Effects of Acute Exposure to Virtually Generated Slip Hazards during Overground Walking
Abstract
:1. Introduction
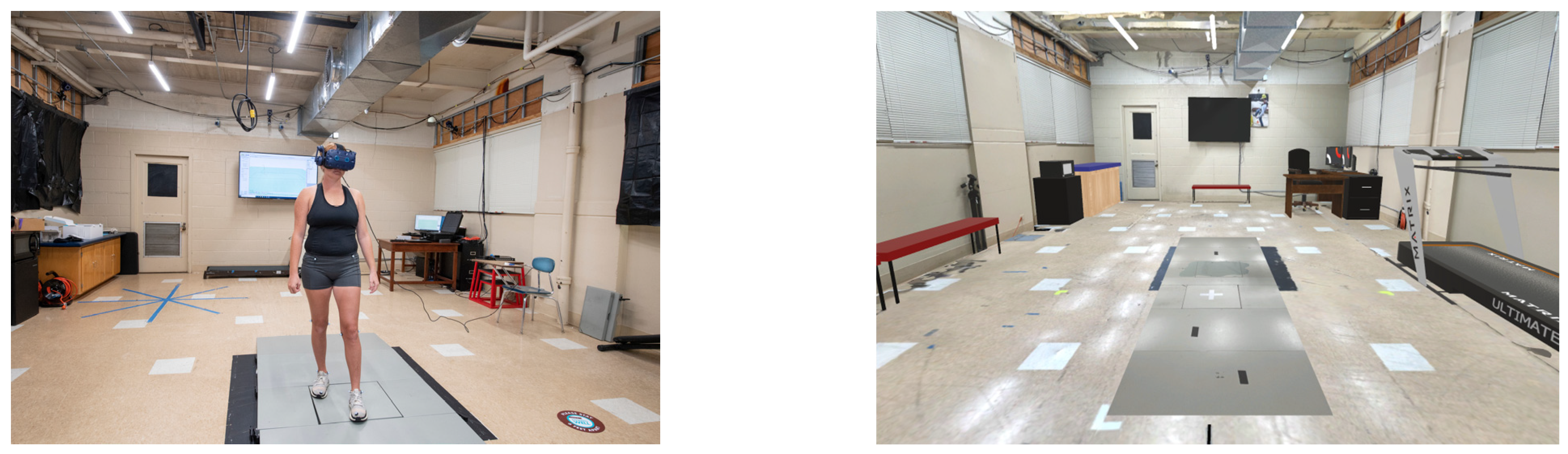
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Instrumentation
2.4. Experimental Procedures
2.5. Data Analysis
2.6. Statistical Analyses
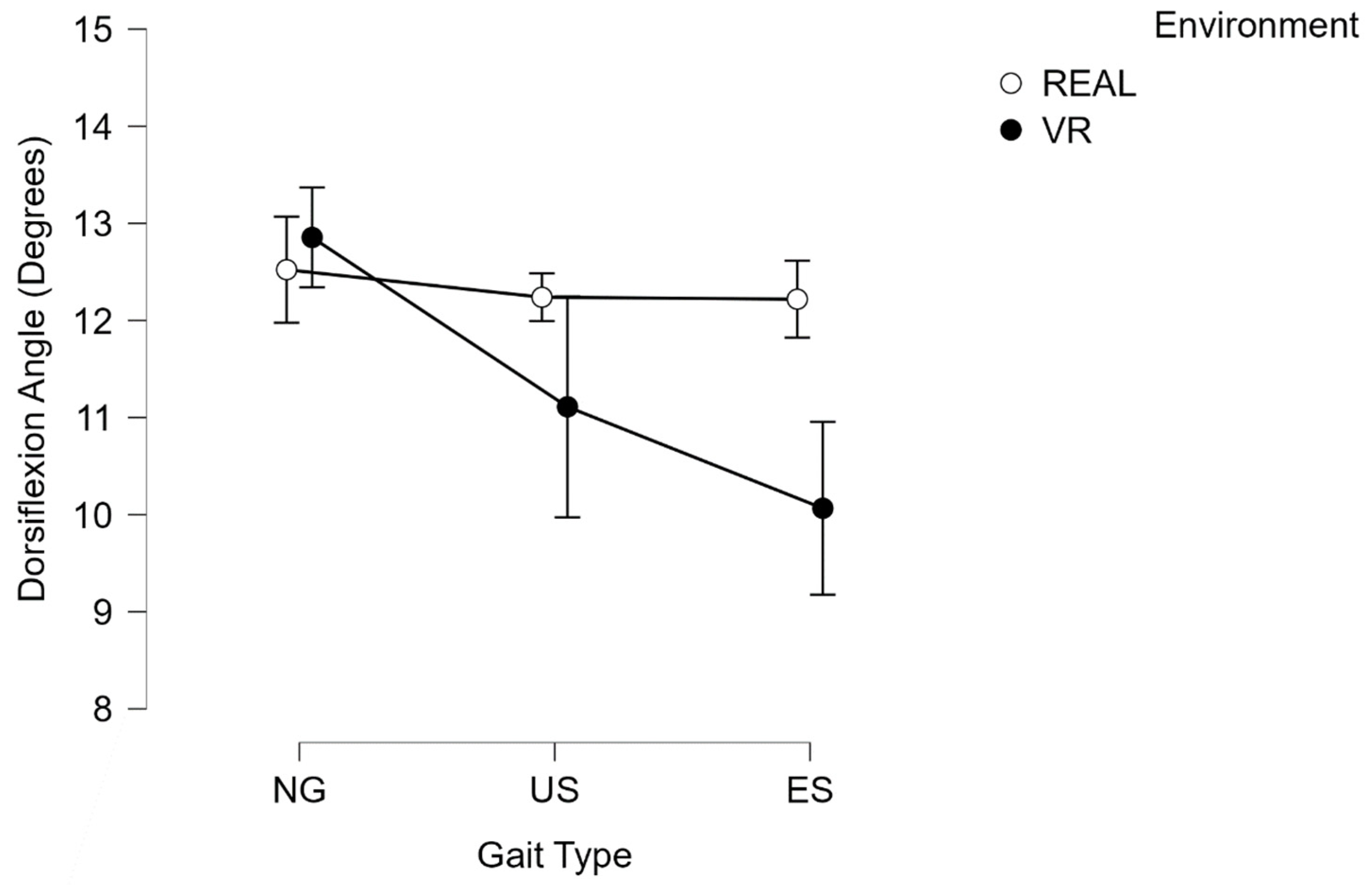
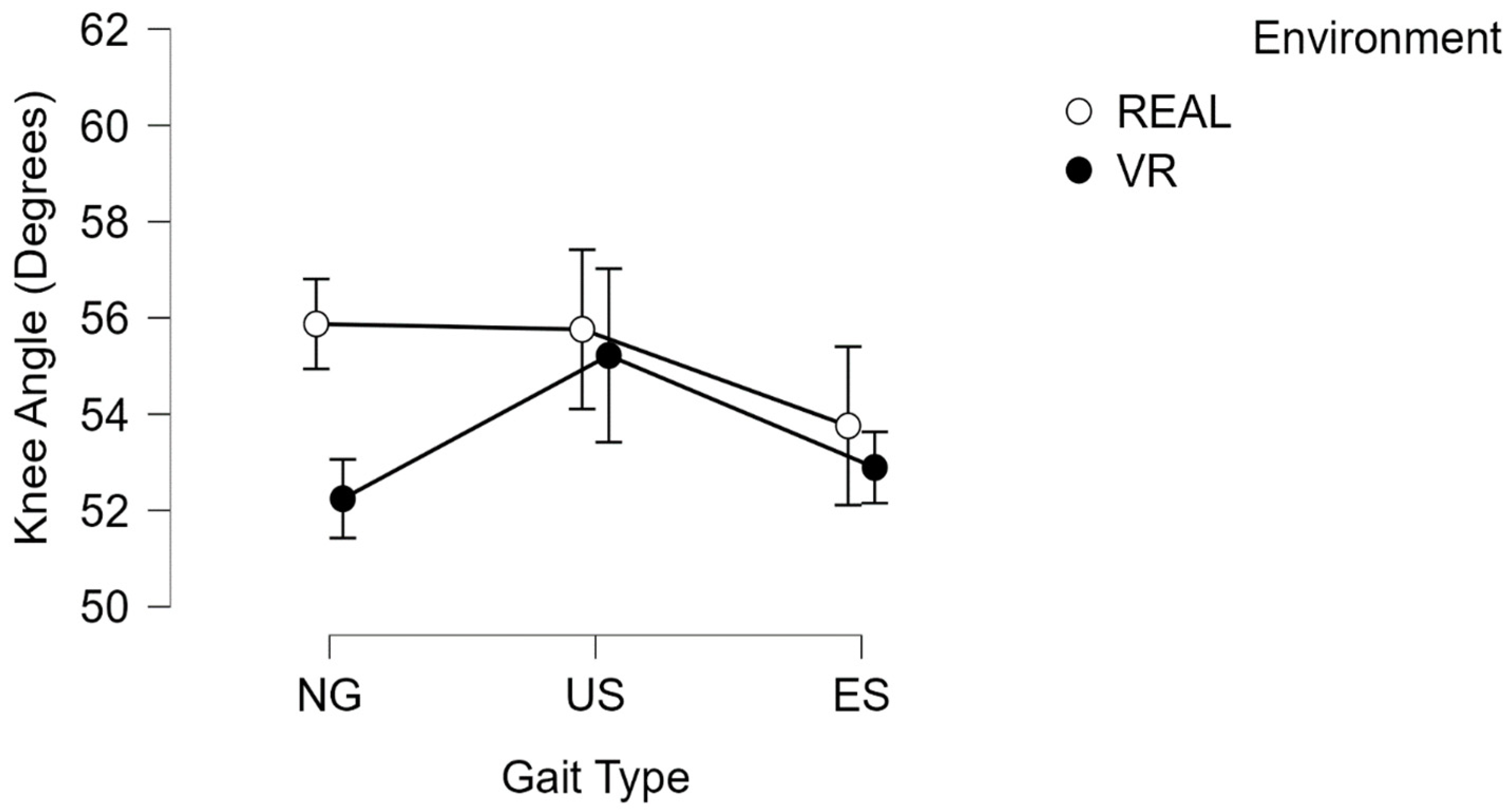
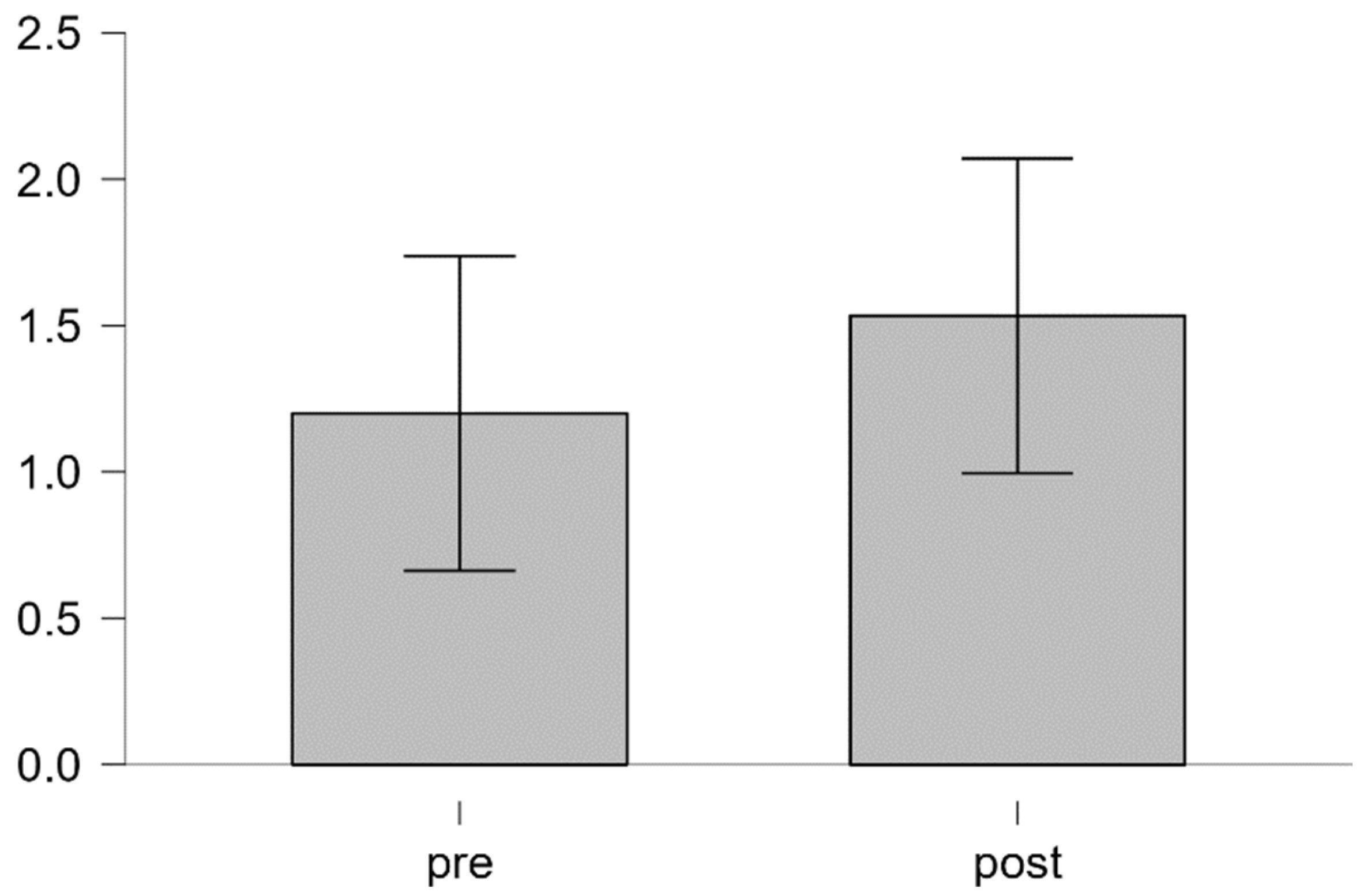
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, H.; Lee, G.; Lee, S.; Ahn, C.R. Assessing