Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons
Abstract
Featured Application
Abstract
1. Introduction
2. Exoskeletons as 3D-Printed Medical Devices
3. Own Studies
- An exoskeleton is a robot for people with deficit(s) that actively supports the user’s movement and must:
- Be adapted to the dimensions of the supported body parts, as well as the kind and level of deficit(s), therapy goals, and functional assessment of the user;
- Read the user’s intent;
- Include built-in appropriate sensors and effectors;
- Have a control system;
- Have a power source;
- Incorporate a fail-safe shutdown system.
- An exoskeleton is not implanted and does not affect the user’s skin, so the requirements in this area are mild;
- An exoskeleton contains moving parts that wear out during operation, necessitating replacement;
- Except for some temporary use by debilitated patients during their recovery, an exoskeleton is intended for permanent use. Therefore, an exoskeleton must:
- Grow with the user;
- Be modified in accordance with changes in the user’s health (improvement or deterioration);
- Support an aging user with neurodegenerative changes, as such changes affect the exoskeleton control system.
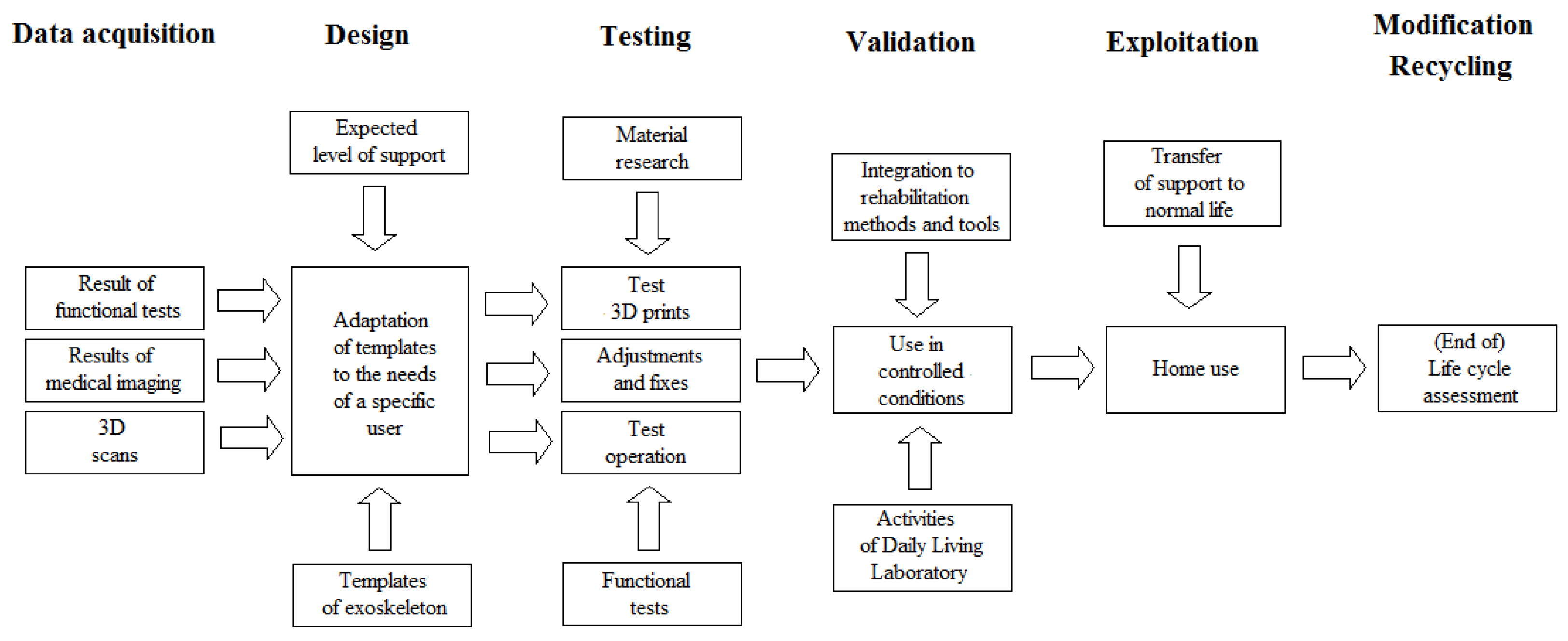
3.1. Planning and Production Cycle
- Stage 1: Data collection based on combined indications for exoskeleton use, functional diagnosis, the results of diagnostic imaging, and 3D scans of the part of the patient’s body on which the exoskeleton is to be fitted. Digitization of this stage eliminates the need for additional, often manual measurements of the user and the impact of the associated inaccuracy/uncertainty;
- Stage 2: Design based on pre-programmed exoskeleton templates in Computer Assisted Design (CAD) software, taking into account the results of the analyses from Stage 1 and the therapy goals derived from the rehabilitation plan and the patient’s priorities (patient-centered therapy);
- Stage 3: Testing, using the results of materials research and optimization (including artificial intelligence-based optimization) of the selected materials and their characteristics (lightness, strength, direction of action, and chemical properties) to produce 3D test prints, followed by operational testing and functional testing of the patient in the exoskeleton to check the optimum fit of the exoskeleton to the user;
