Orthodontic Relapse after Fixed or Removable Retention Devices: A Systematic Review
Abstract
:1. Introduction
1.1. Rationale
- Active removable: plates with added springs, grids, elastic hooks, spring aligners, thermoformed with set-up, and digitally customised elastomers.
- Passive fixed: from classic systems (lingual arches, Maryland bridges, etc.) to all types of bonded retainers (Figure 2).
- Fixed active: cemented grids in the upper jaw and lingual arches with active insertion.
1.2. Objectives
2. Materials and Methods
2.1. Eligibility Criteria
- Study design: Randomized Clinical Trials (RCT), case series with more than 5 case reports (CS), clinical trials (CT), retrospective studies (RS), prospective studies (PS), and observational study (O).
- Human participants in permanent dentition of any age.
- Mobile or fixed retainer.
- English language.
- Only full text is available.
- Study design: reviews, letters, comments, and case series with less than 5 case reports; case reports.
- In vivo and in vitro studies;
- Animal models or dry skulls.
- Interceptive treatments or palatal expansion.
2.2. Information Sources and Search Strategy
2.3. Selection and Data Collection Process
2.4. Quality Assessment
3. Results
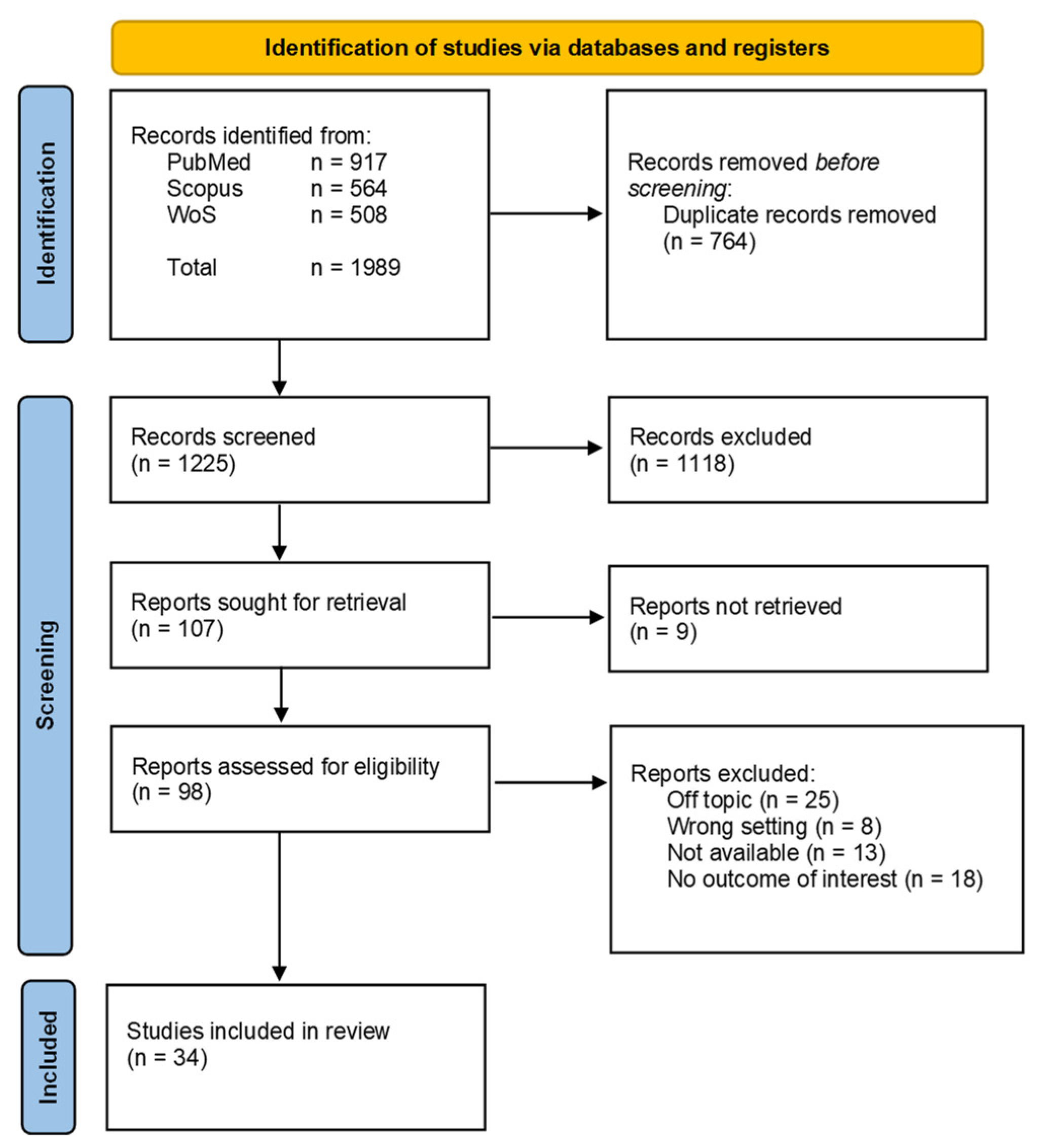
3.1. Study Selection
