Abstract
This study aimed to compare subjective and objective measures of physical activity (PA) in healthcare professionals and assess their adherence to recommended guidelines. A convenience sample of 153 female healthcare professionals (51 nurses, 50 medical caregivers, and 52 physiotherapists) from 24 h healthcare facilities in Poland participated in the study. Subjective assessment was done using an expanded version of the International Physical Activity Questionnaire, while objective assessment involved wearing an Actigraph GT3X accelerometer for seven consecutive days. The results showed no significant correlation between subjective and objective measures of moderate-to-vigorous PA in both occupational and non-occupational activities. Objectively measured PA was significantly lower than self-reported PA, with a large effect size observed for both occupational and total PA. Only 44% of participants met the recommended guidelines for aerobic activity based on accelerometer data, while subjective assessment showed a higher percentage (76%) of healthcare professionals meeting the guidelines. These findings highlight the discrepancy between self-reported and objectively measured PA in healthcare professionals. It emphasizes the need for more accurate assessment methods to understand the actual PA levels of this population. Further research should explore factors influencing PA reporting accuracy and develop interventions to promote regular physical activity among healthcare professionals.
1. Introduction
Regular physical exercise offers numerous health benefits, making the promotion of physical activity a major focus in the field of public health [1,2,3]. Healthcare professionals, including medical doctors, nurses, primary care physicians, and physiotherapists, have a significant role to play in actively promoting physical activity [4,5]. These professionals are expected to possess a comprehensive understanding of healthy behaviors, enabling them to provide counseling and advocate for healthy lifestyles, particularly among populations at higher risk for poor health due to physical inactivity [6,7].
In addition to their knowledge, healthcare professionals should demonstrate high levels of motivation and the ability to engage in health-promoting activities in order to take care of their own well-being [8,9]. The literature emphasizes that healthcare personnel, apart from their understanding of health, diseases, and their determinants, should also lead by example and adopt appropriate lifestyles to serve as role models [5,10,11,12]. Such behavior not only helps in reducing the incidence of diseases among healthcare professionals themselves but also positively influences the patients they care for. The International Council of Nurses (INC) recognizes the significant impact nurses have in influencing people’s health and preventing diseases, through primary prevention strategies and setting an example for others to follow [13,14].
Maintaining a healthy level of physical activity is particularly important for individuals whose work involves repetitive, unidirectional movements with physical exertion, prolonged maintenance of forced and static positions, and tasks such as lifting or carrying heavy objects or people. Healthcare professionals, due to the nature of their work, often fall into this category [15,16,17,18,19]. Moreover, the irregular work schedules of healthcare professionals, including shift work, disrupt their sleep patterns, rest periods, and dietary routines, which can lead to irregular nutrition and further impact their overall health [20,21,22,23,24].
Various studies have explored the attitudes of healthcare professionals toward health behaviors, revealing mixed findings [25,26,27,28,29]. Despite their awareness of the importance of regular physical activity, medical professionals exhibit similar engagement levels as the general population. In other words, less than half of healthcare personnel report participating in regular physical exercise [30,31,32,33,34,35,36].
Most scientific reports on the physical workload associated with healthcare professionals have relied primarily on subjective measurement methods, which have been criticized by researchers for often leading to overestimations [37,38,39,40]. Consequently, this study aims to compare the parameters of self-reported and actual physical activity among female healthcare professionals. By employing more objective measures, this study seeks to provide a more accurate understanding of the levels of physical activity in this professional group.
One important aspect to consider when studying the promotion of physical activity among healthcare professionals is the chosen study population. In this study, we specifically focus on female healthcare professionals. This choice is motivated by the fact that women account for a substantial proportion of the global health and social care workforce. Studying the physical activity levels of female healthcare professionals is crucial for understanding the challenges they encounter in maintaining regular exercise. Women in this field often balance multiple personal and professional responsibilities, making it difficult to prioritize an active lifestyle. By comprehending the unique circumstances they face, we can develop targeted interventions and strategies that effectively promote physical activity within this population.
In light of the above, it is evident that promoting physical activity among healthcare professionals is crucial for improving public health outcomes. These professionals have a unique position to influence the health behaviors of their patients and should serve as role models by adopting healthy lifestyles themselves. Given the physical demands and irregular work schedules experienced by healthcare professionals, it is essential to investigate their actual levels of physical activity using objective measures.
