Abstract
Introduction: This retrospective study aimed to determine skeletal and dental changes after a growth spurt and shortly after treatment using a facemask in skeletal Class III malocclusion with maxillary deficiency. Methods: We retrospectively studied 50 patients (25 patients per group) with skeletal Class III malocclusion who underwent facemask treatment with tooth-anchored (T-A, mean age 7.92) and miniscrew-anchored (M-A, mean age 9.84) intraoral appliances. In both groups, the facemask applied a traction force of 350–400 g to each side, such that the traction was directed 30° forward and downward. Lateral cephalometric radiographs were obtained from all patients before (T1), immediately after (T2), and at an average of 37.11 months after maxillary protraction (T3). A total of 13 cephalometric measurements were analyzed to determine the skeletal and dental changes. A paired t-test was used to verify the effects before, after, and during follow-up periods in each group. Results: An anteroposterior relationship, the values of SNA and ANB, evident in both groups at T2, was significantly improved in the M-A group (p < 0.05). However, the values of ANB and MP–SN, which indicate the relapse of anteroposterior and vertical relation of maxilla and mandible, were significantly higher in the T-A group compared with the M-A group during follow-up period. The maxillary first molars were significantly more extruded and maxillary incisors were more protruded in the T-A group than the M-A group, and this persisted at T3 (p < 0.05). Conclusions: Miniscrew-anchored maxillary protraction increased the skeletal improvement of anteroposterior relationship and reduced the dental and skeletal relapses compared with tooth-anchored maxillary protraction in growing patients with a hyperdivergent patterns and skeletal Class III malocclusion.
1. Introduction
Skeletal Class III malocclusion is strongly affected by genetic and ethnic factors as well as environmental factors. Skeletal Class III malocclusion can occur from deficient maxilla, excessive mandible, and a combination of both. The prevalence is about 4–14% in East Asians, including Chinese, Japanese, and Koreans, and the frequency of maxillary deficiency is high [1,2,3]. A facemask is a common treatment modality for skeletal Class III malocclusion in patients with maxillary hypoplasia [4,5,6]. Orthopedic treatment using an extraoral facemask applies forward and downward forces on the maxilla. This protracts the maxilla after separating the maxillary tubercle posterior–superior suture [7] while limiting forward growth in the mandible and changing the direction of growth via clockwise rotation. Because force is indirectly transferred to the maxilla through a tooth-anchored appliance, undesirable changes in the maxillary teeth can reduce the effect of maxillary advancement [8]. Various methods have been proposed to reduce odontogenic side effects by directly applying force to bone using skeletal anchorage [9,10,11]. Miniplates have been positioned [9] in the maxillary buttress and anterior mandibular chin or on the infrazygomatic crest using various means to avoid influencing dentition development [10,11]. However, these methods have disadvantages, such as a need for additional surgery and the possibility of loosening. Several approaches have been introduced to overcome these limitations, such as intraoral devices with reinforced skeletal anchorage devices on the palatal side that can be easily positioned under local anesthesia [12,13]. These reports describe the effects of palatal-reinforced skeletal anchorage devices, facemasks, and intraoral devices such as mini-implant or miniscrew-assisted rapid palatal expander (MARPE). A forward movement of the maxilla is significantly more associated with bone-anchored than with tooth-anchored devices, which limits dentoalveolar bone effects [14]. Bone-anchored devices can reduce negative side effects such as a lingual inclination of the maxillary anterior teeth and maxillary molar extrusion, while directly delivering orthodontic forces to the maxillary complex [15]. Nevertheless, the effects of an orthodontic treatment of a skeletal Class III malocclusion might not be maintained during the subsequent growth spurt of the mandible. Therefore, long-term studies are needed to evaluate the effectiveness of such treatment. Lee et al.’s study has found that the long-term results are more sustainable for miniplates than tooth-anchored devices [16]. However, there has been no study using palatal miniscrew-anchored devices, and the long-term effects of miniscrew-anchored devices have not been compared. In this study, we aimed to scrutinize skeletal and dental changes in growing Class III patients before and after treatment, as well as during the follow-up period, utilizing a maxillary protraction facemask anchored by teeth and miniscrews. The null hypothesis for this study could be formulated as follows: there is no significant difference in skeletal and dental measurements before and after treatment, as well as during the follow-up period, in growing Class III patients treated with a maxillary protraction facemask anchored by teeth and miniscrews.