3.2. Study Characteristics
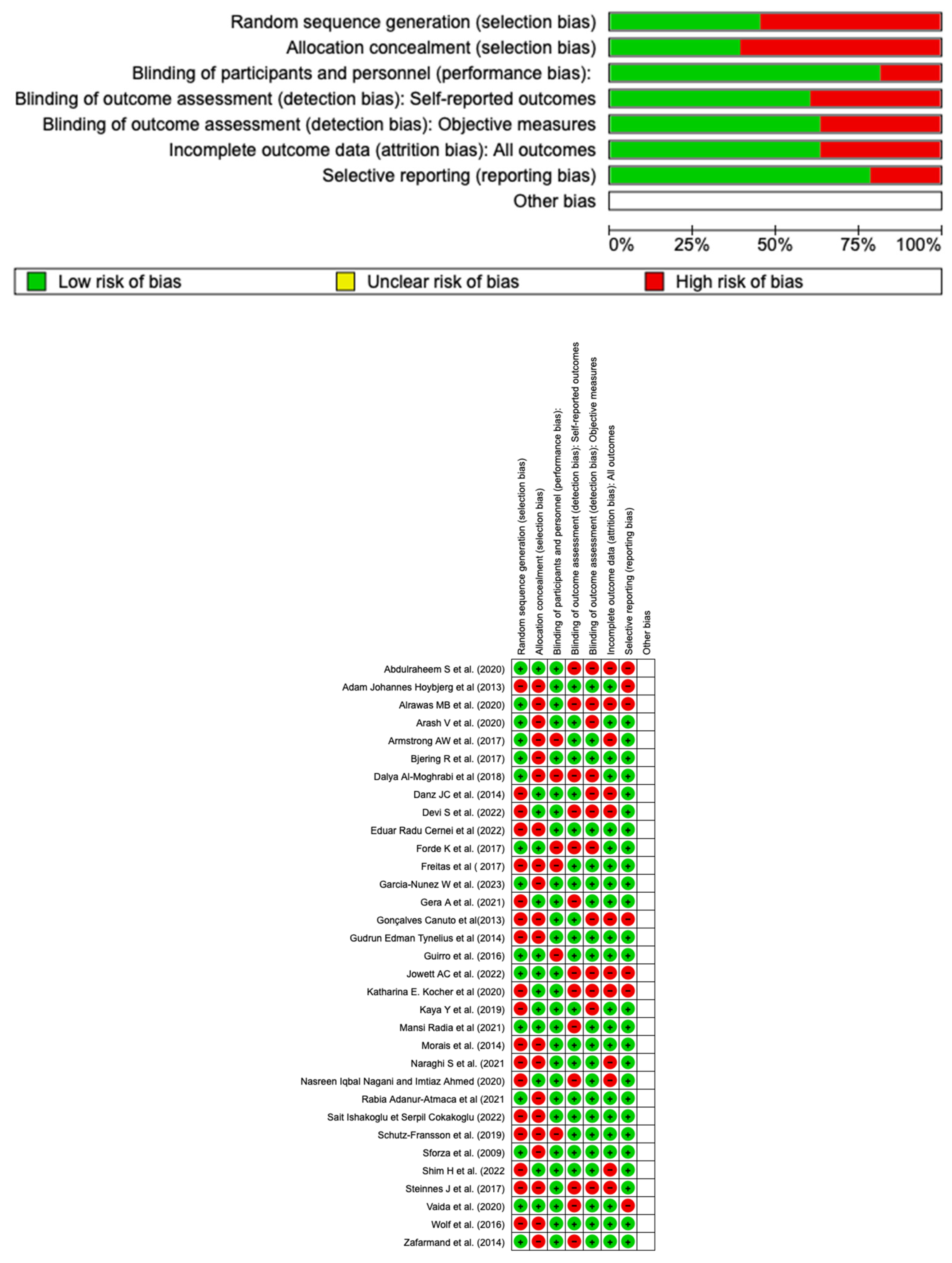
3.3. Quality Assessment and Risk of Bias
4. Discussion
4.1. Bonded Retainers Compared
4.2. Removable Retention Devices Compared
4.3. Bonded Retainers versus Removable Retention Devices
- Broad coverage of studies: The discussion provides a wide range of studies comparing different types of retainers, including bonded and removable retention devices, allowing readers to gain an overview of the current literature on this topic.
- Mention various outcomes assessed in the studies, such as relapse, stability, alignment, and periodontal health. This provides a comprehensive understanding of the factors associated with orthodontic treatment maintenance.
- Comparison of different retainer types such as flexible spiral wire, ceramic interlocking retainers, CAD/CAM retainers, twisted stainless-steel wire, titanium ribbon retainers, magnetic retainers, cemented retainers, Hawley retainers, Essix retainers, etc., allowing readers to compare the strengths and weaknesses of different retainer options.
- Discussion of long-term effects: The text includes studies that evaluate the long-term effects of retention, with very wide follow-up periods providing insights into the stability of orthodontic results over time.