Physical activity (PA) is a key factor in maintaining overall health and well-being. For healthcare professionals who often work in physically demanding conditions, adhering to recommended PA guidelines is crucial. The World Health Organization recommends that adults aged 18–64 should perform at least 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity throughout the week or an equivalent combination of moderate- and vigorous-intensity activity [WHO]. Despite their awareness of these guidelines, studies have shown that less than half of healthcare professionals meet these recommendations [41].
This study aims to analyze the PA patterns of female healthcare professionals more accurately. Specifically, our objectives are to (1) compare self-reported and objectively measured PA levels; (2) evaluate whether they meet PA guidelines; and (3) identify any factors that might affect PA levels.
2. Materials and Methods
The hypothesis of this study is that there is a discrepancy between the self-reported and objectively measured levels of physical activity among female healthcare professionals. It is hypothesized that the self-reported levels of physical activity will generally be higher than the objectively measured levels.
2.1. Study Design and Sample
This cross-sectional study employed a rigorous research design to examine the experiences of healthcare professionals in the Upper Silesian agglomeration of Poland. A convenience sampling approach was utilized to recruit a diverse sample of participants from various healthcare disciplines. A total of 153 healthcare professionals participated in the study, including 51 nurses, 50 medical caregivers, and 52 physiotherapists.
The study was conducted in sixteen 24 h healthcare facilities located in five cities: Katowice, Ruda Śląska, Chorzów, Świętochłowice, and Tarnowskie Góry. These cities were selected to ensure geographical representation within the Upper Silesian agglomeration and capture a range of healthcare settings.
2.2. Participant Selection Criteria
To ensure the relevance and reliability of the study findings, stringent inclusion criteria were established for participant selection. The following criteria had to be met for individuals to be included in the study:
- -
- Willingness to participate: Participants were required to express their voluntary agreement to participate in the entire research program. This ensured their commitment and dedication to the study objectives.
- -
- Professional experience: Participants needed to have a minimum of three years of experience as a nurse, medical caregiver, or physiotherapist. This criterion aimed to include healthcare professionals with sufficient practical knowledge and expertise in their respective roles.
- -
- Employment in 24 h healthcare facilities: Participants were specifically chosen from healthcare facilities that provided round-the-clock healthcare services. This criterion aimed to capture the experiences of professionals working in demanding and high-pressure environments.
- -
- Direct patient care responsibilities: Participants’ roles had to involve direct interaction with patients and the provision of care. This criterion ensured that the study focused on professionals who had regular and significant patient contact, allowing for a comprehensive exploration of their experiences.
2.3. Sociodemographic Characterization
The study included 153 female participants, ranging in age from 25 to 60 years. To provide a comprehensive overview of the sample, relevant sociodemographic information was collected. Table 1 presents the sociodemographic characteristics of the study participants, including age distribution, educational background, years of experience, and employment status.

Table 1.
Sociodemographic and personal characteristics of female healthcare professionals.
By employing a rigorous study design and adhering to stringent participant selection criteria, this research aimed to provide valuable insights into the experiences of healthcare professionals in the Upper Silesian agglomeration of Poland.
2.4. Subjective Assessment of Physical Activity
To evaluate the participants’ perceptions of their physical activity, we used an expanded version of the International Physical Activity Questionnaire (IPAQ). The IPAQ is a well-validated tool designed to measure health-related physical activity in populations [37]. The expanded version of the IPAQ used in this study included 27 items that cover four primary domains of physical activity: (1) work-related activities, (2) transportation-related activities, (3) household chores and gardening, and (4) leisure-time activities.
In each domain, participants were asked to provide information regarding the frequency (number of days in a week) and duration (hours and minutes per day) of their involvement in three types of activities: light-intensity, moderate-intensity activities, and vigorous-intensity activities.
The results from the IPAQ were modified and divided into two categories: occupational and Non-occupational physical Activity.
To ensure accuracy and clarity in evaluating the intensity of physical exercise, direct interviews were conducted with the respondents as a means of validation. This methodological choice facilitated the opportunity to address any doubts or uncertainties that participants may have experienced during the assessment process. By conducting face-to-face interviews, the research team was able to offer guidance and clarification, thereby enhancing the reliability of the subjective assessment of physical activity.
