Abstract
The application of feedback devices for cardiopulmonary resuscitation (CPR) can effectively enhance the quality of life-saving treatment during CPR. This article is a narrative review that selects literature on feedback devices used in chest compression and provides a comprehensive review and analysis of the development and current research status of feedback devices used in CPR. The development status of visual–auditory feedback devices used in chest compression at home and abroad and the advantages and disadvantages of existing feedback devices are the main points of discussion. Based on existing devices and technologies, this article explores the difficulties and deficiencies of current feedback device development. Finally, we propose the future development direction of CPR feedback equipment combined with physiological information data-monitoring devices.
1. Introduction
Cardiac arrest is a serious threat to human life and health. China is the site of approximately 660,000 cases of out-of-hospital cardiac arrest (OHCA) each year [1]. Even in developed areas such as Shanghai, which boasts a well-equipped medical infrastructure and advanced community healthcare facilities, the average hospital admission survival rate over five years is only 4.14%, and the discharge survival rate is only 1.23% [2]. Cardiopulmonary resuscitation (CPR) is widely believed to be the most effective way to rescue patients suffering from cardiac arrest and restore spontaneous respiration and circulation (known as return of spontaneous circulation, ROSC) [3]. To improve the survival rate of patients, timely and high-quality intervention is essential in every component of the chain of survival. In particular, timely and effective CPR is crucial, with chest compression being a key component [4]. Currently, the primary mode to maintain the quality of CPR is a feedback control system, which provides real-time feedback on the effectiveness of CPR to enhance its quality.
The 2010 American Heart Association (AHA) CPR guidelines suggest that the use of new devices for cardiopulmonary resuscitation promotion and feedback may significantly improve the quality of CPR training and practice. In 2015, the AHA updated its CPR guidelines to allow the use of visual and auditory feedback devices during actual CPR to optimize the effectiveness of resuscitation in real time. The 2020 AHA CPR guidelines reaffirm the use of these feedback devices and suggest that physiological parameters such as arterial blood pressure or end-tidal carbon dioxide (ETCO2) may also be useful in monitoring and optimizing CPR quality when feasible. Therefore, this paper aims to review the current research on closed-loop feedback devices used in cardiopulmonary resuscitation, in order to promote the development of closed-loop CPR, enhance the quality of resuscitation, and ultimately improve the survival rate of patients.
2. Classification of Feedback Devices for Cardiopulmonary Resuscitation
The feedback device for CPR has undergone significant development since its early use as a simple metronome. The metronome provides a fixed beat to assist the rescuer in maintaining a steady compression rate, thereby ensuring the quality of CPR and increasing the likelihood of successful resuscitation [5]. Feedback devices for CPR are generally divided into two categories based on the type of feedback information: auditory–visual feedback devices and physiological information data-monitoring feedback devices. Auditory–visual feedback devices provide a certain beat sound and display compression depth graphically or through color differences and can use sound, graphics, or color to correct the rescuer’s compression rate and depth in real time to ensure the quality of CPR. Physiological information data-monitoring feedback devices can monitor one or more parameters, such as cardiac output (CO), coronary perfusion pressure (CPP), mean arterial relaxation pressure (MARP), ECG amplitude spectrum area (AMSA), ETCO2, pulse oxygen saturation waveform, and regional cerebral oxygen saturation (rScO2), to adjust the compression strategy.
Studies have shown that maintaining standard external chest compression can significantly improve the survival rate of patients [6]. However, rescuers often experience physical exhaustion, making it difficult to maintain quality CPR for an extended period. The quality of CPR tends to decline after several minutes of CPR, with studies indicating that only 18% of rescuers are capable of providing qualified chest compression continuously after five minutes of chest compression [7]. The quality of CPR is also related to the physical fitness of rescuers [8], as well as their proficiency in CPR techniques. Thus, feedback devices for CPR play a crucial role in maintaining or improving the quality of CPR.
2.1. Audio-Visual Feedback Devices
In 2015, the American Heart Association endorsed the use of feedback devices during CPR to enhance resuscitation quality [4]. Even for medical professionals, accurately assessing the depth and frequency of CPR may be challenging [9,10], and the quality of resuscitation may decline due to fatigue. Additionally, perceived compression depth and rate may differ from actual ones [11], which underscores the need for audio-visual feedback devices to improve CPR quality and enhance resuscitation quality.
The existing and past audio-visual feedback devices available on the market for cardiopulmonary resuscitation were screened. The analysis includes miniaturized devices specifically designed for manual chest compression, which must accurately measure and display the compression depth during the resuscitation process. Using PubMed, we conducted a comprehensive search for articles published between 1995 and 2023 with the specific keyword “cardiopulmonary resuscitation feedback”. This search yielded a total of 90 publications. Subsequently, we applied relevant filters such as “clinical trial”, “randomized controlled trial”, and “review”, while also limiting the language to English. Thirty-three publications met the above criteria. Furthermore, we conducted meticulous web searches and PubMed searches for the names of audio-visual feedback devices to assess the clinical effectiveness of various audio-visual feedback devices utilized in cardiopulmonary resuscitation. Table 1 outlines the evolution of CPR audio-visual feedback devices.
Currently, the development of audio-visual feedback devices for CPR has reached a relatively mature stage. These devices are predominantly based on two main components: pressure sensors and accelerometers. Pressure sensors measure the force applied to the patient’s chest, which is set based on the patient’s weight and the desired depth of compression. However, since it cannot detect individual compression, a pressure sensor-based feedback device can only provide feedback on compression depth and not on compression rate. On the other hand, accelerometers measure the acceleration of the patient’s chest and use these data to calculate the distance moved during compression. The latest CPR feedback devices on the market are predominantly based on accelerometers, with some models also integrating pressure sensors. While an accelerometer-based feedback device is equipped with an electronic processor capable of calculating the compression rate, it is not well-suited for monitoring the quality of ventilation [12].