2. Materials and Methods
The Institutional Review Board of Pusan National University Dental Hospital approved this study (PNUDH-2022-03-011). The sample size was calculated as described [15]. Here, we compared the results of treating mild skeletal Class III malocclusion in pediatric patients using a facemask and a tooth (FM)- or a miniscrew (FM + MS)-anchored appliance. The angle formed by the intersection of sella-nasion and nasion-A lines (SNA) was significantly increased in the FM + MS, compared with the FM group (2.2° ± 1.3° vs. 1.1° ± 1.0°, p < 0.01). A study power of 90% was assumed; significance level was 5%. The calculation of sample size was based on the previous study using the G*power software 3.1.9.7 (Universität Düsseldorf, Düsseldorf, Germany) [8]. They investigated the treatment outcomes of mild skeletal Class III malocclusion between FM and FM in combination with a miniscrew for anchorage (FM + MS) in growing patients. The SNA values were significantly higher in the FM + MS group than that in the FM group (FM; 1.1 ± 1.0°, FM + MS; 2.2 ± 1.3°). The sample size was calculated based on an alpha significance level of 0.05 and 90% power to detect an effect size of 0.948 between measurements. The power analysis showed that at least 25 patients were needed. Therefore, this retrospective study included 50 patients (28 males and 22 females) who underwent orthodontic treatment at the Department of Orthodontics at the Pusan National University Dental Hospital from 2013 to 2017. During the retrospective study period (2013–2017), patients presenting in the early years were treated primarily with tooth-anchored devices, while patients presenting in the later years were treated primarily with miniscrew-anchored as MSE devices became more widely available. All patients satisfied the following inclusion criteria:
- Skeletal Class III malocclusion (relative anteroposterior position between the maxilla and mandible (ANB) <2°) measured on initial lateral cephalograms and evaluator.
- Anterior cross (including edge-to-edge) bite.
- Cervical vertebral maturation stages (CVMS) I–III.
- No craniofacial malformations or systemic disease.
- No temporomandibular joint disorder (TMD).
- No history of orthodontic treatment.
The patients (n = 25 per group) in the group with tooth-anchored (T-A) devices comprised 9 males and 16 females (mean age, 7.9 years) and those in the miniscrew-anchored (M-A) group comprised 11 males and 14 females (mean age, 9.9 years). Lateral cephalometric radiographs were obtained from all patients before (T1), immediately after (T2), and during follow-up periods, at an average of 37.11 months (standard deviation (SD), 16.74) after maxillary protraction (T3).
2.1. Treatment
A bonded or banded rapid plate expander (RPE) was placed in the middle of the palate in the T-A group; then, a stainless steel wire (0.9 mm) was bent on the buccal side as a petit facemask protraction hook (Figure 1a). Fixation was established in the M-A group using a commercial Maxillary Skeletal Expander (MSE) type 2 (BMK, Seoul, Republic of Korea) and two miniscrews (diameter and length: 1.8 and 11 mm, respectively) on the palatal side. Miniscrews were implanted into the left and right premolars and midpalatal area at the level of the third palatine torus using the self-tapping method under infiltration anesthesia. A stainless steel wire (0.9 mm) was soldered to the buccal side of the hook for protraction to connect the petit facemask and the extraoral rubber band (Figure 1b,c).
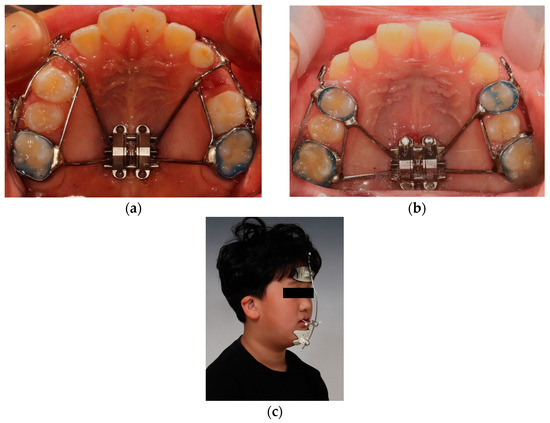
Figure 1.
