Abstract
The aim of this in vitro study was to evaluate the accuracy of impressions made using two different silicones and corresponding stone casts in full-arch implant rehabilitation, using two laboratory scanners. A master model with six dental implants was created, scanned with a 12-megapixel scanner and used as digital master model. Ten implant impressions were obtained via two silicone impressions systems—Coltene® and Zhermack®—using the open-tray technique and poured gypsum. Two extraoral scanning systems (S600 ARTI Zirkonzhan® and Identica T500 Medit®) were used to scan the impressions and stone casts. Best-fit superimpositions were conducted between the master model and the virtual models obtained. A significance level of p < 0.05 was considered. The accuracy of the Medit® scanner was 82.26 [53.18; 111.34] µm for Coltene® silicone and 87.43 [72.00; 102.86] µm for Zhermack® silicone, and the accuracy of the Zirkonzhan® scanner was 69.90 [62.37; 77.43] µm for Coltene® silicone and 80.67 [65.77; 95.57] µm for Zhermack® silicone, without significant differences between scanners. When comparing the two silicones, no significant differences were found for the Medit® (p = 0.112) or Zirkonzhan® scanners (p = 0.162). The Zhermack® scanner showed better accuracy than the corresponding stone casts in the two scanners, Medit® (p = 0.019) and Zirkonzahn® (p = 0.002). The extraoral digitalization of impressions in edentulous dental arches with six implants proves to be a valid technique.
1. Introduction
The exponential growth of CAD/CAM (computer-aided design and computer-aided manufacturing) technology in prosthodontics can be attributed to continuous system development, improved quality control, the introduction of new materials, software refinement and the possibility of virtual evaluation [1].
CAD-CAM has gained widespread acceptance in implant rehabilitation, with a similar accuracy to conventional techniques for fixed prosthodontics [2]. Impression distortions and laboratory errors contribute to the misfit of rehabilitation implants [3,4]. Using a digital workflow can improve efficiency, reducing chair time and omitting some laboratory steps [2].
The digital impression can be acquired via two methods: (i) directly, using an intraoral scanner (IOS) for image acquisition and producing a 3D virtual model without using conventional impressions; and (ii) indirectly, using an extraoral scanner (EOS) to scan the stone model to create a 3D virtual model [5,6,7,8]. The STL (standard tessellation language) files corresponding to a three-dimensional dataset of the model are sent and stored electronically, improving efficiency [9].
Extraoral scanners were introduced in the 1980s to overcome the shortcomings of intraoral scanners at the time, which were considered too slow to be used in office and had limited accuracy. Extraoral scanners were initially developed to scan stone casts, but currently, more advanced systems also allow for the scanning of dental impressions [10,11,12,13,14]. In the indirect digitization of both impressions and models, the initial step is an analog impression.
Various factors can affect the accuracy of complete-arch implant impressions, such as the characteristics of the impression material, the impression technique, the splinting of the impression copings, the depth and angulation of the implants or the connection of the implants [4,6,9,15,16,17,18,19].
According to a systematic review published in 2018, no guidelines can be found to recommend a particular technique and material to achieve the most adequate accuracy in impressions with multiple implants [4]. Achieving an accurate transfer of implant position and angulation is a critical factor in obtaining a satisfactory prosthesis with an accurate fit [7,20,21]. According to several studies and considering the accuracy factor, the use of an intraoral impression with an optical scanner is not recommended in cases of multiple implants [22,23,24].
Although IOSs are increasingly used, they still require a learning curve and a considerable initial investment. In addition, in many clinical situations, using an IOS is less accurate than extraoral scanning [21]. Furthermore, the scanning of impressions benefits from eliminating the model fabrication procedure, which is time-consuming and a potential source of error [25]. For these reasons, scanning conventional impressions may be an interesting option in oral rehabilitation with implants [8,21].