As the earliest device with cardiopulmonary resuscitation feedback function, CPR-plus boasts several advantages, including non-invasiveness, portability, and easy use. The CPR-plus is shown in Figure 1a. It achieves compression depth measurement via a pressure-sensitive compression plate and features a metronome for prompt pacing. In a comparative study examining CPR-plus usage versus non-usage, results showed that nurses using CPR-plus exhibited greater accuracy in compression and more standardized hand positions compared to those not using the device [13].
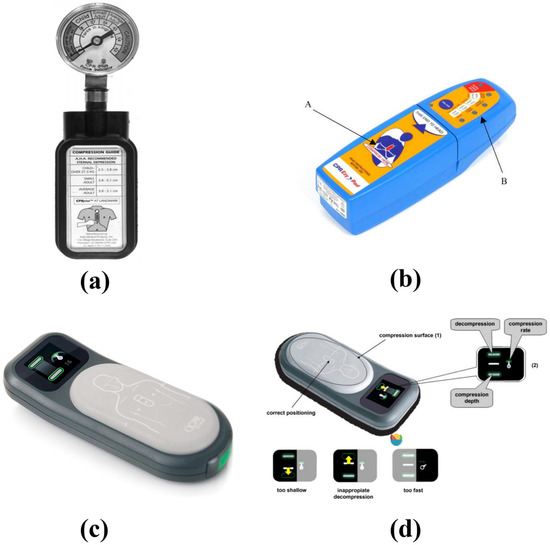
Figure 1.
(a) CPR-plus, (b) CPREzy™ device, (c) CPRmeter™, (d) CPRmeter™ function.

Table 1.
Audio-visual feedback devices for cardiopulmonary resuscitation.
Table 1.
Audio-visual feedback devices for cardiopulmonary resuscitation.
| Device | Feedback | Feedback Technology | Disadvantages | References |
|---|---|---|---|---|
| CPR-plus | Compression depth; Compression rate | Pressure sensor and metronome | Run on batteries; Unable to record historical data; Unable to connect with external devices; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected; Not easy to read | Elding et al. [13] |
| CPREzy™ | Compression depth; Compression rate; Angle of compression; Full chest relaxation | Pressure sensor and metronome | Run on batteries; Unable to record historical data; Unable to connect with external devices; No feedback on pulmonary ventilation; Use carries a certain risk of injury to rescuers; Requires more vigorous compression to drain energy | Perkins et al. [14]; Boyle et al. [15] |
| Zoll PocketCPR™ | Compression depth; Compression rate | Accelerometer; Metronome; Voice prompt | Run on batteries; Unable to record historical data; Unable to connect with external devices; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected; May interfere with normal compression | Zapletal et al. [16] |
| Laerdal CPRmeter™ | Compression depth; Compression rate, duration, and chest compression scores; Full chest relaxation | Accelerometer; Pressure sensor; Metronome | Run on batteries; No feedback on pulmonary ventilation | Zapletal et al. [16] Skorning et al. [17] |
| TrueCPR™ | Visual overview of compression depth; Compression rate; Compression score; Maximum pause time; Compression with pause time | Triaxial magnetic field induction | Run on batteries; Unable to connect with external devices; No feedback on pulmonary ventilation | Smereka et al. [18] Rodríguez-Venegas et al. [19] |
| Feedback Sensor Push | Compression depth; Compression rate | / | Run on batteries; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected | / |
| Cardio First Angel™ | Compression depth; Full chest relaxation | Tensile springs | Unable to record compression parameters; Unable to record historical data; Unable to connect with external devices; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected | Vahedian-Azimi et al. [20] Guenther et al. [21] |
| Beaty | Compression depth | Pressure sensor and metronome | Only compression depth feedback; Run on batteries; Unable to record historical data; Unable to connect with external devices; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected | / |
| CPR-1100 CPR Assist | Compression depth; Compression rate; Device tilt; Sinking of patient’s back | Accelerometer | Run on batteries; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected | / |
| SUNLIFE Palm CPR | Compression depth; Compression rate | Pressure sensor; Metronome; Voice feedback | Poor consistency in achieving adequate recoil; Run on batteries; Unable to connect with external devices; No feedback on pulmonary ventilation; The incorrect angle of compression cannot be detected | Wu et al. [22] |
CPREzy™ is a portable device specifically designed to enhance manual chest compression during cardiopulmonary resuscitation. By utilizing a row of glowing LED lights, it provides a readable and user-friendly display of the current compression force to make it easier for rescuers to observe. The appearance of the CPREzy™ device is shown in Figure 1b, with the compression pad located in the lower half of the device (A) and a smaller upper half (B) consisting of a light indicator. It is imperative for rescuers to verify that none of the green LEDs are activated during the upstroke phase of compression, which signifies the successful release of pressure between consecutive compression cycles. Evaluation studies have shown that the use of CPREzy™ can improve compression speed, increase the number of correct compression, enhance compression effectiveness, and reduce the impact of fatigue on compression quality [15]. The device features a customized display of LED lights based on the individual’s body type and weight. All lights are extinguished between two compression to indicate complete chest rebounding. The device also has an integrated metronome to emit prompts at the recommended chest compression rate. However, it is important to note that improper use of CPREzy™ may cause hand injuries to rescue personnel [14].
The Laerdal CPRmeter™, developed by the Norwegian company Laerdal, is based on an accelerometer design. To enhance measurement accuracy, a pressure sensor was incorporated [16]. The appearance of the CPRmeter™ device is shown in Figure 1c. The top surface of the CPRmeter™ features a gray, hard rubber cap that serves as the contact surface for the rescuer’s hand. Feedback is provided through a 26 × 26 mm color display. Compression depth is represented by a white bar that moves up and down between two green fields, with the two fields turning gray when the compression depth is too deep or too shallow, as seen in Figure 1d. Compression rate is displayed on a speedometer-like display, with the pointer located in the green range and lit up when the rate is appropriate [17]. The CPRmeter™ can be connected to the HeartStart MRx defibrillator (Philips Medical System), allowing for the integration of defibrillation and CPR feedback devices [12,23]. An effectiveness study showed that when the device was used by professionals, it was able to improve compression depth and rate, as well as reduce irregular inclinations. Most users found the CPRmeter™ to be highly beneficial and easy to use, even after minimal training [17]. A comparison study with the Zoll PocketCPR™ showed the CPRmeter™ to perform better in detecting inclinations during compression [16].