exposure to slip, trip, and fall hazards based on abnormal gait patterns predicted from confidence interval estimation. Autom. Constr. 2022, 139, 104253. [Google Scholar] [CrossRef]
- Fatal and Nonfatal Falls, Slips, and Trips in the Construction Industry. 2021. Available online: https://www.bls.gov/opub/ted/2021/fatal-and-nonfatal-falls-slips-and-trips-in-the-construction-industry.htm (accessed on 1 October 2023).
- Pomares, J.C.; Carrión, E.Á.; González, A.; Saez, P.I. Optimization on Personal Fall Arrest Systems. Experimental Dynamic Studies on Lanyard Prototypes. Int. J. Environ. Res. Public Health 2020, 17, 1107. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Qu, X. Pre-impact fall detection. BioMed. Eng. OnLine 2016, 15, 61. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Muehlbauer, T.; Gollhofer, A.; Kressig, R.W.; Zahner, L. An Intergenerational Approach in the Promotion of Balance and Strength for Fall Prevention—A Mini-Review. Gerontology 2011, 57, 304–315. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, H.; Simeonov, P. Preventing falls from roofs: A critical review. Ergonomics 2001, 44, 537–561. [Google Scholar] [CrossRef] [PubMed]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. S2), ii7–ii11. [Google Scholar] [CrossRef] [PubMed]
- National Occupational Research Agenda for Construction. 2018. Available online: https://www.cdc.gov/nora/councils/const/pdfs/National_Occupational_Research_Agenda_for_Construction_June_2018_508.pdf (accessed on 1 October 2023).