The objectives of this in vitro study are to evaluate the accuracy of digital implant impressions in full-arch implant rehabilitation through the use of two silicones, corresponding stone casts and two laboratory scanners. The null hypotheses are that (1) the scanner, (2) silicone and (3) pouring dental cast do not affect the trueness of the impressions.
2. Materials and Methods
Six Straumann bone-level 4.1 implants, each with an internal hexagonal connection (Institut Straumann AG, Basel, Switzerland) and the corresponding screw-retained abutments (SRA) (Institut Straumann AG, Basel, Switzerland), were placed in an artificial mandibular with artificial gingiva, simulating a clinical situation. A 12-megapixel reference scanner was used to scan the master cast (Gom Atos Compact Scan 12 M, GOM Metrology, Braunschweig, Germany). The scan was stored in an STL file and considered the digital master cast (Figure 1).
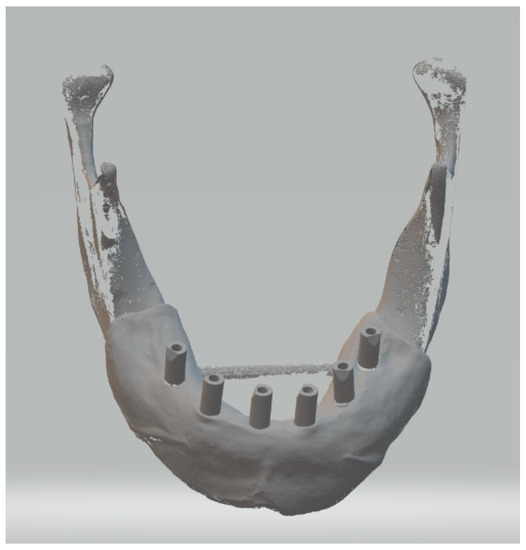
Figure 1.
Digital master cast used in this study.
Based on the master cast, impressions were taken using two silicones with open trays and splinted copings using the double-mix technique. In Group A, 10 impressions were taken using Light Body Type III and Heavy Body Type I silicones (Hydrorise Implant, Zhermack, Rovigo, Italy). In Group B, 10 impressions were taken using Light Body Type III and Heavy Body Type I silicones (Coltene, Altstätten, Switzerland). The trays were made using 3D printing and pre-coated with a silicone adhesive (Coltene, Altstätten, Switzerland) prior to taking the impressions. The workflow is shown in Figure 2. The copings were tightened at 15 Ncm into the SRAs and splinted with methylmethacrylate (Figure 3). After 24 h of polymerization, the splint was sectioned, and additional resin was added in small amounts. After polymerization, the copings were unscrewed, and the impression was removed from the master cast. Subsequently, any excess impression material and the buccal surface of the impression were carefully trimmed with a scalpel to allow for exposure to light. The impressions were then stored for 8 h at 23 °C. All steps were performed by a single experienced operator.
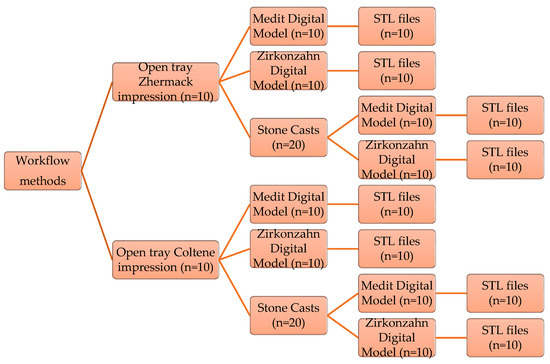
Figure 2.
Stages of the study workflow.

Figure 3.
Master cast with copings splinted with methylmethacrylate.