- Mention compliance and maintenance requirements: The text highlights the importance of patient compliance in correctly wearing removable retention devices and for the prescribed duration. It also emphasised the need for periodic checks of fixed retainers to ensure their integrity and adhesion. This information is crucial for orthodontic practitioners and patients to understand the responsibilities and maintenance required for different retainer types.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CS | Case Series |
| CT | Clinical Trials |
| LII | Little Irregularity Index |
| O | Observational Studies |
| PAR | Peer Assessment Rating Index |
| PRCT | Prospective Randomized Clinical Trials |
| PS RoB | Prospective Studies Risk-of-bias |
| RS | Retrospective Studies |
| SS | Stainless-Steel |
| VFR | Vacuum-performed retainer |
References
- Al-Moghrabi, D.; Johal, A.; O’Rourke, N.; Donos, N.; Pandis, N.; Gonzales-Marin, C.; Fleming, P.S. Effects of Fixed vs Removable Orthodontic Retainers on Stability and Periodontal Health: 4-Year Follow-up of a Randomized Controlled Trial. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 167–174.e1. [Google Scholar] [CrossRef]
- Oppenheim, A. The Crisis in Orthodontia Part I. 2. Tissue Changes during Retention. Skogsborg’s Septotomy. Int. J. Orthod. Dent. Child. 1934, 20, 639–644. [Google Scholar] [CrossRef]
- Cantore, S.; Mirgaldi, R.; Ballini, A.; Coscia, M.F.; Scacco, S.; Papa, F.; Inchingolo, F.; Dipalma, G.; De Vito, D. Cytokine Gene Polymorphisms Associate with Microbiogical Agents in Periodontal Disease: Our Experience. Int. J. Med. Sci. 2014, 11, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Melrose, C.; Millett, D.T. Toward a Perspective on Orthodontic Retention? Am. J. Orthod. Dentofac. Orthop. 1998, 113, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Nota, A.; Marchetti, E.; Padricelli, G.; Marzo, G. The 3D Tele Motion Tracking for the Orthodontic Facial Analysis. Biomed. Res. Int. 2016, 2016, 4932136. [Google Scholar] [CrossRef] [PubMed]
- Quinzi, V.; Scibetta, E.T.; Marchetti, E.; Mummolo, S.; Giannì, A.B.; Romano, M.; Beltramini, G.; Marzo, G. Analyze My Face. J. Biol. Regul. Homeost. Agents 2018, 32, 149–158. [Google Scholar] [PubMed]
- Ahrens, D.G.; Shapira, Y.; Stom, M.M.K.D. An Approach to Rotational Relapse. Am. J. Orthod. 1981, 80, 83–91. [Google Scholar] [CrossRef]
- Reitan, K. Clinical and Histologic Observations on Tooth Movement during and after Orthodontic Treatment. Am. J. Orthod. 1967, 53, 721–745. [Google Scholar] [CrossRef]
- Li, Z.; Yu, M.; Jin, S.; Wang, Y.; Luo, R.; Huo, B.; Liu, D.; He, D.; Zhou, Y.; Liu, Y. Stress Distribution and Collagen Remodeling of Periodontal Ligament During Orthodontic Tooth Movement. Front. Pharmacol. 2019, 10, 1263. [Google Scholar] [CrossRef]
- Meeran, N.A. Cellular Response within the Periodontal Ligament on Application of Orthodontic Forces. J. Indian Soc. Periodontol. 2013, 17, 16–20. [Google Scholar] [CrossRef]
- Dinoi, M.T.; Marchetti, E.; Garagiola, U.; Caruso, S.; Mummolo, S.; Marzo, G. Orthodontic Treatment of an Unerupted Mandibular Canine Tooth in a Patient with Mixed Dentition: A Case Report. J. Med. Case Rep. 2016, 10, 170. [Google Scholar] [CrossRef]
- Lyotard, N.; Hans, M.; Nelson, S.; Valiathan, M. Short-Term Postorthodontic Changes in the Absence of Retention. Angl. Orthod. 2010, 80, 1045–1050. [Google Scholar] [CrossRef]
- Proffit, W.R. Equilibrium Theory Revisited: Factors Influencing Position of the Teeth. Angl. Orthod. 1978, 48, 175–186. [Google Scholar] [CrossRef]
- Little, R.M. Stability and Relapse of Dental Arch Alignment. Br. J. Orthod. 1990, 17, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Del Corso, M.; Inchingolo, F.; Sammartino, G.; Charrier, J.-B. Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) in Human Cell Cultures: Growth Factor Release and Contradictory Results. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 110, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Behrents, R.G.; Harris, E.F.; Vaden, J.L.; Williams, R.A.; Kemp, D.H. Relapse of Orthodontic Treatment Results: Growth as an Etiologic Factor. J. Charles H. Tweed Int. Found. 1989, 17, 65–80. [Google Scholar] [PubMed]
