Mushrooms as Functional Foods for Ménière’s Disease
Abstract
:1. Introduction
2. Ménière’s Disease
Treatment of Ménière’s Disease
3. Ménière’s Disease and Brain Function
4. Five Way Interactions and Ménière’s Disease
5. Nutrition in Idiopathic Endolymphatic Hydrops
6. Mushroom Nutrition in Neurodegenerative Diseases
7. Targeting Neurogenesis with Mushroom Nutraceuticals
8. Mushroom Nutrition in Ménière’s Disease
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Galanakis, C.M. Functionality of Food Components and Emerging Technologies. Foods 2021, 10, 128. [Google Scholar] [CrossRef]
- Shahidi, F. Nutraceuticals and Functional Foods: Whole versus Processed Foods. Trends Food Sci. Technol. 2009, 20, 376–387. [Google Scholar] [CrossRef]
- Łysakowska, P.; Sobota, A.; Wirkijowska, A. Medicinal Mushrooms: Their Bioactive Components, Nutritional Value and Application in Functional Food Production—A Review. Molecules 2023, 28, 5393. [Google Scholar] [CrossRef]
- Coppens, P.; Da Silva, M.F.; Pettman, S. European Regulations on Nutraceuticals, Dietary Supplements and Functional Foods: A Framework Based on Safety. Toxicology 2006, 221, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Rani, M.; Mondal, S.M.; Kundu, P.; Thakur, A.; Chaudhary, A.; Vashistt, J.; Shankar, J. Edible mushroom: Occurrence, management and health benefits. Food Mater. Res. 2023, 3, 21. [Google Scholar] [CrossRef]
- Bell, V.; Silva, C.R.P.G.; Guina, J.; Fernandes, T.H. Mushrooms as Future Generation Healthy Foods. Front. Nutr. 2022, 9, 1050099. [Google Scholar] [CrossRef]
- Yadav, D.; Negi, P.S. Bioactive Components of Mushrooms: Processing Effects and Health Benefits. Food Res. Int. 2021, 148, 110599. [Google Scholar] [CrossRef]
- Chugh, R.M.; Mittal, P.; MP, N.; Arora, T.; Bhattacharya, T.; Chopra, H.; Cavalu, S.; Gautam, R.K. Fungal Mushrooms: A Natural Compound With Therapeutic Applications. Front. Pharmacol. 2022, 13, 925387. [Google Scholar] [CrossRef]
- Dávila Giraldo, L.R.; Pérez Jaramillo, C.C.; Méndez Arteaga, J.J.; Murillo-Arango, W. Nutritional Value and Antioxidant, Antimicrobial and Cytotoxic Activity of Wild Macrofungi. Microorganisms 2023, 11, 1158. [Google Scholar] [CrossRef]
- Galappaththi, M.C.A.; Patabendige, N.M.; Premarathne, B.M.; Hapuarachchi, K.K.; Tibpromma, S.; Dai, D.Q.; Suwannarach, N.; Rapior, S.; Karunarathna, S.C. A Review of Ganoderma Triterpenoids and Their Bioactivities. Biomolecules 2023, 13, 24. [Google Scholar] [CrossRef]
- Bhambri, A.; Srivastava, M.; Mahale, V.G.; Mahale, S.; Karn, S.K. Mushrooms as Potential Sources of Active Metabolites and Medicines. Front. Microbiol. 2022, 13, 837266. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.; Nair, A.; Kulkarni, N.; Todewale, N.; Jobby, R. Exploring Mushroom Polysaccharides for the Development of Novel Prebiotics: A Review. Int. J. Med. Mushrooms 2023, 25, 1–10. [Google Scholar] [CrossRef]
- Kerezoudi, E.N.; Mitsou, E.K.; Gioti, K.; Terzi, E.; Avgousti, I.; Panagiotou, A.; Koutrotsios, G.; Zervakis, G.I.; Mountzouris, K.C.; Tenta, R.; et al. Fermentation of Pleurotus Ostreatus and Ganoderma Lucidum Mushrooms and Their Extracts by the Gut Microbiota of Healthy and Osteopenic Women: Potential Prebiotic Effect and Impact of Mushroom Fermentation Products on Human Osteoblasts. Food Funct. 2021, 12, 1529–1546. [Google Scholar] [CrossRef] [PubMed]
- Ayimbila, F.; Keawsompong, S. Nutritional Quality and Biological Application of Mushroom Protein as a Novel Protein Alternative. Curr. Nutr. Rep. 2023, 12, 290–307. [Google Scholar] [CrossRef] [PubMed]
