Abstract
The functional capacity of the cervical spine plays a central role in healthy living. The aim of this study was to examine the sex-related effect on cervical strength, range of motion (ROM), and the musculoskeletal pain profile in young physically active individuals. A total of 30 males and 30 females (21.53 ± 1.15 years old), without injury or chronic pain at the cervical joint, participated in the study. ROM (forward flexion, extension, lateral flexion-rotation), maximal isometric strength (forward flexion, extension, lateral flexion), and musculoskeletal pain were assessed using an electronic goniometer, a handheld dynamometer, and the Nordic questionnaire, respectively. The results revealed that: (a) females had higher ROM during extension and lateral flexion than males (p < 0.05); (b) males had higher absolute strength than females in all movement directions, and higher relative strength/body mass (at forward flexion) and flexion/extension ratio (p < 0.05); (c) ROM and strength were not significantly different between right and left sides (p > 0.05); (d) a large proportion (43.3%) of the participants had cervical pain; and (e) cervical strength showed a significant small negative correlation with pains (p < 0.05; r = −0.225 to −0.345). In conclusion, the derived reference values may be used by health and fitness professionals to extensively evaluate the cervical spine and to design specific exercise programs for injury prevention and rehabilitation.
1. Introduction
The cervical spine consists of the seven first vertebrae of the spine and plays an important role in daily life because it supports the head, surrounds and protects the spinal cord, and is responsible for a wide range of head and neck motions [1]. Different factors such as the adoption of sedentary life (reduced physical activity) and poor ergonomic conditions (inadequate posture using electronic devices, repetitive and hurried movements, long static and sitting positions, poor sleep quality, etc.), in conjunction with different individual (age, sex, musculoskeletal pain history, etc.) and psychosocial (stress, anxiety, depression, etc.) factors, may affect the prevalence of cervical pain in the adult population [2,3,4,5,6,7,8,9,10,11], although future studies are needed to strengthen these findings. Cervical pain is now one of the most common musculoskeletal disorders (prevalence ranges from 17% to 75%) [4,6,12,13,14,15], with detrimental effects not only for the individual itself, but also for the society and economy in general. Previous systematic reviews demonstrated that sex has been previously well-studied as a potential risk factor for cervical pain; however, the results of studies are mixed regarding this topic [6,16]. Some studies have shown significant sex-related differences in cervical pain (females demonstrated greater prevalence of cervical pain than males), while other studies have found no significant sex-related differences in the prevalence, incidence, or years lived with disability in individuals with neck pain [6,16,17,18]. There is evidence that cervical pain is related to reduced quality of life, increased morbidity and disability, increased sick leave and health care costs, and reduced work productivity [4,14,19,20].
For this reason, the protection of the cervical spine and the maintenance of satisfactory functional capacity levels (range of motion and strength) in the specific body area is of crucial importance [21] for healthy and independent living. The timely and systematic evaluation of cervical range of motion and isometric strength, using specialized tests, can decisively contribute to injury prevention and the rehabilitation process of the cervical joint, since having a good range of motion and isometric strength seems to have beneficial effects on pain elimination [22,23]. The above findings are strengthened by previous investigations, which report that individuals with neck pain, loss of cervical lordosis, migraines, or whiplash show lower levels of cervical strength and/or range of motion compared to healthy individuals [22,23,24,25,26]. Furthermore, reduced craniocervical stability, due to ligament laxity or weakness, abnormalities in the connective tissues, or structural issues in the craniovertebral junction, called “craniocervical instability (CCI)”, is strongly associated with cervical pain and refers to excessive movement or instability between the skull (cranium) and the upper cervical spine (cervical vertebrae) [27]. The deep cervical flexor muscles (DCFs) seem to play a central role in the maintenance of craniocervical stability, since they are considered important stabilizers of the head and neck posture [28]. It has been hypothesized that when muscle performance is reduced, the balance between the stabilizers on the posterior aspect of the neck and the DCFs will be interrupted, resulting in loss of proper alignment and posture, which then probably contributes to cervical impairment [28]. Thus, the maintenance of adequate DCF levels through specific craniocervical flexor-muscle training enhances the ability and improves the neuromuscular control and strength of the DCF (i.e., longus colli and longus capitis), simultaneously reducing neck pain and disability [29,30,31].
In the scientific literature, several studies evaluated and created indicative values or norms for cervical isometric strength using a large variety of devices (fixed frame dynamometers, computerized dynamometers, or handheld dynamometers), testing positions (standing, sitting, supine, prone, or quadruped) and protocols in different populations, such as workers, athletes and non-athletes, younger and older individuals, and males and females [14,21,22,32,33,34,35,36,37,38,39,40,41,42,43]. It should be mentioned that most of the aforementioned studies have mainly focused on absolute cervical isometric strength values, reporting conflicting results concerning age- and sex-related effects [33,38,42,43]. However, there is limited information regarding (a) the relative cervical isometric strength values, (b) the cervical strength asymmetries between left and right sides, and (c) the cervical flexion-to-extension ratios. However, the evaluation and calculation of all the above strength parameters may provide a more complete picture of the proper function, stability, and balance of the cervical spine. There is a notion that the muscular imbalance between the strength of cervical extensor and flexor muscles can be negatively correlated with the stabilization of the cervical spine [24,36]. It has also been reported that low levels of cervical strength and cervical flexor-to-extensor ratio values less than 60% are associated with an increased prevalence and incidence of sport-related concussion in adolescents and adults [36,44,45,46], where other studies have reported no significant relationship between cervical strength and concussion [47].
The measurement and evaluation of the range of motion constitute a basic component of the physical examination of the cervical joint. Numerous studies have evaluated and created indicative values or norms for cervical range of motion using multiple radiological (functional X-rays) or non-radiological devices (goniometers and inclinometers, and electromagnetic, ultrasonic, and optoelectronic systems), testing positions, and protocols in different populations, showing wide variations in the measured values [48,49,50]. Age and sex are two of the most important factors that could affect the cervical range of motion; however, previous studies that examined the age- and sex-related effects on cervical range of motion demonstrated controversial results [48,51,52]. Several studies stated that (a) females have greater cervical ROM than males and (b) cervical ROM is reduced with increasing age, whereas other studies reported no significant differences between males and females, or between different ages [48,51,52]. Therefore, the influence of sex or age on cervical ROM still merits discussion to draw safer conclusions [48].