(a) Conventional rapid palatal expansion (RPE) with traction hook. (b) Miniscrew-assisted rapid palatal expansion (MARPE) with traction hook. Two miniscrews were inserted on anterior palate. (c) Petit-type facemask.
The petit facemask applied a traction force of 350–400 g to each side such that the traction was directed 30° forward and downward (Figure 1c). The application point minimized the counterclockwise rotation of the maxilla by reducing the distance between the action line of the force and the center of maxillary resistance, by positioning the front towing ring as far upward as possible. The patients were instructed to wear the device for at least 14 h each day. Maxillary protraction was continued until a positive overjet formed.
2.2. Lateral Cephalometric Analysis
One examiner (BJC) measured all cephalometric parameters using V-Ceph v. 8.0 software (V-Ceph, Osstem, Seoul, Republic of Korea). We measured nine angular and four linear items to determine skeletal and dental changes immediately after maxillary protraction and again after a growth spurt. Table 1 and Figure 2 show definitions and explanations of the vertical and horizontal distances and angles that were measured using reference points and planes.

Table 1.
Measurement details.
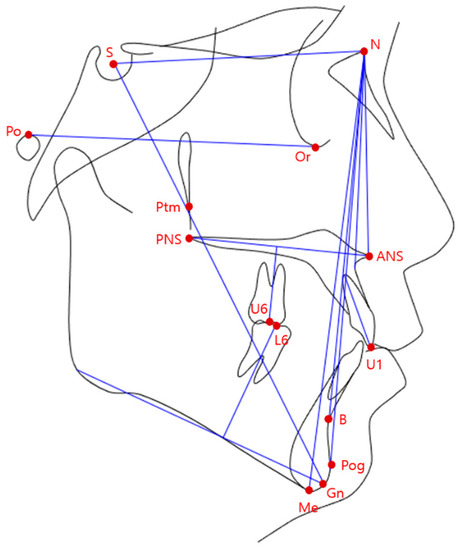
Figure 2.
Reference points and planes.
2.3. Statistical Analysis
The examiner (BJC) measured the points on the lateral cephalometric radiographs once and again two weeks later. The measurements taken twice were analyzed with a paired t-test, with a p-value greater than 0.05 indicating no significant difference between the measurements. Averaged values were analyzed. All 13 measured values assessed using Shapiro–Wilk tests followed by a normal distribution. Homogeneity was verified for the total duration of treatment (T1–T3), including the chronological ages at T1 and T3 in both groups, cervical vertebral maturation stage (CVMS), maxillary protraction period (T1–T2), and follow-up duration (Table 2). Changes in measured values between the T-A and M-A groups were compared using Student’s t-test during forward traction (T1–T2), follow-up (T2–T3), and throughout the entire study (T1–T3). Skeletal and dental changes at T1, T2, and T3 within each group were confirmed using repeated-measures analysis of variance (ANOVA) with the general linear model, followed by post hoc Bonferroni tests. Statistical significance was defined as p < 0.05. All data were statistically analyzed using SPSS 29.0 (IBM Corp., Armonk, NY, USA).

Table 2.
Comparison of age, CVMS, treatment duration between patients treated using tooth- and miniscrew-anchored devices.
3. Results
Miniscrews were not removed from the M-A group until the end of maxillary traction. The total duration (T1–T3), including chronological age at T3, CVMS stages at T1, and T3, the duration of maxillary protraction (T1–T2), and follow-up, did not significantly differ between the T-A and M-A groups. However, chronological age at T1 was significantly higher in the M-A group (Table 2). The average durations of protraction, when a positive overjet was achieved (T1–T2), were not significantly different between the two groups; in the T-A and M-A groups, they were 9.43 ± 9.51 and 10.59 ± 5.96 months (m), respectively. The follow-up (T1–T3) after the growth spurt from the start of treatment in the T-A and M-A groups were 52.05 ± 20.19 and 42.19 ± 9.09 months, respectively.