- Stage 4: Validation, involving testing the use of the exoskeleton by the user under the controlled conditions of the Activities of Daily Living Laboratory. Here, under the supervision of specialists, the user performs all the activities envisaged for later use at home, including those resulting from the rehabilitation plan, hence the need to integrate the exoskeleton with rehabilitation methods and tools. At this stage, the final adjustments of the exoskeleton are made before it is issued to the user;
- Stage 5: Exploitation, covering the normal use of the exoskeleton at home (if necessary, adjustments are also made for hospital or outpatient settings), monitoring its wear, and providing technical support and modernization as needed—e.g., due to wear or damage to the exoskeleton, changes in the user’s health, launching a new version on the market, or better supporting the user;
- Stage 6: Modification and recycling, including significant changes to the mechanical parts and software of the exoskeleton. This process goes beyond servicing to replacement and recycling of the unit as part of the Life Cycle Assessment, as well as monitoring and the implementation of conclusions from the above analyses for the planning and production cycle of the exoskeleton (e.g., considering the fastest wearing elements or necessary structural changes).
3.2. Support of the User Movement
3.3. Selection of Materials for the Exoskeleton
- Three-dimensional printing technology using stereolithography (SLA), selective laser sintering (SLS), and fused-deposition modeling (FDM) has the greatest potential for printing medical devices);
- The possibility of optimizing the material’s parameters and consumption;
- Planned clinical use, including in exoskeletons, orthoses, prostheses, implants, other devices facilitating rehabilitation and care, anatomical models for learning and preoperative planning, dressings, drugs, tissues and organs, and future personalized electronic systems for neuroprostheses and brain–computer interfaces.