- Cham, R.; Redfern, M.S. Lower extremity corrective reactions to slip events. J. Biomech. 2001, 34, 1439–1445. [Google Scholar] [CrossRef]
- Redfern, M.S.; Cham, R.; Gielo-Perczak, K.; Grönqvist, R.; Hirvonen, M.; Lanshammar, H.; Marpet, M.; Pai, C.Y.C., IV; Powers, C. Biomechanics of slips. Ergonomics 2001, 44, 1138–1166. [Google Scholar] [CrossRef]
- Chander, H.; Stewart, E.; Saucier, D.; Nguyen, P.; Luczak, T.; Ball, J.E.; Knight, A.C.; Smith, B.K.; Burch V, R.F.; Prabhu, R.K. Closing the Wearable Gap—Part III: Use of Stretch Sensors in Detecting Ankle Joint Kinematics During Unexpected and Expected Slip and Trip Perturbations. Electronics 2019, 8, 1083. [Google Scholar] [CrossRef]
- Kim, S.; Joo, K.-S.; Liu, J.; Sohn, J.-H. Lower extremity kinematics during forward heel-slip. THC 2019, 27, 345–356. [Google Scholar] [CrossRef]
- Hu, X.; Qu, X. An individual-specific fall detection model based on the statistical process control chart. Saf. Sci. 2014, 64, 13–21. [Google Scholar] [CrossRef]
- Hu, X.; Li, Y.; Chen, G.; Zhao, Z.; Qu, X. Identification of balance recovery patterns after slips using hierarchical cluster analysis. J. Biomech. 2022, 143, 111281. [Google Scholar] [CrossRef]
- Best, R.; Begg, R. Overview of Movement Analysis and Gait Features. In Computational Intelligence and Its Applications; Begg, R., Palaniswami, M., Eds.; IGI Global: Hershey, PA, USA, 2006; pp. 1–69. [Google Scholar] [CrossRef]
- Debelle, H.; Harkness-Armstrong, C.; Hadwin, K.; Maganaris, C.N.; O’Brien, T.D. Recovery From a Forward Falling Slip: Measurement of Dynamic Stability and Strength Requirements Using a Split-Belt Instrumented Treadmill. Front. Sports Act. Living 2020, 2, 82. [Google Scholar] [CrossRef]
- Ferreira, R.N.; Ribeiro, N.F.; Figueiredo, J.; Santos, C.P. Provoking Artificial Slips and Trips towards Perturbation-Based Balance Training: A Narrative Review. Sensors 2022, 22, 9254. [Google Scholar] [CrossRef]
- Cho, G.H.; Hwangbo, G.; Shin, H.S. The Effects of Virtual Reality-based Balance Training on Balance of the Elderly. J. Phys. Ther. Sci. 2014, 26, 615–617. [Google Scholar] [CrossRef] [PubMed]
- Duque, G.; Boersma, D.; Loza-Diaz, G.; Hassan, S.; Suarez, H.; Geisinger, D.; Suriyaarachchi, P.; Sharma, A.; Demontiero, O. Effects of balance training using a virtual-reality system in older fallers. CIA 2013, 2013, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Phu, S.; Vogrin, S.; Al Saedi, A.; Duque, G. Balance training using virtual reality improves balance and physical performance in older adults at high risk of falls. CIA 2019, 14, 1567–1577. [Google Scholar] [CrossRef] [PubMed]
- Prasertsakul, T.; Kaimuk, P.; Chinjenpradit, W.; Limroongreungrat, W.; Charoensuk, W. The effect of virtual reality-based balance training on motor learning and postural control in healthy adults: A randomized preliminary study. BioMed. Eng. OnLine 2018, 17, 124. [Google Scholar] [CrossRef]
- Mirelman, A.; Patritti, B.L.; Bonato, P.; Deutsch, J.E. Effects of virtual reality training on gait biomechanics of individuals post-stroke. Gait Posture 2010, 31, 433–437. [Google Scholar] [CrossRef]
- Liao, Y.-Y.; Yang, Y.-R.; Cheng, S.-J.; Wu, Y.-R.; Fuh, J.-L.; Wang, R.-Y. Virtual Reality-Based Training to Improve Obstacle-Crossing Performance and Dynamic Balance in Patients With Parkinson’s Disease. Neurorehabilit. Neural Repair 2015, 29, 658–667. [Google Scholar] [CrossRef]
