Abstract
Background: The aim of this study was to evaluate the adaptation of a resin-modified glass ionomer to the internal walls of dentin with different conditioning systems, with or without the application of silver diamine fluoride (SDF) and potassium iodide (KI). Methods: Cervical standardized cavities were prepared on the buccal and lingual sides of 15 extracted molars. Molars were then sectioned longitudinally in a buccolingual direction, obtaining two samples from each tooth with two cavities each (60 samples). Samples were randomly divided into three groups (n = 20). Each group was divided into two subgroups. One subgroup did not receive dentin conditioning, one was conditioned with 25% polyacrylic acid—10 s (PA), and one with 37% orthophosphoric acid—5 s (OPA). In the other subgroup, dentine was treated with SDF/KI and not conditioned or conditioned with PA or OPA. All cavities were filled with Riva Light Cure® (RLC). The adaptation of the RLC to the cavity walls was evaluated by SEM at 100× magnification. The area of maximum interfacial gap was magnified at 1000× to measure its size. Kruskal–Wallis and Mann–Whitney U test were used for comparison. A significance level of α = 0.05 was used. Results: No significant differences in the percentage of well-adapted samples were found in subgroups when SDF/KI was used, regardless of whether conditioner was used or not and whether PA or OPA was used (p > 0.05). Regardless of the gap size, dentin treatment with SDF/KI did not negatively influence ionomer adaptation to dentin walls significantly (p > 0.05), except for the subgroup conditioned with OPA (p < 0.05). Furthermore, it improved the adaptation in the axial wall of the subgroup without dentin conditioning (p < 0.05). Conclusion: According to the results of the present in vitro study, the use of SDF/KI did not affect RLC adaptation to the cavity walls. Subsequent use of a conditioner worsens the adaptation of the material to the cavity walls.
1. Introduction
Physiologically and anatomically, dentin is a complex structure, consisting of approximately 70% hydroxyapatite crystals, 18% organic matter, and 12% water and plasma-like fluids. The dentin–pulp complex is derived from the ectomesenchyme, structurally forming a true biological and functional unit [1].
Adhesion to dentin is considered more complex than adhesion to enamel due to its organic component and the presence of a smear layer that obstructs the entrance of the dentinal tubules, decreasing their permeability to adhesive systems and liners. The smear layer should be treated or eliminated, depending on the different bonding strategies and characteristics of the materials to be used [2]. Glass ionomers can chemically bond to dentin due the ion exchange layer at the interface formed by continuous diffuse of aluminum, silicon, fluorine, and strontium when present in the parent glass ionomer, and calcium and phosphorus from dentin [3].
Since Powis et al. [4] introduced polyacrylic acid, it has been used as a conditioner to improve the adhesion of glass ionomers. It contains numerous functional carboxyl ions, which form hydrogen bonds that promote substrate wettability. Its use is recommended at a concentration of 10%, 20%, or 25% [5]. Another alternative is the use of orthophosphoric acid (OPA) at concentrations around 37.5%, between 5 and 10 s [6]. Acid conditioning has been shown to improve the bond strength of glass ionomers to the dentin substrate [6,7,8,9,10]. In addition, the type of conditioner, its application time, and concentration can also influence bond strength [11].
Glass ionomer cements (GIC) are biomaterials that belong to the family of acid-base cements. They are the product of the reaction of weak polymeric acids with phase-separated amorphous sodium–fluorine–aluminum–silicate glass powder [12]. They set in the presence of water and the final structure contains concentrations of unset glass that act as reinforcement. They contain three fundamental components: a soluble polymeric acid, a basic glass, and water. The glass is a complex material consisting of fluorine, calcium or strontium, aluminum silicate, and phosphorus [13]. The polymeric acid solution is mainly polyacrylic acid, although maleic and itaconic acid may be present in lower concentrations to improve handling and increase working time. They set by means of an acid-base reaction 2–3 min after mixing, although the reaction can last up to 48 h. The bioactivity of glass ionomers is produced by an ionic exchange between the material and the substrate that can be maintained over time, with an initial rapid early release phase, followed by a sustained phase [14].
Resin-modified glass ionomer cements (RMGICs) contain the same essential components as conventional GICs, but incorporate a monomer, usually 2-hydroxyethyl methacrylate (HEMA), and a photoinitiator. Therefore, they exhibit two setting reactions: light-curing and the characteristic acid-base reaction of glass ionomers [15].