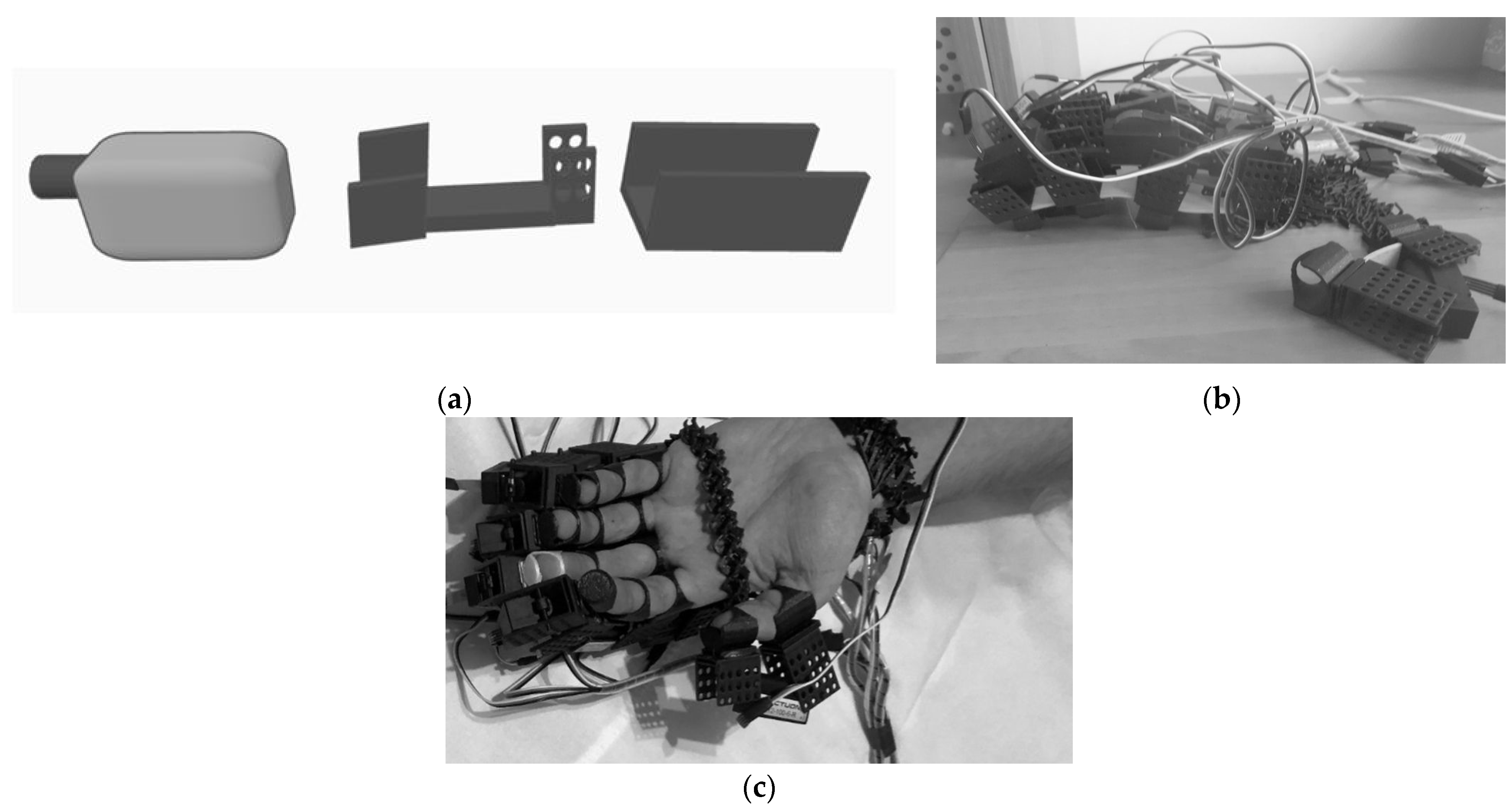
3.4. Design of the Exoskeleton
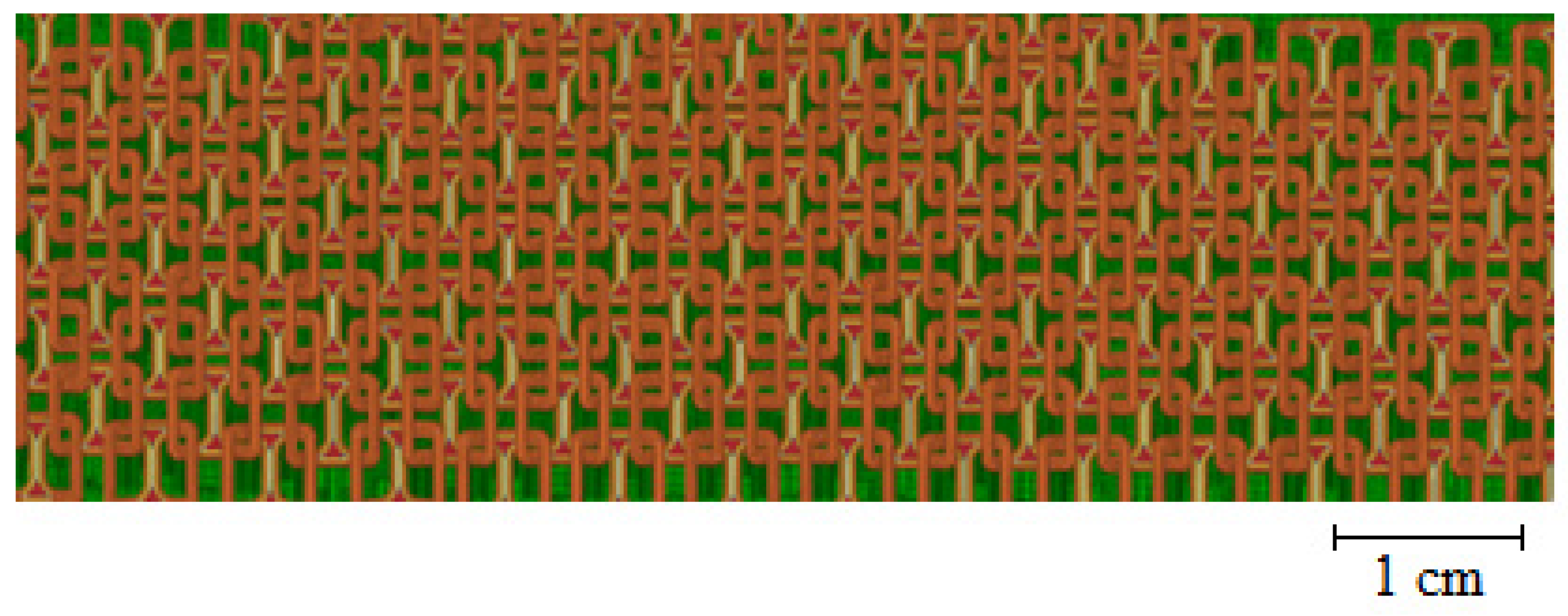
- Chainmail dimensions;
- Separate maximum bending angles in both directions;
- Maximum tensile force;
- Materials;
- Number of layers;
- Shape of the chainmail elements.
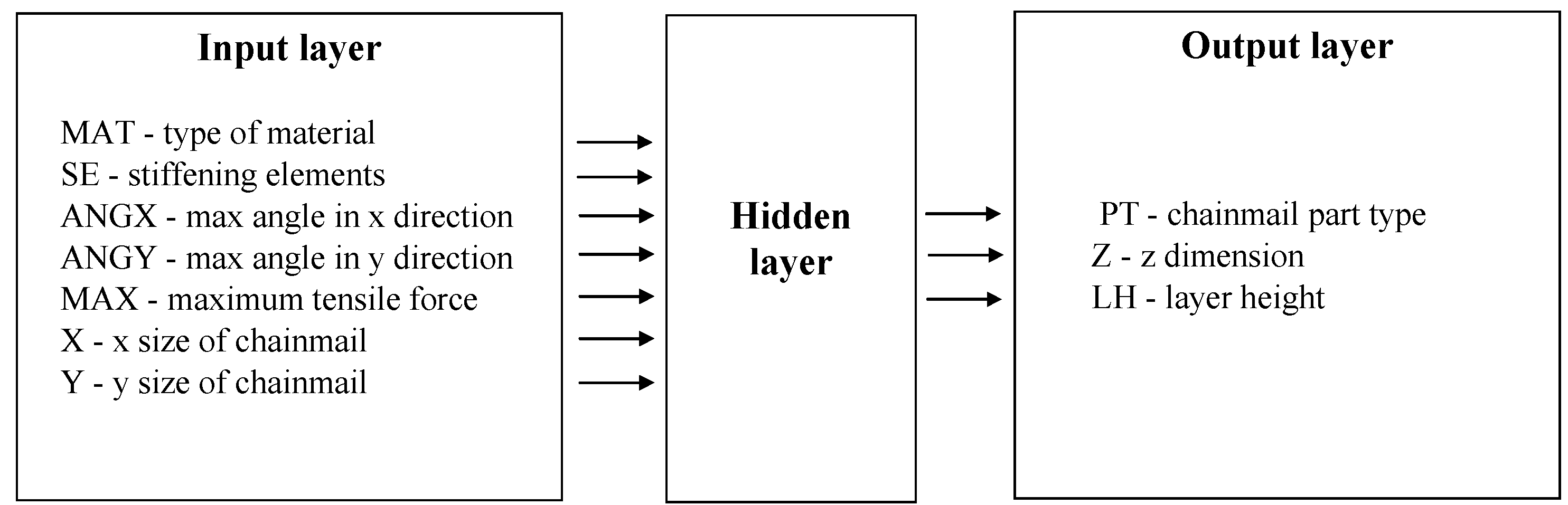
- Determining the required parameters of the chainmail (as part of a personalized therapy for an individually designed exoskeleton);
- The creation of a computational model for chainmail through the use of proprietary software based on artificial intelligence allowing for an optimal description of the chainmail parameters. This software automatically takes into account the inaccuracy resulting from the imbalance between the shape and dimensions of individual chainmail elements and the same parameters for the entire chainmail consisting of many such elements;
- Selecting the values of the parameters for the printing process, selected on the basis of the recommendations from manufacturers of materials and printers, previous research and scientific publications, and the experience of team members;
- Three-dimensional printing and cleaning;
3.5. MDR Directive and ISO 13485, ISO 10993 Standards
3.6. Intellectual Property Rules
3.7. Product or Service Dilemma
4. Discussion
4.1. Findings and Their Implications
4.2. Limitations of the Own Studies