- Fulk, G.D. Locomotor Training and Virtual Reality-based Balance Training for an Individual with Multiple Sclerosis: A Case Report. J. Neurol. Phys. Ther. 2005, 29, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; Bisschop, M.; Myer, G.D.; Benjaminse, A.; Dijkstra, P.U.; van Keeken, H.G.; van Raay, J.J.; Burgerhof, J.G.; Otten, E. Immersive virtual reality improves movement patterns in patients after ACL reconstruction: Implications for enhanced criteria-based return-to-sport rehabilitation. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2280–2286. [Google Scholar] [CrossRef]
- Thornton, M.; Marshall, S.; McComas, J.; Finestone, H.; McCormick, A.; Sveistrup, H. Benefits of activity and virtual reality based balance exercise programmes for adults with traumatic brain injury: Perceptions of participants and their caregivers. Brain Inj. 2005, 19, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Omlor, A.J.; Schwärzel, L.S.; Bewarder, M.; Casper, M.; Damm, E.; Danziger, G.; Mahfoud, F.; Rentz, K.; Sester, U.; Bals, R.; et al. Comparison of immersive and non-immersive virtual reality videos as substitute for in-hospital teaching during coronavirus lockdown: A survey with graduate medical students in Germany. Med. Educ. Online 2022, 27, 2101417. [Google Scholar] [CrossRef]
- Åhman, H.B.; Berglund, L.; Cedervall, Y.; Giedraitis, V.; McKee, K.J.; Rosendahl, E.; Åberg, A.C. Timed ‘Up & Go’ Dual-Task Tests: Age- and Sex-Specific Reference Values and Test–Retest Reliability in Cognitively Healthy Controls. Phys. Ther. 2021, 101, pzab179. [Google Scholar] [CrossRef] [PubMed]
- Tamura, K.; Kocher, M.; Finer, L.; Murata, N.; Stickley, C. Reliability of clinically feasible dual-task tests: Expanded timed get up and go test as a motor task on young healthy individuals. Gait Posture 2018, 60, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Construction Industry Market Is Expected to Be Worth USD 17,247.96 Billion by 2029, Growing at a 7.3% Annual Rate. 2022. Available online: https://www.globenewswire.com/en/news-release/2022/08/23/2502951/0/en/Construction-Industry-Market-Is-Expected-To-Be-Worth-USD-17-247-96-Billion-by-2029-Growing-At-A-7-3-Annual-Rate.html#:~:text=The%20size%20of%20the%20global,USD%2011%2C561.40%20billion%20in%202020 (accessed on 1 October 2023).
- Farra, S.L.; Gneuhs, M.; Hodgson, E.; Kawosa, B.; Miller, E.T.; Simon, A.; Timm, N.; Hausfeld, J. Comparative Cost of Virtual Reality Training and Live Exercises for Training Hospital Workers for Evacuation. Comput. Inf. Nurs 2019, 37, 446–454. [Google Scholar] [CrossRef]
- Booth, V.; Masud, T.; Connell, L.; Bath-Hextall, F. The effectiveness of virtual reality interventions in improving balance in adults with impaired balance compared with standard or no treatment: A systematic review and meta-analysis. Clin. Rehabil. 2014, 28, 419–431. [Google Scholar] [CrossRef]
- Parijat, P.; Lockhart, T.E.; Liu, J. EMG and kinematic responses to unexpected slips after slip training in virtual reality. IEEE Trans. Biomed. Eng. 2015, 62, 593–599. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Bimberg, P.; Weissker, T.; Kulik, A. On the Usage of the Simulator Sickness Questionnaire for Virtual Reality Research. In Proceedings of the 2020 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW), Atlanta, GA, USA, 22–26 March 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 464–467. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed ‘Up & Go’: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Lee, B.-C.; Kim, C.-S.; Seo, K.-H. The Body’s Compensatory Responses to Unpredictable Trip and Slip Perturbations Induced by a Programmable Split-Belt Treadmill. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1389–1396. [Google Scholar] [CrossRef]
- Babadi, S.Y.; Daneshmandi, H. Effects of virtual reality versus conventional balance training on balance of the elderly. Exp. Gerontol. 2021, 153, 111498. [Google Scholar] [CrossRef]
