sacco, I.C.N. Effect of an Educational Booklet for Prevention and Treatment of Foot Musculoskeletal Dysfunctions in People with Diabetic Neuropathy: The FOotCAre (FOCA) Trial II, a Study Protocol of a Randomized Controlled Trial. Trials 2020, 21, 180. [Google Scholar] [CrossRef]
- Veríssimo, J.L.; Sacco, I.C.N.; de Almeida, M.H.M.; Sartor, C.D.; Suda, E.Y. Development of a Customized Booklet of Foot-Ankle Exercises for People with Diabetes Mellitus as a Management and Prevention Tool for Musculoskeletal Complications: A Customized Booklet of Foot-Ankle Exercises for People with Diabetes. Braz. J. Phys. Ther. 2022, 26, 100402. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G.; Bland, J.M. How to Randomise. Br. Med. J. 1999, 319, 703–704. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemmer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement from the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef] [PubMed]
- Sartor, C.; Oliveira, M.; Campos, V.; Ferreira, J.; Sacco, I. Brazilian Journal of Cross-Cultural Adaptation and Measurement Properties of the Brazilian Version of the Michigan Neuropathy Screening Instrument. Braz. J. Phys. Ther. 2018, 22, 222–230. [Google Scholar] [CrossRef]
- McIllhatton, A.; Lanting, S.; Lambkin, D.; Leigh, L.; Casey, S.; Chuter, V. Reliability of Recommended Non-Invasive Chairside Screening Tests for Diabetes-Related Peripheral Neuropathy: A Systematic Review with Meta-Analyses. BMJ Open Diabetes Res. Care 2021, 9, e002528. [Google Scholar] [CrossRef] [PubMed]
- Perkins, B.A.; Olaleye, D.; Zinman, B.; Bril, V. Simple Screening Test for Peripheral Neuropathy in the Diabetes Clinic. Diabetes Care 2001, 24, 250–256. [Google Scholar] [CrossRef]
- Mickle, K.J.; Chambers, S.; Steele, J.R.; Munro, B.J. A Novel and Reliable Method to Measure Toe Flexor Strength. Clin. Biomech. 2008, 23, 683. [Google Scholar] [CrossRef]
- Ellis, S.J.; Stoecklein, H.; Yu, J.C.; Syrkin, G.; Hillstrom, H.; Deland, J.T. The Accuracy of an Automasking Algorithm in Plantar Pressure Measurements. HSS J. 2011, 7, 57–63. [Google Scholar] [CrossRef]
- Burrows, R.F.; Gan, E.T.; Gallus, A.S.; Wallace, E.M.; Burrows, E.A. A Randomised Double-Blind Placebo Controlled Trial of Low Molecular Weight Heparin as Prophylaxis in Preventing Venous Thrombolic Events after Caesarean Section: A Pilot Study. Br. J. Obstet. Gynaecol. 2001, 108, 835–839. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G * Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Suryani, M.; Samekto, W.; Heri-Nugroho; Susanto, H.; Dwiantoro, L. Effect of Foot-Ankle Flexibility and Resistance Exercise in the Secondary Prevention of Plantar Foot Diabetic Ulcer. J. Diabetes Complicat. 2021, 35, 107968. [Google Scholar] [CrossRef] [PubMed]