4.3. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beitler, B.G.; Abraham, P.F.; Glennon, A.R.; Tommasini, S.M.; Lattanza, L.L.; Morris, J.M.; Wiznia, D.H. Interpretation of regulatory factors for 3D printing at hospitals and medical centers, or at the point of care. 3D Print. Med. 2022, 8, 7. [Google Scholar] [CrossRef]
- Benady, A.; Gortzak, Y.; Sofer, S.; Ran, Y.; Rumack, N.; Elias, A.; Efrima, B.; Golden, E.; Segal, O.; Merose, O.; et al. Internal Hemipelvectomy for primary bone sarcomas using intraoperative patient specific instruments- the next step in limb salvage concept. BMC Musculoskelet. Disord. 2022, 23, 1012. [Google Scholar] [CrossRef]
- García, R.I.; Jauregui, I.; Del Amo, C.; Gandiaga, A.; Rodriguez, O.; Margallo, L.; Voces, R.; Martin, N.; Gallego, I.; Minguez, R.; et al. Implementation of an In-House 3D Manufacturing Unit in a Public Hospital’s Radiology Department. Healthcare 2022, 10, 1791. [Google Scholar] [CrossRef]
- Beitler, B.; Roytman, G.R.; Parmer, G.; Tommasini, S.M.; Wiznia, D.H. Evaluating surface coatings to reduce bone cement adhesion to point of care 3D printed molds in the intraoperative setting. 3D Print. Med. 2022, 8, 28. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.J.; Kashlan, K.N.; Flanangan, C.L.; Wright, J.K.; Green, G.E.; Hollister, S.J.; Weatherwax, K.J. Regulatory Considerations in the Design and Manufacturing of ImplanTable 3D-Printed Medical Devices. Clin. Transl. Sci. 2015, 8, 594–600. [Google Scholar] [CrossRef]