Taking all the above into consideration, the main objective of this study was to evaluate and create a comprehensive strength (absolute and relative values, flexion/extension ratio, strength asymmetries), range of motion (ROM), and musculoskeletal pain profile of the cervical spine, using simple, handy, and portable equipment (handheld dynamometer and digital goniometer), in young physically active adults (19–24 years old), while simultaneously examining the possible sex-related differences (males vs. females). It has been hypothesized that males would demonstrate greater cervical strength values than females in all directions of movement, as well as greater cervical flexion/extension ratio values than females, while females would exhibit greater cervical ROM values than males. It was also hypothesized that basic anthropometric characteristics (body height and body mass) would influence cervical absolute strength values, therefore eliminating the differences in relative strength values between males and females. Furthermore, it was hypothesized that males and females would produce similar strength and ROM values in both sides (right and left). Finally, it was hypothesized that cervical strength values would significantly correlate with cervical pain, whereas ROM values would not show a significant correlation with cervical pain.
2. Materials and Methods
2.1. Participants
Sixty (30 women and 30 men) healthy (without chronic health problems) young adults (19–24 years old), voluntarily participated in the present study (Table 1). All the individuals were physically active, participating 3 times per week (1 h/day) in non-organized physical activities (cycling and walking for daily transportation, use of stairways, household and outside home chores), as evaluated using a specific questionnaire created by the American College of Sports Medicine (ACSM) [53]. It should be also mentioned that none of the participants took part in organized exercise programs for physical fitness enhancement or specialized training for the cervical spine that could affect the results of the study. The study excluded participants who (a) suffered from any musculoskeletal or other chronic disease, (b) showed cervical pain, discomfort, or numbness on the day of the measurement, (c) presented an injury at the cervical spine in the last 6 months before the start of the study, (d) suffered from chronic cervical pain, (e) reported the use of any medication (prescribed or not), or (f) followed a physical therapy for the cervical spine. Prior to the start of the study, all the individuals were informed about the testing procedure and signed an informed consent form. The study was approved by the Ethics Committee of the University of Thessaly.

Table 1.
Age and anthropometric characteristics of the sample (mean ± standard deviation).
2.2. Study Design
Before the start of the study, a familiarization session with the experimental testing protocols was carried out. Then, the measurements were performed on one day, with the evaluation of cervical range of motion (ROM) preceding the evaluation of cervical strength. Before the assessment of the cervical ROM and cervical strength, the participants warmed up. The warm-up protocol was performed from a sitting position in a chair (with the back straight, the hands on the thighs of the legs, and the feet flat on the floor) and included 10 repetitions of cervical dynamic movements (forward flexion, extension, lateral flexion and rotation), 10 s of stretching exercises (forward flexion, extension, lateral flexion and rotation) and submaximal isometric contractions at the cervical spine (flexion, extension, lateral flexion) with the participant’s hand as resistance. The measurements took place at the Training Laboratory of the Department of Physical Education and Sports Science of the University of Thessaly and were performed by the same investigator and under the same conditions.
2.3. Testing Procedures
Anthropometric characteristics, musculoskeletal pains, cervical range of motion (forward flexion, extension, lateral flexion, and rotation), and cervical strength (forward flexion, extension, lateral flexion) were measured.
2.3.1. Anthropometric Characteristics
The basic anthropometric characteristics (body mass and body height) were assessed using a calibrated physician’s scale (Seca model 755, Seca, Hamburg, Germany) and a telescopic height rod, respectively, as previously described by the ACSM [53].
2.3.2. Musculoskeletal Pains
Duration and intensity (using a 10-point scale) of pain in the cervical spine, days off from everyday activities, and difficulties in daily activities due to pain were evaluated using the Nordic questionnaire [54] for a time period of 2 months.
2.3.3. Cervical Range of Motion—Cervical Strength
Testing Position
Both cervical ROM and strength were assessed from a standardized sitting position to minimize errors and movement compensation. In the present study, we placed special emphasis on the selection of the proper chair used for the ROM and strength measurements. More specifically, the chair should meet the following criteria: (a) it should be stable without wheels and armrests, (b) it should have a back for better lumbar spine support (not a softback), and (c) it should be a height-adjusted chair depending on the height of the participants (feet flat on the floor, with knee angle approximately 90°). During the measurements, the participants were positioned in a sitting position with their backs straight and stabilized with Velcro straps in the back of the chair, their hands on the thighs of their legs, and their feet flat on the floor (Figure 1). At the beginning of every trial, the participant started from a fixed point with his/her head in the neutral position.

Figure 1.
Setup of the participant during the cervical ROM and strength measurements.
Range of Motion Measurement
Cervical ROM was assessed in 4 directions: (a) extension, (b) forward flexion, (c) lateral flexion (right and left), and (d) rotation (right and left) using an electronic goniometer (K-force Sens, Kinvent, France) and the values demonstrated in degrees (Figure 2). A previous study [55] reported very good reliability and validity for the measurement of wrist range of motion in young healthy adults (21–27 years old) using the electronic goniometer (K-force Sens, Kinvent, Seattle, WA, USA). Furthermore, in our study we found high intrasession reliability (reliability among trials in the same testing occasion) for the measurement of cervical range of motion using the electronic goniometer (K-force Sens, Kinvent). In the total sample, we found high reliability in cervical forward flexion (ICC = 0.987; 95% CI: 0.911–0.995; SEM% = 1.94), extension (ICC = 0.991; 95% CI: 0.952–0.997; SEM% = 1.66), lateral flexion (ICC = 0.987; 95% CI: 0.906–0.996; SEM% = 2.28 for the right side and ICC = 0.988; 95% CI: 0.924–0.996; SEM% = 1.95 for the left side), and rotation (ICC = 0.989; 95% CI: 0.929–0.996; SEM% = 1.20 for the right side and ICC = 0.985; 95% CI: 0.865–0.995; SEM% = 1.25 for the left side). In the present study, the examiner placed and stabilized the electronic goniometer with a Velcro strap at the center of the participant’s forehead. For each direction of movement, the participant performed 3 maximal trials with 20 s rest between each trial and 1 min rest between each direction of movement, and the best score (at each direction) was considered for analysis.