- Iunes, D.H.; Rocha, C.B.J.; Borges, N.C.S.; Marcon, C.O.; Pereira, V.M.; Carvalho, L.C. Self-Care Associated with Home Exercises in Patients with Type 2 Diabetes Mellitus. PLoS ONE 2014, 9, e114151. [Google Scholar] [CrossRef] [PubMed]
- de Castro, J.P.W.; Ferreira, F.C.; Vargas, J.G.F.; Bosso, L.B.; Nabozny, N.; Martins, C.M.; Farhat, G.; Gomes, R.Z. Accuracy of Foot Pressure Measurement on Predicting the Development of Foot Ulcer in Patients with Diabetes: A Systematic Review and Meta-Analysis. J. Diabetes Sci. Technol. 2021, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Searle, A.; Spink, M.J.; Oldmeadow, C.; Chiu, S.; Chuter, V.H. Calf Muscle Stretching Is Ineffective in Increasing Ankle Range of Motion or Reducing Plantar Pressures in People with Diabetes and Ankle Equinus: A Randomised Controlled Trial. Clin. Biomech. 2019, 69, 52–57. [Google Scholar] [CrossRef]
- Zimny, S.; Schatz, H.; Pfohl, M. The Role of Limited Joint Mobility in Diabetic Patients with an At-Risk Foot. Diabetes Care 2004, 27, 942–946. [Google Scholar] [CrossRef]
- Maeshige, N.; Uemura, M.; Hirasawa, Y.; Yoshikawa, Y.; Moriguchi, M.; Kawabe, N.; Fujii, M.; Terashi, H.; Fujino, H. Immediate Effects of Weight-Bearing Calf Stretching on Ankle Dorsiflexion Range of Motion and Plantar Pressure During Gait in Patients with Diabetes Mellitus. Int. J. Lower Extremity Wounds 2021, 1–7. [Google Scholar] [CrossRef]
- Fernando, M.; Crowther, R.; Lazzarini, P.; Sangla, K.; Cunningham, M.; Buttner, P.; Golledge, J. Biomechanical Characteristics of Peripheral Diabetic Neuropathy: A Systematic Review and Meta-Analysis of Findings from the Gait Cycle, Muscle Activity and Dynamic Barefoot Plantar Pressure. Clin. Biomech. 2013, 28, 831–845. [Google Scholar] [CrossRef]
- Mueller, M.J.; Sinacore, D.R.; Hoogstrate, S.; Daly, L. Hip and Ankle Walking Strategies: Effect on Peak Plantar Pressures and Implications for Neuropathic Ulceration. Arch. Phys. Med. Rehabil. 1994, 75, 1196–1200. [Google Scholar] [CrossRef]
- Yavuzer, G.; Yetkin, I.; Toruner, F.B.; Koca, N.; Bolukbas, N. Gait Deviations of Patients with Diabetes Mellitus: Looking beyond Peripheral Neuropathy. Eur. Medicophys. 2006, 42, 127–133. [Google Scholar]
- Grossman, M. On the Concept of Helath Capital and the Demand for Health. J. Polit. Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef]

| Intervention Group (n = 25) Mean (SD) | Control Group (n = 25) Mean (SD) | |
|---|---|---|
| Age (years) | 59.1 (6.4) | 56.5 (9.4) |
| Body mass (kg) | 74.4 (15.6) | 74.2 (14.8) |