- Cho, K.H.; Lee, K.J.; Song, C.H. Virtual-Reality Balance Training with a Video-Game System Improves Dynamic Balance in Chronic Stroke Patients. Tohoku J. Exp. Med. 2012, 228, 69–74. [Google Scholar] [CrossRef]
- Cham, R.; Redfern, M.S. Load Carrying and Corrective Responses to Slip Events. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2001, 45, 962–966. [Google Scholar] [CrossRef]
- Krause, A.; Freyler, K.; Gollhofer, A.; Stocker, T.; Brüderlin, U.; Colin, R.; Töpfer, H.; Ritzmann, R. Neuromuscular and Kinematic Adaptation in Response to Reactive Balance Training—A Randomized Controlled Study Regarding Fall Prevention. Front. Physiol. 2018, 9, 1075. [Google Scholar] [CrossRef]
- Kiper, P.; Luque-Moreno, C.; Pernice, S.; Maistrello, L.; Agostini, M.; Turolla, A. Functional changes in the lower extremity after non-immersive virtual reality and physiotherapy following stroke. J. Rehabil. Med. 2020, 52, jrm00122. [Google Scholar] [CrossRef] [PubMed]
- Chan, Z.Y.S.; MacPhail, A.J.; Au, I.P.; Zhang, J.H.; Lam, B.M.; Ferber, R.; Cheung, R.T. Walking with head-mounted virtual and augmented reality devices: Effects on position control and gait biomechanics. PLoS ONE 2019, 14, e0225972. [Google Scholar] [CrossRef] [PubMed]
- Kastavelis, D.; Mukherjee, M.; Decker, L.; Stergiou, N. The effect of virtual reality on gait variability. Nonlinear Dyn. Psychol. Life Sci. 2010, 14, 239–256. [Google Scholar]
- Cham, R.; Redfern, M.S. Changes in gait when anticipating slippery floors. Gait Posture 2002, 15, 159–171. [Google Scholar] [CrossRef] [PubMed]
- Chander, H.; Wade, C.; Garner, J.C.; Knight, A.C. Slip initiation in alternative and slip-resistant footwear. Int. J. Occup. Saf. Ergon. 2017, 23, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Nishi, T.; Kamogashira, T.; Fujimoto, C.; Kinoshita, M.; Egami, N.; Sugasawa, K.; Yamasoba, T.; Iwasaki, S. Effects of Peripheral Vestibular Dysfunction on Dynamic Postural Stability Measured by the Functional Reach Test and Timed Up and Go Test. Ann. Otol. Rhinol. Laryngol. 2017, 126, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Pohl, P.S.; Gras, L.Z.; Bosch, P.R.; Ganley, K.J.; Mayer, J. Dual Task Timed Up-and-Go for Older Adults with and without Balance Deficits. Phys. Occup. Ther. Geriatr. 2019, 37, 247–259. [Google Scholar] [CrossRef]
- Van Uem, J.M.T.; Walgaard, S.; Ainsworth, E.; Hasmann, S.E.; Heger, T.; Nussbaum, S.; Hobert, M.A.; Mico-Amigo, E.M.; Van Lummel, R.C.; Berg, D.; et al. Quantitative Timed-Up-and-Go Parameters in Relation to Cognitive Parameters and Health-Related Quality of Life in Mild-to-Moderate Parkinson’s Disease. PLoS ONE 2016, 11, e0151997. [Google Scholar] [CrossRef] [PubMed]
- Tachibana, A.; Noah, J.A.; Bronner, S.; Ono, Y.; Onozuka, M. Parietal and temporal activity during a multimodal dance video game: An fNIRS study. Neurosci. Lett. 2011, 503, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Miller, E.K.; Cohen, J.D. An Integrative Theory of Prefrontal Cortex Function. Annu. Rev. Neurosci. 2001, 24, 167–202. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Drexler, J.; Kennedy, R.C. Research in visually induced motion sickness. Appl. Ergon. 2010, 41, 494–503. [Google Scholar] [CrossRef]
- Chattha, U.A.; Janjua, U.I.; Anwar, F.; Madni, T.M.; Cheema, M.F.; Janjua, S.I. Motion Sickness in Virtual Reality: An Empirical Evaluation. IEEE Access 2020, 8, 130486–130499. [Google Scholar] [CrossRef]
- Martirosov, S.; Bureš, M.; Zítka, T. Cyber sickness in low-immersive, semi-immersive, and fully immersive virtual reality. Virtual Real. 2022, 26, 15–32. [Google Scholar] [CrossRef]