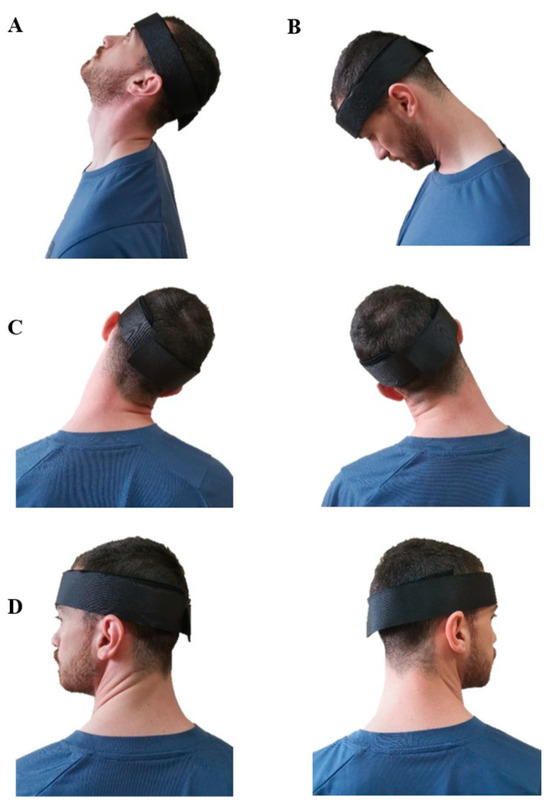
Figure 2.
Cervical range of motion measurements: (A) extension, (B) forward flexion, (C) lateral flexion, and (D) rotation.
Maximal Isometric Strength Measurement
Maximal isometric cervical strength was assessed in three directions: (a) forward flexion, (b) extension, and (c) lateral flexion (right and left) using a handheld dynamometer (K-Force Dynamometer, Kinvent, France) (Figure 3). A previous study [56] demonstrated that the Kinvent k-force handheld dynamometer has good to excellent intra- and inter-rater reliability for almost all the upper (shoulder, elbow, wrist) and lower (hip, knee) limb movements assessed in young males and females (18–30 years old), except for ankle dorsiflexion, where the reliability was moderate in all assessments. Furthermore, Olds et al. [57] also found that the Kinvent k-force handheld dynamometer is reliable and valid for strength and torque measurement during the athletic shoulder test. During the measurements, the investigator placed the handheld dynamometer in the appropriate position, and then he held resistance with both hands (to the participant’s strength) so that the head and neck remained in the neutral position. In more detail, the handheld dynamometer was placed (a) in the center of the forehead just superior to the eyebrows for the forward flexion test, (b) slightly superior to the external occipital protuberance for the extension test, and (c) on the lateral aspect of the head just superior to the ear for lateral (right and left) flexion tests [21,43] (Figure 3).
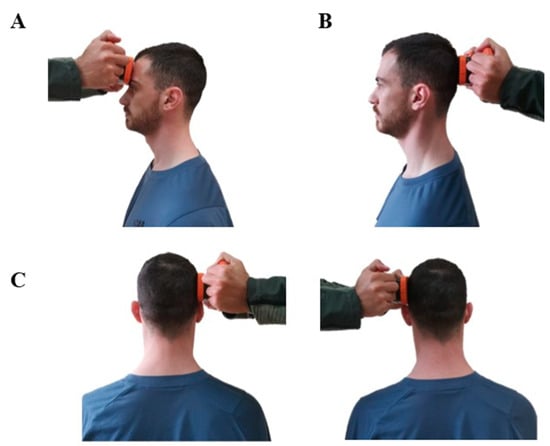
Figure 3.
Cervical maximal isometric strength measurements: (A) forward flexion, (B) extension, and (C) lateral flexion.
In each direction of movement, the participants performed 3 maximal trials (duration of isometric contraction 5 s) with 1 min rest between each trial and 1 min rest between each direction, and the best score was considered for analysis. The absolute cervical strength values (kg) were assessed in each direction of movement, and the relative cervical strength values per unit of body mass (kg of cervical strength/kg of body mass) and body height (kg of cervical strength/cm of body height) were calculated. The cervical flexion (CF) to cervical extension (CE) strength ratio was also calculated using the following equation:
CervicalF/E ratio = (Cervical flexion strength/Cervical extension strength) × 100.
2.4. Statistics
IBM SPSS Statistics v.26 software (IBM Corporation, Armonk, NY, USA) was used to analyze the data. A statistical power analysis (software package GPower 3.0) prior to the study showed that a total number of 60 participants (30 participants per sex group) would yield adequate power (>0.85) and a level of significance (<0.05). Additionally, the Kolmogorov–Smirnov test was used to examine the normal distribution of the data (all variables followed the normal distribution). Independent samples t-tests were used to investigate possible differences in cervical range of motion, maximal strength, and musculoskeletal pains between males and females, while paired t-tests were used to examine possible differences in range of motion and strength values between right and left sides. Furthermore, bivariate correlation analyses were used to examine the associations among neck pain, cervical strength, and range of motion as well as among cervical strength, range of motion, and anthropometric characteristics (body mass and body height). Cohen’s effect sizes were also calculated using the following equation: d = difference between means/pooled SD. The level of significance for all statistical analyses was set at p < 0.05 and the results are presented as mean ± standard deviation.
3. Results
3.1. Cervical Range of Motion
Independent samples t-test showed that females had higher range of motion values at extension (t58 = −4.03, p < 0.01; Cohen d: 1.04; mean % difference: 14.7), as well as at right (t58 = −2.30, p < 0.05; Cohen d: 0.60; mean % difference: 10.5) and left lateral flexion (t58 = −2.70, p < 0.05; Cohen d: 0.70; mean % difference: 11.1) (Table 2). On the other hand, no significant differences were observed between males and females in the range of motion values at forward flexion (t58 = 0.52, p > 0.05), as well as at right (t58 = −0.97, p > 0.05) and left rotation (t58 = −1.48, p > 0.05).

Table 2.
Cervical range of motion values (mean ± standard deviation) in males and females.
Moreover, paired samples t-test analyses showed that there are no statistically significant differences between right and left lateral flexion (t59 = −0.51; p > 0.05; mean % difference: 0.27–0.89) and right and left rotation (t59 = −1.87; p > 0.05; mean % difference: 1.8–2.8) in both males and females.
3.2. Cervical Isometric Strength
3.2.1. Absolute Values
Independent samples t-tests showed that males had statistically greater values of cervical strength in forward flexion (t58 = 7.82; p = 0.000; Cohen d: 2.12; mean % difference: 37.7), extension (t58 = 4.04; p = 0.000; Cohen d: 1.06; mean % difference: 20.4), right lateral flexion (t58 = 4.07; p = 0.000; Cohen d: 1.08; mean % difference: 23.7), and left lateral flexion (t58 = 4.03; p = 0.000; Cohen d: 1.05; mean % difference: 23.3), as well as a greater cervical flexion/extension ratio (t58 = 4.99; p = 0.000; Cohen d: 1.31; mean % difference: 21.8), than females (Table 3). Furthermore, paired samples t-test analyses showed that there were no statistically significant differences between right and left lateral flexion (t59 = −1.42; p > 0.05) in both males (mean % difference: 1.3) and females (mean % difference: 1.8).