- González, A.; Cruz, M.; Losoya, C.; Nobre, C.; Loredo, A.; Rodríguez, R.; Contreras, J.; Belmares, R. Edible Mushrooms as a Novel Protein Source for Functional Foods. Food Funct. 2020, 11, 7400–7414. [Google Scholar] [CrossRef]
- Rauf, A.; Joshi, P.B.; Ahmad, Z.; Hemeg, H.A.; Olatunde, A.; Naz, S.; Hafeez, N.; Simal-Gandara, J. Edible Mushrooms as Potential Functional Foods in Amelioration of Hypertension. Phytother. Res. 2023, 37, 2644–2660. [Google Scholar] [CrossRef]
- Singh, R.S.; Walia, A.K.; Kennedy, J.F. Mushroom Lectins in Biomedical Research and Development. Int. J. Biol. Macromol. 2020, 151, 1340–1350. [Google Scholar] [CrossRef]
- Guillamón, E.; García-Lafuente, A.; Lozano, M.; D’arrigo, M.; Rostagno, M.A.; Villares, A.; Martínez, J.A. Edible Mushrooms: Role in the Prevention of Cardiovascular Diseases. Fitoterapia 2010, 81, 715–723. [Google Scholar] [CrossRef]
- Sousa, A.S.; Araújo-Rodrigues, H.; Pintado, M.E. The Health-Promoting Potential of Edible Mushroom Proteins. Curr. Pharm. Des. 2022, 29, 804–823. [Google Scholar] [CrossRef]
- El-Maradny, Y.A.; El-Fakharany, E.M.; Abu-Serie, M.M.; Hashish, M.H.; Selim, H.S. Lectins Purified from Medicinal and Edible Mushrooms: Insights into Their Antiviral Activity against Pathogenic Viruses. Int. J. Biol. Macromol. 2021, 179, 239–258. [Google Scholar] [CrossRef]
- Zhou, R.; Liu, Z.K.; Zhang, Y.N.; Wong, J.H.; Ng, T.B.; Liu, F. Research Progress of Bioactive Proteins from the Edible and Medicinal Mushrooms. Curr. Protein Pept. Sci. 2018, 20, 196–219. [Google Scholar] [CrossRef]
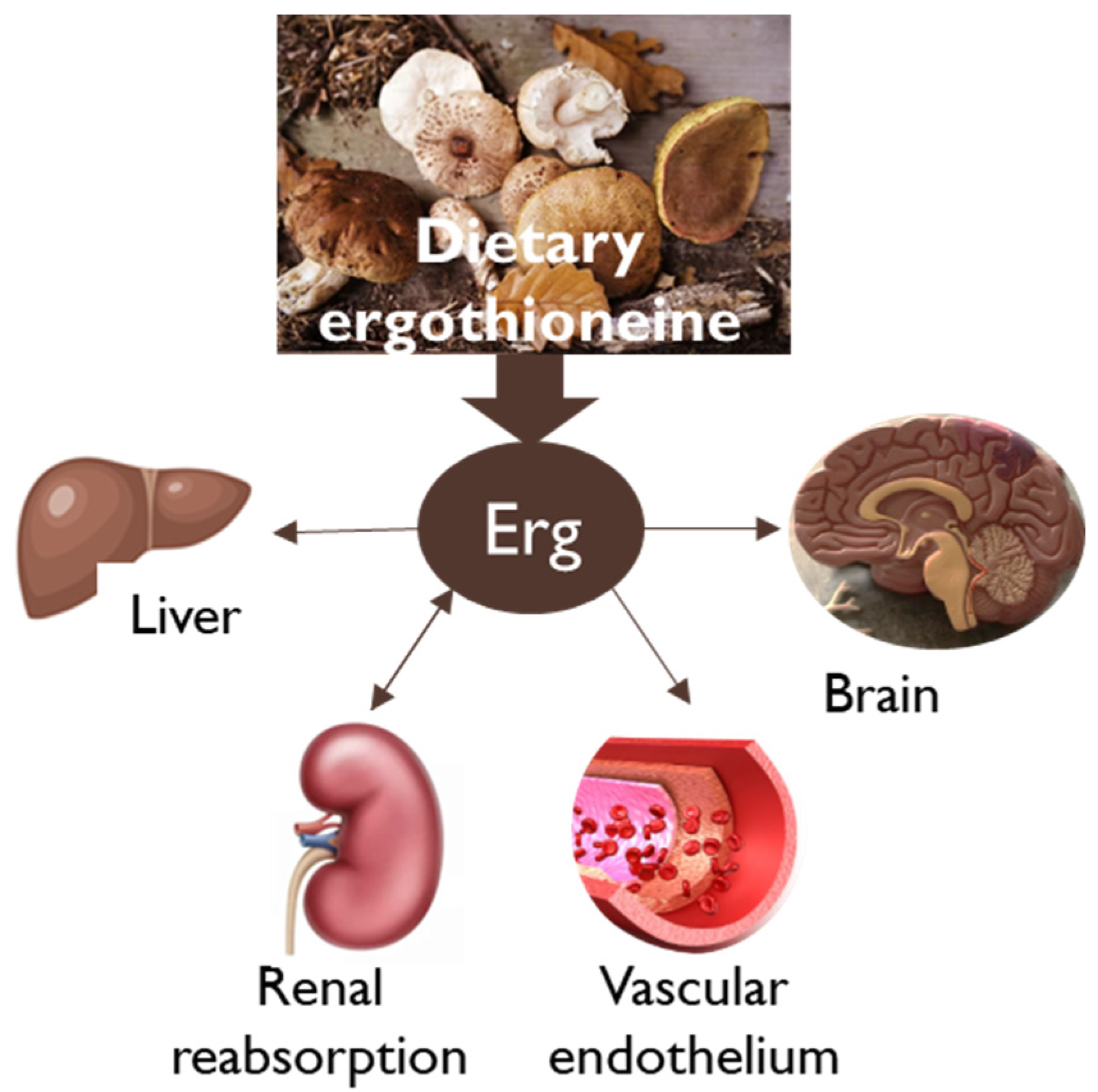
- Tian, X.; Thorne, J.L.; Moore, J.B. Ergothioneine: An Underrecognised Dietary Micronutrient Required for Healthy Ageing? Br. J. Nutr. 2023, 129, 104–114. [Google Scholar] [CrossRef]
- Turck, D.; Bresson, J.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.I.; Mangelsdorf, I.; McArdle, H.J.; Naska, A.; et al. Safety of Synthetic L-ergothioneine (Ergoneine®) as a Novel Food Pursuant to Regulation (EC) No 258/97. EFSA J. 2016, 14, e04629. [Google Scholar] [CrossRef]
- Turck, D.; Bresson, J.L.; Burlingame, B.; Dean, T.; Fairweather-Tait, S.; Heinonen, M.; Hirsch-Ernst, K.I.; Mangelsdorf, I.; McArdle, H.J.; Naska, A.; et al. Statement on the Safety of Synthetic L-Ergothioneine as a Novel Food—Supplementary Dietary Exposure and Safety Assessment for Infants and Young Children, Pregnant and Breastfeeding Women. EFSA J. 2017, 15, e05060. [Google Scholar] [CrossRef]
- Halliwell, B.; Cheah, I.K.; Tang, R.M.Y. Ergothioneine—A Diet-Derived Antioxidant with Therapeutic Potential. FEBS Lett. 2018, 592, 3357–3366. [Google Scholar] [CrossRef]
- Fu, T.T.; Shen, L. Ergothioneine as a Natural Antioxidant Against Oxidative Stress-Related Diseases. Front. Pharmacol. 2022, 13, 850813. [Google Scholar] [CrossRef] [PubMed]
- Kalaras, M.D.; Richie, J.P.; Calcagnotto, A.; Beelman, R.B. Mushrooms: A Rich Source of the Antioxidants Ergothioneine and Glutathione. Food Chem. 2017, 233, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Gründemann, D.; Harlfinger, S.; Golz, S.; Geerts, A.; Lazar, A.; Berkels, R.; Jung, N.; Rubbert, A.; Schömig, E. Discovery of the Ergothioneine Transporter. Proc. Natl. Acad. Sci. USA 2005, 102, 5256–5261. [Google Scholar] [CrossRef]
- Mittal, R.; Aranke, M.; Debs, L.H.; Nguyen, D.; Patel, A.P.; Grati, M.; Mittal, J.; Yan, D.; Chapagain, P.; Eshraghi, A.A.; et al. Indispensable Role of Ion Channels and Transporters in the Auditory System. J. Cell. Physiol. 2017, 232, 743–758. [Google Scholar] [CrossRef] [PubMed]