- McHugh, N. Measuring and Minimizing Cybersickness in Virtual Reality. Master’s Thesis, University of Canterbury, Christchurch, New Zealand, 2019. [Google Scholar] [CrossRef]
- Melo, M.; Vasconcelos-Raposo, J.; Bessa, M. Presence and cybersickness in immersive content: Effects of content type, exposure time and gender. Comput. Graph. 2018, 71, 159–165. [Google Scholar] [CrossRef]
- Mirelman, A.; Rochester, L.; Reelick, M.; Nieuwhof, F.; Pelosin, E.; Abbruzzese, G.; Dockx, K.; Nieuwboer, A.; Hausdorff, J.M. V-TIME: A treadmill training program augmented by virtual reality to decrease fall risk in older adults: Study design of a randomized controlled trial. BMC Neurol. 2013, 13, 15. [Google Scholar] [CrossRef] [PubMed]
- Eikema, D.J.A.; Chien, J.H.; Stergiou, N.; Myers, S.A.; Scott-Pandorf, M.M.; Bloomberg, J.J.; Mukherjee, M. Optic flow improves adaptability of spatiotemporal characteristics during split-belt locomotor adaptation with tactile stimulation. Exp. Brain Res. 2016, 234, 511–522. [Google Scholar] [CrossRef] [PubMed]
- Salinas, M.M.; Wilken, J.M.; Dingwell, J.B. How humans use visual optic flow to regulate stepping during walking. Gait Posture 2017, 57, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Semaan, M.B.; Wallard, L.; Ruiz, V.; Gillet, C.; Leteneur, S.; Simoneau-Buessinger, E. Is treadmill walking biomechanically comparable to overground walking? A systematic review. Gait Posture 2022, 92, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, J.W.; Ghez, C.; Ghilardi, M.F. Adaptation to Visuomotor Transformations: Consolidation, Interference, and Forgetting. J. Neurosci. 2005, 25, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Malfait, N.; Gribble, P.L.; Ostry, D.J. Generalization of Motor Learning Based on Multiple Field Exposures and Local Adaptation. J. Neurophysiol. 2005, 93, 3327–3338. [Google Scholar] [CrossRef]
- Mao, Y.; Chen, P.; Li, L.; Huang, D. Virtual reality training improves balance function. Neural Regen. Res. 2014, 9, 1628–1634. [Google Scholar] [CrossRef]
- Srivastava, A.; Taly, A.B.; Gupta, A.; Kumar, S.; Murali, T. Post-stroke balance training: Role of force platform with visual feedback technique. J. Neurol. Sci. 2009, 287, 89–93. [Google Scholar] [CrossRef]
- Bhatt, T.; Wang, E.; Pai, Y.-C. Retention of Adaptive Control Over Varying Intervals: Prevention of Slip- Induced Backward Balance Loss During Gait. J. Neurophysiol. 2006, 95, 2913–2922. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Derby, H.; Conner, N.O.; Hull, J.M.; Hagan, F.; Barfield, S.; Stewart, T.; Jones, J.A.; Knight, A.C.; Chander, H. Effects of Acute Exposure to Virtually Generated Slip Hazards during Overground Walking. Appl. Sci. 2023, 13, 12848. https://doi.org/10.3390/app132312848
Derby H, Conner NO, Hull JM, Hagan F, Barfield S, Stewart T, Jones JA, Knight AC, Chander H. Effects of Acute Exposure to Virtually Generated Slip Hazards during Overground Walking. Applied Sciences. 2023; 13(23):12848. https://doi.org/10.3390/app132312848
Chicago/Turabian StyleDerby, Hunter, Nathan O. Conner, Jacob M. Hull, Faith Hagan, Sally Barfield, Timothy Stewart, J. Adam Jones, Adam C. Knight, and Harish Chander. 2023. "Effects of Acute Exposure to Virtually Generated Slip Hazards during Overground Walking" Applied Sciences 13, no. 23: 12848. https://doi.org/10.3390/app132312848
APA StyleDerby, H., Conner, N. O., Hull, J. M., Hagan, F., Barfield, S., Stewart, T., Jones, J. A., Knight, A. C., & Chander, H. (2023). Effects of Acute Exposure to Virtually Generated Slip Hazards during Overground Walking. Applied Sciences, 13(23), 12848. https://doi.org/10.3390/app132312848