2.5. Objective Assessment of Physical Activity
For the purpose of objectively assessing participants’ physical activity levels, the Actigraph GT3X accelerometer was selected as the measurement tool. This accelerometer, developed by ActiGraph LLC in Pensacola, FL, USA, is widely recognized and has undergone rigorous validation processes, ensuring its reliability in measuring physical activity. By utilizing this device, the researchers aimed to obtain accurate and trustworthy measurements of participants’ physical activity behaviors.
To facilitate precise and comprehensive data collection, the Actigraph GT3X accelerometer was positioned securely on the participant’s right hip, attached to a waistband. This placement ensured that the accelerometer remained in a consistent and stable position throughout the study period, allowing for uninterrupted monitoring of physical activity. Participants were instructed to wear the device continuously for seven consecutive days, except during water-based activities.
To ensure meticulous data capture, the Actigraph GT3X accelerometer was programmed to collect data at a sampling rate of 60 Hz. This high-frequency sampling provided detailed information about participants’ movement patterns and physical activity levels throughout the entire day. By recording raw acceleration data in 60-s epochs, the researchers were able to capture the nuances and variations in participants’ physical activity behaviors with greater precision. The cut-points used for classifying PA intensity were selected in accordance with the ActiLife software guidelines: light-intensity (200–2689 counts per minute), moderate-intensity (2690–6166 counts per minute), and vigorous-intensity (6167 and above counts per minute).
The selection of the Actigraph GT3X accelerometer as the objective assessment method offered notable advantages over subjective self-report measures commonly used in previous studies. One significant advantage was the elimination of recall bias, which often affects self-reported data due to participants’ imperfect memory of their physical activity. Additionally, this objective assessment method allowed for the accurate measurement of both the intensity and duration of participants’ physical activities, providing a more comprehensive understanding of their actual engagement in physical activity.
The portability and non-intrusiveness of the Actigraph GT3X accelerometer were crucial considerations in its selection. Its compact size and lightweight design ensured minimal interference with participants’ daily routines, allowing for a natural and realistic representation of their physical activity behaviors. Participants were able to carry out their usual activities without significant disruptions while wearing the accelerometer, which enhanced the ecological validity of the study.
In summary, the utilization of the Actigraph GT3X accelerometer in this study offered a robust and scientifically rigorous approach to objectively assess participants’ physical activity levels. Its reliability, accuracy, and non-invasive nature made it an ideal tool for capturing precise data on participants’ physical activity behaviors. This objective assessment method provided valuable insights into the actual engagement of participants in physical activities and contributed to a more comprehensive understanding of their physical activity patterns.
2.6. Data Processing
The initial stage of the study encompassed the acquisition and subsequent processing of the unprocessed accelerometer data. To accomplish this, we employed the ActiLife 5 software (ActiGraph LLC, Pensacola, FL, USA) as our tool of choice. This software provided a comprehensive suite of functionalities that proved instrumental in the manipulation and analysis of the acquired data. Specifically, it facilitated the meticulous removal of non-wear time, which entailed identifying and eliminating periods lasting 60 or more consecutive minutes exhibiting zero counts. Additionally, it allowed for the exclusion of time intervals when the accelerometer was not worn by the participants. The raw data were then subjected to a conversion process utilizing the default filter settings of the ActiLife software, resulting in the transformation of the data into activity counts.
In order to ascertain the intensity of physical activity, we utilized the activity counts per minute (cpm) as a quantifiable metric. This enabled us to delineate three distinct tiers of physical activity intensity: light intensity (200–2689 cpm), moderate intensity (2689–6166 cpm), and vigorous intensity (≥6167 cpm).
It is worth noting that the female healthcare workers participating in the study were explicitly instructed to maintain their usual physical activity patterns while wearing the device. Once the device was returned, we administered a comprehensive questionnaire survey to the participants, focusing on the specific week during which the participants wore the accelerometers. Consistent with the criterion stipulated in the IPAQ questionnaire, only exercise sessions lasting a minimum of 10 min were considered when evaluating the cumulative weekly duration of healthy physical activity.