- Katsube, M.; Watanabe, H.; Suzuki, K.; Ishimoto, T.; Tatebayashi, Y.; Kato, Y.; Murayama, N. Food-Derived Antioxidant Ergothioneine Improves Sleep Difficulties in Humans. J. Funct. Foods 2022, 95, 105165. [Google Scholar] [CrossRef]
- Pang, L.; Wang, T.; Liao, Q.; Cheng, Y.; Wang, D.; Li, J.; Fu, C.; Zhang, C.; Zhang, J. Protective Role of Ergothioneine Isolated from Pleurotus Ostreatus against Dextran Sulfate Sodium-Induced Ulcerative Colitis in Rat Model. J. Food Sci. 2022, 87, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Törős, G.; El-Ramady, H.; Prokisch, J.; Velasco, F.; Llanaj, X.; Nguyen, D.H.H.; Peles, F. Modulation of the Gut Microbiota with Prebiotics and Antimicrobial Agents from Pleurotus Ostreatus Mushroom. Foods 2023, 12, 2010. [Google Scholar] [CrossRef] [PubMed]
- Viceconte, F.R.; Diaz, M.L.; Soresi, D.S.; Lencinas, I.B.; Carrera, A.; Prat, M.I.; Gurovic, M.S.V. Ganoderma Sessile Is a Fast Polysaccharide Producer among Ganoderma Species. Mycologia 2021, 113, 513–524. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Yu, L.; Zhao, J.; Zhang, H.; Chen, W.; Zhai, Q.; Tian, F. Role of Dietary Edible Mushrooms in the Modulation of Gut Microbiota. J. Funct. Foods 2021, 83, 104538. [Google Scholar] [CrossRef]
- Yadav, D.; Negi, P.S. Role of Mushroom Polysaccharides in Improving Gut Health and Associated Diseases. In Microbiome, Immunity, Digestive Health and Nutrition: Epidemiology, Pathophysiology, Prevention and Treatment; Bagchi, D., Downs, B.W., Eds.; Academic Press: Cambridge, MA, USA, 2022; pp. 431–448. ISBN 9780128222386. [Google Scholar]
- Ma, T.; Shen, X.; Shi, X.; Sakandar, H.A.; Quan, K.; Li, Y.; Jin, H.; Kwok, L.Y.; Zhang, H.; Sun, Z. Targeting Gut Microbiota and Metabolism as the Major Probiotic Mechanism—An Evidence-Based Review. Trends Food Sci. Technol. 2023, 138, 178–198. [Google Scholar] [CrossRef]
- Zhao, J.; Hu, Y.; Qian, C.; Hussain, M.; Liu, S.; Zhang, A.; He, R.; Sun, P. The Interaction between Mushroom Polysaccharides and Gut Microbiota and Their Effect on Human Health: A Review. Biology 2023, 12, 122. [Google Scholar] [CrossRef]
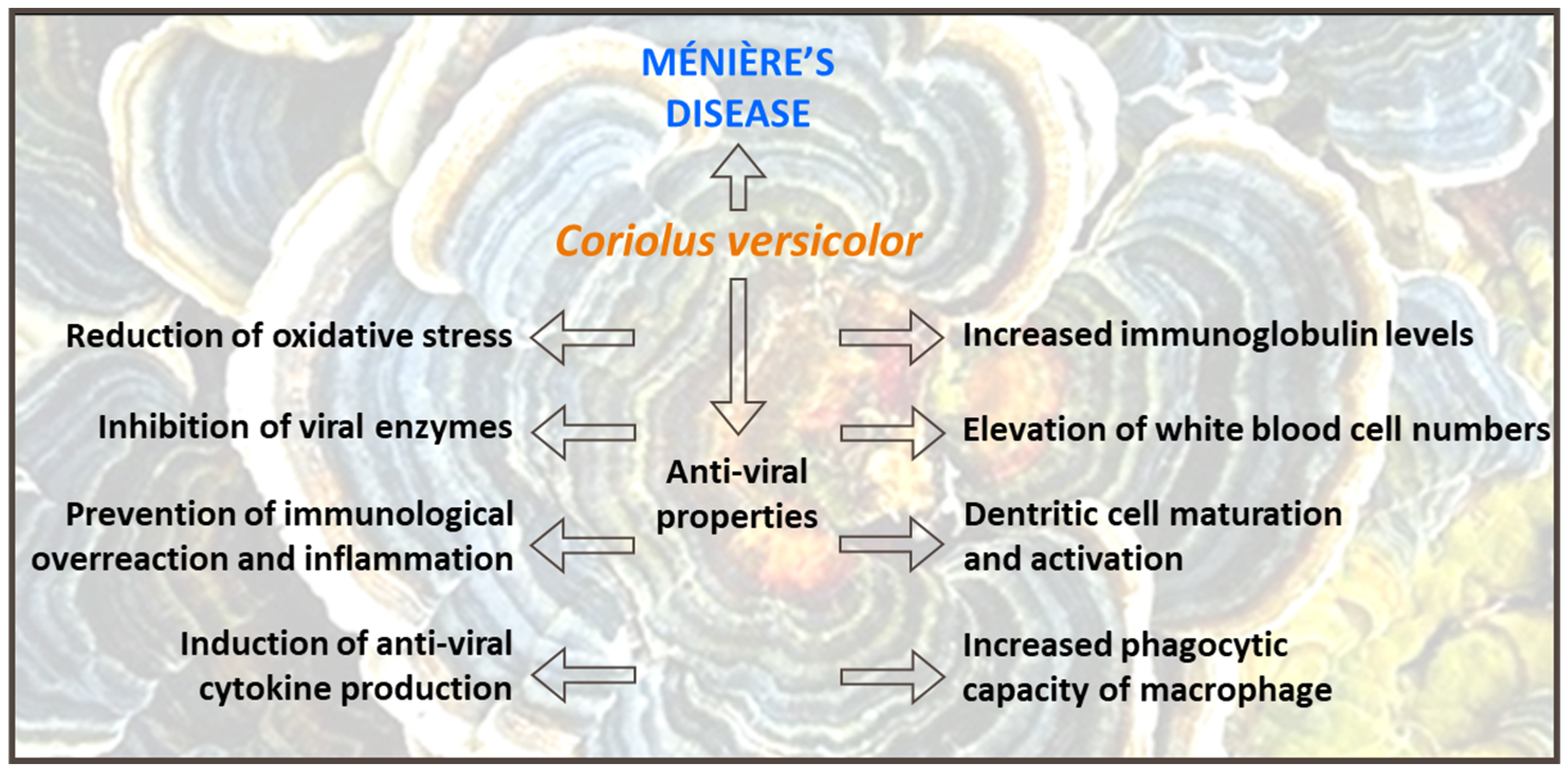
- Trovato-Salinaro, A.; Siracusa, R.; Di Paola, R.; Scuto, M.; Fronte, V.; Koverech, G.; Luca, M.; Serra, A.; Toscano, M.A.; Petralia, A.; et al. Redox Modulation of Cellular Stress Response and Lipoxin A4 Expression by Coriolus Versicolor in Rat Brain: Relevance to Alzheimer’s Disease Pathogenesis. Neurotoxicology 2016, 53, 350–358. [Google Scholar] [CrossRef]
- Sergio, M.; Gabriella, L.; Mario, T.; Francesco, R.; Marialaura, O.; Maria, S.; Angela, T.S.; Antonio, A.; Daniela, A.C.; Maria, L.; et al. Antioxidants, Hormetic Nutrition, and Autism. Curr. Neuropharmacol. 2023, 21. [Google Scholar] [CrossRef]
- Kumar, K.; Mehra, R.; Guiné, R.P.F.; Lima, M.J.; Kumar, N.; Kaushik, R.; Ahmed, N.; Yadav, A.N.; Kumar, H. Edible Mushrooms: A Comprehensive Review on Bioactive Compounds with Health Benefits and Processing Aspects. Foods 2021, 10, 2996. [Google Scholar] [CrossRef]
- Benson, K.F.; Stamets, P.; Davis, R.; Nally, R.; Taylor, A.; Slater, S.; Jensen, G.S. The Mycelium of the Trametes versicolor (Turkey Tail) Mushroom and Its Fermented Substrate Each Show Potent and Complementary Immune Activating Properties in Vitro. BMC Complement. Altern. Med. 2019, 19, 342. [Google Scholar] [CrossRef]