The second-generation CPRmeter™ 2 can be combined with the CPRmeter™ app to promote quality improvement initiatives by sharing details of the CPR, such as compression depth, compression frequency, time duration, and chest compression scores. After the resuscitation is completed, the CPRmeter™ application can report, share, and export statistical data to enable a more detailed analysis of the resuscitation details.
The Zoll PocketCPR™ is a small, battery-powered device used for CPR made in the United States. Its appearance is depicted in Figure 2a. It utilizes an accelerometer to measure the frequency and depth of compression and can be placed on the victim’s chest to provide audio prompts to guide the rescuer in performing CPR, if desired. The feedback on compression depth is provided through the flashing of LED lights, with the metronome increasing the LED flashing rate to reflect the correct compression depth and rate according to the CPR guidelines [12]. However, a study on the Zoll PocketCPR™ demonstrated a high proportion of inadequate compression points during CPR usage, which can be attributed to the device’s lack of a pressure sensor and reliance on an accelerometer, which cannot detect incorrect compression angles. Additionally, the time from the start of measurement to the first recorded chest compression was significantly increased when using the Zoll PocketCPR™, potentially reducing the success rate of resuscitation in practical applications [16]. Despite its limitations, the Zoll PocketCPR™ remains a promising device for improving CPR performance.
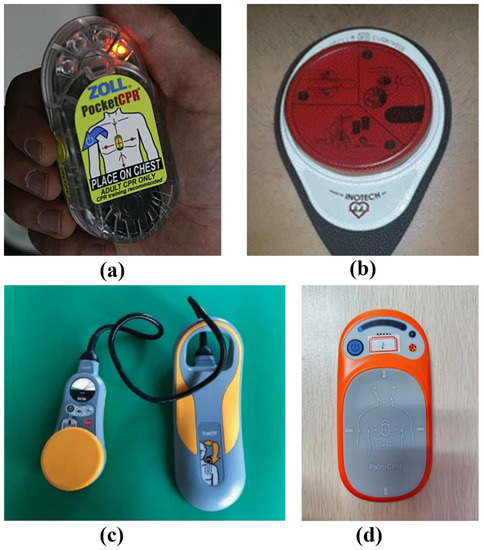
Figure 2.
(a) Zoll Pocket CPR, (b) Cardio First Angel™, (c) True-CPR, (d) Palm CPR feedback device.
Cardio First Angel™ (CFA), on the other hand, shown in Figure 2b, is an entirely mechanical feedback device designed to assist with cardiopulmonary resuscitation (CPR) by providing audio feedback on chest compression. Intriguingly, this device does not require any power source. It relies on a specially designed spring system that emits a sound upon achieving the correct compression depth from 50–60 mm. Additionally, the spring mechanism produces a second sound when the chest fully rebounds, thus confirming both the downward and upward motion of a correct compression. Comparative studies have been conducted to evaluate the effectiveness of standard chest compression performed without the aid of CFA versus those assisted by the CFA device on resuscitation mannequins. Notably, significant improvements were observed in the compression depth when the CFA-assisted method was employed [21]. Furthermore, a clinical trial involving 80 participants demonstrated that the use of CFA substantially increased rates of ROSC and concurrently decreased the risk of rib fractures. These results underscore the potentially transformative impact of the CFA device in improving CPR efficacy and safety [20].
The True-CPR developed by Physio-Control is a smart compression feedback device from the United States that can provide real-time CPR feedback, displaying compression depth and rate on a highly visible dial. The external appearance of the True-CPR device is depicted in Figure 2c. In addition, the device provides metronome prompts for cardiac resuscitation and ventilation guidance to assist rescuers in adhering to recommended guidelines. Unlike other feedback devices that use accelerometers, True-CPR is the only device to use Tri-Axis Field Induction (TFI), a proprietary technology based on physical control. TFI uses a three-dimensional magnetic field to accurately measure the distance between two objects (chest pad and back pad) during the resuscitation process, enabling accurate measurement of chest compression depth and providing high-quality real-time feedback. True-CPR compensates for misalignment between the chest and back pads, ensuring accurate measurement of compression depth even when misaligned [24]. This feature greatly improves the ability to measure compression depth on flexible surfaces. Moreover, the True-CPR device can enhance the proportion of full chest release during compression [18]. Research evaluating the use of the True-CPR device on a basic life support (BLS) ambulance in Barcelona showed that the device significantly improved the quality of chest compression performed by emergency technicians without increasing the time of the first defibrillation [19].
Corscience’s Feedback Sensor Push (COR.CPR-RRB) is a sophisticated device for monitoring chest compression. It delivers precise measurements of compression depth and frequency, thereby enabling comprehensive data collection, analysis, and transfer. Notably, the device can be integrated with a host system, such as a defibrillator or monitor, further enhancing its utility [25].
Beaty, a device developed by Medical Feedback Technologies, offers real-time audio feedback regarding the efficacy of chest compression during the process of cardiopulmonary resuscitation (CPR) through the utilization of pressure sensors. This device serves as a guiding mechanism for medical professionals to precisely calibrate the depth of chest compression. Moreover, an audible alert is activated upon the achievement of a compression depth of 5 cm [26].
CPR-1100 CPR Assist, developed by Nihon Kohden, presents chest compression depth and frequency information. This device employs orange lights to indicate the recommended compression frequency and blue lights to signify the desired compression depth. Furthermore, Nihon Kohden’s CPR-1100 CPR Assist establishes a Bluetooth connection with a computer for the purpose of recording the quality of chest compression. Moreover, CPR-1100 CPR Assist exhibits compatibility with defibrillators through a Bluetooth connection [27].