The maxillomandibular anteroposterior relationship improved due to anteroposterior skeletal changes in both groups at T2, and that in the M-A group was statistically significant (T-A vs. M-A: SNA, 1.43° vs. 2.07°; ANB, 2.22° vs. 2.88°; T1–T2, p < 0.05). The anteroposterior relationship during follow-up from T2 to T3 relapsed slightly, and the amount of recurrence was significantly greater in the T-A group (ANB, −1.48° vs. −0.37°, p < 0.05). However, both groups maintained a better anteroposterior skeletal relationship during follow-up (T3) than before treatment (T1; T-A vs. M-A: ANB, 0.73° vs. 2.51°; p < 0.05) (Table 3).

Table 3.
Comparison of skeletal and dental measurements between patients with tooth- and miniscrew-anchored devices at pretreatment (T1), posttreatment (T2), and follow-up (T3).
According to the maxillary protraction, the mandible rotated clockwise during treatment (T1–T2), more significantly in the T-A, than in the M-A group (MP–SN: 1.74° vs. 0.53°, p < 0.05). However, this regressed in a counterclockwise direction during follow-up, and the amount of change was significantly greater in the T-A group (MP–SN: −3.98° vs. −2.09°, p < 0.05). The mandibular angle changed in the direction of a decrease due to regression in the counterclockwise direction in both groups after follow-up compared with before treatment. However, the difference between them did not reach statistical significance (T-A vs. M-A; MP–SN, −0.24° vs. −0.97°; p > 0.05) The mandible opened more and the lower face was longer immediately after treatment (T2) in the T-A, than the M-A group (MP–SN: 1.74° vs. 0.53°; N–Me, 3.14 vs. 1.25 mm; T1–T2 p < 0.05; Table 4). This resulted in a significantly greater increase in the length of the lower face in the T-A group even after follow-up (N–Me: 10.24 vs. 7.90 mm, p < 0.05; Table 3).

Table 4.
Comparison of treatment outcomes of tooth-anchored devices during T1, T2, and T3.
The maxillary first molars were immediately and significantly more extruded due to the difference in odontogenic changes between the two groups after treatment in the T-A, than the M-A group (U6/NF: 1.88 vs. 0.49 mm, p < 0.001). A significant amount of extrusion was maintained in the T-A group even until follow-up (U6/NF: 4.56 vs. 2.60 mm, p < 0.001) (Table 3).
The mandibular anterior teeth were linguoverted immediately after treatment (T2) in both groups because of the extraoral facemasks. Linguoversion was significantly greater in the T-A than the M-A group (IMPA: −5.04° vs. −2.61°, p < 0.05). However, this trend recovered during follow-up, and changes from T1 to T3 did not significantly differ between the groups (IMPA: −0.31° vs. 0.53°, p > 0.05; Table 3). Comparisons of changes between before and after treatment (T2) and follow-up (T3) revealed significant changes in SNA, SNB, ANB, N–Me, U6/NF, and MP–SN between these time points in the T-A group. The ANB value significantly increased after treatment and significantly decreased during follow-up, but did not significantly differ between before treatment or after follow-up (ANB: −0.13° vs. 0.60°, p > 0.05; Table 4). All other SNA, SNB, MP–SN, N–Me, and U6/NF items significantly differed among T1, T2, and T3 (p < 0.05; Table 4). Changes in SNA, ANB, MP–SN, N–Me, and U6/NF were significant at the three time points in the M-A group. Unlike the T-A group, the SNB did not significantly change between before treatment and after follow-up. Unlike the T-A group, the ANB value also significantly increased immediately after treatment and during follow-up compared with that before treatment (ANB at T1 vs. T2, vs. T3: −1.30° vs. 1.58° vs. 1.20°, p > 0.001; Table 5).

Table 5.
Comparison of treatment outcomes of miniscrew-anchored device during T1, T2, and T3.