Table 3.
Cervical absolute strength values (mean ± standard deviation) in males and females.
3.2.2. Relative Values
When the cervical strength values were adjusted to body height, independent samples t-tests showed that males had statistically greater strength values at forward flexion (t58 = 7.05; p = 0.000; Cohen d: 2; mean % difference: 30), extension (t58 = 2.82; p = 0.007; Cohen d: 0.5; mean % difference: 9), right lateral flexion (t58 = 3.03; p = 0.004; Cohen d: 0.67; mean % difference: 12.5), and left lateral flexion (t58 = 2.98; p = 0.004; Cohen d: 0.5; mean % difference: 12.4) than females (Figure 4).
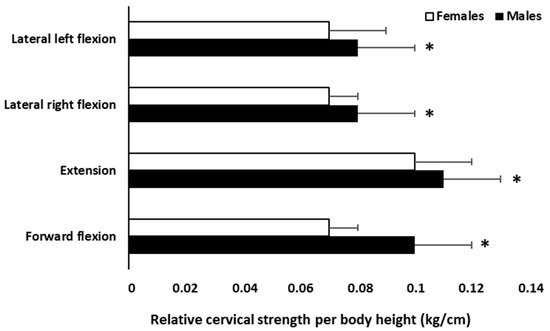
Figure 4.
Differences in relative cervical strength values (per body height) between males and females. * p < 0.05 significant difference between males and females.
On the other hand, when the values were adjusted to body mass, independent samples t-tests showed no statistically significant differences between males and females in cervical extension (t58 = 0.66; p = 0.513), right lateral flexion (t58 = 1.39; p = 0.170), and left lateral flexion (t58 = 1.33; p = 0.188) (Figure 5). The only significant difference between males and females was found in forward flexion, where males showed greater relative cervical strength values than females (t58 = 5.86; p = 0.000; Cohen d: 1.43; mean % difference: 21.7).
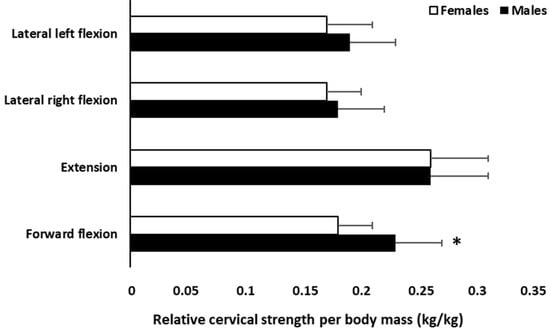
Figure 5.
Differences in relative cervical strength values (per body mass) between males and females. * p < 0.05 significant difference between males and females.
3.3. Relationship of Anthropometric Characteristics with Cervical Strength and ROM
Bivariate correlation analysis presented a significant positive correlation of body mass with cervical forward flexion (r = 0.716, p = 0.000), extension (r = 0.619, p = 0.000), right lateral flexion (r = 0.657, p = 0.000), and left lateral flexion (r = 0.647, p = 0.000) in the total sample (males and females). Furthermore, bivariate correlation analysis displayed a significant positive correlation of body height with cervical forward flexion (r = 0.665, p = 0.000), extension (r = 0.480, p = 0.000), right lateral flexion (r = 0.465, p = 0.000), and left lateral flexion (r = 0.464, p = 0.000) in the total sample (males and females).
Nevertheless, no significant relationship was found between anthropometric characteristics (body mass and body height) and range of motion measurements in both males and females (p > 0.05).
3.4. Cervical Pain
3.4.1. Prevalence of Cervical Pain
According to data analysis, 43.3% of the total sample presented short-term cervical pain in the last 2 months (no significant difference in the prevalence of pain was observed between males and females), while 56.7% of the sample had no cervical pain.
In those who experienced cervical pain, the mean duration of pain (total days of pain in 2 months) was 2.54 ± 0.99 days and the mean intensity of pain (from 1 to 10) was 3.65 ± 1.41, while the days off from daily activities due to cervical pain were 0.46 ± 1.96 days and the days with difficulties in daily activities due to cervical pain were 3.81 ± 7.14 days. It should be mentioned that independent samples t-tests showed that there were no significant differences between males and females in the duration and intensity of cervical pain, as well as in the days off from daily activities due to cervical pain (p > 0.05).
3.4.2. Relationship of Cervical Strength and ROM with Cervical Pain
Bivariate correlation analysis showed a statistically significant small negative correlation of the duration of cervical pain (total days of pain) with cervical forward flexion strength (r = −0.288, p < 0.05), extension strength (r = −0.255, p < 0.05), right lateral flexion strength (r = −0.287, p < 0.05), and left lateral flexion strength (r = −0.345, p < 0.05). On the contrary, bivariate correlation analysis showed that cervical ROM did not significantly associate with cervical pain (p > 0.05).
4. Discussion
In the present study, we documented a sex-related effect in absolute cervical strength values, with males presenting greater values (20–38%, depending on the movement direction) than females in all the tested movement directions. The results of this study are in line with previous investigations in the scientific literature in which males have greater absolute cervical strength values in comparison with females [32,33,34,37,43]. The sex-related differences in cervical strength values may be attributed to different factors, such as the head and neck anthropometric parameters and geometry/morphology (i.e., females have smaller external neck and vertebral dimensions, as well as more slender necks and less neck cross-sectional area) [37], the basic anthropometric characteristics (body mass and/or body height) [34], the higher concentrations of anabolic hormones observed in male individuals, and probably the higher voluntary neural activity of the muscle actions [58,59], as well as the different lifestyle behaviors (i.e., higher levels of physical activity observed in males compared to females).
As mentioned earlier, the basic anthropometric characteristics (body mass and body height) could affect absolute cervical strength values. This notion has been strengthened by the results of this and previous studies which reported a significant relationship between body mass, body height, or body mass index with cervical strength measurements [32,41], although there are studies that did not find a significant relationship between basic anthropometric characteristics and cervical strength values [33]. It seems that the correlation of basic anthropometric characteristics (especially of body mass) with cervical strength is higher in physically active and trained individuals, whereas this correlation in a normal population is much lower [34,35]. Furthermore, some researchers found sex-related differences in the correlation of basic anthropometric characteristics with cervical strength [34,38]. It should also be mentioned that in the present study, when the absolute cervical strength values were adjusted to body height, significant sex-related differences (males reported greater values than females) remained after height adjustment; however, the differences between males and females were significantly lower (forward flexion: 30%, extension: 9%, lateral flexion: 12.4–12.5%) compared to those observed in absolute values (forward flexion: 37.7%, extension: 20.4%, lateral flexion: 23.3–23.7%). On the other hand, when the absolute values were adjusted to body weight, the only sex-related difference between males and females was observed in forward flexion (21.7%), while in the other movement directions, no significant sex-related differences were observed. The results of this study are in line with those of Peolsson et al. [40], who reported greater sex-related differences in absolute cervical strength values (mean difference 55%) compared to relative values per body mass (mean difference 30%) or body mass index (mean difference 41%).