High density GICs are materials of very high viscosity, whose glasses have been improved by the addition of strontium, bioactive glasses, or even zirconium. This results in a reduction in their working and hardening times, and a notable improvement in their physical–chemical and mechanical properties, together with a minimum solubility. They can be self- or light-cured [16].
Silver diamine fluoride (SDF) is a cost-effective and easy-to-use alternative for the remineralization of carious dentin (13). SDF is presented in an alkaline colorless liquid form (pH 10), composed of 24–27% silver (Ag), 8.5–10.5% ammonia (NH3), and approximately 38% fluoride (F) [9]. Currently, a triple mechanism of action of SDF against caries lesions is described: Firstly, due to the high concentrations of fluoride, a greater diffusion is achieved in enamel and dentin, favoring their remineralization. Secondly, silver possesses a bactericidal action and remains in the demineralized and hypomineralized areas, hardening them and preventing their reinvasion by means of a series of metabolites. Thirdly, ammonia stabilizes the solution and maintains the pH [17]. Furthermore, in dentin, SDF favors the maintenance the collagen matrix’s integrity due to its ability to inhibit bacterial metalloproteinases, which play an important role in the enzymatic degradation of collagen. Potassium iodide (KI) decreases blackening of dentin caused by SDF [18].
The combined use of SDF/KI and bioactive restorative materials such as GICs has been proposed in minimally invasive procedures for the treatment of deep carious lesions, aiming to preserve viable demineralized dentin by exploiting their remineralization ability [19].
One problem that could arise is the adaptation of GICs to cavity walls and their bond strength to SDF/KI-treated dentin. A recent systematic review concludes, not without highlighting the methodological disparity among the included studies, that the application of SDF/KI has no adverse impact on bond strength [20]. Interestingly, some studies even indicate that it increased the bond strength of GICs on SDF/KI-treated dentin [10].
To our knowledge, there are no studies that evaluate the adaptation between RMGICs and dentin when the latter is treated with SDF/KI, nor the influence of the use or absence of a dentin conditioning system before the application of the ionomer. Accordingly, the objective of the present in vitro study was to evaluate the adaptation of a high-viscosity resin-reinforced glass ionomer (Riva Light Cure®) to dentin walls treated with different conditioning systems, with or without the application of SDF/KI, by means of scanning electron microscopy.
The null hypothesis was that the use of SDF/KI does not influence the adaptation of the glass ionomer to cavity walls regardless of dentin conditioning.
2. Materials and Methods
2.1. Sample Preparation
An experimental in vitro study was devised on human molars whose extraction was indicated for periodontal or surgical reasons from donors aged between 40 and 60 years old. The protocol for this study was approved by the Ethics Committee of the Universitat de València (ref. 158063760605607). Written informed consent was obtained from the donors prior to the use of the tooth samples in the present study. The materials used for the present study are described in Table 1

Table 1.
Material characteristics.
Once extracted, the teeth were preserved at room temperature in a 0.1% thymol solution for one week. Organic debris was removed with ultrasonic tips and curettes. The teeth were then inspected under magnification and 15 molars free of caries, cracks, or any other structural defect were selected. They were preserved in physiological saline solution until their use at 4 °C, within 6 months of extraction.
In each tooth, two class V cavities were prepared, one on the buccal side and one on the lingual/palatal side, with the coronal margin in enamel and the apical margin in dentin (1 mm apically from the dentinoenamel junction). The cavity proportions were as follows: 4 mm in length by 4 in width by 2 in depth (2 × 4 × 4). An ISO 835 diamond bur was used to perform the cavities, which was replaced after preparing five cavities. A schematic representation of the cavities view is shown in Figure 1A. Once the cavities were prepared, the teeth were sectioned longitudinally in a buccal/lingual–palatal direction with a diamond disc (ISO 806 104356524 220 Komet, Lemgo, Germany) until the cavity limit was reached, at which point they were separated by fracture by using a dental elevator (Figure 1B). In this way, two samples from each molar with two cavities each were obtained (n = 30 molar halves; n = 60 cavities).
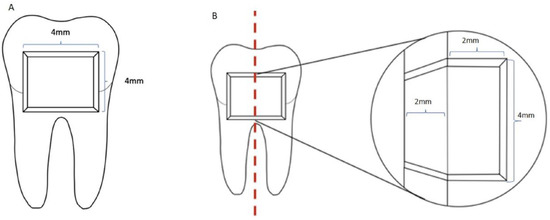
Figure 1.