4. Discussion
This longitudinal study aimed to determine short- and long-term skeletal and dental changes associated with maxillary protraction using tooth- and palatal bone-anchored devices in children with a maxillary bone deficiency. Our patients with Class III malocclusions underwent maxillary protraction between the ages of 6 and 10 years and were followed up until they reached the age of 16 years.
The average ages at the start of treatment were 7.92 and 9.84 years in the T-A and M-A groups, respectively. Thus, the T-A group started treatment earlier. This is thought to be attributable to the tendency to select a T-A device for younger patients, considering the maturity of the maxillary suture and the degree of invasiveness of maxillary traction according to age. However, the CVMS did not significantly differ between the groups before treatment, so bone maturation was similar. In addition, age, treatment (T1–T2), and follow-up (T2–T3) did not significantly differ between the groups, which might have affected the treatment outcomes (Table 2).
4.1. Skeletal and Dental Changes during Maxillary Protraction (between T1 and T2)
The maxilla in both groups was immediately protracted after maxillary traction. The mandible rotated in the posteroinferior direction because we used a facemask to apply force to the chin area of the mandible. This increased the degree of improvement in the anterior–posterior relationship between the maxilla and the mandible (Table 3). More anterior maxillary movement was evident in the M-A group because the orthopedic force was directly transmitted to the circummaxillary suture through the miniscrew-anchored appliance. This result was consistent with previous findings. A bone-anchored device delivers twice as much maxillary traction than a tooth-anchored device [15]. The total amount of maxillary traction immediately increases using a bone-anchored device [16,17]. In contrast, one study found no difference in maxillary traction between bone- and tooth-anchored appliances [13]. However, that study found that a bone-anchored device is required to minimize the side effects of tooth movement caused by the forward movement of the posterior and anterior teeth to which the device is anchored [13,18]. The authors considered that this difference was due to using a hyrax-type PRE as a tooth-anchored device and implanting two miniscrews into the third palatal rugae area using the anterior arm of the hybrid hyrax RPE as a bone-anchored device to strengthen the anchorage. To increase the effects of the response to maxillary traction in all patients, the maxilla was widened by 0.5 mm/day for 1 or 2 weeks if narrow, and both groups started treatment at the age of ~9 years.
The present study found that the mandible rotated clockwise, and the lower face lengthened in both groups immediately after maxillary traction using a facemask. The vertical dimension of the lower face increased as the MP–SN value increased due to the clockwise rotation of the mandible, and the increase was significantly greater in the T-A group, which was consistent with previous results (Table 3) [13,19]. We considered that this difference between the groups was due to the significantly greater extrusion of the maxillary first molar in the T-A than the M-A group during maxillary protraction. The maxillary first molars were fixed to the palate with a miniscrew-anchored device, so extrusion rarely occurred in the M-A group. However, the amount of extrusion was significant in the T-A group because the maxillary first molar was not fixed to the palate (Table 3). The vertical dimension of the lower face increased more when a facemask was used with a tooth- than a bone-anchored device [13,14], which was attributed to the extrusion of the maxillary molars [16]. In contrast, maxillary first molars have extruded immediately after facemask treatment using a bone- or a tooth-anchored device [15]. This is because a mini-implant was positioned in front of the lingual arch in the oral device, and anchoring was strengthened only for forward movement. Mini-implant was not included in the device, so vertical extrusive force was not prevented.
A lingual inclination of the mandibular anterior teeth that occurred during maxillary traction was immediately evident after treatment (T2) in both groups in the present study (Table 3).