- Willemsen, K.; Nizak, R.; Noordmans, H.J.; Castelein, R.M.; Weinans, H.; Kruyt, M.C. Challenges in the design and regulatory approval of 3D-printed surgical implants: A two-case series. Lancet Digit. Health 2019, 1, e163–e171. [Google Scholar] [CrossRef]
- Ramaraju, H.; Landry, A.M.; Sashidharan, S.; Shetty, A.; Crotts, S.J.; Maher, K.O.; Goudy, S.L.; Hollister, S.J. Clinical grade manufacture of 3D printed patient specific biodegradable devices for pediatric airway support. Biomaterials 2022, 289, 121702. [Google Scholar] [CrossRef]
- Rahman, Z.; Barakh Ali, S.F.; Ozkan, T.; Charoo, N.A.; Reddy, I.K.; Khan, M.A. Additive Manufacturing with 3D Printing: Progress from Bench to Bedside. AAPS J. 2018, 20, 101. [Google Scholar] [CrossRef]
- Beer, N.; Hegger, I.; Kaae, S.; De Bruin, M.L.; Genina, N.; Alves, T.L.; Hoebert, J.; Kälvemark Sporrong, S. Scenarios for 3D printing of personalized medicines—A case study. Explor. Res. Clin. Soc. Pharm. 2021, 4, 100073. [Google Scholar] [CrossRef]
- Czyżewski, W.; Jachimczyk, J.; Hoffman, Z.; Szymoniuk, M.; Litak, J.; Maciejewski, M.; Kura, K.; Rola, R.; Torres, K. Low-Cost Cranioplasty—A Systematic Review of 3D Printing in Medicine. Materials 2022, 15, 4731. [Google Scholar] [CrossRef]
- Ballardini, R.M.; Mimler, M.; Minssen, T.; Salmi, M. 3D Printing, Intellectual Property Rights and Medical Emergencies: In Search of New Flexibilities. IIC—Int. Rev. Intellect. Prop. Compet. Law 2022, 53, 1149–1173. [Google Scholar] [CrossRef]