In addition to the questionnaire, we requested the participants to diligently maintain daily physical activity logs. These logs served as a detailed record, documenting the duration, nature, and intensity of both occupational and non-occupational physical activities engaged by the participants. Consequently, this meticulous documentation facilitated the categorization of the participants’ overall weekly physical activity into two distinct domains: occupational physical activity (oPA), representing physical exertion during working hours, and non-occupational physical activity (noPA), encompassing physical activities performed outside of work-related obligations.
The interpretation of the obtained results was predicated upon established guidelines delineating healthy levels of physical activity. Central to this analysis was the determination of the percentage of healthcare professionals who successfully adhered to the recommended threshold of 150 min of moderate-to-vigorous physical activity per week.
Given the distinctive nature of physical activities within healthcare professions and the compelling scientific evidence underscoring the detrimental impact of occupational, physical activity on health outcomes, we deemed it imperative to delineate and evaluate physical activity patterns in terms of their occupational and non-occupational components.
2.7. Statistical Methods
The obtained results underwent rigorous statistical analysis to provide a comprehensive understanding of the data. Various statistical measures were employed, including arithmetic means (), standard deviations (SD), minimum (min), and maximum (max) values, to describe the central tendency and dispersion of the observed variables.
Furthermore, the relationship between subjectively and objectively measured physical activity was assessed using the Spearman correlation, which measures the strength and direction of the association between two variables. This allowed us to investigate the extent to which subjective and objective measures of physical activity align with each other.
The Wilcoxon signed-rank test was utilized to determine the differences between physical activity data collected from questionnaires and accelerometers. This non-parametric test takes into account the paired nature of the data and provides insights into whether there are significant disparities between the two measurement methods. Additionally, the matched-pairs rank biserial correlation coefficient effect size for the paired Wilcoxon signed-rank test was calculated, offering a standardized measure of the effect observed.
Moreover, the association between the subjective and objective assessment tools and the extent to which participants met physical activity recommendations was examined using the chi-squared test of independence. This statistical test enabled us to assess whether there is a significant relationship between the assessment tools and the achievement of physical activity guidelines.
A significance value of p = 0.05 was set to determine the statistical significance of the results. This threshold indicates that findings with p-values less than 0.05 were considered statistically significant, providing evidence to reject the null hypothesis.
All statistical analyses were performed using IBM SPSS software version 21, a widely recognized and robust tool for statistical analysis in the scientific community.
3. Results
The Spearman correlation analysis revealed that no significant relationship was observed between subjectively and objectively measured levels of moderate-to-vigorous physical activity (MVPA) in both occupational and non-occupational contexts. Specifically, for occupational, physical activity, the Spearman correlation coefficient (RS) was found to be 0.11 (p = 0.321) in a sample of 78 participants. Similarly, for non-occupational physical activity, the RS value was −0.11 (p = 0.254) in a sample of 111 participants (Table 2). These results suggest a weak positive relationship between subjective and objective measures of occupational PA and a weak negative relationship for non-occupational PA. However, neither correlation was statistically significant.

Table 2.
The relationship between subjectively and objectively measured physical activity.
Regarding the measured recommended physical activity, which encompasses total MVPA, no significant correlation was observed with the health personnel’s self-assessment. It is worth noting, however, that a weak positive correlation was identified between light physical activity and total physical activity. This weak positive correlation can be attributed to the dominance of low-intensity activities within the participants’ total weekly physical activity.
The statistical analysis of our study, using a Wilcoxon signed rank test, revealed a significant difference between objectively measured physical activity and the self-reported physical activity levels declared by the participants within the same week. This significant difference was observed regardless of the type and intensity of physical activity performed (Table 3).

Table 3.
Differences between subjective and objective measured levels of physical activity.
The effect size was calculated using the Wilcoxon effect size (Rc). In the case of occupational PA, the Rc was −0.61, indicating a large effect size. Similarly, for total PA, the Rc was also −0.61, signifying a large effect size. These large effect sizes suggest a considerable discrepancy between self-reported and objectively measured PA levels, emphasizing the importance of utilizing objective measurement tools for accurate PA assessment in healthcare professionals.