For the digitalization of the master cast impressions with extraoral scanners, ScanAnalogs (dynamic abutment solutions; Lleida, Spain) were screwed into the copings. TiO2 particles were sprayed to obtain a coating of a minimum thickness on the impressions, according to the ISO-12836 [26]. To digitalize the impressions, two laboratory scanners were used: a blue-LED scanner (Identica T500; Medit, Seoul, Republic of Korea) and a structured-light optical scanner (S600 ARTI; Zirkonzahn, South Tyrol, Italy). The images obtained were stored in STL files (Figure 4).
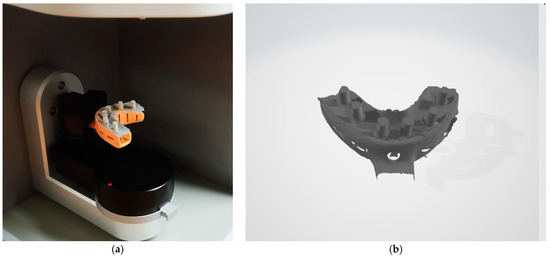
Figure 4.
(a) Digital impression with ScanAnalogs; (b) digital impression—STL File.
Before pouring the gypsum, the ScanAnalogs were removed, and the multiunit analogs were screwed into the transfers. Subsequently, the impressions were cleaned and dried, and artificial gingiva were placed on the impressions (Gingifast elastic, Zhermack). Type IV plaster (Elite Rock; Zhermack) was used for casting, with a water/powder ratio of 20 mL:100 g, according to the manufacturer’s recommendations. The impressions were poured under constant vibration. After 2 h, the impression and cast were separated by unscrewing the transfers.
For digitalization with extraoral scanners, ScanBodies (Institut Straumann AG, Basel, Switzerland) were placed, and the stone casts were sprayed with TiO2 particles. Scanning was carried out using the two described scanners, and the scans were saved in STL files. All scans were performed in a controlled environment. A total of eight digital casts were obtained for the study groups (Table 1).

Table 1.
Definition of the study groups.
The scans obtained were edited in Exocad to place digital replicas corresponding to the ScanBodies and ScanAnalogs used. After this process, the files were exported as STL files with the virtual position of each implant (Figure 5). Best-fit superimpositions were performed between the scans of the impressions and the models obtained with the two scanners and the master model through the use of a 3D analysis software (Geomagic Control X 2022.0.1, 3D Systems, Rock Hill, SC, USA). For each analysis, the overall RMS (root mean square) was calculated as a measure of accuracy. The RMS values represent the average of the negative and positives values through the use of the following formula:
where represents the sum of the measured points, and and are the measurement points of the master cast and the virtual cast compared, respectively.
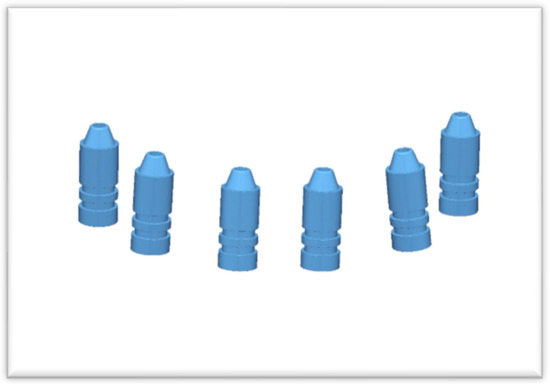
Figure 5.
Virtual position of each implant in the master cast.
The obtained data are described as median and interquartile range (IQR) values or mean ± confidence interval (CI) values at 95% for the different groups. The Shapiro–Wilk test was used to determine the normality of the distributions, and the equality of variance was determined via the Levene test. The discrepancies between groups were compared via the nonparametric Mann–Whitney U test (α = 0.05). A statistically significant at p < 0.05 was used. A statistical analysis was performed with the software SPSS 25.0 (SPSS Inc., Chicago, IL, USA).
3. Results
Overall best-fit measurements were performed between the 80 virtual models and the master model. The RMS values were presented in Table 2 and Figure 6. For the impression groups, the RMS values ranged between 69.90 and 87.43 µm, and for the stone-cast groups, they ranged between 81.74 and 110.62 µm.