| Height (cm) | 162.0 (0.1) | 164.0 (0.1) |
| Body mass index (kg/m2) | 23.5 (4.8) | 22.9 (3.6) |
| Sex (Male/Female) | (M = 6/F = 19) | (M = 5/F = 20) |
| Type 2 Diabetes (number of participants, %) | 22 (88%) | 19 (76%) |
| Time of onset of diabetes (years) | 13.8 (10.0) | 18.2 (9.8) |
| Education | ||
| Elementary education incomplete | 4 (16%) | 2 (8%) |
| Elementary education complete | 6 (24%) | 7 (28%) |
| High school complete | 7(28%) | 9 (36%) |
| Higher education incomplete | 1 (4%) | 2 (8%) |
| Higher education complete | 7 (28%) | 5 (20%) |
| Socioeconomic status | ||
| 1 to 3 Brazilian minimum salary/month | 13 (52%) | 15 (60%) |
| 3 to 5 Brazilian minimum salary/month | 5 (20%) | 4 (16%) |
| Up to 5 Brazilian minimum salary/month | 6 (24%) | 2 (8%) |
| DPN symptoms (MNSI score) | 5.4 (1.9) | 6.9 (2.1) |
| DPN severity (Fuzzy score) | 4.4 (2.6) | 4.6 (2.3) |
| Tactile sensitivity (number of areas, median (IQR)) | 0 (0–4) | 0 (0–3) |
| Vibration Perception (number of feet, %) | ||
| absent—L | 10 (40%) | 6 (24%) |
| absent—R | 10 (40%) | 9 (36%) |
| reduced—L | 5 (20%) | 9 (36%) |
| reduced—R | 3 (12%) | 5 (20%) |
| Foot Strength (%BW) | ||
| Hallux—L | 13.8 (6.6) | 11.7 (6.2) |
| Hallux—R | 13.8 (6.9) | 13.6 (6.8) |
| Toe—L | 9.4 (5.2) | 9.3 (5.1) |
| Toe—R | 9.7 (4.2) | 8.5 (2.9) |
| Intervention Group (n = 25) | Control Group (n = 25) | Between-Group Difference (CI 95%) | GEE Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | p | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | p | 8 Weeks | 16 Weeks | Group × Time | Group | Time |
| DPN symptoms (MNSI score) | 5.3 (0.5) | 5.6 (0.5) | - | 6.2 (0.6) | 6.0 (0.6) | - | −0.9 (−2.3 to 0.6) | −0.4 (−1.9 to 1.2) | 0.276 | 0.132 | 0.346 |
| DPN severity (Fuzzy score) | 3.7 (0.5) | 3.9 (0.6) | - | 3.3 (0.5) | 3.6 (0.4) | - | 0.4 (−1.0 to 1.8) | 0.4 (−1.1 to 1.8) | 0.765 | 0.641 | 0.002 |
| Tactile sensitivity (number of areas, (median, IQR]) | 0 [0–1] | 0 [0–0] | - | 0 [0–2] | 0 [0–0.75] | - | - | 0.056 | 0.618 | 0.669 | |
| Vibration Perception (number of participants, %) | |||||||||||
| absent—L | 2 (11.8%) | 1 (7.1%) | 0.876 | 2 (11.1%) | 2 (11.1%) | 0.615 | - | - | - | - | |
| absent—R | 10 (55.6%) | 5 (14.3%) | 0.529 | 9 (52.9%) | 0 (0.0%) | 0.476 | - | - | - | - | |
| reduced—L | 9 (52.9%) | 8 (57.1%) | 0.581 | 8 (44.4%) | 8 (44.4%) | 0.677 | - | - | - | - | |
| reduced—R | 2 (11.1%) | 7 (50%) | 0.018 | 1 (5.9%) | 7 (38.9%) | 0.702 | - | - | - | - | |
| Foot Strength (%BW) | |||||||||||
| Hallux—L | 13.8 (1.1) | 13.1 (1.3) | - | 11.6 (1.3) | 12.0 (1.2) | - | 2.2 (−1.3 to 5.6) | 1.0 (−2.5 to 4.7) | 0.716 | 0.270 | 0.989 |