In terms of overall physical activity levels, the average recommended amount of physical activity based on accelerometer measurements was found to be 158 min per week for moderate-to-vigorous physical activity (MVPA). However, participants self-reported a significantly higher weekly MVPA of 271 min (Table 3). This disparity highlights the tendency for individuals to overestimate their level of physical activity when relying on self-reporting methods.
The statistical analysis conducted using the chi-squared test revealed that the association between meeting physical activity recommendations, as assessed through subjective and objective measurements, did not reach statistical significance (Figure 1). This implies that there is no compelling evidence to support a significant relationship between the two assessment methods in terms of determining whether individuals meet the recommended levels of physical activity.
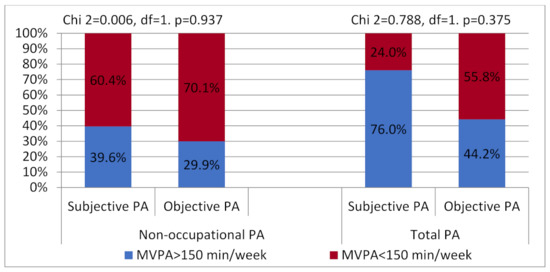
Figure 1.
The relationship between meeting physical activity recommendations using subjective and objective assessment.
4. Discussion
Physical activity is an important aspect of maintaining good health and reducing the risk of chronic diseases. However, measuring physical activity can be challenging as it can be assessed both subjectively (e.g., through self-reporting) and objectively (e.g., using wearable devices). The relationship between the subjective and objective assessment of physical activity in health personnel is an important topic, as health personnel is often involved in promoting physical activity to their patients.
In our conducted study, we discovered that there existed no statistically significant correlation between the physical activity (PA) as reported subjectively and the same activity objectively measured. Moreover, it was observed that the self-reported levels of physical activity were notably higher across all categories of activity, encompassing occupational, non-occupational, and overall physical activity. These outcomes closely resembled the findings of Lee et al. [42], who also identified an absence of substantial association between self-reported and objectively measured physical activity. It is worth noting that the overestimation of self-reported physical activity levels is a frequently encountered phenomenon, thereby leading to the potential for misleading assessments concerning the true levels of individuals’ physical activity. The disparities existing between subjective and objective measurements of physical activity have been consistently underscored in various scientific studies [42,43,44,45,46].
In our study, we found that the average recommended level of physical activity, as measured by accelerometers, amounted to 158 min per week. This duration surpasses the health guidelines set by the World Health Organization (WHO) for maintaining optimal well-being. This noteworthy disparity underscores the significance of physical activity in promoting good health and highlights the need to encourage individuals to engage in regular exercise. Furthermore, our investigation revealed that a considerable proportion of moderate-to-vigorous physical activity (MVPA) was carried out during non-working hours. This observation is particularly noteworthy due to the distinct effects that different types of physical activity have on an individual’s health and overall well-being. Various scientific studies encompassing diverse populations have extensively examined the health benefits associated with both occupational and leisure-time physical activity [42,47,48,49]. These investigations consistently indicate that engaging in physical activity during leisure time yields greater advantages in terms of health outcomes.
Interestingly, the research conducted by Wolff et al. [50] demonstrated a positive correlation between higher levels of occupational, physical activity among healthcare workers and increased perceptions of job stress and exhaustion. This finding suggests that while occupational, physical activity may offer certain health benefits, it may also contribute to elevated stress levels and feelings of exhaustion among healthcare professionals. In our study, only 44% of health workers monitored by accelerometers met the WHO guidelines for aerobic physical activity. A higher percentage of participants met the criteria for the recommended standards obtained in other studies. Abu Saad et al. [51] classified 54.4% of healthcare workers as sufficiently physically active. In a study published by Song et al. [52] on a population of 1502 healthcare workers, 56.2% met the recommended guidelines for aerobic activity. However, in these studies, physical activity was assessed using subjective assessment (questionnaires). In our research, using subjective assessment, the percentage of participants meeting physical activity guidelines was 76%.