In the present study, we also found no significant difference in lateral flexion cervical strength between the right and left side (mean % difference: 1.3–1.8) in both males and females. The results of the present study are in agreement with previous studies that also reported no significant differences between right and left lateral flexion in adults and adolescents [21,32,60], due to the bilateral arrangement of the involved musculature in different activities of daily life, as well as in different sport activities. On the other hand, Vernon et al. [26] and Chiu et al. [33] demonstrated significant difference (6–11%) in cervical lateral flexion strength between the right and left sides in males, but no difference was found in women [33]. Chiu et al. [33] hypothesized that the sex-related difference in strength asymmetry between the right and left sides may be because men were more involved in heavy manual work and most people are right-handed, leading to higher demand on the neck muscles on the right side in male individuals.
Regarding the cervical flexion-to-extension ratio, in the present study, we reported a significant difference between males and females, with males (mean ratio value: 89.17%) presenting greater ratio values than females (mean ratio value: 69.75%). Most previous studies that evaluated the cervical flexion-to-extension ratio in healthy males and females, using different dynamometers, reported values ranging from approximately 60 to 75% [21,24,26,34]. In the present study, the cervical flexion-to-extension ratio value for females agrees with the normal values reported in the international literature, while the mean cervical flexion-to-extension ratio value in males is much higher. In the present study, the greater flexion-to-extension ratio value in males compared to females may be attributed to the greater difference observed in cervical forward flexion strength. Indeed, we reported sex-related differences in cervical flexion that were almost double those in extension strength values. The finding of this study agrees with a previous study which found greater sex-related differences in cervical flexion compared to extension (females have 32% weaker neck strength during flexion and 20% during extension than males) [37]. From the results of the present study, it seems that males should emphasize specific exercise programs for improvement, especially of cervical extensor muscles, to change the flexion-to-extension ratio values to more normal levels, according to the scientific literature. This is of crucial importance since there is a notion that high cervical flexion-to-extension ratio values, as observed in the males of the present study, may be associated with the loss of cervical lordosis [24] and the dropped head syndrome [61].
Concerning cervical ROM, many studies have evaluated and created indicative values or norms in different age groups, but it seems that quite large differences exist between them [48], making the comparisons of ROM values difficult among studies. The reported measurements vary considerably due to differences in measurement instruments (radiological or non-radiological), testing positions and setups (constrained or unconstrained), testing protocols, and subjects’ characteristics [48,49,50]. In our study, females showed significantly higher values in extension (mean % difference: 14.7) and both right (mean % difference: 10.5, with medium effect size) and left (mean % difference: 11, with medium effect size) lateral flexion in comparison with males, while no differences were observed in forward flexion and rotation (no differences in ROM values were observed between right and left side at lateral flexion and rotation in both males and females). The sex-related difference in cervical ROM has been made “a subject of debate” in an attempt to draw safer conclusions on this topic. Several studies showed that females exceed males at cervical ROM and others showed no significant differences between males and females [48,49,50,51,52]. Differences in subjects’ characteristics, as well as in testing protocols, may account for these equivocal findings among studies regarding the sex-related effect on cervical ROM.
Previous studies reported that age is an important factor that could affect sex-related differences in cervical ROM [48,51]. According to the systematic review and meta-analysis of Pan et al. [48], in the younger age group (20 s), no sex-related differences in the cervical ROM were observed, probably because in most cases the youngest age group exhibited the greatest ROM level. On the other hand, males in their 30 s and 40 s revealed lower ROM values than females, while males in their 50 s displayed greater ROM values (although not significant) than females [48]. The authors assumed that the females of this age (50 s) experienced menopause, something that can reduce spine mobility [62,63]. After this period of life, older females (60 s) once more showed greater cervical ROM values than males.
An additional important finding of this study is that 43.3% of the total sample presented short-term cervical pain. Previous studies reported a similar prevalence of neck pain in young adults as well as in middle-aged individuals [13,14,15]. In the present study, no significant differences were observed between males and females in the musculoskeletal pain parameters (prevalence of pain, duration, and intensity of pain, negative impact of musculoskeletal pains in daily activities). Other studies in the scientific literature reported conflicting results regarding the sex-related effect on musculoskeletal pain of the cervical joint. Several studies reported that cervical pain is more common in females than males, while other studies, in line with the results of the present study, reported no differences in cervical pain between males and females [16]. Previous investigators who demonstrated sex-related differences in musculoskeletal pain of the cervical joint mentioned that the lower cervical strength level is an important factor that may be the cause of this situation [41,64]. It is not clear whether weak cervical muscles promote cervical pain or if cervical pain results in weaker musculature, but it seems that there is a connection between cervical pain and weakness [41]. In the present study, we also found a significant negative association between cervical pain and cervical strength, while no significant association was observed between range of motion values and cervical pain. The association between cervical range of motion and musculoskeletal pain shows conflicting results in the international literature, strengthening the importance of future studies on this topic. Some studies found significant associations between cervical range of motion and pain, whereas others did not find significant associations [23,50].
This study has some limitations that could affect its outcomes, and, as a result, their generalizability. Firstly, the findings of this study are clearly limited to young (19–24 years old) physically active males and females, without any chronic health problems. Future studies could evaluate and create indicative values for cervical strength, ROM, and musculoskeletal pain in other age groups (children and adolescents, middle-aged and older individuals) as well as in individuals with different health and physical activity/training status. Furthermore, the results of this study are limited to the testing position (sitting position in a chair), the testing protocols, and the equipment (handheld dynamometer for cervical strength measurements and digital goniometer for cervical ROM measurements) used for the evaluation of cervical strength and ROM. Another limitation of this study is the fact that, except for the basic anthropometric characteristics (body mass and body height), we did not measure any head or neck anthropometric characteristics (absolute and relative neck length, neck circumference, head circumference etc.) in order to examine their association with cervical strength and ROM values in males and females. Additionally, the sample size (although it yielded adequate power, as mentioned in the Methods section) may be an additional limitation of this study. A larger sample could further strengthen the findings of the present study. Finally, the equipment (electronic goniometer, k-force Sens, Kinvent and handheld dynamometer, k-force dynamometer, Kinvent) that we used recently arrived on the market and, until now, there has been limited information regarding its reliability and validity. To the best of our knowledge, although there is no published information regarding the test-retest reliability of the electronic goniometer and the handheld dynamometer used at the cervical joint, previous studies in other joints reported good/high levels of reliability and validity.