Table 2.
Accuracy (RMS ± 95% CI) in µm between each group and the master model.
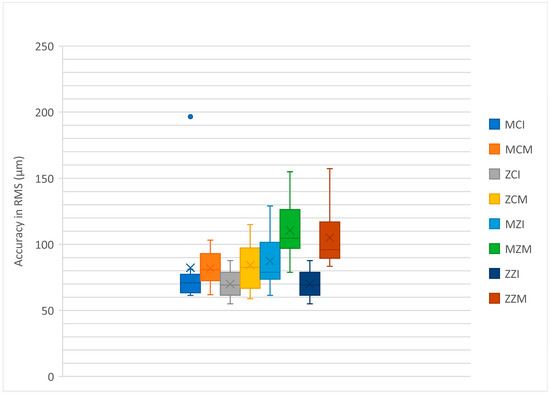
Figure 6.
Boxplot diagram of the study groups.
The Mann–Whitney U test did not show statistically significant differences between the STLs achieved with the Identica T500 Medit® and S600 ARTI Zirkonzhan scanners for the comparison between the silicones (groups MZI vs. ZZI, p = 0.384 and groups MCI vs. ZCI, p = 0.705) and between the stone casts (groups MZM vs. ZZM, p = 0.406 and groups MCM vs. ZCM, p = 0.821).
No statistically significant differences were observed for the Medit scanner (Mann–Whitney U, p = 0.112) and the Zirkonzhan scanner (Mann–Whitney U, p = 0.162) when comparing the two silicones studied (groups MCI vs. MZI and ZCI vs. ZCI). The stone casts (groups MCM vs. MZM and ZCM vs. ZZM) presented statistically significant differences for both the Medit scanner (Mann–Whitney U, p = 0.005) and the Zirkonzhan scanner (Mann–Whitney U, p = 0.041), with the best results found for the stone casts from the Coltene silicone.
Mann–Whitney U tests were used to compare the silicone impressions and the corresponding stone casts without statistically significant differences between the Coltene® silicone impressions and the corresponding digitized stone casts acquired with the Medit® (groups MCI vs. MCM, p = 0.096) and Zirkonzhan® scanners (grupos ZCI vs. ZCM, p = 0.059). The accuracy of the impressions made with Zhermack® silicone was higher than the corresponding stone casts for both scanners (groups MZI vs. MZM, p = 0.019 and groups ZZI vs. ZZM, p = 0.002).
4. Discussion
This study did not identify statistically significant differences between the extraoral scanners used, between the impression materials or between the Coltene silicone and the corresponding stone casts. Thus, the first two null hypothesis are accepted, and the third null hypothesis is partially rejected, since statistically significant differences were reported for the Zhermack silicone when compared with the corresponding stone casts.
Accuracy is defined by trueness and precision as precision corresponds to reproducibility between repeated measurements and trueness describes the closeness of real dimensions [20,21]. To evaluate the accuracy between the master model and the virtual models, a digital software (Geomagic X) with a best-fit superimposition algorithm was used. This method has been recommended for accuracy analysis, although some authors report that it does not adequately show real divergences as positive and negative deviations between reference and virtual models could drive results to cancel each other out [15,22,23,24]. On the other hand, the global best-fit superposition also does not allow one to determine the direction of the discrepancies [6]. Another technique used is the local best-fit superposition in which certain areas of overlap are defined. Nevertheless, the global best-fit algorithm presents a higher degree of repeatability, whereas the local best-fit algorithm involves error-prone manual selection. [24].