The discrepancy between self-reported and objectively measured physical activity (PA) among healthcare professionals in our study has important implications. Participants reported higher levels of PA than what was objectively measured by the Actigraph GT3X accelerometer. This suggests that healthcare professionals may overestimate their PA when self-reporting, which could influence the design and outcomes of interventions aiming to increase PA in this group. Several factors could contribute to the overestimation of self-reported PA. Recall bias is one potential factor, where participants may not remember their exact PA levels, leading to inaccurate self-reporting. Additionally, social desirability bias may play a role, with participants potentially overreporting their PA to align with societal norms or expectations of health behaviors in healthcare professionals. Misinterpretation of the International Physical Activity Questionnaire (IPAQ) questions could also lead to overreporting. For instance, participants may have different interpretations of what constitutes moderate or vigorous activity, leading them to overestimate their PA levels.
These findings highlight the importance of using objective measures, such as accelerometers, alongside self-report measures to accurately assess PA levels in healthcare professionals. Further research is needed to investigate these potential sources of discrepancy and to develop strategies to improve the accuracy of self-reported PA.
5. Strengths and Limitations
The present study has several strengths that contribute to the robustness of its findings. One significant strength is the utilization of both subjective and objective measurements to assess physical activity levels. By incorporating both self-report measures and objective data from accelerometers, the study provides a more comprehensive evaluation of participants’ physical activity behaviors. This approach helps to mitigate potential biases or inaccuracies that may arise from relying solely on self-reported information. Moreover, the study employed validated measures of physical activity, such as the International Physical Activity Questionnaire (IPAQ) and the Actigraph accelerometer, which enhanced the validity and reliability of the obtained results.
This study has several limitations. First, the use of a convenience sample may limit the generalizability of the findings. Second, selection bias could have occurred if those who chose to participate were more active than those who did not. Finally, the findings may not be generalizable to other healthcare professional populations or geographical locations. Future research should aim to address these limitations. Moreover, viewed from another perspective, the cross-sectional design employed restricts the ability to establish causality or determine the temporal sequence of events. Longitudinal studies would provide more insight into the dynamic nature of physical activity behaviors and their associations with various factors over time.
Additionally, the study lacks specific information on recommended physical activities, particularly regarding strength activities and vigorous physical activities. The absence of this information limits a comprehensive understanding of the participants’ adherence to different types and intensities of physical activity. Including such details would have allowed for a more nuanced interpretation of the findings and a better assessment of participants’ compliance with established guidelines.
Despite these limitations, the study’s inclusion of both subjective and objective measurements, along with the use of validated assessment tools, contributes to its overall strength. However, future research incorporating longitudinal designs and more detailed information on specific types of physical activities could provide a more comprehensive understanding of the physical activity behaviors of healthcare professionals.
6. Conclusions
- 1.
- The findings of the study indicate that there was no statistically significant relationship observed between subjectively reported physical activity and objectively measured physical activity among the female population of health workers included in the research.
- 2.
- When objective measurement methods were employed, it was found that a mere 44% of female health personnel successfully met the aerobic physical activity guidelines set forth by the World Health Organization (WHO).
- 3.
- In order to obtain a more precise and comprehensive evaluation of physical activity levels among female health professionals, it is recommended that objective measures, such as accelerometers or pedometers, be employed in conjunction with self-report measures. This combined approach would enable a more accurate assessment of the levels of physical activity in the target population of health professionals.
Our findings underscore the importance of accurate assessment methods in quantifying physical activity levels among female healthcare professionals. The observed discrepancy between self-reported and objectively measured physical activity points to the potential limitations of relying solely on self-reports. This highlights the need for incorporating objective measures, such as accelerometers, to provide a more accurate representation of actual physical activity levels. The role of healthcare professionals in promoting and modeling healthy behaviors, including regular physical activity, is crucial. Despite the demanding nature of their work, it is essential for healthcare professionals to find ways to integrate physical activity into their lives. Not only does this benefit their own health, but it also positions them as role models for their patients, potentially influencing their patients’ behaviors and health outcomes.
Future Directions
This study suggests several future research directions. Further research should explore factors influencing PA reporting accuracy among healthcare professionals. This could include examining the role of personal characteristics, workplace culture, and environmental factors. Additionally, the research could develop and test interventions designed to promote regular physical activity among healthcare professionals. These interventions could focus on education about the benefits of physical activity, motivation and behavior change strategies, and strategies to integrate physical activity into daily routines.