Cavity design (A); longitudinal view of the cavities after molar sectioning (B).
Twenty molar halves were randomly assigned to a group, accordingly with the dentin-conditioning procedure (25% polyacrylic acid (PA) for 10 s or 37% orthophosphoric acid (OPA) for 5 s). The 10 remaining molar halves were the control group, which received no dentin conditioning. Each group was divided in two subgroups. At the same time, SDF/KI were applied to one of the cavities from each half (subgroup). The distribution and process of the different conditioning procedures is shown in Table 2.

Table 2.
Study subgroups accordingly dentin conditioning procedures and SDF/KI application (n = 10 cavities) in each subgroup.
Once the cavity was conditioned according to the procedure described in Table 2, the Riva Light Cure® was applied. The capsule was first activated, vibrated for 10 s at 4800 rpm, placed in the applicator, and placed in the cavity. The material was adapted to the walls using a plastic instrument, an acetate strip was placed on the surface of the material and light cured with a 1500 mW/cm2 LED lamp (Masters, Madrid, Spain) for 20 s.
The samples were kept at room temperature for 24 h, each specimen was stored individually in labelled Eppendorf tubes with PBS, and then thermocycled. The thermocycling process was performed manually by immersing the specimens alternately in a cold-water bath at a temperature of 5 °C and hot water at 55 °C alternately for 30 s for 1500 cycles. The bath used was Fisherbrand™ (Fisher Scientific SL. Madrid, Spain).
2.2. Sample Visualization under Scanning Electron Microscopy (SEM)
The specimens for each group were dehydrated, mounted on aluminum stubs, and then gold-sputter coated by the Polaron Range SC7640 Sputter Coater (Quorum Technologies LTD, Ashford, Kent, UK). Scanning electron microscopy (SEM) (Hitachi S-4800, Hitachi High-Technologies Corporation, Japan) was used to assess the marginal adaptation of the RLC to the cavity walls. SEM was set on 10 kV for both magnifications (100× and 1000×). At 100×, the interface between the restorative material and dentin was observed along all cavity walls (coronal, axial, and cervical). At any point where interfacial gap was visible on each wall, the image was magnified and the maximum maladaptation at 1000× was measured in µm (Figure 2). The measurement was performed from the surface of the material to the surface of dentin, using the SEM visualization software, as shown in Figure 2c.
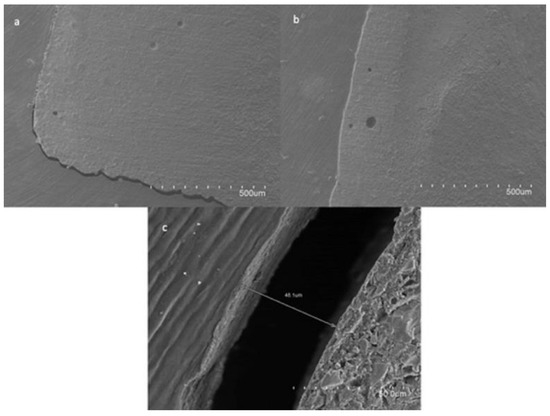
Figure 2.
Representative SEM images of the samples. Images at 100× magnification with interfacial gap (a) and without interfacial gap (b), and image at 1000× magnification measuring the maximum interfacial gap (c). Scale bar: the distance between two points represents 50 µm in panels a and b (magnification ×100), and 5 µm in figure c (magnification ×1000).
2.3. Statistical Analysis
The interfacial gap values for each wall and cavity, measured in micrometers (µm), did not follow a normal distribution (Kolmogorov–Smirnov). The mismatch values, as a function of the dentin conditioning system for each wall, were compared using the Kruskal–Wallis test. Two-by-two comparisons were made with the non-parametric Dunn’s test. The Mann–Whitney U test was used to compare the interfacial gap values in the mesial and distal cavities of each molar sample, one of which had been treated with SDF/KI. The percentage of samples with interfacial gap in each subgroup was compared by means of χ2 test. SPSS 25.0 statistical package (IBM Inc., Chicago, IL, USA) was used for the analysis. A significance level of α = 0.05 was used in the calculations.