The Sunlife Palm CPR chest compression feedback meter, developed by China Suzhou Shangling Research, provides indicator lights on the top to give feedback on compression depth by quantity and color and feedback on compression rate by R light color. The Palm CPR is shown in Figure 2d. The device can connect to a mobile terminal to monitor, record, and provide real-time feedback on the quality of cardiopulmonary resuscitation, including the patient’s physiological parameters and the rescuer’s performance indicators. These data can be used for real-time resuscitation and quality improvement projects after resuscitation is completed in the system scale [28]. Studies have shown that Palm CPR has good consistency in average compression depth, moderate consistency in average frequency and depth compliance times, but poor consistency in rebound times [22].
2.2. Research on Feedback Devices Based on Physiological Information Data Monitoring in China and Abroad
Simple feedback systems have been shown to improve the effectiveness of chest compression during CPR. However, a limitation of such systems is the lack of personalization for individual patients and a standardized execution. To address this issue, feedback devices utilizing physiological data monitoring are needed. Due to the limitations of the prehospital environment, invasive detection is often difficult. Therefore, non-invasive detection of physiological parameters of cardiac arrest patients is crucial in the development of a closed-loop feedback module for automatic chest compressors. By monitoring real-time physiological parameters and observing the effects of chest compression, intelligent closed-loop control can be achieved.
A study by Lampe et al. at Northwell Health established a time-dependent function correlating carotid blood flow during cardiac arrest resuscitation and response to varying chest compression. By predicting the carotid blood flow generated by subsequent chest compression, the study aimed to optimize CPR parameters in real time, maximizing carotid blood flow [29]. Sebastian et al. evaluated the feasibility of using a machine-controlled closed-loop CPR (MC-CPR) system to optimize coronary perfusion pressure (CPP) during CPR. Their real-time hemodynamic simulations demonstrated that MC-CPR, controlled by a closed-loop machine, significantly outperformed the AHA CPR guidelines in improving coronary perfusion pressure [30]. Jaureguibeitia et al. proposed a machine learning algorithm for impedance-based ventilation detection in mechanical CPR. Using adaptive signal processing, they demonstrated feasible ventilation detection and suggested ventilation rate feedback during resuscitation [31].
In China, researchers at the Academy of Military Medical Sciences, including Zhang et al., have developed a mechanical chest compression closed-loop control system. The system consists of two parts: the LabVIEW control platform and the mechanical chest compression controller. A fuzzy neural network and fuzzy PID control strategy are used to effectively regulate compression depth. The closed-loop control algorithm combines beneficial factor (BF), which reflects blood flow perfusion degree, and dangerous factor (RF), which reflects rib fracture risk, based on chest compression resuscitation theory and intelligent control theory. The algorithm-enhanced chest compression system, verified through a LUCAS automatic chest compressor, outperforms traditional systems [32]. In another study, Wang et al. proposed a chest compression closed-loop controller based on a fuzzy control algorithm that adjusts the compression depth according to CPP and evaluated the performance of the fuzzy controller by computer simulation and compared it with the traditional PID controller [33]. In 2021, Li et al. from Shandong University developed an auxiliary control system for a chest compression device based on ETCO2. The system seamlessly integrates ETCO2 measurement with an automated chest compression device, enabling precise tracking of compression depth and frequency. By determining the difference signal, it dynamically adjusts the compression depth and frequency of the chest compression device based on the determined control signal [34].
2.3. Application Status and Effects of Cardiopulmonary Resuscitation Feedback Devices
CPR feedback devices are widely utilized in CPR training. In studies investigating CPR training, it has been observed that training with a feedback device enhances CPR competency and overall quality more significantly than traditional CPR training methods [35]. Furthermore, the utilization of feedback devices can augment skill acquisition and overall performance in cardiopulmonary resuscitation [36]. In a comparative study evaluating the impact of device-based real-time visual feedback against traditional instructor-led chest compression skills training and self-efficacy, the group guided by the QPCR feedback device demonstrated enhanced accuracy in compression depth and frequency, surpassing the results achieved through traditional methods by 24.47% and 19.63%, respectively [37]. It has been shown that the TrueCPR™ device effectively enhances resuscitation skills among nursing students. Participants who used TrueCPR™ during training exhibited an 18% increase in adequate compression rate and a 23% increase in full chest release [18].
From a practical standpoint, the combination of current CPR audio-visual feedback devices and smartphones offers a more accessible feedback tool for emergency situations. By utilizing the data collected through a smartphone’s built-in accelerometer, real-time assessment of compression depth and frequency can be achieved, aligning closely with the actual values. This enables accurate real-time feedback on CPR quality through a dedicated CPR mobile application [38].
2.4. Integration of Feedback Devices with Defibrillator and Related Equipment
Real CPR Help™ is an enhanced functionality integrated into Zoll’s AED Plus, utilizing accelerometer technology within the ZOLL defibrillator electrodes, furnishing real-time feedback concerning the accuracy of CPR compression in terms of depth and frequency. Audio and visual prompts guide the operator through the CPR process. Notably, unlike the autonomous small free-standing AVF device discussed in Section 2.1, the utilization of Real CPR Help™ is contingent upon its integration with the CPR Dashboard; it cannot function independently. The CPR Dashboard, in addition to presenting data on compression depth and frequency, also exhibits an indicator illustrating coronary perfusion pressure. This inclusion offers a more intuitive representation of the patient’s circulatory effectiveness. A comparative study conducted on the effectiveness of Real CPR Help™ demonstrated noteworthy outcomes. The overall quality of CPR demonstrated a marked improvement with the implementation of Real CPR Help™. The proportion of participants who achieved sufficient compression depth surged from 25% to 78.1%, and the percentage of participants executing compression with proper technique increased from 50% to 86.5% [39].