- Saccomanno, S.; Quinzi, V.; D’Andrea, N.; Albani, A.; Coceani Paskay, L.; Marzo, G. Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review. Healthcare 2021, 9, 825. [Google Scholar] [CrossRef]
- Devi, S.; Jain, R.K. Comparison of Retention Characteristics of Clear Bow Hawley’s and Vacuum Formed Retainers—A Randomized Controlled Trial. J. Orofac. Sci. 2022, 14, 128. [Google Scholar] [CrossRef]
- Vermesan, D.; Inchingolo, F.; Patrascu, J.M.; Trocan, I.; Prejbeanu, R.; Florescu, S.; Damian, G.; Benagiano, V.; Abbinante, A.; Caprio, M.; et al. Anterior Cruciate Ligament Reconstruction and Determination of Tunnel Size and Graft Obliquity. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 357–364. [Google Scholar]
- Minervini, G.; Lucchese, A.; Perillo, L.; Serpico, R.; Minervini, G. Unilateral Superior Condylar Neck Fracture with Dislocation in a Child Treated with an Acrylic Splint in the Upper Arch for Functional Repositioning of the Mandible. Cranio 2017, 35, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Kartal, Y.; Kaya, B. Fixed Orthodontic Retainers: A Review. Turk. J. Orthod. 2019, 32, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; D’Amico, C.; Cicciù, M.; Fiorillo, L. Temporomandibular Joint Disk Displacement: Etiology, Diagnosis, Imaging, and Therapeutic Approaches. J. Craniofac. Surg. 2023, 34, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of Temporomandibular Disorders (TMD) in Pregnancy: A Systematic Review with Meta-analysis. J. Oral Rehabil. 2023, 50, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Sinha, A.; Sonar, S.; Batra, P.; Raghavan, S. A Prospective Randomized Controlled Trial on the Comparative Clinical Efficiency and Hygiene of a Ceramic Inter Locking Retainer and a Flexible Spiral Wire Bonded Retainer. Indian J. Dent. Res. 2021, 32, 174. [Google Scholar] [CrossRef]
- Edman Tynelius, G.; Bondemark, L.; Lilja-Karlander, E. A Randomized Controlled Trial of Three Orthodontic Retention Methods in Class I Four Premolar Extraction Cases—Stability after 2 Years in Retention. Orthod. Craniofac. Res. 2013, 16, 105–115. [Google Scholar] [CrossRef]
- Forde, K.; Storey, M.; Littlewood, S.J.; Scott, P.; Luther, F.; Kang, J. Bonded versus Vacuum-Formed Retainers: A Randomized Controlled Trial. Part 1: Stability, Retainer Survival, and Patient Satisfaction Outcomes after 12 Months. Eur. J. Orthod. 2018, 40, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Jowett, A.C.; Littlewood, S.J.; Hodge, T.M.; Dhaliwal, H.K.; Wu, J. CAD/CAM Nitinol Bonded Retainer versus a Chairside Rectangular-Chain Bonded Retainer: A Multicentre Randomised Controlled Trial. J. Orthod. 2023, 50, 55–68. [Google Scholar] [CrossRef]
- Arash, V.; Teimoorian, M.; Farajzadeh Jalali, Y.; Sheikhzadeh, S. Clinical Comparison between Multi-Stranded Wires and Single Strand Ribbon Wires Used for Lingual Fixed Retainers. Prog. Orthod. 2020, 21, 22. [Google Scholar] [CrossRef]
- Shim, H.; Foley, P.; Bankhead, B.; Kim, K.B. Comparative Assessment of Relapse and Failure between CAD/CAM Stainless Steel and Standard Stainless Steel Fixed Retainers in Orthodontic Retention Patients:A Randomized Controlled Trial. Angl. Orthod. 2022, 92, 87–94. [Google Scholar] [CrossRef]
- Armstrong, A.W.; Oliver, D.R.; Araújo, E.A.; Thiesen, G.; Kim, K.B. Comparing Orthodontic Relapse of Mandibular Anterior Teeth with Traditional Bonded versus Magnetic Retainers after 2 Years of Retention. J. World Fed. Orthod. 2017, 6, 45–49. [Google Scholar] [CrossRef]
- Alrawas, M.B.; Kashoura, Y.; Tosun, Ö.; Öz, U. Comparing the Effects of CAD/CAM Nickel-Titanium Lingual Retainers on Teeth Stability and Periodontal Health with Conventional Fixed and Removable Retainers: A Randomized Clinical Trial. Orthod. Craniofac. Res. 2021, 24, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Nunez, W.; Vezina, G.C.; Aras, I. Comparison of 2 Different Wear Protocols of Vacuum-Formed Retainers with Respect to the Conventional Parameters and 3-Dimensional Superimpositional Analysis. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 743–755.e1. [Google Scholar] [CrossRef] [PubMed]
- Naraghi, S.; Ganzer, N.; Bondemark, L.; Sonesson, M. Comparison of Post-Treatment Changes with and without Retention in Adolescents Treated for Maxillary Impacted Canines—A Randomized Controlled Trial. Eur. J. Orthod. 2021, 43, 121–127. [Google Scholar] [CrossRef]