4.2. Skeletal and Dental Changes between T2 and T3
The period from the end of maxillary traction (T2) until the final follow-up (T3) averaged at 42.62 and 31.6 m in the T-A and M-A groups, respectively. At the time of the final follow-up (T3), the respective average ages of the patients and CVMS stages were 12.12 and 13.34 years and stages VI and V in the T-A and M-A groups, respectively. Most of the final follow-up assessments proceeded after pubertal growth peaked (Table 2). Therefore, skeletal and dental changes occurred due to mandibular growth in both groups, resulting in a recurrence pattern in the skeletal anteroposterior relationship (T-A vs. M-A: SNB, +2.71° vs. +1.66°; ANB, −1.48° vs. −0.37°, p < 0.05; Table 3). Considering the skeletal linguoversion relationship, the recurrence rate was greater in the T-A group. This indicated that the improvement due to the dentoalveolar effect was greater than that of the skeletal improvement immediately after maxillary protraction in this group. As MP–SN decreased during normal growth, a closing phenomenon of the mandible developed with a significantly decreased MP–SN in the T-A vs. the M-A group (−3.98° vs. −2.09°, p < 0.05). This was consistent with the counterclockwise rotation of the mandible after an average of 7 years of follow-up in a previous study (Sn–GoGn: −5°) [20]. These mandibular rotation and position changes were attributed to mandibular residual growth and direction, consistent with previous long-term study [21]. In addition, we confirmed a greater recurrence rate during maxillary protraction because the mandible was more open in the T-A group. Similarly, the pattern of the anteroposterior relationship was more recurrent when a tooth-anchored device served as an intraoral device rather than a miniplate during follow-up after facemask treatment and the mandible was closed (miniplate vs. tooth-anchored appliance: ANB, −1.1° vs. −2.4°; FMA: −1.2° vs. −3.5°; p < 0.05) [16].
The lingual mandibular anterior teeth were tilted labially in both groups during follow-up in the present study due to recurrence. However, the difference did not reach significance (T-A vs. M-A: IMPA +4.72° vs. +3.14°; p > 0.05). Others have also found no significant differences between groups with tooth- and bone-anchored devices in terms of recurrence of the lingual slope of mandibular anterior teeth that relapse during long-term follow-up (bone- vs. tooth-anchored: IMPA, +4.9° vs. +4.7°) [16].
4.3. Overall Skeletal and Dental Changes (T1–T3)
The present findings showed that the amounts of maxillary protraction and of improvements in the maxillomandibular anteroposterior relationship were greater after maxillary protraction using a miniscrew- rather than a tooth-anchored device, even after growth peaked (T-A vs. M-A): SNA, +2.65° vs. +3.29°; ANB, +0.73° vs. +2.51° p < 0.05). These results were consistent with the those of the study described above using a tooth-anchored device vs. a miniplate (SNA +2.7° vs. +3.9°; ANB, +1.4° vs. +3.3°; p < 0.05) [16].
In addition, even after the period of maximum growth (T3), maxillary first molar extrusion was maintained when a tooth-anchored device was used, as was the situation immediately after treatment (T2). This resulted in a large increase in the vertical dimension of the lower face (T-A vs. M-A: U6/NF, +4.56 vs. +2.60 mm; N–Me, +10.24 vs. +7.90 mm, p < 0.05). In contrast, the vertical dimension of the lower face did not significantly differ between groups treated with a tooth-anchored device and a miniplate, which was inconsistent [16]. This might be because we prevented extrusion by directly holding the maxillary first molar in an oral device, whereas the miniplate did not directly prevent such an extrusion. In addition, the difference might have occurred because the average observation period was 6.5 years, which was longer than in our study.
Although there was a trend toward decreased skeletal improvement with facemask treatment during T2–T3, ANB remained within normal range in both groups, with a positive overjet at T3. This may reduce the need for orthognathic surgery in patients with Class III malocclusion, regardless of the type of intraoral device. This is consistent with a previous study by Mandall et al., showing that early facemask treatment reduces the need for orthognathic surgery by one-third compared to no-treatment patients [22].
This study included follow-up starting before and ending at an average of 3.9 years after treatment. We confirmed that the maxillomandibular anteroposterior relationship can be improved even when teeth serve as anchors for maxillary traction. However, better improvement was achieved by bone anchoring, and first molar extrusion could not be avoided. This dentoalveolar effect may have increased the anterior facial vertical dimension after treatment. In light of these, maxillary protraction using a miniscrew-anchored device that connects and fixes the maxillary first molar to the palatal area is more effective for pediatric patients with skeletal Class III malocclusions and a hyperdivergent skeletal pattern during long-term follow-up. This indicates favorable stability.