3. Current Limitations of Cardiopulmonary Resuscitation Closed-Loop Feedback Devices and Future Development
To improve the quality and success rate of CPR and provide effective guidance for rescuers, as well as personalize chest compression for cardiac arrest patients, feedback devices for CPR are continuously being developed. These feedback devices have achieved significant results in terms of improving the quality of CPR and increasing the survival rate of cardiac arrest patients. However, some limitations and problems still remain.
- Limited Application Scenario
The application scenario for these devices is limited, and their reliability is questionable in special environments such as earthquakes, fires, explosions, mine collapses, traffic accidents, uneven support surfaces, soft compressible situations, and patient transport. The measurement results during artificial CPR may not be accurate when using a manual chest compression auditory feedback device, and the reliability of the device is questioned.
- A Non-Intuitive Feedback Mode
The closed-loop feedback mode used in these devices is not intuitive, and its practicality is moderate. The moving parts of the pressure sensor may cause harm to the rescuers, and additional force may be required to perform chest compression due to the obstruction of the device. This increases the fatigue of the rescuers, making it harder for them to provide effective CPR. Due to the feedback device generally providing indications of compression through indicator lights, it takes time for unfamiliar users to learn and understand, which may delay the time of on-site rescue.
- Limitations of Feedback Parameters
Artificial chest compression audio-visual feedback devices primarily provide feedback on the quality of CPR, such as compression rate and depth. However, they do not assess the patient’s physiological response to CPR, presenting a limitation in the scope of their feedback.
- Limited Contribution to Improving Chest Compression Quality
The current audio-visual feedback devices on the market are only able to provide feedback on the depth and frequency of the compression, and some products can only provide feedback on the depth. During chest compression, body posture, hand placement, and compression position significantly influence the quality of cardiopulmonary resuscitation (CPR). However, the current audio-visual feedback devices lack the ability to comprehensively assess and provide guidance on these critical aspects. As a result, the effective utilization of such devices requires individuals who have undergone relevant training. Furthermore, these current audio-visual feedback devices are unable to provide personalized guidance based on the unique differences of individual patients.
Simple feedback systems for artificial chest compression can enhance compression effectiveness, ensure AHA cardiopulmonary resuscitation guideline adherence, reduce the risk of chest compression, and achieve the recommended compression depth and frequency. However, these systems have a limitation in adjusting compression parameters according to the patient’s physiological state. The closed-loop feedback in automatic chest compressors offers a viable solution to this issue. These compressors incorporate a real-time monitoring and closed-loop feedback module for physiological parameters, utilizing the feedback from physiological parameters of cardiac arrest cases to assess the effectiveness of chest compression and achieve individualized closed-loop control of automatic chest compression.
In the future, feedback research for CPR will advance towards individualized, intelligent, and multi-functional directions. Vital sign parameters such as ECG, blood pressure, oxygen saturation, ETCO2, etc. will be monitored to enable intelligent closed-loop feedback for patient resuscitation and provide accurate chest compression. Automatic CPR machines are expected to meet these requirements. Currently, closed-loop feedback in automatic CPR machines remains in the research stage and has not been introduced in market products. Most CPR machines on the market can only perform a compression function or CPR quality monitoring function, lacking the integration of multi-function basic life support equipment with feedback systems.
In automatic external chest compression, statistical data from adult patients with out-of-hospital cardiac arrest who were admitted have shown that compared to manual compression, mechanical automatic external chest compression devices increase cerebral blood flow, significantly improve organ perfusion pressure, and demonstrate higher end-tidal CO2 levels [40] as well as slightly better recovery of spontaneous circulation [4]. However, there was no significant difference in 4 h survival rate between patients who received treatment with a mechanical CPR algorithm and those who received manual CPR treatment based on the AHA guidelines [41]. Moreover, mechanical CPR, when contrasted with manual compression, also fails to yield a noteworthy enhancement in the incidence of ROSC [42]. Automatic external chest compression also lack effective feedback on compression effectiveness, emphasizing the need for equipment that can provide feedback on the quality of chest compression to prevent low-quality compression during CPR.
In the future, automatic CPR is expected to utilize various intelligent algorithms to monitor multiple vital sign parameters, combining respiratory support control technology, extracorporeal 3D CPR technology, and synchronous automatic extracorporeal electric resuscitation technology to create a real-time feedback system of multi-parameter analysis and individualization. With the application of 5G and telemedicine, real-time transmission of feedback status and physiological parameters will be realized. Thus, the application of closed-loop feedback to mechanical CPR presents a broad prospect for the future of CPR technology [43].
4. Equipment Support of CPR Feedback Physiological Parameter Monitoring
In a comprehensive questionnaire survey encompassing 1652 emergency physicians in China, a variety of methodologies for quality monitoring of CPR were examined. Among the participants, 93.1% (1514) stated that they assessed the quality of CPR by directly observing the actual procedures being performed. A limited proportion of respondents—16.0% (256) and 13.8% (228)—reported the routine utilization of audio-visual feedback devices during chest compression and end-expiratory carbon dioxide monitoring during CPR, respectively. The predominant impediment to the usage of these tools was cited as a lack of necessary equipment. Additionally, a mere 1.3% (22) of respondents indicated the routine use of invasive arterial pressure monitoring during CPR. The primary deterrent to the implementation of this method was the challenge associated with establishing arterial access [44].
In the context of clinical practices in China, the predominant approach for assessing the quality of CPR performance remains reliant on emergency physicians. The lack of availability of advanced equipment and technological constraints has impeded widespread adoption of audio-visual feedback devices and monitoring mechanisms which can evaluate blood flow perfusion efficacy directly during emergency CPR. Consequently, clinical cardiopulmonary resuscitation quality feedback still needs physiological parameter monitoring equipment, particularly non-invasive physiological parameter monitoring equipment. End-tidal carbon dioxide is the most ideal physiological parameter in cardiopulmonary resuscitation feedback monitoring because of its non-invasive nature, lower acquisition cost compared to multi-parameter monitors, and recommendation by the AHA to use the waveform of carbon dioxide in CPR guidelines.