- Fogarasi, M.; Coburn, J.C.; Ripley, B. Algorithms used in medical image segmentation for 3D printing and how to understand and quantify their performance. 3D Print. Med. 2022, 8, 18. [Google Scholar] [CrossRef] [PubMed]
- Christensen, A.; Rybicki, F.J. Maintaining safety and efficacy for 3D printing in medicine. 3D Print. Med. 2017, 3, 1. [Google Scholar] [CrossRef]
- Fan, Z.; Xie, N. Analysis of Technical Evaluation for Current Regulation of 3D Printed Customized Medical Device. Chin. J. Med. Instrum. 2018, 42, 279–281. [Google Scholar] [CrossRef]
- Di Prima, M.; Coburn, J.; Hwang, D.; Kelly, J.; Khairuzzaman, A.; Ricles, L. Additively manufactured medical products—The FDA perspective. 3D Print. Med. 2016, 2, 1. [Google Scholar] [CrossRef]
- Otero, J.J.; Vijverman, A.; Mommaerts, M.Y. Use of fused deposit modeling for additive manufacturing in hospital facilities: European certification directives. J. Craniomaxillofac. Surg. 2017, 45, 1542–1546. [Google Scholar] [CrossRef]
- Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32017R0745 (accessed on 17 December 2022).
- ISO 13485:2016; Quality Management Systems. International Organization for Standardization: Geneva, Switzerland, 2016. Available online: https://www.iso.org/standard/59752.html (accessed on 17 December 2022).
- ISO 10993-1:2018; Biological Evaluation of Medical Devices. International Organization for Standardization: Geneva, Switzerland, 2018. Available online: https://www.iso.org/standard/68936.html (accessed on 17 December 2022).