The use of rigid custom trays is not a critical factor in the accuracy of implant impressions because elastomeric materials have high degrees of dimensional stability and satisfactory degrees of inherent rigidity [15]. However, in our study, we used rigid custom trays with holes to accommodate the impression copings to facilitate and standardize the impressions made. Splinted open-tray impressions were used in our study and were found to be more accurate than non-splinting closed-tray impressions for completely edentulous patients [20]. However, the splinting technique used in this study to minimize polymerization shrinkage cannot be used in full-arch immediate-loading implant protocols. The sectioning of the splint 24 h after polymerization and the subsequently addition of more resin would require a second appointment [4]. Regarding the impression material, both polyethers (PEs) and polyvinylsiloxanes (PVSs) are excellent impression materials for implant rehabilitations [4]. In the present study, all the impressions were made using polyvinylsiloxanes.
A study by Banjar et al. showed RMS values of 85.9 ± 30.2 µm in the best-fit superimposition of stone casts created using an intraoral scanner [9]. In our study, in the silicone groups, the RMS values ranged between 69.90 and 87.43 µm. This study also showed RMS values of 111.8 ± 26.1 µm in casts printed with a stereolithographic 3D printer [9]. In our study, in the stone model groups, the RMS values ranged between 81.74 and 110.62 µm.
The optical impressions proved to be reliable for short-spans cases. However, when considering long-span cases with more than five implants, the accuracy of the impressions made via intraoral scanning is not comparable to the accuracy of the conventional impressions [22]. In these cases, the use of laboratory scanners for the digitalization of impressions can be a valid alternative, as demonstrated in our study in which it showed better accuracy than the corresponding stone casts for one of the studied elastomers, Zhermack silicone. In the present study, the differences between the Coltene and Zhermack groups might be related to differences in optical or mechanical properties between the silicones. However, this information is not supported by the literature.
The digital acquisition of implant impressions allows for the elimination of some laboratory phases, leading to error reduction. In IOS, the larger the area to scan, the more images must be overlapped, accumulating distortions of the generated area. Laboratory scanners do not reveal this pattern since large parts of the impression are simultaneously captured, minimizing the effect of error [20]. Furthermore, it is difficult to acquire accurate scans due to narrow and deep shapes that may be hidden in the impressions [8]. However, in impressions from completely edentulous patients, there are no deep surfaces, which increases the scan accuracy potential [27]. Also, screwing the ScanAnalog into the coping might be easier in edentulous arches.
In addition to accuracy, there are some limitations for a complete digital workflow in full-arch implant rehabilitation which are mostly related to digital facebows and the virtual articulation of the casts [20].
One of the limitations of this study is the use of an antireflective spray, which may increase discrepancies in ScanBodies and ScanAnalogs scanning.
Another limitation of our study is the use of a reference model designed with parallel multiunits of the same brand, given that the results could be different if some or all of them had very subgingival angulations or positions. However, it should be noted that in full-arch impressions, the appropriate selection of the abutment often allows for the correction of the most unfavorable situations [24]. In addition, further in vivo research is required.
The use of rotational ScanBodies in this investigation does not allow one to extrapolate the results in terms of accuracy for single rehabilitations. This was limited by the fact that the brand of the implants used did not present a non-rotational digital library for the multiunits used since their indication is for non-unitary clinical situations. Further investigations with non-rotation ScanBodies may increase clinical indications for the techniques used in our study. Also, the potential wear on scanBodies and scanAnalogs due to repeated tightening may affect the accuracy [20]. In our study, we changed these components every five uses; however, this parameter was not assessed in this investigation.
Taking into account that for long-span scanning, the IOS cannot achieve the necessary accuracy for implant rehabilitations, more studies on the digitization of conventional impressions should be carried out, especially for trans-arch implants. In the future, clinical decision making between IOS and scanning impressions should be based on several aspects, such as number of implants or the distances between implants.
These promising results allow for the execution of new investigations into the impact of discrepancies found in the passivity of structures in implant-supported prostheses. More studies are needed with respect to the complete CAD-CAM process.