4.1. End-Tidal Carbon Dioxide Monitoring Equipment
The infrared method is routinely utilized in clinical settings, primarily due to its main absorption wavelength for CO2 at 4260 nm. Based on this property, CO2 concentration can be deduced from its absorption rate. Two modes of application are prevalent for the infrared method: bypass flow and mainstream flow [45].
In mainstream flow mode, the sensor is directly connected to the patient’s tracheal tube connector, becoming an integral part of the artificial airway. The airflow actively traverses the sensor. The key advantages of the mainstream infrared method lie in its swift medical diagnostic response due to the sensor’s direct contact with the airflow. Conversely, the bypass flow mode does not directly connect the sensor to the ventilation loop. Instead, exhaled gas is extracted through an air pump and then measured in a dedicated chamber. The reaction rate of recognition is moderately slower in this setup, leading to an approximately 3 s time delay between chest undulations and exhaled gas [45].
Infinium Medical has developed the Cleo EtCO2 Monitor with Vitals, an intuitive device for non-invasively measuring patients’ vital signs, including blood pressure, SpO2, rapid temperature, and exhaled carbon dioxide. The device supports continuous monitoring over extended periods and is applicable in a variety of settings. Its uses encompass both intubated and non-intubated applications, on-site inspections, bedside monitoring, and more [46].
Masimo’s Emma Capnograph, a portable real-time carbon dioxide analyzer, provides continuous and clear visualizations of carbon dioxide measurements. The device can display EtCO2 and respiratory rate measurements, along with real-time ETCO2 waveforms within a timeframe of 15 s [47].
4.2. The Application of End-Tidal Carbon Dioxide in Cardiopulmonary Resuscitation Feedback
End-tidal carbon dioxide (ETCO2), serving as an indirect measure of blood flow during cardiopulmonary resuscitation (CPR), is widely employed as a guiding tool in the CPR process [48]. Throughout the course of CPR, ETCO2 maintains a direct correlation with cardiac output, thus making it a common metric for gauging output during CPR [49].
Existing research suggests a linear relationship between the depth of chest compression and end-expiratory carbon dioxide values. An analysis utilizing mixed-effects models on a sample of 230 subjects revealed a 4.0% increase in ETCO2 (p < 0.0001) for each 10 mm augmentation in chest compression depth and a 1.7% increase (p = 0.02) in ETCO2 with every 10-compression/min increase in chest compression frequency [50].
In another study encompassing 583 patients with both in-hospital (2%) and out-of-hospital (27%) cardiac arrests, chest compression rates ranged from 95 to 125/min, with depths varying between 31 and 59 mm. The mixed-effects model also demonstrated that for each 10 mm increase in compression depth, ETCO2 increased by 1.4 mm (p < 0.001). Conversely, ETCO2 decreased by 3.0 mmHg (p < 0.001) for every 10-compression/min rise in ventilation rate. The compression frequency did not exhibit a significant effect on ETCO2 [49].
5. Conclusions
In summary, this paper emphasizes the importance of CPR feedback in basic life support, discusses the evolution of CPR feedback devices from simple to personalized, and highlights how technological advancements will make CPR devices increasingly intelligent with closed-loop feedback.
Modern CPR is a crucial step in basic life support, and to improve the quality of CPR and minimize the risk of injury, real-time and effective CPR feedback is vital. CPR feedback devices can truly improve CPR quality in training and real life. In complex out-of-hospital settings such as accidents, they can also provide effective assistance and improve the efficiency of treating cardiac arrest patients, thus exhibiting a broad scope of applicability. Over time, CPR feedback devices have evolved from simple visual and auditory feedback based on manual compression to personalized feedback from automated CPR machines using real-time physiological monitoring. The latest CPR devices leverage technological advancements to provide increasingly intelligent feedback, incorporating a diverse range of monitoring data with deep learning algorithms to predict blood flow perfusion and support accurate compression.
Author Contributions
Conceptualization, S.M. and Y.W.; methodology, Y.W.; formal analysis, Y.W.; investigation, Y.W.; writing—original draft preparation, Y.W.; writing—review and editing, S.M. and Z.C.; visualization, Y.W.; supervision B.F. and S.H.; project administration, B.F.; funding acquisition, B.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Automatic Basic Life Support Integrated Machine Development, grant number TJUWYY2022009.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to its retrospective nature as a literature review.