- Kıvrak, İ.; Kıvrak, Ş.; Karababa, E. Assessment of Bioactive Compounds and Antioxidant Activity of Turkey Tail Medicinal Mushroom Trametes versicolor (Agaricomycetes). Int. J. Med. Mushrooms 2020, 22, 559–571. [Google Scholar] [CrossRef]
- Karmali, A.; Bugalho, A.; Fernandes, T. Coriolus Versicolor Supplementation in CIN-1 (LSIL) HPV Infection: Mode of Action. Clin. J. Mycol. 2007, 2, 6–10. [Google Scholar]
- Moshtaghi, O.; Sahyouni, R.; Lin, H.W.; Ghavami, Y.; Djalilian, H.R. A Historical Recount: Discovering Menière’s Disease and Its Association with Migraine Headaches. Otol. Neurotol. 2016, 37, 1199–1203. [Google Scholar] [CrossRef]
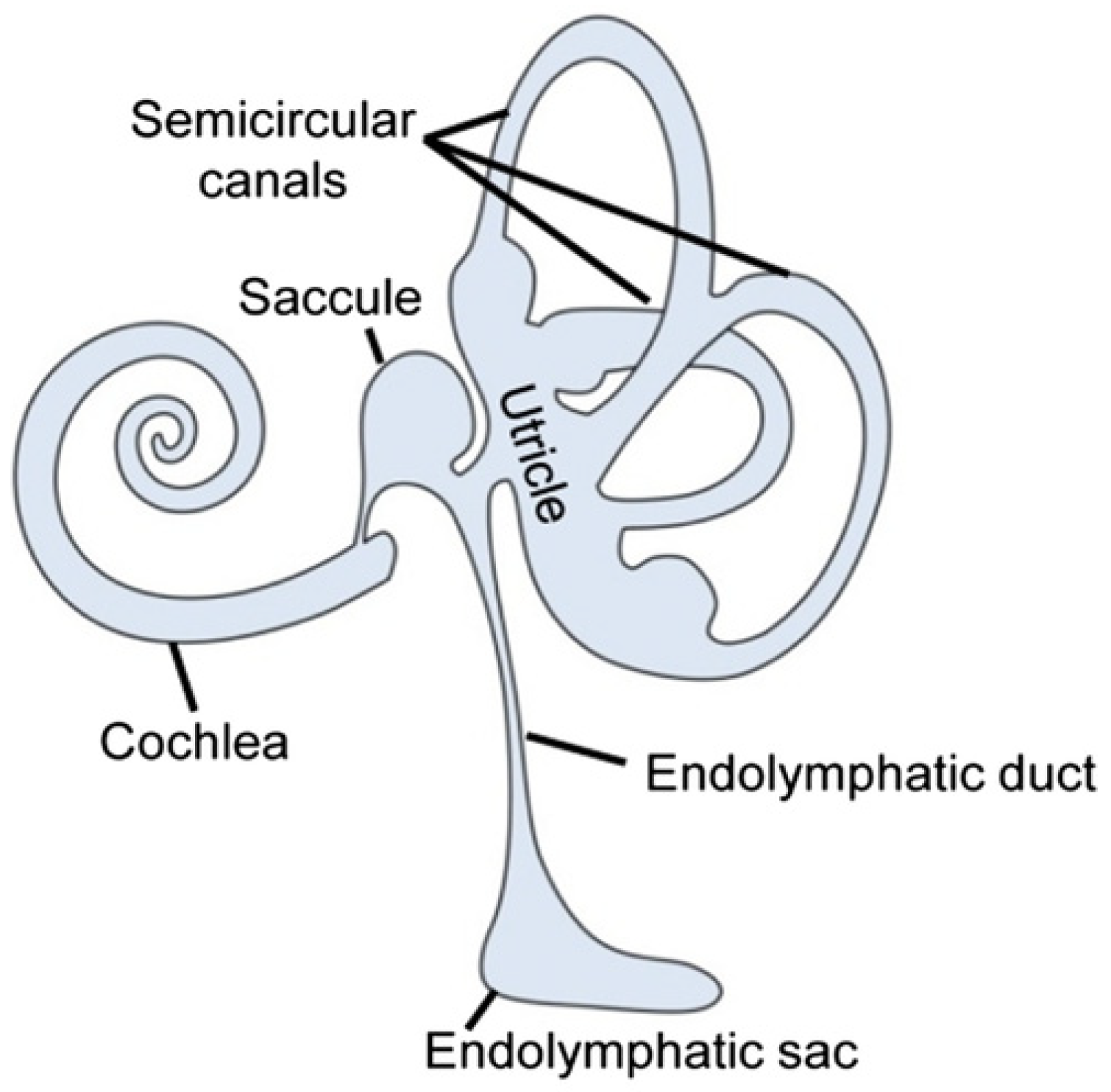
- Nakashima, T.; Pyykkö, I.; Arroll, M.A.; Casselbrant, M.L.; Foster, C.A.; Manzoor, N.F.; Megerian, C.A.; Naganawa, S.; Young, Y.H. Meniere’s Disease. Nat. Rev. Dis. Primers 2016, 2, 16028. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Q.; Pan, X.; Li, W.; Liu, W.; Jiang, W.; Huang, L.; Peng, A.; Zhang, Z. Up-Regulated Expression of Interferon-Gamma, Interleukin-6 and Tumor Necrosis Factor-Alpha in the Endolymphatic Sac of Meniere’s Disease Suggesting the Local Inflammatory Response Underlies the Mechanism of This Disease. Front. Neurol. 2022, 13, 781031. [Google Scholar] [CrossRef]
- Møller, M.N.; Kirkeby, S.; Cayé-Thomasen, P. Innate Immune Defense in the Inner Ear—Mucines Are Expressed by the Human Endolymphatic Sac. J. Anat. 2017, 230, 297–302. [Google Scholar] [CrossRef]
- Koenen, L.; Andaloro, C. Meniere Disease; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Koç, A. Benign Paroxysmal Positional Vertigo: Is It Really an Otolith Disease? J. Int. Adv. Otol. 2022, 18, 62–70. [Google Scholar] [CrossRef]
- Weinreich, H.M.; Agrawal, Y. The Link Between Allergy and Menière’s Disease. Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 227. [Google Scholar] [CrossRef]
- Pan, T.; Zhao, Y.; Ding, Y.J.; Lu, Z.Y.; Ma, F.R. The Pilot Study of Type Ⅰ Allergic Reaction in Meniere’s Disease Patients. Chin. J. Otorhinolaryngol. Head Neck Surg. 2017, 52, 89–92. [Google Scholar] [CrossRef]
- Dai, Q.; Wang, D.; Zheng, H. The Polymorphic Analysis of the Human Potassium Channel Kcne Gene Family in Meniere’s Disease. A Preliminary Study. J. Int. Adv. Otol. 2019, 15, 130–134. [Google Scholar] [CrossRef]
- Martín-Sierra, C.; Gallego-Martinez, A.; Requena, T.; Frejo, L.; Batuecas-Caletrió, A.; Lopez-Escamez, J.A. Variable Expressivity and Genetic Heterogeneity Involving DPT and SEMA3D Genes in Autosomal Dominant Familial Meniere’s Disease. Eur. J. Hum. Genet. 2016, 25, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Lopes, K.D.C.; Sartorato, E.L.; Da Silva-Costa, S.M.; De Macedo Adamov, N.S.; Ganança, F.F. Ménière’s Disease: Molecular Analysis of Aquaporins 2, 3 and Potassium Channel KCNE1 Genes in Brazilian Patients. Otol. Neurotol. 2016, 37, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Doi, K.; Sato, T.; Kuramasu, T.; Hibino, H.; Kitahara, T.; Horii, A.; Matsushiro, N.; Fuse, Y.; Kubo, T. Ménière’s Disease Is Associated with Single Nucleotide Polymorphisms in the Human Potassium Channel Genes, KCNE1 and KCNE3. ORL 2005, 67, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Brandalise, F.; Roda, E.; Ratto, D.; Goppa, L.; Gargano, M.L.; Cirlincione, F.; Priori, E.C.; Venuti, M.T.; Pastorelli, E.; Savino, E.; et al. Hericium Erinaceus in Neurodegenerative Diseases: From Bench to Bedside and Beyond, How Far from the Shoreline? J. Fungi 2023, 9, 551. [Google Scholar] [CrossRef]
- NIH. Ménière’s Disease. Available online: https://www.nidcd.nih.gov/health/menieres-disease (accessed on 20 March 2023).