5. Conclusions
From the results of the present study, it seems that young physically active males have higher absolute cervical strength values than females (a greater difference was observed in cervical forward flexion strength). It should be mentioned that the differences in basic anthropometric characteristics (in body height and especially in body mass) between males and females affect the absolute cervical strength values. In the present study, no cervical strength asymmetries between the right and left sides were observed in males and females, while the cervical flexion-to-extension ratio was greater in males compared to females. Concerning the range of motion, females have higher ROM values during extension and lateral flexion than males, while ROM values during forward flexion and right and left rotation did not differ between males and females. It should be mentioned that no ROM differences between the right and left sides were observed in males and females. Finally, it seems that cervical strength values are significantly correlated with cervical pain, while, no correlation was observed between ROM values and cervical pain.
Author Contributions
Conceptualization, C.B., K.K. and V.G. (Vassilis Gerodimos); methodology, C.B. and V.G. (Vaggelis Gymnopoulos); investigation, C.B. and V.G. (Vaggelis Gymnopoulos); data curation, C.B. and K.K.; writing—original draft preparation, C.B.; writing—review and editing, K.K. and V.G. (Vassilis Gerodimos); supervision, V.G. (Vassilis Gerodimos). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Thessaly (protocol code: 1857 and date of approval: 8 December 2021).
Informed Consent Statement
Informed consent was obtained from all subjects and participant’s parents involved in the study.
Data Availability Statement
Data are unavailable due to privacy or ethical restrictions.
Acknowledgments
We wish to thank our subjects for their participation in the present study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kaiser, J.T.; Reddy, V.; Lugo-Pico, J.G. Anatomy, Head and Neck: Cervical Vertebrae. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Cimmino, M.A.; Ferrone, C.; Cutolo, M. Epidemiology of chronic musculoskeletal pain. Best Pract. Res. Clin. Rheumatol. 2011, 25, 173–183. [Google Scholar] [CrossRef] [PubMed]
- Damasceno, G.M.; Ferreira, A.S.; Nogueira, L.A.C.; Reis, F.J.J.; Andrade, I.C.S.; Meziat-Filho, N. Text neck and neck pain in 18–21-year-old young adults. Eur. Spine J. 2018, 27, 1249–1254. [Google Scholar] [CrossRef]
- Genebra, C.V.D.S.; Maciel, N.M.; Bento, T.P.F.; Simeão, S.F.A.P.; De Vitta, A. Prevalence and factors associated with neck pain: A population-based study. Braz. J. Phys. Ther. 2017, 21, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Hansraj, K.K. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg. Technol. Online 2014, 25, 277–279. [Google Scholar]
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.M.; Kolahi, A.-A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef]
- Lee, W.-H.; Ko, M.-S. Effect of sleep posture on neck muscle activity. J. Phys. Ther. Sci. 2017, 29, 1021–1024. [Google Scholar] [CrossRef]
- Lei, J.-X.; Yang, P.-F.; Yang, A.-L.; Gong, Y.-F.; Shang, P.; Yuan, X.-C. Ergonomic Consideration in Pillow Height Determinants and Evaluation. Healthcare 2021, 9, 1333. [Google Scholar] [CrossRef]
- Malchaire, J.; Roquelaure, Y.; Cock, N.; Piette, A.; Vergracht, S.; Chiron, H. Musculoskeletal complaints, functional capacity, personality and psychosocial factors. Int. Arch. Occup. Environ. Health 2001, 74, 549–557. [Google Scholar] [CrossRef]
- Shahwan, B.S.; D’Emeh, W.M.; Yacoub, M.I. Evaluation of computer workstations ergonomics and its relationship with reported musculoskeletal and visual symptoms among university employees in Jordan. Int. J. Occup. Med. Environ. Health 2022, 35, 141–156. [Google Scholar] [CrossRef]
- Walankar, P.P.; Kemkar, M.; Govekar, A.; Dhanwada, A. Musculoskeletal pain and risk factors associated with smartphone use in university students. Indian J. Occup. Environ. Med. 2021, 25, 220–224. [Google Scholar] [CrossRef]
- Algarni, A.D.; Al-Saran, Y.; Al-Moawi, A.; Bin Dous, A.; Al-Ahaideb, A.; Kachanathu, S.J. The Prevalence of and Factors Associated with Neck, Shoulder, and Low-Back Pains among Medical Students at University Hospitals in Central Saudi Arabia. Pain Res. Treat. 2017, 2017, 1235706. [Google Scholar] [CrossRef] [PubMed]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Karatrantou, K.; Gerodimos, V. A comprehensive wellness profile in sedentary office employees: Health, musculoskeletal pains, functional capacity, and physical fitness indices. Work 2023, 74, 1481–1489. [Google Scholar] [CrossRef]
- Todd, A.; McNamara, C.L.; Balaj, M.; Huijts, T.; Akhter, N.; Thomson, K.; Kasim, A.; Eikemo, T.A.; Bambra, C. The European epidemic: Pain prevalence and socioeconomic inequalities in pain across 19 European countries. Eur. J. Pain 2019, 23, 1425–1436. [Google Scholar] [CrossRef] [PubMed]
- Jahre, H.; Grotle, M.; Smedbråten, K.; Dunn, K.M.; Øiestad, B.E. Risk factors for non-specific neck pain in young adults. A systematic review. BMC Musculoskelet. Disord. 2020, 21, 366. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.M.; May, S.; Klaber-Moffett, J.; Sharp, D.M.; Gardiner, E. Risk factors for the onset of non-specific neck pain: A systematic review. J. Epidemiol. Community Health 2010, 64, 565–572. [Google Scholar] [CrossRef]
- Kim, R.; Wiest, C.; Clark, K.; Cook, C.; Horn, M. Identifying risk factors for first-episode neck pain: A systematic review. Musculoskelet. Sci. Pract. 2018, 33, 77–83. [Google Scholar] [CrossRef]