- Marew, T.; Birhanu, G. Three dimensional printed nanostructure biomaterials for bone tissue engineering. Regen. Ther. 2021, 18, 102–111. [Google Scholar] [CrossRef]
- Kruppa, C.; Benner, S.; Brinkemper, A.; Aach, M.; Reimertz, C.; Schildhauer, T.A. Neue Technologien und Robotik [New technologies and robotics]. Unfallchirurgie 2022, 126, 9–18. [Google Scholar] [CrossRef]
- Kataria, S.; Ravindran, V. Musculoskeletal care—At the confluence of data science, sensors, engineering, and computation. BMC Musculoskelet. Disord. 2022, 23, 169. [Google Scholar] [CrossRef]
- Yoo, H.J.; Lee, S.; Kim, J.; Park, C.; Lee, B. Development of 3D-printed myoelectric hand orthosis for patients with spinal cord injury. J. Neuroeng. Rehabil. 2019, 16, 162. [Google Scholar] [CrossRef]
- Ou, Y.K.; Wang, Y.L.; Chang, H.C.; Chen, C.C. Design and Development of a Wearable Exoskeleton System for Stroke Rehabilitation. Healthcare 2020, 8, 18. [Google Scholar] [CrossRef]
- Dudkowiak, A.; Dostatni, E.; Rojek, I.; Mikołajewski, D. The Environmental Analysis of a Product Manufactured with the Use of an Additive Technology. In Advances in Manufacturing III: Production Engineering: Research and Technology Innovations, Industry 4.0; Trojanowska, J., Kujawińska, A., Machado, J., Pavlenko, I., Eds.; Lecture Notes in Mechanical Engineering; Springer: Cham, Switzerland, 2022; Volume 2, pp. 76–89. ISSN 2195-4356. [Google Scholar]
- Rojek, I.; Mikołajewski, D.; Dostatni, E.; Macko, M. AI-Optimized Technological Aspects of the Material Used in 3D Printing Processes for Selected Medical Applications. Materials 2020, 13, 5437. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Kotlarz, P.; Tyburek, K.; Kopowski, J.; Dostatni, E. Traditional Artificial Neural Networks versus Deep Learning in Optimization of Material Aspects of 3D Printing. Materials 2021, 14, 7625. [Google Scholar] [CrossRef] [PubMed]
- Rojek, I.; Mikołajewski, D.; Kopowski, J.; Kotlarz, P.; Piechowiak, M.; Dostatni, E. Reducing Waste in 3D Printing Using a Neural Network Based on an Own Elbow Exoskeleton. Materials 2021, 14, 5074. [Google Scholar] [CrossRef] [PubMed]
- Kopowski, J.; Mikołajewski, D.; Kotlarz, P.; Dostatni, E.; Rojek, I. A Semi-Automated 3D-Printed Chainmail Design Algorithm with Preprogrammed Directional Functions for Hand Exoskeleton. Appl. Sci. 2022, 12, 5007. [Google Scholar] [CrossRef]
- Rojek, I.; Kopowski, J.; Kotlarz, P.; Dorożyński, J.; Dostatni, E.; Mikołajewski, D. Deep Learning in Design of Semi-Automated 3D Printed Chainmail with Pre-Programmed Directional Functions for Hand Exoskeleton. Appl. Sci. 2022, 12, 8106. [Google Scholar] [CrossRef]
- Li, N.; Yang, T.; Yu, P.; Chang, J.; Zhao, L.; Zhao, X.; Elhajj, I.H.; Xi, N.; Liu, L. Bio-inspired upper limb soft exoskeleton to reduce stroke-induced complications. Bioinspir. Biomim. 2018, 13, 066001. [Google Scholar] [CrossRef]
- Cui, L.; Phan, A.; Allison, G. Design and fabrication of a three dimensional printable non-assembly articulated hand exoskeleton for rehabilitation. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4627–4630. [Google Scholar] [CrossRef]
- Rojek, I.; Kowal, M.; Stoic, A. Predictive compensation of thermal deformations of ball screws in CNC machines using neural networks. Teh. Vjesn. 2017, 24, 1697–1703. Available online: https://hrcak.srce.hr/file/280258 (accessed on 12 November 2022).