- Shih, R.D.; Walsh, B.; Eskin, B.; Allegra, J.; Fiesseler, F.W.; Salo, D.; Silverman, M. Diazepam and Meclizine Are Equally Effective in the Treatment of Vertigo: An Emergency Department Randomized Double-Blind Placebo-Controlled Trial. J. Emerg. Med. 2017, 52, 23–27. [Google Scholar] [CrossRef]
- Watkins, L.E.; Sprang, K.R.; Rothbaum, B.O. Treating PTSD: A Review of Evidence-Based Psychotherapy Interventions. Front. Behav. Neurosci. 2018, 12, 400414. [Google Scholar] [CrossRef] [PubMed]
- de Cates, C.; Winters, R. Intratympanic Steroid Injection; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Russo, F.Y.; Nguyen, Y.; De Seta, D.; Bouccara, D.; Sterkers, O.; Ferrary, E.; Bernardeschi, D. Meniett Device in Meniere Disease: Randomized, Double-Blind, Placebo-Controlled Multicenter Trial. Laryngoscope 2017, 127, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; George, B.; Galbraith, K.; Harrington-Benton, N.A.; Judd, O.; Kaski, D.; Maarsingh, O.R.; MacKeith, S.; Ray, J.; Van Vugt, V.A.; et al. Positive pressure therapy for Ménière’s disease. Cochrane Database Syst. Rev. 2023, 2, CD015248. [Google Scholar] [CrossRef]
- Pullens, B.; Verschuur, H.P.; van Benthem, P.P. Surgery for Ménière’s disease. Cochrane Database Syst. Rev. 2013, 2, CD005395. [Google Scholar] [CrossRef]
- Chiarella, G.; Marcianò, G.; Viola, P.; Palleria, C.; Pisani, D.; Rania, V.; Casarella, A.; Astorina, A.; Scarpa, A.; Esposito, M.; et al. Nutraceuticals for Peripheral Vestibular Pathology: Properties, Usefulness, Future Perspectives and Medico-Legal Aspects. Nutrients 2021, 13, 3646. [Google Scholar] [CrossRef]
- Viola, P.; Pisani, D.; Scarpa, A.; Cassandro, C.; Laria, C.; Aragona, T.; Ciriolo, M.; Spadera, L.; Ralli, M.; Cavaliere, M.; et al. The Role of Endogenous Antisecretory Factor (AF) in the Treatment of Ménière’s Disease: A Two-Year Follow-up Study. Preliminary Results. Am. J. Otolaryngol. 2020, 41, 102673. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lyu, Y.; Li, Y.; Jian, H.; Wang, J.; Song, Y.; Kong, L.; Fan, Z.; Wang, H.; Zhang, D. Triple Semicircular Canal Plugging versus Labyrinthectomy for Meniere Disease: A Retrospective Study. Laryngoscope 2023, 133, 3178–3184. [Google Scholar] [CrossRef] [PubMed]
- Eraslan Boz, H.; Kırkım, G.; Koçoğlu, K.; Çakır Çetin, A.; Akkoyun, M.; Güneri, E.A.; Akdal, G. Cognitive Function in Meniere’s Disease. Psychol. Health Med. 2023, 28, 1076–1086. [Google Scholar] [CrossRef] [PubMed]
- Sarna, B.; Abouzari, M.; Lin, H.W.; Djalilian, H.R. A Hypothetical Proposal for Association between Migraine and Meniere’s Disease. Med. Hypotheses 2020, 134, 109430. [Google Scholar] [CrossRef]
- Zhong, J.; Li, X.; Xu, J.; Chen, W.; Gao, J.; Lu, X.; Liang, S.; Guo, Z.; Lu, M.; Li, Y.; et al. Analysis of Cognitive Function and Its Related Factors after Treatment in Meniere’s Disease. Front. Neurosci. 2023, 17, 1137734. [Google Scholar] [CrossRef]
- Chari, D.A.; Liu, Y.H.; Chung, J.J.; Rauch, S.D. Subjective Cognitive Symptoms and Dizziness Handicap Inventory (DHI) Performance in Patients With Vestibular Migraine and Menière’s Disease. Otol. Neurotol. 2021, 42, 883–889. [Google Scholar] [CrossRef]
- Xie, D.; Welgampola, M.S.; Miller, L.A.; Young, A.S.; D’Souza, M.; Breen, N.; Rosengren, S.M. Subjective Cognitive Dysfunction in Patients with Dizziness and Vertigo. Audiol. Neurotol. 2022, 27, 122–132. [Google Scholar] [CrossRef]
- Dornhoffer, J.R.; Liu, Y.F.; Zhao, E.E.; Rizk, H.G. Does Cognitive Dysfunction Correlate with Dizziness Severity in Meniére’s Disease Patients. Otol. Neurotol. 2021, 42, E323–E331. [Google Scholar] [CrossRef]
- Cornelius, C.; Perrotta, R.; Graziano, A.; Calabrese, E.J.; Calabrese, V. Stress Responses, Vitagenes and Hormesis as Critical Determinants in Aging and Longevity: Mitochondria as a “Chi”. Immun. Ageing 2013, 10, 15. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Jia, X.; Wang, Z.; Huang, F.; Su, C.; Du, W.; Jiang, H.; Wang, H.; Wang, J.; Wang, F.; Su, W.; et al. A Comparison of the Mini-Mental State Examination (MMSE) with the Montreal Cognitive Assessment (MoCA) for Mild Cognitive Impairment Screening in Chinese Middle-Aged and Older Population: A Cross-Sectional Study. BMC Psychiatry 2021, 21, 485. [Google Scholar] [CrossRef]
- Lee, I.H.; Yu, H.; Ha, S.S.; Son, G.M.; Park, K.J.; Lee, J.J.; Kim, D.K. Association between Late-Onset Ménière’s Disease and the Risk of Incident All-Cause Dementia. J. Pers. Med. 2021, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Halmágyi, G.M.; Akdal, G.; Welgampola, M.S.; Wang, C. Neurological Update: Neuro-Otology 2023. J. Neurol. 2023, 270, 6170–6192. [Google Scholar] [CrossRef] [PubMed]
- Kabade, V.; Hooda, R.; Raj, C.; Awan, Z.; Young, A.S.; Welgampola, M.S.; Prasad, M. Machine Learning Techniques for Differential Diagnosis of Vertigo and Dizziness: A Review. Sensors 2021, 21, 7565. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.A.; Vivar, G.; Navab, N.; Möhwald, K.; Maier, A.; Hadzhikolev, H.; Brandt, T.; Grill, E.; Dieterich, M.; Jahn, K.; et al. Modern Machine-Learning Can Support Diagnostic Differentiation of Central and Peripheral Acute Vestibular Disorders. J. Neurol. 2020, 267, 143–152. [Google Scholar] [CrossRef] [PubMed]