| Hallux—R | 13.8 (1.0) | 14.0 (1.1) | - | 11.6 (1.0) | 13.3 (1.2) | - | 2.2 (−0.6 to 4.9) | 0.6 (−2.5 to 3.8) | 0.415 | 0.453 | 0.346 |
| Toes—L | 10.5 (1.1) | 10.2 (1.0) | - | 9.3 (1.0) | 9.7 (0.9) | - | 1.1 (−1.8 to 4.1) | 0.6 (−2.2 to 3.3) | 0.629 | 0.638 | 0.394 |
| Toes—R | 8.6 (0.9) | 10.3 (1.0) | - | 8.9 (0.7) | 9.1 (0.8) | - | 0.3 (−0.6 to 1.9) | 1.2 (−1.3 to 3.7) | 0.210 | 0.478 | 0.344 |
| Intervention Group (n = 25) | Control Group (n = 25) | Between-Group Difference (CI 95%) | GEE Analysis | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Region of Interest | Variables | Baseline Estimated Mean (SE) | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | Baseline Estimated Mean (SE) | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | 8 Weeks | 16 Weeks | Group × Time | Group | Time |
| Toes | Contact Area [cm2] | 10.26 (0.56) | 18.26 (1.03) | 19.02 (1.02) | 10.76 (0.49) | 18.06 (0.89) | 17.76 (0.94) | 0.20 (−2.47 to 2.87) | 1.25 (−1.47 to 3.98) | 0.384 | 0.844 | <0.001 |
| Peak [kPa] | 391.10 (26.82) | 325.42 (27.68) | 365.34 (29.73) | 361.56 (19.21) | 365.02 (29.57) | 366.29 (29.83) | −39.59 (−118.99 to 39.79) | −0.95 (−83.51 to 81.60) | 0.209 | 0.886 | 0.269 | |
| Pressure–time integral [(kPa)·s] | 133.54 (9.70) | 104.11 (8.50) | 129.79 (16.09) | 120.08 (8.01) | 118.78 (10.30) | 116.10 (9.13) | −14.66 (−40.85 to 11.53) | 13.68 (−22.58 to 49.96) | 0.054 | 0.784 | 0.045 | |
| Hallux | Contact Area [cm2] | 18.15 (0.61) | 8.48 (0.54) | 8.37 (0.35) | 16.07 (0.59) | 8.87 (0.59) | 8.84 (0.56) | −0.38 (−1.97 to 1.20) | −0.46 (−1.77 to 0.84) | 0.185 | 0.886 | <0.001 |
| Peak [kPa] | 406.20 (41.89) | 457.92 (58.67) | 457.98 (53.12) | 353.08 (29.76) | 402.18 (51.63) | 420.45 (53.76) | 55.73 (−97.45 to 208.92) | 37.52 (−110.61 to 185.67) | 0.876 | 0.411 | 0.030 | |
| Pressure–time integral [(kPa)·s] | 122.46 (13.57) | 133.79 (25.34) | 137.03 (18.24) | 96.82 (9.85) | 106.86 (14.63) | 127.91 (17.52) | 26.92 (−30.42 to 84.27) | 9.11 (−40.46 to 58.70) | 0.296 | 0.293 | 0.003 | |
| Forefoot medial | Contact Area [cm2] | 9.46 (0.40) | 10.78 (0.58) | 10.65 (0.64) | 10.03 (0.60) | 9.94 (0.75) | 10.45 (0.71) | 0.83 (−1.03 to 2.70) | 0.20 (−1.68 to 2.09) | 0.133 | 0.860 | 0.025 |
| Peak [kPa] | 294.05 (29.69) | 326.05 (35.43) | 341.09 (48.19) | 322.56 (33.79) | 289.13 (44.75) | 311.74 (37.57) | 36.91 (−74.95 to 148.79) | 29.34 (−90.43 to 149.12) | 0.172 | 0.787 | 0.763 | |
| Pressure–time integral [(kPa)·s] | 102.36 (9.67) | 110.24 (12.76) | 120.21 (15.25) | 114.20 (15.72) | 101.30 (19.67) | 117.07 (15.89) | 8.93 (−37.02 to 54.89) | 3.14 (−40.04 to 46.32) | 0.358 | 0.998 | 0.259 | |