3. Results
3.1. Influence of SDF/KI in RLC Adaptation
In all samples in which no dentin conditioning procedure was used, regardless of whether SDF/KI was applied or not, a gap between GIC and the cavity walls was observed. In the samples in which PA was used, gaps were observed in 80% of the samples in which SDF/KI was not used, and in 90% of those in which it was used (p = 0.237). In the samples in which dentin was conditioned with OPA, gaps were observed in 77.8% of the samples in which SDF/KI was used and in 62.5% of those in which it was not used (p = 0.21). No significant differences were found in the global percentage of samples with gaps with regards to the dentin conditioning system (p > 0.05). According to these results, the null hypothesis could not be rejected.
Table 3 shows the mean, standard deviation, median, and interquartile range for the interfacial gap values in each study subgroup. The gap in the cavities in which SDF/KI was used were similar to those in the cavities in which it was not used. In the coronal wall the OPA + GIC subgroup showed a significantly lower gap than the OPA + SDF/KI + GIC subgroup (p < 0.05). The same was observed for the total interfacial gap. In the axial wall, the SDF/KI + GIC subgroup showed a significantly lower mismatch than the GIC subgroup (p < 0.05). In all subgroups the lowest median interfacial gap values were found in the axial and cervical walls.

Table 3.
Interfacial gap values in µm.
3.2. Comparison between Groups
In Figure 3a, it can be observed that, in the coronal wall, the OPA + GIC subgroup showed a significantly lower interfacial gap than the rest of the subgroups. In the axial wall, the interfacial gap was significantly lower in subgroups in which dentin conditioning with PA or with OPA was used, and in the SDF/KI + GIC subgroup, than in the GIC subgroup (Figure 3b). In the cervical wall from the subgroup in which the dentin was conditioned with OPA, significantly less interfacial gap was found than in GIC subgroup (Figure 3c). Finally, when comparing the mean gap in all the walls, the OPA + GIC subgroup again showed lower gap values than the rest of the subgroups (Figure 3d).
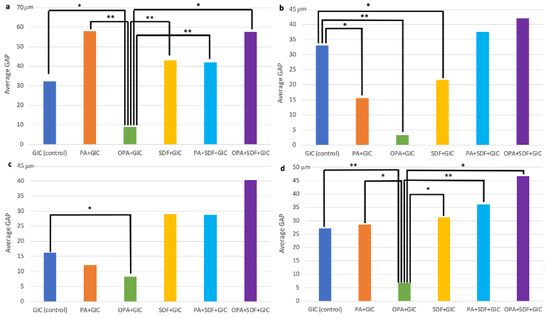
Figure 3.
Gap size comparison between the study subgroups. (a) Coronal wall, (b) axial wall, (c) cervical wall, (d) mean. Statistically significant differences are indicated with an asterisk: * p < 0.05; ** p < 0.01.
4. Discussion
GICs are suitable materials for restorative procedures where there are no substantial mechanical requirements, with a highlighted application in “atraumatic restorative techniques” (ART) and in minimally invasive restorative procedures [21]. The current paradigm for the treatment of dental caries involves the approach form a biological perspective, involving the use of therapies based on the application of fluorides, calcium, phosphates, or other bioactive components. The surgical–restorative approach is reserved for deep cavitated lesions, following the criteria of the selective removal of carious dentin in combination with the use of materials with remineralizing, restorative, and/or bioinductive potential [22].
Although some studies show that RMGICs are less biocompatible than conventional ionomers [23], others claim that the pulpal inflammatory response and odontoblastic changes produced are similar to those produced by conventional GICs [7].
The adaptation of the restorative material to the cavity walls is essential for a correct sealing of the interface between the material and the substrate to avoid microleakage. Therefore, the study of the adaptation of the material to the cavity walls is an adequate criterion to evaluate interfacial sealing. The use of SEM makes it possible to evaluate the adaptation of the material around the entire perimeter and to accurately measure the possible presence of gaps [5,24]. One drawback is the possible removal of the material from the cavity walls caused by the drying of the samples and the vacuum of the SEM. However, direct scanning of the samples was selected in this study because indirect epoxy resin replicas showed some disadvantages, such as time consumption. It is also more likely that areas with excess resin or voids will remain. Furthermore, even when specimens can be replicated to preserve fidelity or to withstand the SEM vacuum conditions, it is difficult to determine the extent to which the structures of interest have been masked or altered by the preparation or replication process [25].