Author Contributions
Conceptualization, M.N.-J., J.P. and A.N.; methodology, M.N.-J. and A.N.; software, M.N.-J., J.P. and A.N.; validation, M.N.-J.; formal analysis, M.N.-J. and A.N.; investigation, M.N.-J.; resources, M.N.-J.; data curation, M.N.-J.; writing—original draft preparation, M.N.-J.; writing—review and editing, A.N. and J.P.; visualization, J.P.; supervision, A.N.; project administration, A.N.; funding acquisition, J.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the Jerzy Kukuczka Academy of Physical Education in Katowice.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jakicic, J.M.; Kraus, W.E.; Powell, K.E.; Campbell, W.W.; Janz, K.F.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; 2018 Physical Activity Guidelines Advisory Committee. Association between Bout Duration of Physical Activity and Health: Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Jemna, D.-V.; David, M.; Depret, M.-H.; Ancelot, L. Physical Activity and Healthcare Utilization in France: Evidence from the European Health Interview Survey (EHIS) 2014. BMC Public Health 2022, 22, 1355. [Google Scholar] [CrossRef] [PubMed]
- Kraus, W.E.; Janz, K.F.; Powell, K.E.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L.; 2018 Physical Activity Guidelines Advisory Committee. Daily Step Counts for Measuring Physical Activity Exposure and Its Relation to Health. Med. Sci. Sports Exerc. 2019, 51, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka, A.; Niestrój-Jaworska, M.; Mynarski, A.; Polechoński, J. Association Between Objectively Measured Physical Activity And Musculoskeletal Disorders, and Perceived Work Ability among Adult, Middle-Aged and Older Women. Clin. Interv. Aging 2019, 14, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- Niestrój-Jaworska, M.; Dębska-Janus, M.; Polechoński, J.; Tomik, R. Health Behaviors and Health-Related Quality of Life in Female Medical Staff. Int. J. Environ. Res. Public Health 2022, 19, 3896. [Google Scholar] [CrossRef]
- Dębska, M.; Dębski, P.; Polechoński, J.; Rozpara, M.; Tomik, R. The Dark Triad of Personality in the Context of Health Behaviors: Ally or Enemy? Int. J. Environ. Res. Public Health 2021, 18, 4113. [Google Scholar] [CrossRef]
- Teychenne, M.; White, R.L.; Richards, J.; Schuch, F.B.; Rosenbaum, S.; Bennie, J.A. Do We Need Physical Activity Guidelines for Mental Health: What Does the Evidence Tell Us? Ment. Health Phys. Act. 2020, 18, 100315. [Google Scholar] [CrossRef]
- Schenk, L.; Sonntag, P.-T.; Beck, P.; Khan, Z.; Peppler, L.; Schouler-Ocak, M. Organisational and Staff-Related Effects on Cultural Competence in the Hospital Setting: A Cross-Sectional Online Survey of Nursing and Medical Staff. BMC Health Serv. Res. 2022, 22, 644. [Google Scholar] [CrossRef]
- Stanulewicz, N.; Knox, E.; Narayanasamy, M.; Shivji, N.; Khunti, K.; Blake, H. Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 17, 17. [Google Scholar] [CrossRef]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among Healthcare Workers: A Realist Review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef]
- Martin, S.D.; Urban, R.W.; Johnson, A.H.; Magner, D.; Wilson, J.E.; Zhang, Y. Health-Related Behaviors, Self-Rated Health, and Predictors of Stress and Well-Being in Nursing Students. J. Prof. Nurs. 2022, 38, 45–53. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Kelly, S.A.; Stephens, J.; Dhakal, K.; McGovern, C.; Tucker, S.; Hoying, J.; McRae, K.; Ault, S.; Spurlock, E.; et al. Interventions to Improve Mental Health, Well-Being, Physical Health, and Lifestyle Behaviors in Physicians and Nurses: A Systematic Review. Am. J. Health Promot. 2020, 34, 929–941. [Google Scholar] [CrossRef]