| Forefoot central | Contact Area [cm2] | 26.18 (0.57) | 26.81 (0.76) | 26.59 (0.77) | 27.22 (0.55) | 27.47 (0.63) | 27.03 (0.61) | −0.65 (−2.61 to 1.29) | −0.43 (−2.36 to 1.49) | 0.546 | 0.419 | 0.224 |
| Peak [kPa] | 554.00 (36.21) | 592.86 (49.06) | 596.23 (34.83) | 556.96 (32.51) | 558.92 (43.88) | 585.06 (45.04) | 33.94 (−95.07 to 162.96) | 11.16 (−100.43 to 122.76) | 0.742 | 0.784 | 0.304 | |
| Pressure–time integral [(kPa)·s] | 205.91 (16.62) | 198.47 (16.29) | 200.23 (12.18) | 192.64 (11.27) | 184.84 (11.51) | 191.37 (11.78) | 13.62 (−25.48 to 52.73) | 8.86 (−24.36 to 42.08) | 0.919 | 0.482 | 0.525 | |
| Forefoot lateral | Contact Area [cm2] | 12.29 (0.38) | 12.39 (0.58) | 12.30 (0.45) | 11.72 (0.47) | 12.31 (0.52) | 11.74 (0.53) | 0.08 (−1.45 to 1.62) | 0.55 (−0.82 to 1.93) | 0.558 | 0.531 | 0.309 |
| Peak [kPa] | 455.69 (37.04) | 460.79 (51.91) | 454.30 (56.75) | 465.58 (44.45) | 479.59 (51.36) | 440.05 (38.89) | −18.79 (−161.94 to 124.34) | 14.24 (−120.60 to 149.09) | 0.773 | 0.940 | 0.615 | |
| Pressure–time integral [(kPa)·s] | 164.05 (13.35) | 149.90 (12.43) | 160.28 (18.94) | 148.15 (13.86) | 149.82 (13.30) | 137.67 (11.72) | 0.08 (−35.61 to 35.77) | 22.61 (−21.05 to 66.27) | 0.241 | 0.448 | 0.745 | |
| Midfoot | Contact Area [cm2] | 14.95 (0.91) | 14.90 (1.10) | 14.98 (0.96) | 15.19 (0.78) | 15.54 (0.92) | 14.69 (0.96) | −0.64 (−3.47 to 2.18) | 0.28 (−2.38 to 2.95) | 0.245 | 0.881 | 0.379 |
| Peak [kPa] | 167.23 (17.79) | 161.60 (16.43) | 151.64 (16.48) | 176.90 (22.21) | 163.70 (19.53) | 164.37 (17.99) | −2.10 (−52.14 to 47.92) | 12.72 (−60.55 to 35.10) | 0.860 | 0.732 | 0.123 | |
| Pressure–time integral [(kPa)·s] | 58.76 (5.69) | 52.08 (6.42) | 51.02 (7.79) | 59.52 (7.60) | 56.05 (7.17) | 51.58 (6.14) | −3.97 (−22.85 to 14.91) | −0.56 (−20.01 to 18.89) | 0.647 | 0.844 | 0.114 | |
| Heel | Contact Area [cm2] | 35.12 (1.08) | 37.03 (1.29) * | 36.59 (1.18) | 34.55 (1.24) | 34.33 (1.60) * | 34.28 (1.49) | 2.70 (1.18 to 4.22) | 2.30 (−1.43 to 6.05) | 0.043 * | 0.314 | 0.177 |
| Peak [kPa] | 341.93 (16.62) | 338.21 (19.01) & | 339.93 (15.71) | 389.30 (23.44) | 402.37 (21.17) & | 378.44 (22.73) | −64.16 (−119.93 to −8.39) | −38.51 (−92.69 to 15.66) | 0.568 | 0.020 & | 0.776 | |
| Pressure–time integral [(kPa)·s] | 100.95 (5.81) | 93.86 (4.06) | 90.11 (3.73) | 105.08 (5.07) | 104.55 (6.34) | 102.15 (5.85) | −10.69 (−25.45 to 4.06) | −12.03 (−25.65 to 1.58) | 0.439 | 0.159 | 0.061 | |