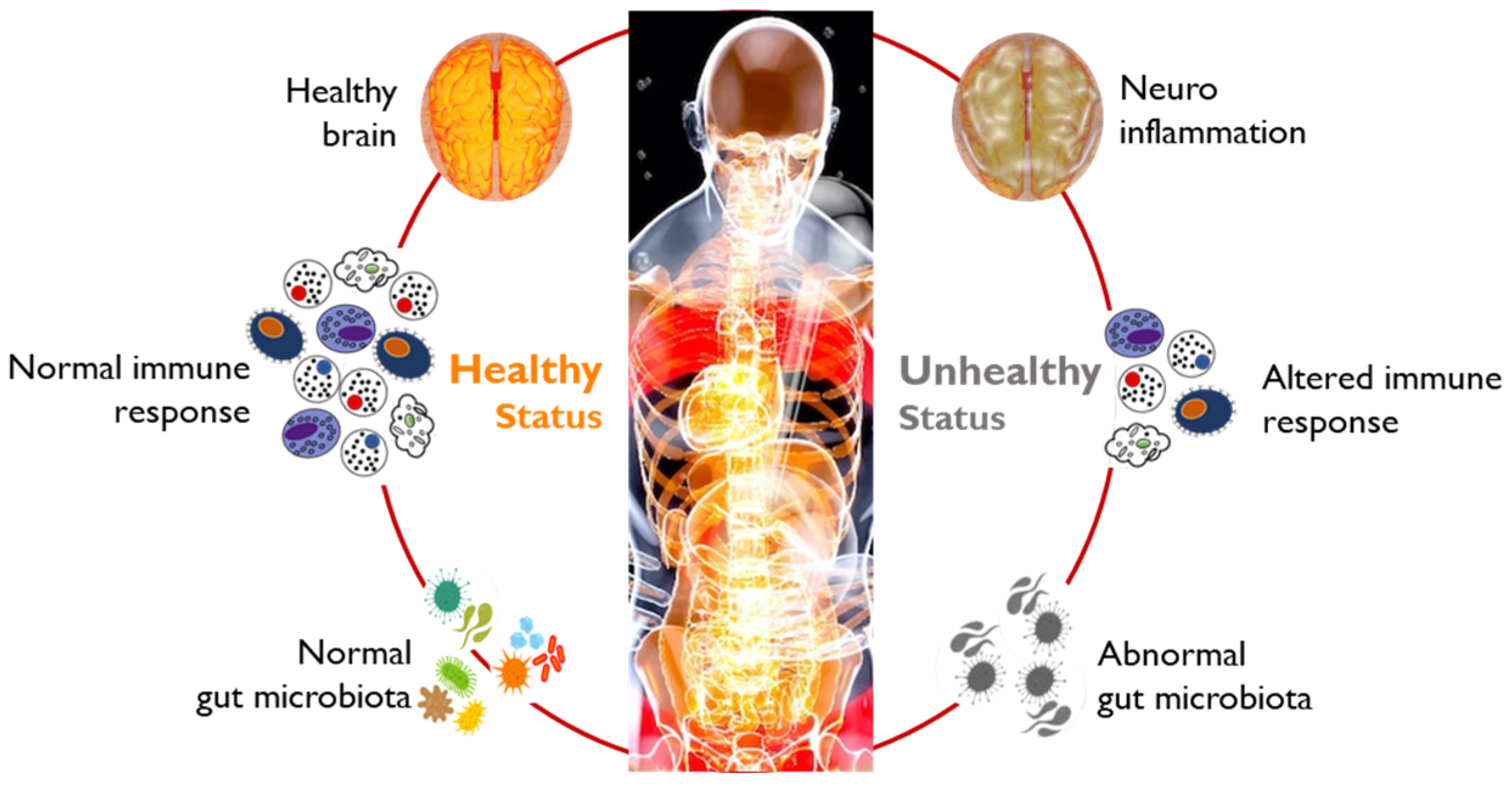
- Zhang, Y.; Chen, R.; Zhang, D.D.; Qi, S.; Liu, Y. Metabolite Interactions between Host and Microbiota during Health and Disease: Which Feeds the Other? Biomed. Pharmacother. 2023, 160, 114295. [Google Scholar] [CrossRef]
- Farooq, R.K.; Alamoudi, W.; Alhibshi, A.; Rehman, S.; Sharma, A.R.; Abdulla, F.A. Varied Composition and Underlying Mechanisms of Gut Microbiome in Neuroinflammation. Microorganisms 2022, 10, 705. [Google Scholar] [CrossRef]
- Fung, T.C.; Olson, C.A.; Hsiao, E.Y. Interactions between the Microbiota, Immune and Nervous Systems in Health and Disease. Nat. Neurosci. 2017, 20, 145–155. [Google Scholar] [CrossRef]
- Strandwitz, P. Neurotransmitter Modulation by the Gut Microbiota. Brain Res. 2018, 1693, 128–133. [Google Scholar] [CrossRef]
- Altveş, S.; Yildiz, H.K.; Vural, H.C. Interaction of the Microbiota with the Human Body in Health and Diseases. Biosci. Microbiota Food Health 2020, 39, 23–32. [Google Scholar] [CrossRef]
- Fakharian, F.; Thirugnanam, S.; Welsh, D.A.; Kim, W.K.; Rappaport, J.; Bittinger, K.; Rout, N. The Role of Gut Dysbiosis in the Loss of Intestinal Immune Cell Functions and Viral Pathogenesis. Microorganisms 2023, 11, 1849. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Wang, X.; Li, L. Human Gut Microbiome: The Second Genome of Human Body. Protein Cell 2010, 1, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Elzayat, H.; Mesto, G.; Al-Marzooq, F. Unraveling the Impact of Gut and Oral Microbiome on Gut Health in Inflammatory Bowel Diseases. Nutrients 2023, 15, 3377. [Google Scholar] [CrossRef]
- Sittipo, P.; Choi, J.; Lee, S.; Lee, Y.K. The Function of Gut Microbiota in Immune-Related Neurological Disorders: A Review. J. Neuroinflamm. 2022, 19, 154. [Google Scholar] [CrossRef] [PubMed]
- Beane, K.E.; Redding, M.C.; Wang, X.; Pan, J.H.; Le, B.; Cicalo, C.; Jeon, S.; Kim, Y.J.; Lee, J.H.; Shin, E.C.; et al. Effects of Dietary Fibers, Micronutrients, and Phytonutrients on Gut Microbiome: A Review. Appl. Biol. Chem. 2021, 64, 36. [Google Scholar] [CrossRef]
- Carneiro, L.; Pellerin, L. Nutritional Impact on Metabolic Homeostasis and Brain Health. Front. Neurosci. 2022, 15, 767405. [Google Scholar] [CrossRef]
- Jeng, Y.; Young, Y.H. Evolution of Geriatric Meniere’s Disease during the Past Two Decades. J. Formos. Med. Assoc. 2023, 122, 65–72. [Google Scholar] [CrossRef]
- Basura, G.J.; Adams, M.E.; Monfared, A.; Schwartz, S.R.; Antonelli, P.J.; Burkard, R.; Bush, M.L.; Bykowski, J.; Colandrea, M.; Derebery, J.; et al. Clinical Practice Guideline: Ménière’s Disease. Otolaryngol. Neck Surg. 2020, 162, S1–S55. [Google Scholar] [CrossRef]
- Oberman, B.S.; Patel, V.A.; Cureoglu, S.; Isildak, H. The Aetiopathologies of Ménière’s Disease: A Contemporary Review L’eziopatogenesi Della Sindrome Di Ménière: Stato Dell’arte. Aggiorn. Acta Otorhinolaryngol. Ital. 2017, 37, 250–263. [Google Scholar] [CrossRef]
- De Luca, P.; Cassandro, C.; Ralli, M.; Gioacchini, F.M.; Turchetta, R.; Orlando, M.P.; Iaccarino, I.; Cavaliere, M.; Cassandro, E.; Scarpa, A. Dietary Restriction for The Treatment of Meniere’s Disease. Transl. Med. UniSa 2020, 22, 5–9. [Google Scholar]
- Oğuz, E.; Cebeci, A.; Geçici, C.R. The Relationship between Nutrition and Ménière’s Disease. Auris Nasus Larynx 2021, 48, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.H.; Kim, J.S.; Kim, H.J.; Choi, J.Y.; Koo, J.W.; Choi, K.D.; Park, J.Y.; Lee, S.H.; Choi, S.Y.; Oh, S.Y.; et al. Prevention of Benign Paroxysmal Positional Vertigo with Vitamin D Supplementation. Neurology 2020, 95, e1117–e1125. [Google Scholar] [CrossRef] [PubMed]
- McCullough, P.; Amend, J. Results of Daily Oral Dosing with up to 60,000 International Units (Iu) of Vitamin D3 for 2 to 6 Years in 3 Adult Males. J. Steroid Biochem. Mol. Biol. 2017, 173, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Papadimitriou, D.T. The Big Vitamin D Mistake. J. Prev. Med. Public Health 2017, 50, 278–281. [Google Scholar] [CrossRef] [PubMed]
- Hussain, K.; Murdin, L.; Schilder, A.G. Restriction of salt, caffeine and alcohol intake for the treatment of Ménière’s disease or syndrome. Cochrane Database Syst. Rev. 2018, 12, CD012173. [Google Scholar] [CrossRef] [PubMed]
- Eckhard, A.H.; Zhu, M.Y.; O’Malley, J.T.; Williams, G.H.; Loffing, J.; Rauch, S.D.; Nadol, J.B.; Liberman, M.C.; Adams, J.C. Inner Ear Pathologies Impair Sodium-Regulated Ion Transport in Meniere’s Disease. Acta Neuropathol. 2019, 137, 343–357. [Google Scholar] [CrossRef]
- Atayik, M.C.; Çakatay, U. Redox Signaling in Impaired Cascades of Wound Healing: Promising Approach. Mol. Biol. Rep. 2023, 50, 6927–6936. [Google Scholar] [CrossRef]
- Poon, H.F.; Calabrese, V.; Scapagnini, G.; Butterfield, D.A. Free Radicals: Key to Brain Aging and Heme Oxygenase as a Cellular Response to Oxidative Stress. J. Gerontol. Ser. A 2004, 59, M478–M493. [Google Scholar] [CrossRef]
- Liuzzi, G.M.; Petraglia, T.; Latronico, T.; Crescenzi, A.; Rossano, R. Antioxidant Compounds from Edible Mushrooms as Potential Candidates for Treating Age-Related Neurodegenerative Diseases. Nutrients 2023, 15, 1913. [Google Scholar] [CrossRef]