- Kaya, Y.; Tunca, M.; Keskin, S. Comparison of Two Retention Appliances with Respect to Clinical Effectiveness. Turk. J. Orthod. 2019, 32, 72–78. [Google Scholar] [CrossRef]
- Gera, A.; Gera, S.; Cattaneo, P.M.; Cornelis, M.A. Does Quality of Orthodontic Treatment Outcome Influence Post-Treatment Stability? A Retrospective Study Investigating Short-Term Stability 2 Years after Orthodontic Treatment with Fixed Appliances and in the Presence of Fixed Retainers. Orthod. Craniofac. Res. 2022, 25, 368–376. [Google Scholar] [CrossRef]
- Nagani, N.I.; Ahmed, I. Effectiveness of Two Types of Fixed Lingual Retainers in Preventing Mandibular Incisor Relapse. J. Coll. Physicians Surg. Pak. 2020, 30, 282–286. [Google Scholar] [CrossRef]
- Adanur-Atmaca, R.; Çokakoğlu, S.; Öztürk, F. Effects of Different Lingual Retainers on Periodontal Health and Stability. Angl. Orthod. 2021, 91, 468–476. [Google Scholar] [CrossRef]
- Cernei, E.R.; Dascalu, C.G.; Anistoroaei, D.; Golovcencu, L.; Sodor-Botezatu, A.; Zegan, G. Efficiency of Two Different Types of Upper Bonded Retainers. In Proceedings of the 2022 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 17–18 November 2022; pp. 1–4. [Google Scholar]
- Hoybjerg, A.J.; Currier, G.F.; Kadioglu, O. Evaluation of 3 Retention Protocols Using the American Board of Orthodontics Cast and Radiograph Evaluation. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 16–22. [Google Scholar] [CrossRef]
- Radia, M.; Trivedi, K.; Shah, A.; Parikh, T.; Panchal, H. Evaluation of Long-Term Stability of Curve of Spee Levelled with Continuous Archwires in Two Different Retention Protocol. APOS 2021, 11, 229–234. [Google Scholar] [CrossRef]
- İshakoğlu, S.; Çokakoğlu, S. Evaluation of Relapse with Thermoplastic Retainers Equipped with Microsensors. Angl. Orthod. 2022, 92, 340–346. [Google Scholar] [CrossRef]
- Edman Tynelius, G.; Petrén, S.; Bondemark, L.; Lilja-Karlander, E. Five-Year Postretention Outcomes of Three Retention Methods--a Randomized Controlled Trial. Eur. J. Orthod. 2015, 37, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Kocher, K.E.; Gebistorf, M.C.; Pandis, N.; Fudalej, P.S.; Katsaros, C. Long-Term Effectiveness of Maxillary and Mandibular Bonded Orthodontic Retainers. Oral Health Prev. Dent. 2020, 18, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Canuto, L.F.G.; de Freitas, M.R.; de Freitas, K.M.S.; Cançado, R.H.; Neves, L.S. Long-Term Stability of Maxillary Anterior Alignment in Non-Extraction Cases. Dent. Press J. Orthod. 2013, 18, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Freitas, K.M.S.; Guirro, W.J.G.; de Freitas, D.S.; de Freitas, M.R.; Janson, G. Relapse of Anterior Crowding 3 and 33 Years Postretention. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 798–810. [Google Scholar] [CrossRef]
- Wolf, M.; Schulte, U.; Küpper, K.; Bourauel, C.; Keilig, L.; Papageorgiou, S.N.; Dirk, C.; Kirschneck, C.; Daratsianos, N.; Jäger, A. Post-Treatment Changes in Permanent Retention. J. Orofac. Orthop. 2016, 77, 446–453. [Google Scholar] [CrossRef]
- Schütz-Fransson, U.; Lindsten, R.; Bjerklin, K.; Bondemark, L. Mandibular Incisor Alignment in Untreated Subjects Compared with Long-Term Changes after Orthodontic Treatment with or without Retainers. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 234–242. [Google Scholar] [CrossRef]
- Morais, J.F.; de Freitas, M.R.; de Freitas, K.M.S.; de Janson, G.; Castello Branco, N. Postretention Stability after Orthodontic Closure of Maxillary Interincisor Diastemas. J. Appl. Oral Sci. 2014, 22, 409–415. [Google Scholar] [CrossRef]
- Guirro, W.J.G.; Freitas, K.M.S.; Janson, G.; de Freitas, M.R.; Quaglio, C.L. Maxillary Anterior Alignment Stability in Class I and Class II Malocclusions Treated with or without Extraction. Angl. Orthod. 2016, 86, 3–9. [Google Scholar] [CrossRef]
- Zafarmand, A.H.; Qamari, A.; Zafarmand, M.M. Mandibular Incisor Re-Crowding: Is It Different in Extraction and Non-Extraction Cases? Oral Health Dent. Manag. 2014, 13, 669–674. [Google Scholar]
- Stability and Relapse after Orthodontic Treatment of Deep Bite Cases—A Long-Term Follow-Up Study—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/23197574/ (accessed on 6 June 2023).