- Daffner, S.D.; Hilibrand, A.S.; Hanscom, B.S.M.; Brislin, B.T.; Vaccaro, A.R.; Albert, T.J. Impact of Neck and Arm Pain on Overall Health Status. Spine 2003, 28, 2030–2035. [Google Scholar] [CrossRef]
- Ijzelenberg, W.; Burdorf, A. Risk Factors for Musculoskeletal Symptoms and Ensuing Health Care Use and Sick Leave. Spine 2005, 30, 1550–1556. [Google Scholar] [CrossRef]
- Eagle, S.R.; Nagai, T.; Morgan, P.; Hendershot, R.; Sell, T.C. Naval Special Warfare (NSW) crewmen demonstrate diminished cervical strength and range of motion compared to NSW students. Work 2017, 58, 111–119. [Google Scholar] [CrossRef]
- De Loose, V.; Oord, M.V.D.; Burnotte, F.; Van Tiggelen, D.; Stevens, V.; Cagnie, B.; Danneels, L.; Witvrouw, E. Functional Assessment of the Cervical Spine in F-16 Pilots with and without Neck Pain. Aviat. Space Environ. Med. 2009, 80, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Stenneberg, M.S.; Rood, M.; de Bie, R.; Schmitt, M.A.; Cattrysse, E.; Scholten-Peeters, G.G. To What Degree Does Active Cervical Range of Motion Differ between Patients with Neck Pain, Patients with Whiplash, and Those without Neck Pain? A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabilit. 2017, 98, 1407–1434. [Google Scholar] [CrossRef] [PubMed]
- Alpayci, M.; Şenköy, E.; Delen, V.; Şah, V.; Yazmalar, L.; Erden, M.; Toprak, M.; Kaplan, Ş. Decreased neck muscle strength in patients with the loss of cervical lordosis. Clin. Biomech. 2016, 33, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, B.; Johnson, C.L.; Curran-Everett, D.; Maluf, K.S. Reliability and group differences in quantitative cervicothoracic measures among individuals with and without chronic neck pain. BMC Musculoskelet. Disord. 2012, 13, 215. [Google Scholar] [CrossRef]
- Vernon, H.T.; Aker, P.; Aramenko, M.; Battershill, D.; Alepin, A.; Penner, T. Evaluation of neck muscle strength with a modified sphygmomanometer dynamometer: Reliability and validity. J. Manip. Physiol. Ther. 1992, 15, 343–349. [Google Scholar]
- Steilen, D.; Hauser, R.; Woldin, B.; Sawyer, S. Chronic Neck Pain: Making the Connection between Capsular Ligament Laxity and Cervical Instability. Open Orthop. J. 2014, 8, 326–345. [Google Scholar] [CrossRef]
- Janda, V. Muscles and motor control in cervicogenic disorders: Assessment and Management. In Physical Therapy of the Cervical and Thoracic Spine, 2nd ed.; Churchill Livingstone: New York, NY, USA, 1994; pp. 195–216. [Google Scholar]
- Suvarnnato, T.; Puntumetakul, R.; Uthaikhup, S.; Boucaut, R. Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: A randomized controlled trial. J. Pain Res. 2019, 12, 915–925. [Google Scholar] [CrossRef]
- O’Leary, S.; Jull, G.; Kim, M.; Vicenzino, B. Specificity in retraining craniocervical flexor muscle performance. J. Orthop. Sports Phys. Ther. 2007, 37, 3–9. [Google Scholar] [CrossRef]
- O’Leary, S.; Jull, G.; Kim, M.; Uthaikhup, S.; Vicenzino, B. Training Mode–Dependent Changes in Motor Performance in Neck Pain. Arch. Phys. Med. Rehabilit. 2012, 93, 1225–1233. [Google Scholar] [CrossRef]
- Catenaccio, E.; Mu, W.; Kaplan, A.; Fleysher, R.; Kim, N.; Bachrach, T.; Zughaft Sears, M.; Jaspan, O.; Caccese, J.; Kim, M.; et al. Characterization of Neck Strength in Healthy Young Adults. PM&R 2017, 9, 884–891. [Google Scholar] [CrossRef]
- Chiu, T.T.; Lam, T.-H.; Hedley, A.J. Maximal isometric muscle strength of the cervical spine in healthy volunteers. Clin. Rehabil. 2002, 16, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Garcés, G.L.; Medina, D.; Milutinovic, L.; Garavote, P.; Guerado, E. Normative database of isometric cervical strength in a healthy population. Med. Sci. Sports Exerc. 2002, 34, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.F.; Gatherer, D.; Jenkins, P.J.; Maclean, J.G.; Hutchison, J.D.; Nutton, R.W.; Simpson, A.H. Age-related differences in the neck strength of adolescent rugby players: A cross-sectional cohort study of Scottish schoolchildren. Bone Joint Res. 2012, 1, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Nutt, S.; McKay, M.J.; Gillies, L.; Peek, K. Neck strength and concussion prevalence in football and rugby athletes. J. Sci. Med. Sport 2022, 25, 632–638. [Google Scholar] [CrossRef]
- Vasavada, A.N.; Danaraj, J.; Siegmund, G.P. Head and neck anthropometry, vertebral geometry and neck strength in height-matched men and women. J. Biomech. 2008, 41, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Mehlsen, J.; Bülow, P.M.; Østergaard, K.; Danneskiold-Samsøe, B. Maximal Isometric Strength of the Cervical Musculature in 100 Healthy Volunteers. Spine 1999, 24, 1343–1348. [Google Scholar] [CrossRef]
- McBride, L.; James, R.S.; Alsop, S.; Oxford, S.W. Intra and Inter-Rater Reliability of a Novel Isometric Test of Neck Strength. Sports 2022, 11, 2. [Google Scholar] [CrossRef]
- Peolsson, A.; Öberg, B.; Hedlund, R. Intra- and inter-tester reliability and reference values for isometric neck strength. Physiother. Res. Int. 2001, 6, 15–26. [Google Scholar] [CrossRef]
- Salo, P.K.; Ylinen, J.J.; Mälkiä, E.A.; Kautiainen, H.; Häkkinen, A.H. Isometric Strength of the Cervical Flexor, Extensor, and Rotator Muscles in 220 Healthy Females Aged 20 to 59 Years. J. Orthop. Sports Phys. Ther. 2006, 36, 495–502. [Google Scholar] [CrossRef]
- Valkeinen, H.; Ylinen, J.; Mälkiä, E.; Alen, M.; Häkkinen, K. Maximal force, force/time and activation/coactivation characteristics of the neck muscles in extension and flexion in healthy men and women at different ages. Eur. J. Appl. Physiol. 2002, 88, 247–254. [Google Scholar] [CrossRef]