- Fekete, M.; Szarvas, Z.; Fazekas-Pongor, V.; Feher, A.; Csipo, T.; Forrai, J.; Dosa, N.; Peterfi, A.; Lehoczki, A.; Tarantini, S.; et al. Nutrition Strategies Promoting Healthy Aging: From Improvement of Cardiovascular and Brain Health to Prevention of Age-Associated Diseases. Nutrients 2022, 15, 47. [Google Scholar] [CrossRef]
- Rai, S.N.; Mishra, D.; Singh, P.; Vamanu, E.; Singh, M.P. Therapeutic Applications of Mushrooms and Their Biomolecules along with a Glimpse of in Silico Approach in Neurodegenerative Diseases. Biomed. Pharmacother. 2021, 137, 111377. [Google Scholar] [CrossRef]
- Jiang, X.; Li, S.; Feng, X.; Li, L.; Hao, J.; Wang, D.; Wang, Q. Mushroom Polysaccharides as Potential Candidates for Alleviating Neurodegenerative Diseases. Nutrients 2022, 14, 4833. [Google Scholar] [CrossRef]
- Al-Qudah, M.A.; Al-Dwairi, A. Mechanisms and Regulation of Neurotrophin Synthesis and Secretion. Neurosci. J. 2016, 21, 306–313. [Google Scholar] [CrossRef]
- Iskusnykh, I.Y.; Zakharova, A.A.; Pathak, D. Glutathione in Brain Disorders and Aging. Molecules 2022, 27, 324. [Google Scholar] [CrossRef]
- Calabrese, V.; Cornelius, C.; Dinkova-Kostova, A.T.; Calabrese, E.J. Vitagenes, Cellular Stress Response, and Acetylcarnitine: Relevance to Hormesis. BioFactors 2009, 35, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, V.; Ontario, M. Mushroom Nutrition In Neurodegenerative Diseases. Clin. J. Mycol. 2022, 6. [Google Scholar] [CrossRef]
- Trovato Salinaro, A.; Pennisi, M.; Di Paola, R.; Scuto, M.; Crupi, R.; Cambria, M.T.; Ontario, M.L.; Tomasello, M.; Uva, M.; Maiolino, L.; et al. Neuroinflammation and Neurohormesis in the Pathogenesis of Alzheimer’s Disease and Alzheimer-Linked Pathologies: Modulation by Nutritional Mushrooms. Immun. Ageing 2018, 15, 8. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, S.; Thakur, R.; Shankar, J. Role of Heat-Shock Proteins in Cellular Function and in the Biology of Fungi. Biotechnol. Res. Int. 2015, 2015, 132635. [Google Scholar] [CrossRef]
- Zhao, X.; Yin, K.; Feng, R.; Miao, R.; Lin, J.; Cao, L.; Ni, Y.; Li, W.; Zhang, Q. Genome-Wide Identification and Analysis of the Heat-Shock Protein Gene in L. Edodes and Expression Pattern Analysis under Heat Shock. Curr. Issues Mol. Biol. 2023, 45, 614–627. [Google Scholar] [CrossRef]
- Trovato, A.; Siracusa, R.; Di Paola, R.; Scuto, M.; Ontario, M.L.; Bua, O.; Di Mauro, P.; Toscano, M.A.; Petralia, C.C.T.; Maiolino, L.; et al. Redox Modulation of Cellular Stress Response and Lipoxin A4 Expression by Hericium Erinaceus in Rat Brain: Relevance to Alzheimer’s Disease Pathogenesis. Immun. Ageing 2016, 13, 23. [Google Scholar] [CrossRef]
- Das, U.N. Lipoxins as Biomarkers of Lupus and Other Inflammatory Conditions. Lipids Health Dis. 2011, 10, 76. [Google Scholar] [CrossRef]
- Cordaro, M.; Modafferi, S.; D’Amico, R.; Fusco, R.; Genovese, T.; Peritore, A.F.; Gugliandolo, E.; Crupi, R.; Interdonato, L.; Di Paola, D.; et al. Natural Compounds Such as Hericium Erinaceus and Coriolus Versicolor Modulate Neuroinflammation, Oxidative Stress and Lipoxin A4 Expression in Rotenone-Induced Parkinson’s Disease in Mice. Biomedicines 2022, 10, 2505. [Google Scholar] [CrossRef]
- Ólafsdóttir, H.F.; Bush, D.; Barry, C. The Role of Hippocampal Replay in Memory and Planning. Curr. Biol. 2018, 28, R37–R50. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, D.W.; White, C.M.; Rees, C.L.; Komendantov, A.O.; Hamilton, D.J.; Ascoli, G.A. Hippocampome.Org: A Knowledge Base of Neuron Types in the Rodent Hippocampus. Elife 2015, 4, e09960. [Google Scholar] [CrossRef] [PubMed]
- Ferreiro, E.; Fernandes, T. Targeting Neurogenesis with Mushroom Nutrition: A Mini Review. Clin. J. Mycol. 2022, 6. [Google Scholar] [CrossRef]
- Audesse, A.J.; Webb, A.E. Mechanisms of Enhanced Quiescence in Neural Stem Cell Aging. Mech. Ageing Dev. 2020, 191, 111323. [Google Scholar] [CrossRef]
- Ruan, J.; Hu, X.; Liu, Y.; Han, Z.; Ruan, Q. Vulnerability to Chronic Stress and the Phenotypic Heterogeneity of Presbycusis with Subjective Tinnitus. Front. Neurosci. 2022, 16, 1046095. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.J.; Kim, J.; Kim, S.H. The Change of Hippocampal Volume and Its Relevance with Inner Ear Function in Meniere’s Disease Patients. Auris Nasus Larynx 2016, 43, 620–625. [Google Scholar] [CrossRef]
- Barros, A.B.; Ferrão, J.; Fernandes, T. A Safety Assessment of Coriolus Versicolor Biomass as a Food Supplement. Food Nutr. Res. 2016, 60, 29953. [Google Scholar] [CrossRef]
- Piatti, V.C.; Ewe, L.A.; Leutgeb, J.K. Neurogenesis in the Dentate Gyrus: Carrying the Message or Dictating the Tone. Front. Neurosci. 2013, 7, 45461. [Google Scholar] [CrossRef]
- Uffelman, C.N.; Chan, N.I.; Davis, E.M.; Wang, Y.; McGowan, B.S.; Campbell, W.W. An Assessment of Mushroom Consumption on Cardiometabolic Disease Risk Factors and Morbidities in Humans: A Systematic Review. Nutrients 2023, 15, 1079. [Google Scholar] [CrossRef]
- He, F.; Ru, X.; Wen, T. NRF2, a Transcription Factor for Stress Response and Beyond. Int. J. Mol. Sci. 2020, 21, 4777. [Google Scholar] [CrossRef]