The design of this study has some limitations. Because this is a retrospective study, experimenter bias may have been involved. In actual clinical practice, when selecting a tooth- or bone-anchored device, orthodontist’s bias may be reflected due to the patient’s cooperation in the process of installing the miniscrew under infiltration anesthesia. Considering these factors, it is unfortunate that the age at treatment initiation (T1) was different between the two groups in this study. In addition, although this study has the advantage of an average follow-up period of 37 months, it is difficult to determine whether mandibular growth is complete in all patients when considering CVMS. Therefore, it is difficult to accurately determine the skeletal and dental difference in facemask treatment between the two groups over a longer period of time until growth is complete. Future studies could support the facemask treatments in growing patients with maxillary deficiency if a study is designed that matches patient age with bone age, CVMS, at the start of treatment, regardless of intraoral device type, and if long-term studies are conducted until mandibular growth is complete. Finally, this study did not include untreated mild skeletal Class III patients as controls; however, it is not ethical to expose control subjects to radiation when control patients are untreated.
5. Conclusions
Compared to tooth-anchored devices, the protraction of maxilla was greater in miniscrew-anchored devices after treatment, and the effect was maintained within an average of 37-month-long follow-up periods, after the peak phase of mandibular growth. However, using tooth-anchored devices, the maxillary first molars were more extruded and the clockwise rotation of the mandible increased the lower facial height, but during the follow-up, the mandible relapsed into counterclockwise rotation, causing the mandible to shift anteriorly. In addition, the extrusion of the maxillary first molars persisted after the follow-up period, resulting in a greater increase in lower facial height with the tooth-anchored device than with the bone-anchored device. Therefore, miniscrew-anchored devices may be a useful tool in the treatment of skeletal Class III malocclusion by increasing the amount of maxillary anterior protraction and reducing the increase in facial height in patients with hyperdivergent vertical patterns and maxillary deficiency.
Author Contributions
Conceptualization, J.-C.B., Y.-K.C. and Y.-I.K.; methodology, J.-C.B., H.H.J., S.-H.K., S.-S.K. and S.-B.P.; formal analysis, J.-C.B., H.H.J., S.-H.K., S.-S.K., S.-B.P., Y.-K.C. and Y.-I.K.; writing—original draft preparation, J.-C.B., Y.-K.C. and Y.-I.K.; writing—review and editing, J.-C.B., H.H.J., S.-H.K., S.-S.K., S.-B.P., Y.-K.C. and Y.-I.K.; funding acquisition, Y.-I.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Research Foundation of Republic of Korea (NRF) grant funded by the Korean government (2021R1A2C1003240).
Institutional Review Board Statement
The Institutional Review Board of Pusan National University Dental Hospital approved this study (PNUDH-2022-03-011).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The authors declare that the materials are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Baik, H.-S.; Kim, K.-H.; Park, Y. The distributions and trends in maloclusion patients-A 10 year study of 2155 patients from YDSH. Korean J. Orthod. 1995, 25, 87–100. [Google Scholar]
- Ishii, H.; Morita, S.; Takeuchi, Y.; Nakamura, S. Treatment effect of combined maxillary protraction and chincap appliance in severe skeletal Class III cases. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Allwright, W.C. A survey of handicapping dentofacial anomalies among Chinese in Hong Kong. Int. Dent. J. 1964, 14, 505–519. [Google Scholar]
- Nanda, R. Biomechanical and clinical considerations of a modified protraction headgear. Am. J. Orthod. 1980, 78, 125–139. [Google Scholar] [CrossRef]