In this study, we aimed to evaluate the adaptation of a high-viscosity RMGIC to cavity walls with different dentin conditioning systems followed by the use or absence of SDF/KI. For this purpose, Riva Light Cure® was used. This material replaces dentine and chemically bonds to the tooth. Accordingly, following the manufacturer’s recommendations, no etching or bonding is required. In addition, since it is a high-density material, it can be used in restorations that need to support load [20].
A study that evaluated the interface between Riva Light Cure® and dentin treated with different conditioning systems found that etching with 37% OPA for 5 s or with PA for 10 s reported the presence of resin tags inside the dentin tubules, while when GIC was applied without prior conditioning, an empty interface was found between the restorative material and the dentin [6]. In the present study, it was decided to use these same dentin conditioning times and systems. It should be noted that, although interfacial gaps were found in all samples regardless of the conditioning system used, when OPA was used for 5 s, the gaps were significantly lower in all walls (p < 0.05). This is probably due to the infiltration of the resin component of Riva Light Cure® into the partially demineralized dentin. This short treatment time allows partial demineralization without a significant loss of calcium ions that could negatively affect the ionic bonding of the material to the dentin substrate [10].
Tanumiharja et al. [9] evaluated the adaptation of conventional GICs and RMGICs with and without prior conditioning with PA, finding similar adaptation with the two types of GICs with and without conditioning. However, they were able to identify hybridization areas when PA was used. In the present study, conditioning with PA alone significantly improved adaptation in the axial wall (p < 0.05).
The RMGIC had a thermal expansion coefficient of 25.4 × 10 °C, which was quite high compared with the tooth structure. Therefore, after thermocycling, there were slight changes in marginal adaptation [26]. The samples in this study were subjected to thermocycling to simulate oral cavity conditions, although our samples exposed cavity walls that are not exposed under physiological conditions. This may have influenced our results, constituting a limitation of this study.
This study aimed to evaluate the effect of SDF/KI on the adaptation of Riva Light Cure® to dentin followed or not by conditioning with 10 s of PA or 5 s or OPA. Other authors have evaluated the influence of SDF/KI on the bond strength of restorative materials to enamel and dentin. A systematic review and meta-analysis [27] concluded that pre-application of SDF/KI does not alter the adhesion of GICs, and even improves adhesion [28]. The results obtained in this study indicate that SDF/KI did not cause significant changes in the presence of interfacial gaps (p > 0.05) independently of the dentin conditioning procedure. Even in the subgroup without conditioning, a significantly higher adaptation was found with SDF/KI in the axial wall (p < 0.05). These results agree with a recent meta-analysis performed by Fröhlich et al. [12], in which it was found that the adhesion of GICs to SDF/KI-treated dentin did not differ significantly from untreated dentin, even improving in some cases, which could be explained by the chemical adhesion that GICs exhibit with the dentin substrate. In this meta-analysis, no difference was found in GIC adhesion with or without dentin rinsing after SDF/KI placement, as is the case when dentin bonding systems are used. The study by François et al. showed that the interface between a GIC and healthy dentin was not affected by the use of SDF/KI [29].
Lastly, it should be highlighted that SDF was used with a double layer of KI to reduce the dark staining caused by silver. According to the literature reviewed, KI does not seem to influence GICs adaptation [21].
The cavities were cut in half in order to have a sample that could be visualized on SEM once prepared, so as not to disturb the interface between the GIC and the dentine wall. On the other hand, we had samples with identical characteristics in the SDF/KI and non-SDF/KI subgroups. Although this could be a limitation, as it does not reproduce the clinical situation, we believe that it could allow a better assessment of the interface adaptation.
5. Conclusions
According to the results of the present in vitro study, the use of SDF/KI did not affect the Riva Light Cure® adaptation to the cavity walls. The size of gap was higher when SDF/KI was followed by dentin conditioning with OPA. The gap size in the SDF/KI was not affected by the post conditioning with PA. In the axial wall SDF/KI improves adaptation when used without any conditioner. Thus, from a practical point of view, the use of SDF/KI does not interfere with the adaptation of the glass ionomer to the cavity walls. Subsequent use of a conditioner does not improve the adaptation of the material to the cavity walls.