Informed Consent Statement
Patient consent was waived due to its retrospective nature as a literature review.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kiguchi, T.; Okubo, M.; Nishiyama, C.; Maconochie, I.; Ong, M.E.H.; Kern, K.B.; Wyckoff, M.H.; McNally, B.; Christensen, E.F.; Tjelmeland, I.; et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation 2020, 152, 39–49. [Google Scholar] [CrossRef]
- Dai, Z.; Lin, Q.; Xu, Y. A 5-year trend observation study on out-of-hospital cardiac arrest resuscitation outcomes. Chin. J. Emerg. Med. 2022, 31, 497–503. [Google Scholar]
- Kouwenhoven, W.B.; Jude, J.R.; Knickerbocker, G.G. Closed-chest cardiac massage. JAMA 1960, 173, 1064–1067. [Google Scholar] [CrossRef] [PubMed]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M.; Lavonas, E.J.; Magid, D.J. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S337–S357. [Google Scholar] [CrossRef] [PubMed]
- Ateyyah, K.A.; Cady, C.E.; Poltrock, J.T.; Pirrallo, R.G. A Novel Use of a Metronome in Dispatcher-assisted Cardiopulmonary Resuscitation. Prehosp. Emerg. Care 2015, 19, 131–134. [Google Scholar] [CrossRef]
- Youness, H.; Al Halabi, T.; Hussein, H.; Awab, A.; Jones, K.; Keddissi, J. Review and Outcome of Prolonged Cardiopulmonary Resuscitation. Crit. Care Res. Pract. 2016, 2016, 7384649. [Google Scholar] [CrossRef]
- Hightower, D.; Thomas, S.H.; Stone, C.K.; Dunn, K.; March, J.A. Decay in quality of closed-chest compression over time. Ann. Emerg. Med. 1995, 26, 300–303. [Google Scholar] [CrossRef]
- Lancaster, G.D.; Stilley, J.D.; Franke, W.D. How Does Rescuer Fitness Affect the Quality of Prolonged Cardiopulmonary Resuscitation? Prehosp. Emerg. Care 2022, 26, 195–203. [Google Scholar] [CrossRef]
- Hamilton, R. Nurses’ knowledge and skill retention following cardiopulmonary resuscitation training: A review of the literature. J. Adv. Nurs. 2005, 51, 288–297. [Google Scholar] [CrossRef]
- Kaye, W.; Mancini, M.E. Retention of cardiopulmonary resuscitation skills by physicians, registered nurses, and the general public. Crit. Care Med. 1986, 14, 620–622. [Google Scholar] [CrossRef]
- Pozner, C.N.; Almozlino, A.; Elmer, J.; Poole, S.; McNamara, D.; Barash, D. Cardiopulmonary resuscitation feedback improves the quality of chest compression provided by hospital health care professionals. Am. J. Emerg. Med. 2011, 29, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Gruber, J.; Stumpf, D.; Zapletal, B.; Neuhold, S.; Fischer, H. Real-time feedback systems in CPR. Trends Anaesth. Crit. Care 2012, 2, 287–294. [Google Scholar] [CrossRef]
- Elding, C.; Baskett, P.; Hughes, A. The study of the effectiveness of chest compression using the CPR-plus. Resuscitation 1998, 36, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Augre, C.; Rogers, H.; Allan, M.; Thickett, D.R. CPREzy (TM): An evaluation during simulated cardiac arrest on a hospital bed. Resuscitation 2005, 64, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Boyle, A.J.; Wilson, A.M.; Connelly, K.; McGuigan, L.; Wilson, J.; Whitbourn, R. Improvement in timing and effectiveness of external cardiac compression with a new non-invasive device: The CPR-Ezy. Resuscitation 2002, 54, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Zapletal, B.; Greif, R.; Stumpf, D.; Nierscher, F.; Frantal, S.; Haugk, M.; Ruetzler, K.; Schlimp, C.; Fischer, H. Comparing three CPR feedback devices and standard BLS in a single rescuer scenario: A randomised simulation study. Resuscitation 2014, 85, 560–566. [Google Scholar] [CrossRef]
- Skorning, M.; Beckers, S.K.; Brokmann, J.; Roertgen, D.; Bergrath, S.; Veiser, T.; Heussen, N.; Rossaint, R. New visual feedback device improves performance of chest compression by professionals in simulated cardiac arrest. Resuscitation 2010, 81, 53–58. [Google Scholar] [CrossRef]
- Smereka, J.; Szarpak, L.; Czekajlo, M.; Abelson, A.; Zwolinski, P.; Plusa, T.; Dunder, D.; Dabrowski, M.; Wiesniewska, Z.; Robak, O.; et al. The TrueCPR device in the process of teaching cardiopulmonary resuscitation A randomized simulation trial. Medicine 2019, 98, e15995. [Google Scholar] [CrossRef]
- Rodríguez-Venegas, J.C.; Carmona-Jiménez, F.; Muñoz, I.; Palma-Padró, P.; Alonso, S. The True-CPR device. A new way to give great quality CPR? Resuscitation 2015, 96, 69–70. [Google Scholar] [CrossRef]
- Vahedian-Azimi, A.; Hajiesmaeili, M.; Amirsavadkouhi, A.; Jamaati, H.; Izadi, M.; Madani, S.J.; Hashemian, S.M.; Miller, A.C. Effect of the Cardio First Angel device on CPR indices: A randomized controlled clinical trial. Crit. Care 2016, 20, 147. [Google Scholar] [CrossRef]
- Guenther, S.P.W.; Schirren, M.; Boulesteix, A.L.; Busen, H.; Poettinger, T.; Pichlmaier, A.M.; Khaladj, N.; Hagl, C. Effects of the Cardio First AngelTM on chest compression performance. Technol. Health Care 2018, 26, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z. Consistency Study on Compression Quality of Two CPR Feedback Devices. Lingnan J. Emerg. Med. 2020, 25, 143–145. [Google Scholar]
- Philips. Q-CPR™ Measurement and Feedback Tool CPR Meter. Available online: https://www.usa.philips.com/healthcare/product/HCNOCTN89/qcpr-measurement-and-feedback-tool-cpr-meter#features (accessed on 7 October 2022).
- Physio-Control TrueCPR Coaching Device. Available online: https://www.aedsuperstore.com/physio-control-true-cpr-coaching-device.html (accessed on 7 October 2022).
- Feedback Sensor for Effective Chest Compression. Available online: https://www.corscience.com/products/defibrillation/feedback-sensor-push/ (accessed on 29 July 2023).
- Beaty. The Power to Save Lives. Available online: https://www.imbeaty.com/ (accessed on 29 July 2023).
- Kohden, N. CPR Assist Improving Quality of Resuscitation. Available online: https://ae.nihonkohden.com/en/products/resuscitation/cpr-1100.html (accessed on 29 July 2023).
- PalmCPR Chest Compression Feedback Device. Available online: https://www.sunlifescience.com/cn/PalmCPR.htm (accessed on 7 October 2022).