- Versteegh, T.; Beaudet, D.; Greenbaum, M.; Hellyer, L.; Tritton, A.; Walton, D. Evaluating the reliability of a novel neck-strength assessment protocol for healthy adults using self-generated resistance with a hand-held dynamometer. Physiother. Can. 2015, 67, 58–64. [Google Scholar] [CrossRef]
- Elliott, J.; Heron, N.; Versteegh, T.; Gilchrist, I.A.; Webb, M.; Archbold, P.; Hart, N.D.; Peek, K. Injury Reduction Programs for Reducing the Incidence of Sport-Related Head and Neck Injuries Including Concussion: A Systematic Review. Sports Med. 2021, 51, 2373–2388. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.L.; Fletcher, E.N.; Fields, S.K.; Kluchurosky, L.; Rohrkemper, M.K.; Comstock, R.D.; Cantu, R.C. Neck Strength: A Protective Factor Reducing Risk for Concussion in High School Sports. J. Prim. Prev. 2014, 35, 309–319. [Google Scholar] [CrossRef]
- Gillies, L.; McKay, M.; Kertanegara, S.; Huertas, N.; Nutt, S.; Peek, K. The implementation of a neck strengthening exercise program in elite rugby union: A team case study over one season. Phys. Ther. Sport 2022, 55, 248–255. [Google Scholar] [CrossRef]
- Garrett, J.M.; Mastrorocco, M.; Peek, K.; Hoek, D.J.v.D.; McGuckian, T.B. The Relationship between Neck Strength and Sports-Related Concussion in Team Sports: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2023, 53, 585–593. [Google Scholar] [CrossRef]
- Pan, F.; Arshad, R.; Zander, T.; Reitmaier, S.; Schroll, A.; Schmidt, H. The effect of age and sex on the cervical range of motion—A systematic review and meta-analysis. J. Biomech. 2018, 75, 13–27. [Google Scholar] [CrossRef]
- Thoomes-de Graaf, M.; Thoomes, E.; Fernández-de-Las-Peñas, C.; Plaza-Manzano, G.; Cleland, J.A. Normative values of cervical range of motion for both children and adults: A systematic review. Musculoskelet Sci, Pract. 2020, 49, 102–182. [Google Scholar] [CrossRef]
- Williams, M.A.; McCarthy, C.J.; Chorti, A.; Cooke, M.W.; Gates, S. A Systematic Review of Reliability and Validity Studies of Methods for Measuring Active andPassive Cervical Range of Motion. J. Manip. Physiol. Ther. 2010, 33, 138–155. [Google Scholar] [CrossRef]
- Dvorak, J.; Antinnes, J.A.; Panjabi, M.; Loustalot, D.; Bonomo, M. Age and Gender Related Normal Motion of the Cervical Spine. Spine 1992, 17, S393–S398. [Google Scholar] [CrossRef]
- Zárate-Tejero, C.A.; Rodríguez-Rubio, P.R.; Brandt, L.; Krauss, J.; Hernández-Secorún, M.; Lucha-López, O.; Hidalgo-García, C. Association between Age, Sex and Cervical Spine Sagittal Plane Motion: A Descriptive and Correlational Study in Healthy Volunteers. Life 2023, 13, 461. [Google Scholar] [CrossRef]
- Ferguson, B. ACSM’s Guidelines for Exercise Testing and Prescription, 9th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014; Volume 58, p. 328. [Google Scholar]
- Jannatbi, L.I.; Nigudgi, S.R.; Shrinivas, R. Assessment of musculoskeletal disorders by standardized Nordic questionnaire among computer engineering students and teaching staff of Gulbarga city. Int. J. Community Med. Public Health 2016, 3, 668–674. [Google Scholar]
- Tekin, F.; Can-Akman, T.; Kitiş, A. Evaluation of the validity and reliability of the KFORCE Sens® electrogoniometer in evaluation of wrist proprioception. Hand Surg. Rehabil. 2022, 41, 183–188. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, M.B.; Oliveira, C.; Ornelas, G.; Soares, T.; Souto, J.; Póvoa, A.R.; Ferreira, L.M.A.; Ricci-Vitor, A.L. Intra-Rater and Inter-Rater Reliability of the Kinvent Hand-Held Dynamometer in Young Adults. Med. Sci. Forum 2023, 22, 12. [Google Scholar] [CrossRef]
- Olds, M.; McLaine, S.; Magni, N. Validity and Reliability of the Kinvent Handheld Dynamometer in the Athletic Shoulder Test. J. Sport Rehabil. 2023, 32, 764–772. [Google Scholar] [CrossRef]
- Häkkinen, K.; Pakarinen, A. Muscle strength and serum testosterone, cortisol and SHBG concentrations in middle-aged and elderly men and women. Acta Physiol. Scand. 1993, 148, 199–207. [Google Scholar] [CrossRef]
- Ryushi, T.; Hakkinen, K.; Kauhanen, H.; Komi, P.V. Muscle fiber characteristics, muscle cross-sectional area and force production in strength athletes, physically active males and females. Scand. J. Sports Sci. 1988, 10, 7–15. [Google Scholar]
- Olivier, P.E.; Du Toit, D.E. Isokinetic neck strength profile of senior elite rugby union players. J. Sci. Med. Sport 2008, 11, 96–105. [Google Scholar] [CrossRef]
- Gourie-Devi, M.; Nalini, A.; Sandhya, S. Early or late appearance of “dropped head syndrome” in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 2003, 74, 683–686. [Google Scholar] [CrossRef]
- Kyllönen, E.S.; Heikkinen, J.E.; Väänänen, H.K.; Kurttila-Matero, E.; Wilen-Rosenqvist, G.; Lankinen, K.S.; Vanharanta, J.H. Influence of estrogen-progestin replacement therapy and exercise on lumbar spine mobility and low back symptoms in a healthy early postmenopausal female population: A 2-year randomized controlled trial. Eur. Spine J. 1998, 7, 381–386. [Google Scholar] [CrossRef]
- Cunha, S.; Costa-Paiva, L.; Pinto-Neto, A.M.; Fonsechi-Carvesan, G.; Nanni, L.; Morais, S.S. Postmenopausal Women with Osteoporosis and Musculoskeletal Status: A Comparative Cross-Sectional Study. J. Clin. Med. Res. 2011, 3, 168–176. [Google Scholar] [CrossRef][Green Version]
- Staudte, H.W.; Dühr, N. Age- and sex-dependent force-related function of the cervical spine. Eur. Spine J. 1994, 3, 155–161. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).