Author Contributions
Conceptualization, J.G., A.A.-C. and C.L.; Data curation, C.L.; Formal analysis, J.G.; Funding acquisition, L.F.; Investigation, A.A.-C.; Methodology, J.G., A.A.-C. and C.L.; Project administration, L.F.; Resources, J.L.S.; Software, C.L.; Supervision, J.L.S., L.F. and C.L.; Visualization, J.L.S. and L.F.; Writing—original draft, J.G. and A.A.-C.; Writing—review and editing, J.L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Universitat de València (ref. 158063760605607).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Arola, D.D.; Gao, S.; Zhang, H.; Masri, R. The Tooth: Its Structure and Properties. Dent. Clin. N. Am. 2017, 61, 651–668. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J. Dentin bonding as a function of dentin structure. Dent. Clin. N. Am. 2002, 46, 277–301. [Google Scholar] [CrossRef] [PubMed]
- Tian, K.V.; Mahmoud, M.Z.; Cozza, P.; Licoccia, S.; Fang, D.C.; Di Tommaso, D.; Chass, G.A.; Neville Greaves, G. Periodic vs. molecular cluster approaches to resolving glass structure and properties: Anorthite a case study. J. Non Cryst. Soli. 2016, 451, 138–145. [Google Scholar] [CrossRef]
- Powis, D.R.; Follerås, T.; Merson, S.A.; Wilson, A.D. Improved Adhesion of a Glass Ionomer Cement to Dentin and Enamel. J. Dent. Res. 1982, 61, 1416–1422. [Google Scholar] [CrossRef] [PubMed]
- Tay, F.R.; Smales, R.J.; Ngo, H.; Wei, S.H.; Pashley, D.H. Effect of different conditioning protocols on adhesion of a GIC to dentin. J. Adhes. Dent. 2001, 3, 153–167. [Google Scholar]
- Ebaya, M.M.; Ali, A.I.; Mahmoud, S.H. Evaluation of Marginal Adaptation and Microleakage of Three Glass Ionomer-Based Class V Restorations: In Vitro Study. Eur. J. Dent. 2019, 13, 599–606. [Google Scholar] [CrossRef]
- Eskandarizadeh, A.; Parizi, M.T.; Goroohi, H.; Badrian, H.; Asadi, A.; Khalighinejad, N. Histological assessment of pulpal responses to resin modified glass ionomer cements in human teeth. Dent. Res. J. 2015, 12, 144–149. [Google Scholar]
- Fröhlich, T.T.; Botton, G.; Rocha, R.O. Bonding of Glass-Ionomer Cement and Adhesives to Silver Diamine Fluoride-treated Dentin, An Updated Systematic Review and Meta-Analysis. J. Adhes. Dent. 2022, 24, 29–38. [Google Scholar]
- Fung, M.H.T.; Duangthip, D.; Wong, M.C.M.; Lo, E.C.M.; Chu, C.H. Randomized Clinical Trial of 12% and 38% Silver Diamine Fluoride Treatment. J. Dent. Res. 2017, 97, 171–178. [Google Scholar] [CrossRef]
- Gupta, J.; Thomas, M.S.; Radhakrishna, M.; Srikant, N.; Ginjupalli, K. Effect of silver diamine fluoride-potassium iodide and 2% chlorhexidine gluconate cavity cleansers on the bond strength and microleakage of resin-modified glass ionomer cement. J. Conserv. Dent. 2019, 22, 201–206. [Google Scholar]
- Hamama, H.H.; Burrow, M.F.; Yiu, C. Effect of dentine conditioning on adhesion of resin-modified glass ionomer adhesives. Aust. Dent. J. 2014, 59, 193–200. [Google Scholar] [CrossRef]
- Pedersen, M.T.; Tian, K.V.; Dobó-Nagy, C.; Chass, G.A.; Neville Greaves, G.; Yue, Y. Phase separation in an ionomer glass: Insight from calorimetry and phase transition. J. Non Cryst. Soli. 2015, 415, 24–29. [Google Scholar] [CrossRef]
- Tian, K.V.; Chass, G.A.; Di Tommaso, D. Simulations reveal the role of composition into the atomic-level flexibility of bioactive glass cements. Phys. Chem. Chem. Phys. 2016, 18, 837–845. [Google Scholar] [CrossRef]
- Kumari, P.D.; Khijmatgar, S.; Chowdhury, A.; Lynch, E.; Chowdhury, C.R. Factors influencing fluoride release in atraumatic restorative treatment (ART) materials: A review. J. Oral Biol. Craniofac. Res. 2019, 9, 315–320. [Google Scholar] [CrossRef]