- Özdemir, D.; Mehel, D.M.; Küçüköner, Ö.; Ağrı, İ.; Yemiş, T.; Akgül, G.; Özgür, A. Vestibular Evoked Myogenic Potentials in Patients With Low Vitamin B12 Levels. Ear Nose Throat J. 2021, 100, NP231–NP235. [Google Scholar] [CrossRef] [PubMed]
- Jorfi, M.; Maaser-Hecker, A.; Tanzi, R.E. The Neuroimmune Axis of Alzheimer’s Disease. Genome Med. 2023, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Kishimoto-Urata, M.; Urata, S.; Fujimoto, C.; Yamasoba, T. Role of Oxidative Stress and Antioxidants in Acquired Inner Ear Disorders. Antioxidants 2022, 11, 1469. [Google Scholar] [CrossRef]
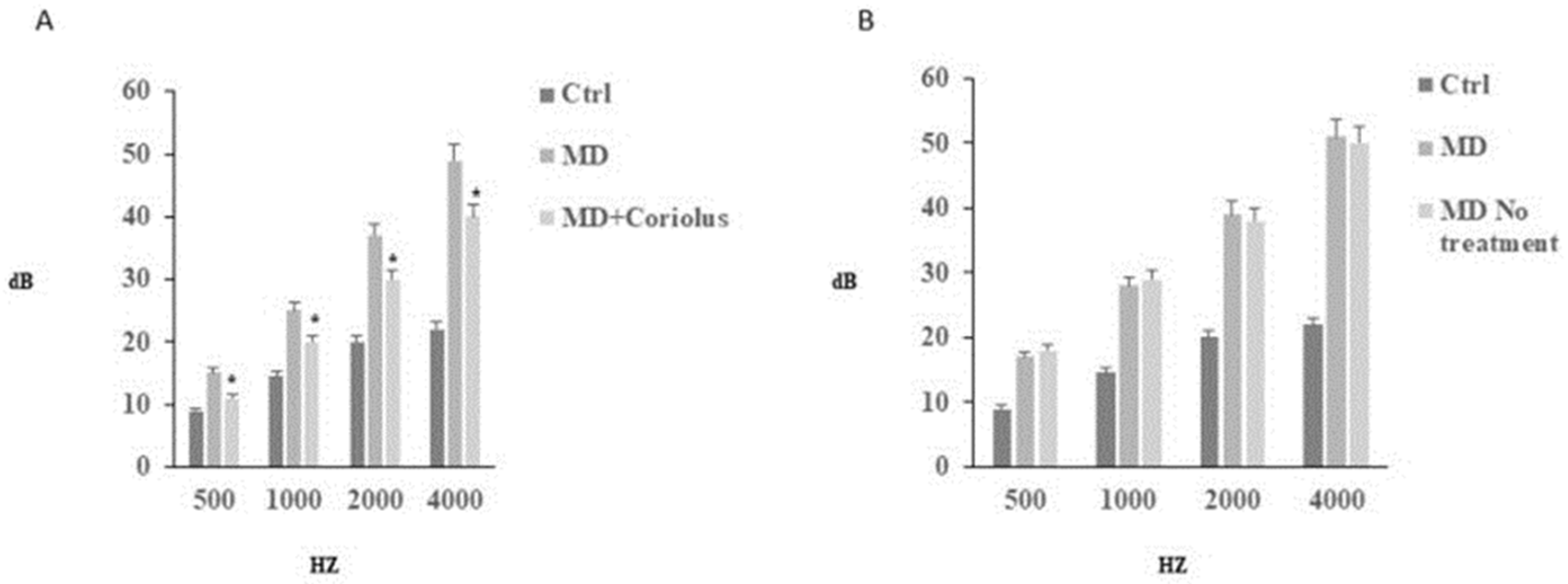
- Scuto, M.; Di Mauro, P.; Ontario, M.L.; Amato, C.; Modafferi, S.; Ciavardelli, D.; Salinaro, A.T.; Maiolino, L.; Calabrese, V. Nutritional Mushroom Treatment in Meniere’s Disease with Coriolus Versicolor: A Rationale for Therapeutic Intervention in Neuroinflammation and Antineurodegeneration. Int. J. Mol. Sci. 2019, 21, 284. [Google Scholar] [CrossRef]
- Di Paola, R.; Siracusa, R.; Fusco, R.; Ontario, M.; Cammilleri, G.; Pantano, L.; Scuto, M.; Tomasello, M.; Spano, S.; Salinaro, A.T.; et al. Redox Modulation of Meniere Disease by Coriolus Versicolor Treatment, a Nutritional Mushroom Approach with Neuroprotective Potential. Curr. Neuropharmacol. 2023; in press. CN-2023-0107.R2-MS. [Google Scholar]
- Owen, J.B.; Allan Butterfiel, D. Measurement of Oxidized/Reduced Glutathione Ratio. Methods Mol. Biol. 2010, 648, 269–277. [Google Scholar]
- Habtemariam, S. Trametes versicolor (Synn. Coriolus versicolor) Polysaccharides in Cancer Therapy: Targets and Efficacy. Biomedicines 2020, 8, 135. [Google Scholar] [CrossRef] [PubMed]
- Saidia, A.R.; Ruel, J.; Bahloul, A.; Chaix, B.; Venail, F.; Wang, J. Current Advances in Gene Therapies of Genetic Auditory Neuropathy Spectrum Disorder. J. Clin. Med. 2023, 12, 738. [Google Scholar] [CrossRef]
- Shearer, A.E.; Hansen, M.R. Auditory Synaptopathy, Auditory Neuropathy, and Cochlear Implantation. Laryngoscope Investig. Otolaryngol. 2019, 4, 429–440. [Google Scholar] [CrossRef]
- Moser, T.; Starr, A. Auditory Neuropathy—Neural and Synaptic Mechanisms. Nat. Rev. Neurol. 2016, 12, 135–149. [Google Scholar] [CrossRef]
- Cali, E.; Dominik, N.; Manole, A.; Houlden, H. Riboflavin Transporter Deficiency. In GeneReviews; Adam, M.P., Feldman, J., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2021. [Google Scholar]
- De Siati, R.D.; Rosenzweig, F.; Gersdorff, G.; Gregoire, A.; Rombaux, P.; Deggouj, N. Auditory Neuropathy Spectrum Disorders: From Diagnosis to Treatment: Literature Review and Case Reports. J. Clin. Med. 2020, 9, 1074. [Google Scholar] [CrossRef] [PubMed]
- Alberio, T.; Brughera, M.; Lualdi, M. Current Insights on Neurodegeneration by the Italian Proteomics Community. Biomedicines 2022, 10, 2297. [Google Scholar] [CrossRef] [PubMed]
- Reddy, D.S.; Abeygunaratne, H.N. Experimental and Clinical Biomarkers for Progressive Evaluation of Neuropathology and Therapeutic Interventions for Acute and Chronic Neurological Disorders. Int. J. Mol. Sci. 2022, 23, 11734. [Google Scholar] [CrossRef] [PubMed]
| Edible Mushrooms | Bioactive Compounds | Health Benefits |
|---|---|---|
| Agaricus bisporus Pleurotus ostreatus Coriolus versicolor Lentinula edodes Flammulina velutipes Ganoderma lucidum Cordyceps sinensis Auricularia auricular Pleurotus sajor-caju Hericium erinaceus Grifola frondosa | Polyphenols Dietary fibres Lectins Terpenoids Antioxidants Flavonoids Peptidoglycans B-glucan Phytosterois Funcional proteins | Anti-diabetic Anti-inflamatory Anti-carcinogenic Anti-microbial Anti-oxidative Anti-proliferative Cholesterol-lowering Anti-viral Immuno-modulatory Osteoporosis Pre-biotic Anti-hypertensive Obesity Anti-cataractogenic Anti-viral Anti-ageing Gastrointestinal health |
| In the Absence of Proteolytic Enzymes | In the Presence of | ||
|---|---|---|---|
| Pepsin | Trypsin | ||
| Cytochrome P-450 | 0.51 nmoles | 0.49 nmoles | 0.52 nmoles |
| Cytochrome P-450 reductase | 11.9 mU | 9.52 mU | 11.1 mU |
| Glucoamylase/Beta-glucanase activity | 6.9 U | ND | ND |
| Glucose 2-oxidase activity | 49.5 mU | ND | ND |
| Laccase activity | 521.5 mU | 522.6 mU | ND |
| Peroxidase activity | 67.2 mU | 60.4 mU | 52.6 mU |
| Protease activity | 5.9 U | 5.0 U | 5.7 U |
| Protein content | 17.3 mg | 15.7 mg | 16.6 mg |
| Protein-bound polysaccharide | 91.5 mg | 80.5 mg | 78.1 mg |
| Reducing sugars | 14.8 mg | 14.5 mg | 261 mg * |
| Secondary metabolites (Thrombin inhibitors) | 59% | 54.20% | 52% |
| Superoxide dismutase (SOD) activity | 77.1 mU | 61.2 U | 68.5 U |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bell, V.; Fernandes, T.H. Mushrooms as Functional Foods for Ménière’s Disease. Appl. Sci. 2023, 13, 12348. https://doi.org/10.3390/app132212348
Bell V, Fernandes TH. Mushrooms as Functional Foods for Ménière’s Disease. Applied Sciences. 2023; 13(22):12348. https://doi.org/10.3390/app132212348
Chicago/Turabian StyleBell, Victoria, and Tito Horácio Fernandes. 2023. "Mushrooms as Functional Foods for Ménière’s Disease" Applied Sciences 13, no. 22: 12348. https://doi.org/10.3390/app132212348
APA StyleBell, V., & Fernandes, T. H. (2023). Mushrooms as Functional Foods for Ménière’s Disease. Applied Sciences, 13(22), 12348. https://doi.org/10.3390/app132212348