- Rojek, I. Models for Better Environmental Intelligent Management within Water Supply System. Water Resour. Manag. 2014, 28, 3875–3890. [Google Scholar] [CrossRef]
- Rojek, I. Classifier models in intelligent CAPP systems. In Man-Machine Interactions; Cyran, K.A., Kozielski, S., Peters, J.F., Stanczyk, U., Wakulicz-Deja, A., Eds.; Advances in Intelligent and Soft Computing; Springer: Berlin/Heidelberg, Germany, 2009; pp. 311–319. [Google Scholar] [CrossRef]
- Rojek, I. Neural Networks as Prediction Models for Water Intake in Water Supply System. In Artificial Intelligence and Soft Computing—ICAISC 2008, Proceedings of the 9th International Conference, Zakopane, Poland, 22–26 June 2008; Rutkowski, L., Tadeusiewicz, R., Zadeh, L.A., Zurada, J.M., Eds.; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2008; Volume 5097, pp. 1109–1119. [Google Scholar] [CrossRef]
- Kawala-Janik, A.; Bauer, W.; Zolubak, M.; Baranowski, J. Early-stage pilot study on using fractional-order calculus-based filtering for the purpose of analysis of electroencephalography signals. Stud. Log. Gramm. Rhetor. 2016, 47, 103–111. [Google Scholar] [CrossRef]
- Baranowski, J.; Bauer, W.; Zagórowska, M.; Kawala-Janik, A.; Dziwiński, T.; Piątek, P. Adaptive non-integer controller forwater tank system. In Theoretical Developments and Applications of Non-Integer Order Systems; Lecture Notes in Electrical Engineering; Springer: Cham, Switzerland, 2016; Volume 357, pp. 271–280. [Google Scholar]
- Keeling, A.B.; Piitz, M.; Semrau, J.A.; Hill, M.D.; Scott, S.H.; Dukelow, S.P. Robot enhanced stroke therapy optimizes rehabilitation (RESTORE): A pilot study. J. Neuroeng. Rehabil. 2021, 18, 10. [Google Scholar] [CrossRef]
- Shi, K.; Mu, F.; Huang, R.; Huang, K.; Peng, Z.; Zou, C.; Yang, X.; Cheng, H. Multimodal Human-Exoskeleton Interface for Lower Limb Movement Prediction Through a Dense Co-Attention Symmetric Mechanism. Front. Neurosci. 2022, 16, 796290. [Google Scholar] [CrossRef]
- Gerardin, E.; Bontemps, D.; Babuin, N.T.; Herman, B.; Denis, A.; Bihin, B.; Regnier, M.; Leeuwerck, M.; Deltombe, T.; Riga, A.; et al. Bimanual motor skill learning with robotics in chronic stroke: Comparison between minimally impaired and moderately impaired patients, and healthy individuals. J. Neuroeng. Rehabil. 2022, 19, 28. [Google Scholar] [CrossRef]
- Shahid, T.; Gouwanda, D.; Nurzaman, S.G.; Gopalai, A.A. Moving toward Soft Robotics: A Decade Review of the Design of Hand Exoskeletons. Biomimetics 2018, 3, 17. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojek, I.; Mikołajewski, D.; Dostatni, E.; Kopowski, J. Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons. Appl. Sci. 2023, 13, 1060. https://doi.org/10.3390/app13021060
Rojek I, Mikołajewski D, Dostatni E, Kopowski J. Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons. Applied Sciences. 2023; 13(2):1060. https://doi.org/10.3390/app13021060
Chicago/Turabian StyleRojek, Izabela, Dariusz Mikołajewski, Ewa Dostatni, and Jakub Kopowski. 2023. "Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons" Applied Sciences 13, no. 2: 1060. https://doi.org/10.3390/app13021060
APA StyleRojek, I., Mikołajewski, D., Dostatni, E., & Kopowski, J. (2023). Specificity of 3D Printing and AI-Based Optimization of Medical Devices Using the Example of a Group of Exoskeletons. Applied Sciences, 13(2), 1060. https://doi.org/10.3390/app13021060