5. Conclusions
When observing the limitations of this in vitro study, we conclude that there are no statistically significant differences in digitization between the scanners evaluated, nor between the types of silicone studied. Regarding the differences between the impressions and stone casts, the scanning impressions showed better accuracy than the scanning stone casts only for one of the elastomers studied, Zhermack silicone.
The extraoral scanning of impressions in edentulous dental arches with six implants proves to be a valid technique and can potentially be used to build implant-supported prostheses.
Author Contributions
Conceptualization, M.A.S.-F.; methodology, R.P., P.R.A. and D.M.; software, P.R.A.; validation, M.A.S.-F. and M.H.F.; formal analysis, M.A.S.-F.; investigation, M.A.S.-F. and D.M.; resources, M.A.S.-F.; data curation, M.M.S.-F.; writing—original draft preparation, M.A.S.-F.; writing—review and editing, D.M.; visualization, M.H.F.; supervision, M.H.F.; project administration, D.M. and M.H.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef]
- Zeller, S.; Guichet, D.; Kontogiorgos, E.; Nagy, W.W. Accuracy of three digital workflows for implant abutment and crown fabrication using a digital measuring technique. J. Prosthet. Dent. 2019, 121, 276–284. [Google Scholar] [CrossRef]
- Patzelt, S.B.; Lamprinos, C.; Stampf, S.; Att, W. The time efficiency of intraoral scanners: An in vitro comparative study. J. Am. Dent. Assoc. 2014, 145, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Setti, P.; Pera, F.; Pera, P.; Pesce, P. Accuracy of multi-unit implant impression: Traditional techniques versus a digital procedure. Clin. Oral Investig. 2018, 22, 1253–1262. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. J. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Lee, S.J.; Betensky, R.A.; Gianneschi, G.E.; Gallucci, G.O. Accuracy of digital versus conventional implant impressions. Clin. Oral Implant. Res. 2015, 26, 715–719. [Google Scholar] [CrossRef]
- Ren, X.; Son, K.; Lee, K. Accuracy of proximal and occlusal contacts of single implant crowns fabricated using different digital scan methods: An in vitro study. Materials 2021, 14, 2843. [Google Scholar] [CrossRef]
- Sampaio-Fernandes, M.A.; Pinto, R.; Sampaio-Fernandes, M.M.; Sampaio-Fernandes, J.C.; Marques, D.; Figueiral, M.H. Accuracy of silicone impressions and stone models using two laboratory scanners: A 3D evaluation. Int. J. Prosthodont. 2022; ahead of print. [Google Scholar] [CrossRef]
- Banjar, A.; Chen, Y.W.; Kostagianni, A.; Finkelman, M.; Papathanasiou, A.; Chochlidakis, K.; Papaspyridakos, P. Accuracy of 3D printed implant casts versus stone casts: A comparative study in the anterior maxilla. J. Prosthodont. 2021, 30, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Runkel, C.; Güth, J.F.; Erdelt, K.; Keul, C. Digital impressions in dentistry—Accuracy of impression digitalisation by desktop scanners. Clin. Oral Investig. 2020, 24, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, Y.; Koizumi, H.; Furuchi, M.; Sato, Y.; Ohkubo, C.; Matsumura, H. Use of digital impression systems with intraoral scanners for fabricating restorations and fixed dental prostheses. J. Oral Sci. 2018, 60, 1–7. [Google Scholar] [CrossRef]
- García-Martínez, I.; CáceresMonllor, D.; Solaberrieta, E.; Ferreiroa, A.; Pradíes, G. Accuracy of digitization obtained from scannable and nonscannable elastomeric impression materials. J. Prosthet. Dent. 2021, 125, 300–306. [Google Scholar] [CrossRef]