- Bahsi, E.; Sagmak, S.; Dayi, B.; Cellik, O.; Akkus, Z. The evaluation of microleakage and fluoride release of different types of glass ionomer cements. Niger. J. Clin. Pract. 2019, 22, 961–970. [Google Scholar] [CrossRef]
- Najeeb, S.; Khurshid, Z.; Zafar, M.; Khan, A.; Zohaib, S.; Martí, J.M.N.; Sauro, S.; Matinlinna, J.P.; Rehman, I.U. Modifications in Glass Ionomer Cements: Nano-Sized Fillers and Bioactive Nanoceramics. Int. J. Mol. Sci. 2016, 17, 1134. [Google Scholar] [CrossRef]
- Horst, J.A.; Ellenikiotis, H.; Milgrom, P.L. UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale.; Indications and Consent. J. Calif. Dent. Assoc. 2016, 44, 16–28. [Google Scholar]
- Zhao, I.S.; Gao, S.S.; Hiraishi, N.; Burrow, M.F.; Duangthip, D.; Mei, M.L.; Lo, E.C.M.; Chu, C.H. Mechanisms of silver diamine fluoride on arresting caries: A literature review. Int. Dent. J. 2018, 68, 67–76. [Google Scholar] [CrossRef]
- Crystal, Y.O.; Niederman, R. Evidence-Based Dentistry Update on Silver Diamine Fluoride. Dent. Clin. N. Am. 2019, 63, 45–68. [Google Scholar] [CrossRef]
- Jiang, M.; Mei, M.L.; Wong, M.C.M.; Chu, C.H.; Lo, E.C.M. Effect of silver diamine fluoride solution application on the bond strength of dentine to adhesives and to glass ionomer cements: A systematic review. BMC Oral Health 2020, 20, 40. [Google Scholar] [CrossRef]
- Tüzüner, T.; Dimkov, A.; Nicholson, J.W. The effect of antimicrobial additives on the properties of dental glass-ionomer cements: A review. Acta Biomater. Odontol. Scand. 2019, 5, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Bjørndal, L.; Simon, S.; Tomson, P.L.; Duncan, H.F. Management of deep caries and the exposed pulp. Int. Endod. J. 2019, 52, 949–973. [Google Scholar] [CrossRef] [PubMed]
- Oliva, A.; della Ragione, F.; Salerno, A.; Riccio, V.; Tartaro, G.; Cozzolino, A.; D'amato, S.; Pontoni, G.; Zappia, V. Biocompatibility studies on glass ionomer cements by primary cultures of human osteoblasts. Biomaterials 1996, 17, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Tanumiharja, M.; Burrow, M.F.; Tyas, M.J. Microtensile bond strengths of glass ionomer (polyalkenoate) cements to dentine using four conditioners. J. Dent. 2000, 28, 361–366. [Google Scholar] [CrossRef]
- Soares, C.J.; Celiberto, L.; Dechichi, P.; Fonseca, R.B.; Martins, L.R. Marginal integrity and microleakage of direct and indirect composite inlays: SEM and stereomicroscopic evaluation. Braz. Oral Res. 2005, 7, 295–301. [Google Scholar] [CrossRef]
- Pontes, D.G.; Guedes-Neto, M.V.; Cabral, M.F.; Cohen-Carneiro, F. Microleakage evaluation of class V restorations with conventional and resin-modified glass ionomer cements. Oral Health Dent. Manag. 2014, 13, 642–646. [Google Scholar]
- Soubhagya, M.; Goud, K.M.; Deepak, B.S.; Thakur, S.; Nandini, T.N.; Arun, J. Comparative in vitro evaluation of internal adaptation of resin-modified glass ionomer.; flowable composite and bonding agent applied as a liner under composite restoration: A scanning electron microscope study. J. Int. Oral Health 2015, 7, 27–31. [Google Scholar]
- Tanumiharja, M.; Burrow, M.F.; Cimmino, A.; Tyas, M.J. The evaluation of four conditioners for glass ionomer cements using field-emission scanning electron microscopy. J. Dent. 2001, 29, 131–138. [Google Scholar] [CrossRef]
- Zhao, I.S.; Chu, S.; Yu, O.Y.; Mei, M.L.; Chu, C.H.; Lo, E.C.M. Effect of silver diamine fluoride and potassium iodide on shear bond strength of glass ionomer cements to caries-affected dentine. Int. Dent. J. 2019, 69, 341–347. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).