- Bjering, R.; Sandvik, L.; Midtbø, M.; Vandevska-Radunovic, V. Stability of Anterior Tooth Alignment 10 Years out of Retention. J. Orofac. Orthop. 2017, 78, 275–283. [Google Scholar] [CrossRef]
- Steinnes, J.; Johnsen, G.; Kerosuo, H. Stability of Orthodontic Treatment Outcome in Relation to Retention Status: An 8-Year Follow-Up. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Inchingolo, A.M.; Dipalma, G. Non-Hodgkin Lymphoma Affecting the Tongue: Unusual Intra-Oral Location. Head Neck Oncol. 2011, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Vaida, L.L.; Bud, E.S.; Halitchi, L.G.; Cavalu, S.; Todor, B.I.; Negrutiu, B.M.; Moca, A.E.; Bodog, F.D. The Behavior of Two Types of Upper Removable Retainers—Our Clinical Experience. Children 2020, 7, 295. [Google Scholar] [CrossRef]
- Reddy, L.K.V.; Madithati, P.; Narapureddy, B.R.; Ravula, S.R.; Vaddamanu, S.K.; Alhamoudi, F.H.; Minervini, G.; Chaturvedi, S. Perception about Health Applications (Apps) in Smartphones towards Telemedicine during COVID-19: A Cross-Sectional Study. J. Pers. Med. 2022, 12, 1920. [Google Scholar] [CrossRef] [PubMed]
- Rathi, S.; Chaturvedi, S.; Abdullah, S.; Rajput, G.; Alqahtani, N.M.; Chaturvedi, M.; Gurumurthy, V.; Saini, R.; Bavabeedu, S.S.; Minervini, G. Clinical Trial to Assess Physiology and Activity of Masticatory Muscles of Complete Denture Wearer Following Vitamin D Intervention. Medicina 2023, 59, 410. [Google Scholar] [CrossRef] [PubMed]
- Mummolo, S.; Mancini, L.; Quinzi, V.; D’Aquino, R.; Marzo, G.; Marchetti, E. Rigenera® Autologous Micrografts in Oral Regeneration: Clinical, Histological, and Radiographical Evaluations. Appl. Sci. 2020, 10, 5084. [Google Scholar] [CrossRef]


| Articles screening strategy | Keywords: “relapse” and “orthodontic” |
| Boolean Indicators: (“A” AND “B”) | |
| Timespan: 10 years (2013–2023) | |
| Electronic Database: Pubmed, Web of Science, Scopus |
| Criteria | Application in the Present Study |
|---|---|
| Population | patients after fixed orthodontic therapy that received removable retention devices or fixed retainers |
| Intervention | analysis of the retention device |
| Comparison | comparison between the various types of devices, whether mobile or stationary and the degree of reception with each of them |
| Outcomes | stability over time or relapse |
| Study design | Randomised Clinical Trials (RCT), case series with more than 5 case reports (CS), clinical trials (CT), retrospective studies (RS), prospective studies (PS); observational study (O) |
| Author(s) and Year | Study Design | Number of Patients | Average Age (Years) | Retainer Type | Follow Up | Outcomes |
|---|---|---|---|---|---|---|
| Sinha, A. et al. (2021) [25] | PRCT | 40 | 15.61 ± 1.13 and 5.83 ± 1.07 | Flexible spiral wire versus ceramic interlocking bonded | Not available | Both retainers maintained their results at the end of treatment, although with a slight relapse in both groups. |
| Tynelius, G.E. et al. (2013) [26] | RCT | 75 (45F and 30M) | 14.4 | Removable vacuum-formed retainer (covering palate and the upper teeth from 3-3); bonded 3-3 retainer; Ortho-Tain positioner | 24 months | All devices maintained the orthodontic results achieved, with minimal and acceptable relapse. |
| Forde, K. et al. (2017) [27] | RCT | 30 | 16 and 17 | Bonded versus vacuum-formed retainers | 12 months | There was no significant difference in stability or retainer survival in the maxilla. In the mandible, bonded retainers are more effective at maintaining mandibular labial segment alignment but have a higher failure rate. |
| Jowett, A.C. et al. (2022) [28] | RCCT | 68 | Not available | CAD/CAM Memotain® retainer versus Ortho-FlextechTM | 6 months | A high number of failures were recorded with the CAD/CAM retainer (50%) on the upper arch compared to the other |
| Arash, V. et al. (2020) [29] | PS | 250 (99 M and 151 F) | 13–30 | Stainless-steel twisted wire (G&H) versus titanium ribbon (Retainium®) | 24 months | It has the same clinical effect, but the ribbon retainer has less failure in terms of detachment |
| Shim, H. et al. (2022) [30] | RCT | 46 (18 M and 28 F) | CAD/CAM 16.5 (median 15.3), Lab 15.8 (median 13.6), Traditional 15.2 (median 13.6) | CAD/CAM stainless-steel Dentaflex retainer (Dentaurum) versus Dentaflex retainer manually bent versus Ortho-FlexTech (Reliance) | 3–6 months | The CAD/CAM group showed the slightest variation in the inter-canine distance between T3 and T1 and the minor variation, together with the traditional group, in the frontal group. The CAD/CAM group had the highest failure rate, and the traditional group had the lowest. |
| Armstrong, A.W. et al. (2017) [31] | CS | 80 | Not Available | Magnetic retainer versus canine–canine bonded retainer (0.0195-inch twist flex wire) | Not available | There are no significant differences in the efficacy of canine-to-canine retainers bonded to each tooth and the magnetic retainer. |