| Intervention Group (n = 25) | Control Group (n = 25) | Between-Group Difference (CI 95%) | GEE Analysis | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline Estimated Mean (SE) | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | Baseline Estimated Mean (SE) | 8-Week Estimated Mean (SE) | 16-Week Estimated Mean (SE) | 8 Weeks | 16 Weeks | Group × Time | Group | Time |
| ANKLE | |||||||||||
| Ankle ROM (degree) | 24.07 (0.65) | 23.66 (0.82) | 24.63 (0.96) | 23.44 (0.65) | 22.71 (0.83) | 24.65 (0.81) | 0.96 (−1.47 to 3.40) | 0.00 (−2.43 to 2.43) | 0.718 | 0.494 | 0.065 |
| Ankle dorsiflexion at heel strike (degree) | −2.53 (1.76) | −0.04 (1.14) | −2.15 (1.81) | −0.51 (1.60) | −0.82 (1.70) | 0.31 (1.49) | −0.78 (−3.25 to 4.82) | −1.76 (−6.49 to 2.95) | 0.463 | 0.437 | 0.738 |
| Ankle plantarflexion at push off (degree) | −9.27 (2.05) | −7.21(1.59) | −10.34 (1.93) | −5.20 (1.83) | −5.33 (2.00) | −8.34 (1.66) | −1.75 (−6.76 to 3.26) | −2.00 (−7.00 to 2.99) | 0.759 | 0.134 | 0.215 |
| Ankle plantarflexor moment at heel strike (Nm/BM·Height) | −0.05 (0.01) | −0.04 (0.01) | −0.05 (0.02) | −0.05 (0.01) | −0.03 (0.01) | −0.07 (0.03) | −0.01 (−0.04 to 0.02) | −0.02 (−0.10 to 0.06) | 0.690 | 0.835 | 0.492 |
| Ankle plantarflexor moment at push off (Nm/BM·Height) | 1.29 (0.03) | 1.28 (0.04) | 1.20 (0.05) | 1.23 (0.05) | 1.16 (0.08) | 1.25 (0.03) | 0.12 (−0.06 to 0.31) | −0.05 (−1.72 to 0.06) | 0.163 | 0.435 | 0.372 |
| Ankle peak eccentric power at the push off (W/BM·Height) | 2.24 (0.10) | 2.17 (0.11) | 2.06 (0.13) | 2.36 (0.16) | 2.20 (0.18) | 2.32 (0.11) | −0.02 (−0.46 to 0.41) | −2.51 (−5.87 to 8.41) | 0.623 | 0.397 | 0.345 |
| KNEE AND HIP | |||||||||||
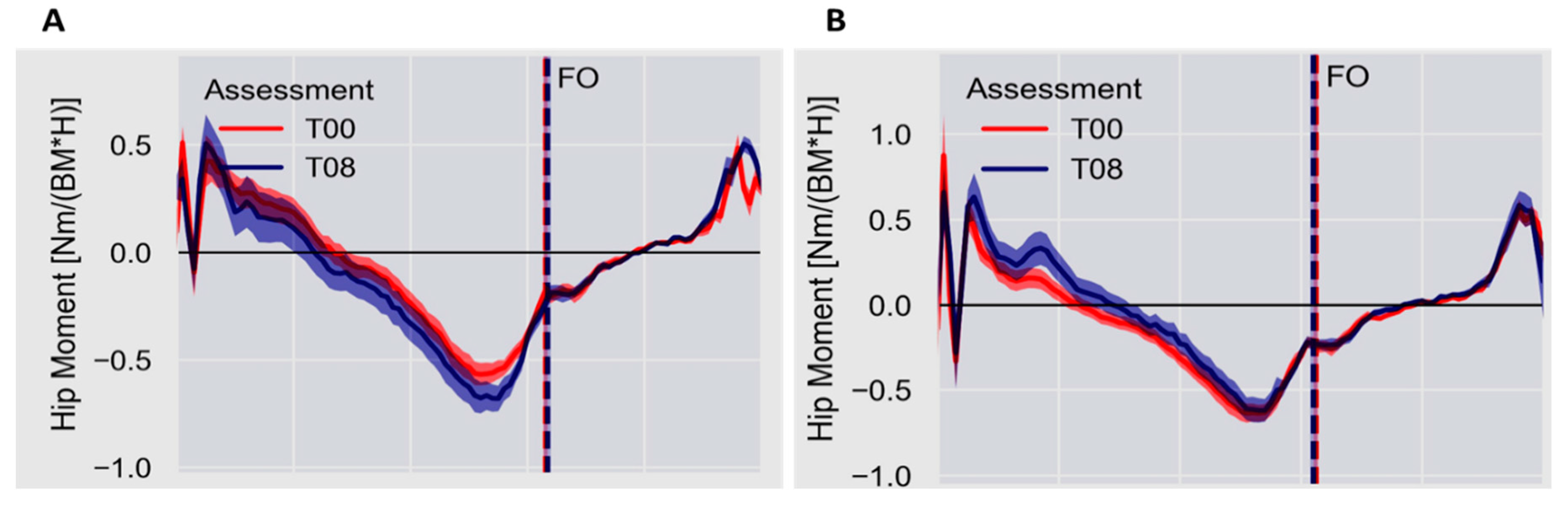
| Hip flexor moment at heel strike (Nm/BM·Height) | 0.09 (0.12) | 0.24 (0.08) * | 0.27 (0.09) | 0.20 (0.24) | 0.45 (0.27) *# | 0.26 (0.33) # | −0.21 (−0.27 to −0.15) | 0.01 (−1.22 to 0.15) | 0.010 * | 0.266 | 0.007 # |
| Hip extensor moment at push off (Nm/BM·Height) | −0.76 (0.05) | −0.83 (0.05) | −0.94 (0.07) | −0.75 (0.05) # | −0.73 (0.07) | −0.96 (0.06) # | −0.09 (−0.26 to 0.08) | 0.02 (−0.16 to 0.21) | 0.317 | 0.693 | <0.001 # |
| Knee flexor moment at heel strike (Nm/BM·Height) | 0.21 (0.03) | 0.18 (0.04) | 0.28 (0.07) & | 0.33 (0.05) | 0.28 (0.04) | 0.41 (0.05) & | −0.09 (−0.22 to 0.03) | −0.13 (−0.32 to 0.05) | 0.921 | 0.045 & | 0.063 |
| Knee flexor moment at push off (Nm/BM·Height) | 0.05 (0.01) | 0.03 (0.01) | 0.05 (0.01) | 0.01 (0.02) | 0.02 (0.02) # | 0.07 (0.01) # | 0.01 (−0.04 to 0.07) | −0.01 (−0.06 to 0.02) | 0.185 | 0.563 | 0.009 # |
| OXFORD FOOT MODEL | |||||||||||
| Hindfoot to tibia ROM (degree) | 20.09 (1.81) | 22.19 (2.31) | 20.66 (1.67) | 20.34 (1.34) | 22.61 (1.77) | 27.44 (5.20) | −0.41 (−5.30 to 6.13) | −6.58 (−16.57 to 3.40) | 0.486 | 0.323 | 0.256 |