- Lampe, J.W.; Padmanaban, S.; Becker, L.B.; Zanos, T.P. Towards Personalized Closed-Loop Mechanical CPR: A Model Relating Carotid Blood Flow to Chest Compression Rate and Duration. IEEE Trans. Biomed. Eng. 2020, 67, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, P.S.; Kosmopoulos, M.N.; Gandhi, M.; Oshin, A.; Olson, M.D.; Ripeckyj, A.; Bahmer, L.; Bartos, J.A.; Theodorou, E.A.; Yannopoulos, D. Closed-loop machine-controlled CPR system optimises haemodynamics during prolonged CPR. Resuscitation Plus 2020, 3, 100021. [Google Scholar] [CrossRef]
- Jaureguibeitia, X.; Irusta, U.; Aramendi, E.; Owens, P.C.; Wang, H.E.; Idris, A.H. Automatic Detection of Ventilations During Mechanical Cardiopulmonary Resuscitation. IEEE J. Biomed. Health Inform. 2020, 24, 2580–2588. [Google Scholar] [CrossRef]
- Zhang, G. Study on Optimization Control of Closed-Loop Automatic External Chest Compression CPR. Ph.D. Thesis, The Academy of Military Medical Sciences of the PLA Academy of Military Science, Beijing, China, 2013. [Google Scholar]
- Wang, C.F. Closed-loop controller for chest compression based on coronary perfusion pressure: A computer simulation study. Med. Biol. Eng. Comput. 2016, 54, 273–281. [Google Scholar] [CrossRef]
- Li, K. An Assistive Control Method and System for External Chest Compression Device Based on PETCO-2. CN Patent 202111493254.8, 8 December 2021. [Google Scholar]
- Misztal-Okonska, P.; Goniewicz, K.; Goniewicz, M.; Ranse, J.; Hertelendy, A.J.; Gray, L.; Carlstrom, E.; Sorensen, J.L.; Khorram-Manesh, A. Importance of Immediate Electronic-Based Feedback to Enhance Feedback for First-Time CPR Trainees. Int. J. Environ. Res. Public Health 2021, 18, 3885. [Google Scholar] [CrossRef]
- Gugelmin-Almeida, D.; Tobase, L.; Polastri, T.F.; Peres, H.H.C.; Timerman, S. Do automated real-time feedback devices improve CPR quality? A systematic review of literature. Resusc. Plus 2021, 6, 100108. [Google Scholar] [CrossRef]
- Lee, P.H.; Lai, H.Y.; Hsieh, T.C.; Wu, W.R. Using real-time device-based visual feedback in CPR recertification programs: A prospective randomised controlled study. Nurse Educ. Today 2023, 124, 105755. [Google Scholar] [CrossRef]
- Stumpf, E.; Ambati, R.; Shekhar, R.; Staffa, S.J.; Zurakowski, D.; Sinha, P. A Smartphone application to provide real-time cardiopulmonary resuscitation quality feedback. Am. J. Emerg. Med. 2022, 60, 34–39. [Google Scholar] [CrossRef]
- Malwina, B.; Zuzanna, S.; Jakub, R.; Tomasz, F. Improvement of the quality of cardiopulmonary resuscitation performed with Real CPR Help® device among medical students and medical workers. Med. Res. J. 2021, 6, 177–183. [Google Scholar]
- Rubertsson, S.; Lindgren, E.; Smekal, D.; Ostlund, O.; Silfverstolpe, J.; Lichtveld, R.A.; Boomars, R.; Ahlstedt, B.; Skoog, G.; Kastberg, R.; et al. Mechanical chest compression and simultaneous defibrillation vs. conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest: The LINC randomized trial. JAMA 2014, 311, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.L.; Brooks, S.C. Mechanical versus manual chest compression for cardiac arrest. Cochrane Database Syst. Rev. 2018, 8, CD007260. [Google Scholar] [CrossRef]
- Sheraton, M.; Columbus, J.; Surani, S.; Chopra, R.; Kashyap, R. Effectiveness of Mechanical Chest Compression Devices over Manual Cardiopulmonary Resuscitation: A Systematic Review with Meta-analysis and Trial Sequential Analysis. West. J. Emerg. Med. 2021, 22, 810–819. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Fan, B.; Fan, H.; Hou, S. Review of Portable Basic Life Support Equipment. Disaster Med. Public Health Prep. 2022, 16, 373–379. [Google Scholar] [CrossRef]
- Yin, L. Exploring New Physiological Monitoring Indicators for Cardiopulmonary Resuscitation and Innovations in AED Teaching Methods. Ph.D. Thesis, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China, 2021. [Google Scholar]
- Yalin, W.; Guang, Z.; Taihu, W. End-expiratory carbon dioxide monitoring technology and equipment brief introduction. Med. Equip. 2014, 35, 117–120. [Google Scholar]
- EtCO2 Monitoring Device. Available online: https://infiniummedical.com/etco2-monitoring-device/ (accessed on 7 October 2022).
- EMMA® Capnograph Portable Real-Time Capnography. Available online: https://www.masimo.com/products/ventilator/capnography/emma-capnograph/ (accessed on 7 October 2022).
- Edelson, D.P.; Eilevstjonn, J.; Weidman, E.K.; Retzer, E.; Vanden Hoek, T.L.; Abella, B.S. Capnography and chest-wall impedance algorithms for ventilation detection during cardiopulmonary resuscitation. Resuscitation 2010, 81, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Sheak, K.R.; Wiebe, D.J.; Leary, M.; Babaeizadeh, S.; Yuen, T.C.; Zive, D.; Owens, P.C.; Edelson, D.P.; Daya, M.R.; Idris, A.H.; et al. Quantitative relationship between end-tidal carbon dioxide and CPR quality during both in-hospital and out-of-hospital cardiac arrest. Resuscitation 2015, 89, 149–154. [Google Scholar] [CrossRef]
- Murphy, R.A.; Bobrow, B.J.; Spaite, D.W.; Hu, C.; McDannold, R.; Vadeboncoeur, T.F. Association between Prehospital CPR Quality and End-Tidal Carbon Dioxide Levels in Out-of-Hospital Cardiac Arrest. Prehosp. Emerg. Care 2016, 20, 369–377. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).