| Alrawas, M.B. et al. (2020) [32] | RCT | 60 | 20 | CAD/CAM NiTi, multi-stranded stainless steel, single-stranded titanium and vacuum-formed removable retainer | 6 months | All retainers showed some relapse in the mandibular anterior teeth and had the same clinical failure rate in maintaining teeth alignment. |
| Garcia-Nunez, W. et al. (2023) [33] | CS | 34 | 18.3 ± 6.6 and 18.6 ± 5.7 | Vacuum-formed retainer wear part-time versus full-time | 6 months | Some relapses occurred with both protocols at the end of the 1st month. Part-time wear was less effective in maintaining results during the 1st and the 6th month after debonding. |
| Naraghi, S. et al. (2021) [34] | RCT | 63 (39 F and 24 M) | 12.9 | Mainly vacuum-formed retainers. Bonded retainers only in patients who had spaces before orthodontic treatment | 12 months | The two groups had no clinically significant difference; however, the irregularity difference was statistically significant (0.4 versus 1.3 mm). Retainers are not necessary in these cases. |
| Devi, S. et al. (2022) [18] | RCT | 46 | >18 | Clear bow Hawley versus Vacuum-formed retainer | 12 months | No difference was found between the two devices so they can be used equally. |
| Kaya, Y. et al. (2019) [35] | RCT | 30 | 17.53 ± 3.89 (Essix) and 16.54 ± 2.24 (Hawley) | Essix versus Hawley retainers | 12 months | No statistically significant differences were found in the two groups, although irregularity increased. The clinical effectiveness of the two devices was similar. |
| Gera, A. et al. (2021) [36] | RS | 287 | 18.3 ± 10.2 | Fixed retainer (0.021 in 6-filament round stainless steel) on the upper and lower arch and upper mobile | 24 months | Stability was good during this evaluation period. |
| Nasreen Iqbal Nagani and Imtiaz Ahmed (2020) [37] | RCT | 54 | 14–30 | Fibre-reinforced composite retainers (INOD, U.P. Fiber Splint, 2 mm) versus 0.0175” stainless steel wire (All Star Orthodontics) | 12 months | Fibre-reinforced retainers are more effective in preventing mandibular incisor relapse. |
| Rabia Adanur-Atmaca et al. (2021) [38] | RCT | 132 | 16 | 0.0160” × 0.022” dead-soft eight-braided stainless-steel wire, 0.0215” 5-strand stainless-steel wire, 0.014” CAD/CAM nitinol retainer (Memotain®), connected bonding pads | 12 months | There was no clinically significant relapse in any groups after one year. |
| Dalya Al-Moghrabi et al. (2018) [1] | RCT | 82 | 21 | Fixed retainer versus removable retainer | 4 years | Fixed retention offers the potential benefit of improved preservation of the mandibular labial segment’s alignment. |
| Eduar Radu Cernei et al. (2022) [39] | RS | 150 | 11–15 | Bonded upper retainers | 12 months | Splinx retainer group reported almost twice as many relapses as Ortho Flextech Group, but not statistically significant. |
| Adam Johannes Hoybjerg et al. (2013) [40] | RS | 90 | 15.2 | Fixed versus removable retainers (Essix and Hawley) | Not available | The upper Hawley/lower bonded showed the most significant amount of settling, and the upper Essix/lower related had the least settling, but these differences were statistically insignificant |
| Mansi Radia et al. (2021) [41] | RCT | 20 | 18 ± 2 | Fixed retainer; Removable retainer | 12 months | occlusal coverage of the Essix retainer does not allow any extrusion and retains the curve of Spee. |
| Sait Ishakoglu et Serpil Cokakoglu (2022) [42] | SP | 42 | 17.83–18.15 | Essix retainer | 12 months | A wear time of at least nine h/d is recommended to maintain mandibular anterior alignment. |
| Gudrun Edman Tynelius et al. (2014) [43] | RCT | 49 | Not Available | Removable retainer covering the palate and anterior teeth; Fixed retainer; Prefabricated positioner | 5 years | The three retention methods (removable vacuum-formed retainer covering the palate and the anterior maxillary teeth from canine-to-canine and bonded canine-to-canine retainer in the lower arch; maxillary removable vacuum-formed retainer combined with the stripping of the lower anterior teeth; and prefabricated positioner had similar clinical results. |
| Katharina, E. Kocher et al. (2020) [44] | RS | 80 | 12–28 | Fixed retainers: 0.016” × 0.022” eight-strand braided SS wire (Ormco) bonded to all six anterior teeth and 0.027” round β-titanium (Ormco) | Not Available | Mandibular 0.016”× 0.022” braided SS retainers bonded to all six anterior teeth are more effective in maintaining anterior alignment than 0.027” round β-titanium retainers bonded only to the canines. Both retainers maintain inter-canine width. In the maxilla, 0.016” × 0.022” braided SS retainers hold the anterior alignment. |
| Gonçalves Canuto et al. (2013) [45] | RS | 23 | 13.6 | Upper Hawley retainer and lower bonded retainer canine–canine. | 4.92 years | The maxillary incisors irregularity increased significantly (1.52 mm) during long-term posttreatment. |