- Roberts, C.A.; Subteiny, J.D. An american board of orthodontics ease report, use of the face mask in the treatment of maxillary skeletal, retrusion. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Delaire, J. Manufacture of the “orthopedic mask”. Revue Stomatol. Chir. Maxillo-Fac. 1971, 72, 579–582. [Google Scholar]
- Nartallo-Turley, P.E.; Turley, P.K. Cephalometric effects of combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998, 68, 217–224. [Google Scholar]
- Kama, J.D.; Baran, S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur. J. Orthod. 2006, 28, 496–502. [Google Scholar] [CrossRef]
- De Clerck, H.J.; Cornelis, M.A.; Cevidanes, L.H.; Heymann, G.C.; Tulloch, C.J. Orthopedic traction of the maxilla with miniplates: A new perspective for treatment of midface deficiency. J. Oral Maxillofac. Surg. 2009, 67, 2123–2129. [Google Scholar] [CrossRef]
- Cha, B.-K.; Lee, N.-K.; Choi, D.-S. Maxillary protraction treatment of skeletal Class III children using miniplate anchorage. Korean J. Orthod. 2007, 37, 73–84. [Google Scholar]
- Cha, B.-K.; Choi, D.-S.; Ngan, P.; Jost-Brinkmann, P.-G.; Kim, S.-M. Maxillary protraction with miniplates providing skeletal anchorage in a growing Class III patient. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 99–112. [Google Scholar] [CrossRef]
- Nienkemper, M.; Wilmes, B.; Pauls, A.; Drescher, D. Maxillary protraction using a hybrid hyrax-facemask combination. Prog. Orthod. 2013, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.; Wilmes, B.; Drescher, D.; Martin, C.; Weaver, B.; Gunel, E. Comparison of two maxillary protraction protocols: Tooth-borne versus bone-anchored protraction facemask treatment. Prog. Orthod. 2015, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Cha, B.-K.; Ngan, P.W. Skeletal anchorage for orthopedic correction of growing class III patients. Semin. Orthod. 2011, 17, 124–137. [Google Scholar] [CrossRef]
- Seiryu, M.; Ida, H.; Mayama, A.; Sasaki, S.; Sasaki, S.; Deguchi, T.; Takano-Yamamoto, T. A comparative assessment of orthodontic treatment outcomes of mild skeletal Class III malocclusion between facemask and facemask in combination with a miniscrew for anchorage in growing patients: A single-center, prospective randomized controlled trial. Angle Orthod. 2020, 90, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.-J.; Choi, D.-S.; Jang, I.; Cha, B.-K. Comparison of facemask therapy effects using skeletal and tooth-borne anchorage: A longitudinal retrospective study. Angle Orthod. 2022, 92, 307–314. [Google Scholar] [CrossRef]
- Choi, Y.-K.; Park, J.-J.; Jeon, H.-R.; Kim, Y.-I. Comparison of the skeletodental effects of miniscrew-anchored and tooth-anchored facemask treatment in growing patients with skeletal class III malocclusions. Orthod. Craniofac. Res. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Chieruzzi, M.; Pagano, S.; De Carolis, C.; Eramo, S.; Kenny, J.M. Scanning Electron Microscopy Evaluation of Dental Root Resorption Associated with Granuloma. Microsc. Microanal. 2015, 21, 1264–1270. [Google Scholar] [CrossRef]
- Kircelli, B.; Pektas, Z. Midfascial protraction with skeletally anchored facemask therapy: A novel approach and preliminary results. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 440–449. [Google Scholar] [CrossRef]
- Maino, G.B.; Cremonini, F.; Maino, G.; Paoletto, E.; De Maio, M.; Spedicato, G.A.; Palone, M.; Lombardo, L. Long-term skeletal and dentoalveolar effects of hybrid rapid maxillary expansion and facemask treatment in growing skeletal Class III patients: A retrospective follow-up study. Prog. Orthod. 2022, 23, 44. [Google Scholar] [CrossRef]
- Lee, W.-C.; Shieh, Y.S.; Liao, Y.F.; Lee, C.-H.; Huang, C.-S. Long-term maxillary anteroposterior changes following maxillary protraction with or without expansion: A meta-analysis and meta-regression. PLoS ONE 2021, 16, e0247027. [Google Scholar] [CrossRef]
- Mandall, N.; Cousley, R.; DiBiase, A.; Dyer, F.; Littlewood, S.; Mattick, R.; Nute, S.J.; Doherty, B.; Stivaros, N.; McDowall, R.; et al. Early class III protraction facemask treatment reduces the need for orthognathic surgery: A multi-centre, two-arm parallel randomized, controlled trial. J. Orthod. 2016, 43, 164–175. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).