| Hindfoot to tibia peak angle (degree) | 10.30 (1.34) | 14.54 (1.94) | 10.51 (1.74) | 10.92 (1.63) | 12.04 (1.83) | 14.28 (3.20) | 2.59 (−2.74 to 7.75) | −3.76 (−10.92 to 3.38) | 0.243 | 0.760 | 0.129 |
| Forefoot to hindfoot ROM (degree) | 11.98 (1.40) | 11.78 (1.31) | 12.00 (1.17) | 13.35 (0.87) | 13.31 (1.11) | 14.18 (1.12) | −1.53 (−4.89 to 1.83) | 2.17 (−1.01 to 5.36) | 0.865 | 0.109 | 0.726 |
| Forefoot to hindfoot peak angle (degree) | 8.04 (1.97) | 9.23 (4.21) | 5.38 (0.72) | 8.35 (0.78) | 8.69 (0.95) | 10.70 (3.21) | 0.53 (−7.93 to 9.00) | −5.31 (−11.71 to 1.15) | 0.346 | 0.426 | 0.930 |
| Hallux to forefoot ROM (degree) | 23.35 (2.15) | 27.00 (2.55) | 26.35 (2.13) | 23.77 (2.10) | 24.26 (2.11) | 25.31 (1.45) | 2.74 (−3.76 to 9.24) | 1.04 (−4.02 to 6.11) | 0.760 | 0.598 | 0.417 |
| Hallux to forefoot peak angle (degree) | 21.31 (2.95) | 23.29 (2.50) | 18.42 (5.90) | 24.68 (4.13) | 23.84 (1.42) | 21.19 (1.43) | −0.55 (−6.20 to 5.09) | −2.77 (−14.67 to 9.13) | 0.852 | 0.452 | 0.396 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, É.Q.; Veríssimo, J.L.; Ferreira, J.S.S.P.; Cruvinel-Júnior, R.H.; Monteiro, R.L.; Suda, E.Y.; Sacco, I.C.N. Effects of a Home-Based Foot–Ankle Exercise Program with Educational Booklet for Foot Dysfunctions in People with Diabetic Neuropathy: Results of the FOCA-II Randomized Controlled Clinical Trial. Appl. Sci. 2023, 13, 1423. https://doi.org/10.3390/app13031423
Silva ÉQ, Veríssimo JL, Ferreira JSSP, Cruvinel-Júnior RH, Monteiro RL, Suda EY, Sacco ICN. Effects of a Home-Based Foot–Ankle Exercise Program with Educational Booklet for Foot Dysfunctions in People with Diabetic Neuropathy: Results of the FOCA-II Randomized Controlled Clinical Trial. Applied Sciences. 2023; 13(3):1423. https://doi.org/10.3390/app13031423
Chicago/Turabian StyleSilva, Érica Q., Jady L. Veríssimo, Jane S. S. P. Ferreira, Ronaldo H. Cruvinel-Júnior, Renan L. Monteiro, Eneida Y. Suda, and Isabel C. N. Sacco. 2023. "Effects of a Home-Based Foot–Ankle Exercise Program with Educational Booklet for Foot Dysfunctions in People with Diabetic Neuropathy: Results of the FOCA-II Randomized Controlled Clinical Trial" Applied Sciences 13, no. 3: 1423. https://doi.org/10.3390/app13031423
APA StyleSilva, É. Q., Veríssimo, J. L., Ferreira, J. S. S. P., Cruvinel-Júnior, R. H., Monteiro, R. L., Suda, E. Y., & Sacco, I. C. N. (2023). Effects of a Home-Based Foot–Ankle Exercise Program with Educational Booklet for Foot Dysfunctions in People with Diabetic Neuropathy: Results of the FOCA-II Randomized Controlled Clinical Trial. Applied Sciences, 13(3), 1423. https://doi.org/10.3390/app13031423