| Freitas et al. (2017) [46] | RS | 28 (9 M and 19 F) | 12.72 | Hawley plate in the maxillary arch; Fixed bonded retainer canine–canine in the mandibular arc | 33 years | In the short term (within three years), relapse occurred in both the upper (2.18 mm according to the Little irregularity index) and lower arch (1.58 mm). In the long term, only mandibular incisors showed relapse (3.86 mm) |
| Wolf et al. (2016) [47] | RS | 30 | Not available | Twistflex retainer Dentaflex 0.45 mm three-strand twisted steel wire bonded from lower canine to canine | 6 months | Superimposition of the models immediately after debonding and six months later showed changes in the three planes of space, especially for the canines. Increased inter-canine diameter and reduced OVJ during treatment are risk factors for relapse. |
| Schutz-Fransson et al. (2019) [48] | RS | 105 | Not available | Canine-to-canine retainer (0.028” spring hard wire) or a Twist flex retainer (0.0195”) | 12 years | No significant differences were shown in patients who wore a retainer and those who did not wear a retainer in the long term, as recurrence occurred in both cases. To maintain good stability of the results, patients should wear the retainer lifelong. |
| Morais et al. (2014) [49] | O | 30 (17 F and 13 M) | Not available | Hawley retainer | 5.6 years | After orthodontic treatment and Hawley retainer, lateral diastemas are very stable; central diastemas, on the other hand, in 60% of cases, have recurrences. |
| Guirro et al. (2016) [50] | O | 103 | 13.06 | Hawley | 7.52 years | Although relapse occurred in the maxillary arch, both in extraction and non-extraction cases, the results were not statistically significant. |
| Zafarmand et al. (2014) [51] | RS | 40 (non-extraction group: 4 M and 15 F) (Extraction group: 6 M and 15 F) | Non-extraction group: 16.2 Extraction group: 14.9 | Hawley retainer | 4 years | Relapse values were not statistically significant in the group subjected to extractions (2.11 mm according to the Irregularity Index) and in the group not subjected to extractions (1.65 mm); in both cases, the phenomenon occurred within four years after retention. |
| Danz, J.C. et al. (2014) [52] | RS | 61 | 11–29 | Lower bonded retainer and an upper removable bite plate | 11.9 years | 10% of the patients showed relapse equal to or more significant than 50% incisor overlap, and their overbite increase was low. |
| Bjering, R. et al. (2017) [53] | CS | 51 | 12–26 | Relapse fixed and mobile | 10 years | Long-term outcome ten years after retention and the possible influence of treatment-related factors on posttreatment stability of the dental arches. Patients with extraction had LII scores 1.0 mm lower than patients treated without extraction. |
| Steinnes, J. et al. (2017) [54] | CS | 67 | 20–50 | Relapse fixed and mobile | 8 years | Evaluates the stability of orthodontic treatment outcome and retention status seven or more years after active treatment. Anterior LII in the total study sample after treatment was only about 1 mm in both arches. |
| Abdulraheem, S. et al. (2020) [55] | RS | 92 | 12–27 | Lower lingual bonded retainer versus no retainer | 12 years | The LII showed equal values before treatment and at the follow-up registrations. A certain percentage of incisors is due to growth and not orthodontic relapse. |
| Vaida et al. (2020) [56] | RS | 618 | 11–17 | Removable retainers | 6–12 months | Evaluate the behaviour of two types of removable retainers. A total of 9.1% of the patients presented mild recurrences, mainly in the first six months (58.9%), while 2.6% presented severe recurrences, mainly in the first six months (62.5%). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, F.; Inchingolo, A.M.; Ceci, S.; Carpentiere, V.; Garibaldi, M.; Riccaldo, L.; Di Venere, D.; Inchingolo, A.D.; Malcangi, G.; Palermo, A.; et al. Orthodontic Relapse after Fixed or Removable Retention Devices: A Systematic Review. Appl. Sci. 2023, 13, 11442. https://doi.org/10.3390/app132011442
Inchingolo F, Inchingolo AM, Ceci S, Carpentiere V, Garibaldi M, Riccaldo L, Di Venere D, Inchingolo AD, Malcangi G, Palermo A, et al. Orthodontic Relapse after Fixed or Removable Retention Devices: A Systematic Review. Applied Sciences. 2023; 13(20):11442. https://doi.org/10.3390/app132011442
Chicago/Turabian StyleInchingolo, Francesco, Angelo Michele Inchingolo, Sabino Ceci, Vincenzo Carpentiere, Mariagrazia Garibaldi, Lilla Riccaldo, Daniela Di Venere, Alessio Danilo Inchingolo, Giuseppina Malcangi, Andrea Palermo, and et al. 2023. "Orthodontic Relapse after Fixed or Removable Retention Devices: A Systematic Review" Applied Sciences 13, no. 20: 11442. https://doi.org/10.3390/app132011442
APA StyleInchingolo, F., Inchingolo, A. M., Ceci, S., Carpentiere, V., Garibaldi, M., Riccaldo, L., Di Venere, D., Inchingolo, A. D., Malcangi, G., Palermo, A., Tartaglia, F. C., & Dipalma, G. (2023). Orthodontic Relapse after Fixed or Removable Retention Devices: A Systematic Review. Applied Sciences, 13(20), 11442. https://doi.org/10.3390/app132011442