- Guth, J.F.; Keul, C.; Stimmelmayr, M.; Beuer, F.; Edelhoff, D. Accuracy of digital models obtained by direct and indirect data capturing. Clin. Oral Investig. 2013, 17, 1201–1208. [Google Scholar] [CrossRef]
- Mandelli, F.; Gherlone, E.; Gastaldi, G.; Ferrari, M. Evaluation of the accuracy of extraoral laboratory scanners with a single-tooth abutment model: A 3D analysis. J. Prosthodont. Res. 2017, 61, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; So, J.S.; Hochstedler, J.L.; Ercoli, C. The accuracy of implant impressions: A systematic review. J. Investig. Clin. Dent. 2008, 100, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Giménez, B.; Ozcan, M.; Martinez-Rus, F.; Pradies, G. Accuracy of a digital impression system based on parallel confocal laser technology for implants with consideration of operator experience and implant angulation and depth. Int. J. Oral Maxillofac. Implant. 2014, 29, 853–862. [Google Scholar] [CrossRef]
- Imburgia, M.; Logozzo, S.; Hauschild, U.; Veronesi, G.; Mangano, C.; Mangano, F.G. Accuracy of four intraoral scanners in oral implantology: A comparative in vitro study. BMC Oral Health 2017, 17, 92. [Google Scholar] [CrossRef] [PubMed]
- Giménez, B.; Özcan, M.; Martínez-Rus, F.; Pradíes, G. Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin. Implant. Dent. Relat. Res. 2015, 17 (Suppl. S1), 54–64. [Google Scholar] [CrossRef] [PubMed]
- Baig, M.R.; Buzayan, M.M.; Yunus, N. Accuracy of a new elastomeric impression material for complete-arch dental implant impressions. J. Investig. Clin. Dent. 2018, 9, 12320. [Google Scholar] [CrossRef]
- Amin, S.; Weber, H.P.; Finkelman, M.; El Rafie, K.; Kudara, Y.; Papaspyridakos, P. Digital vs. conventional full-arch implant impressions: A comparative study. Clin. Oral Impl Res. 2017, 28, 1360–1367. [Google Scholar] [CrossRef]
- Abou-Ayash, S.; Mathey, A.; Gäumann, F.; Mathey, A.; Donmez, M.B.; Yilmaz, B. In vitro scan accuracy and time efficiency in various implant-supported fixed partial denture situations. J. Dent. 2022, 128, 104358. [Google Scholar] [CrossRef]
- Bi, C.; Wang, X.; Tian, F.; Qu, Z.; Zhao, J. Comparison of accuracy between digital and conventional implant impressions: Two and three dimensional evaluations. J. Adv. Prosthodont. 2022, 14, 236–249. [Google Scholar] [CrossRef]
- Michelinakis, G.; Apostolakis, D.; Kamposiora, P.; Papavasiliou, G.; Özcan, M. The direct digital workflow in fixed implant prosthodontics: A narrative review. BMC Oral. Health 2021, 21, 37. [Google Scholar] [CrossRef] [PubMed]
- Natsubori, R.; Fukazawa, S.; Chiba, T.; Tanabe, N.; Kihara, H.; Kondo, H. In vitro comparative analysis of scanning accuracy of intraoral and laboratory scanners in measuring the distance between multiple implants. Int. J. Implant. Dent. 2022, 8, 18. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.H.; Lee, K.T.; Kim, H.Y.; Kim, J.H.; Kim, W.C. White light scanner-based repeatability of 3-dimensional digitizing of silicon rubber abutment teeth impressions. J. Adv. Prosthodont. 2013, 5, 452–456. [Google Scholar] [CrossRef]
- ISO 12836:2015; Dentistry—Digitizing Devices for CAD/CAM Systems for Indirect Dental Restorations—Test Methods for Assessing Accuracy. ISO Publication: Geneva, Switzerland, 2015.
- Leggeri, A.; Carosi, P.; Mazzetti, V.; Arcuri, C.; Lorenzi, C. Techniques to Improve the Accuracy of Intraoral Digital Impression in Complete Edentulous Arches: A Narrative Review. Appl. Sci. 2023, 13, 7068. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).