- Grabowska, H.; Nowakowska, H.; Grabowski, W.; Gaworska-Krzemińska, A. Funkcja Wychowawcza Pielęgniarki w Aspekcie ICNP. Pielęg. Pol. 2017, 65, 552–557. [Google Scholar] [CrossRef][Green Version]
- Nilsson, J.; Mischo-Kelling, M.; Thiekoetter, A.; Deufert, D.; Mendes, A.C.; Fernandes, A.; Kirchhoff, J.W.; Lepp, M. Nurse Professional Competence (NPC) Assessed among Newly Graduated Nurses in Higher Educational Institutions in Europe. Nord. J. Nurs. Res. 2019, 39, 159–167. [Google Scholar] [CrossRef]
- Clari, M.; Garzaro, G.; Di Maso, M.; Donato, F.; Godono, A.; Paleologo, M.; Dimonte, V.; Pira, E. Upper Limb Work-Related Musculoskeletal Disorders in Operating Room Nurses: A Multicenter Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 2844. [Google Scholar] [CrossRef] [PubMed]
- Min, A.; Min, H.; Hong, H.C. Work Schedule Characteristics and Fatigue among Rotating Shift Nurses in Hospital Setting: An Integrative Review. J. Nurs. Manag. 2019, 27, 884–895. [Google Scholar] [CrossRef]
- Otto, A.-K.; Bischoff, L.L.; Wollesen, B. Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3586. [Google Scholar] [CrossRef] [PubMed]
- Rypicz, Ł.; Karniej, P.; Witczak, I.; Kołcz, A. Evaluation of the Occurrence of Work-Related Musculoskeletal Pain among Anesthesiology, Intensive Care, and Surgical Nurses: An Observational and Descriptive Study. Nurs. Health Sci. 2020, 22, 1056–1064. [Google Scholar] [CrossRef]
- Sharma, F.; Kalra, S.; Rai, R.; Chorsiya, V.; Dular, S. Work-Related Musculoskeletal Disorders, Workability and Its Predictors among Nurses Working in Delhi Hospitals: A Multicentric Survey. J. Clin. Diagn. Res. 2022, 16, 1–6. [Google Scholar] [CrossRef]
- Cheong, Z.Y.; Lopez, V.; Tam, W.S.W. Barriers to Healthy Eating among Nurses Working in Hospitals: A Meta-Synthesis. J. Adv. Nurs. 2022, 78, 314–331. [Google Scholar] [CrossRef]
- Heath, G.; Dorrian, J.; Coates, A. Associations between Shift Type, Sleep, Mood, and Diet in a Group of Shift Working Nurses. Scand. J. Work. Environ. Health 2019, 45, 402–412. [Google Scholar] [CrossRef]
- Horton Dias, C.; Dawson, R.M. Hospital and Shift Work Influences on Nurses’ Dietary Behaviors: A Qualitative Study. Workplace Health Saf. 2020, 68, 374–383. [Google Scholar] [CrossRef]
- Marko, S.; Wylie, S.; Utter, J. Enablers and Barriers to Healthy Eating among Hospital Nurses: A Systematic Review. Int. J. Nurs. Stud. 2023, 138, 104412. [Google Scholar] [CrossRef]
- Pepłońska, B.; Nowak, P.; Trafalska, E. The Association between Night Shift Work and Nutrition Patterns among Nurses: A Literature Review. Med. Pract. 2019, 70, 363–376. [Google Scholar] [CrossRef]
- Berent, D.; Skoneczny, M.; Macander, M.; Wojnar, M. The Association among Health Behaviors, Shift Work and Chronic Morbidity: A Cross-Sectional Study on Nurses Working in Full-Time Positions. J. Public Health Res. 2021, 11, 2099. [Google Scholar] [CrossRef] [PubMed]
- Chiang, S.-L.; Chiang, L.-C.; Tzeng, W.-C.; Lee, M.-S.; Fang, C.-C.; Lin, C.-H.; Lin, C.-H. Impact of Rotating Shifts on Lifestyle Patterns and Perceived Stress among Nurses: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 5235. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.L.; Danaee, M.; Zulkarnain, J. The Association between Physical Activity and Work Schedule among Hospital Nurses: A Cross-Sectional Study. Malays. J. Mov. Health Exerc. 2019, 8, 15–32. [Google Scholar]
- Mazzola, J.J. Barriers to Healthy Nutrition and Exercise Behaviors Among Healthcare Workers. In Mental Health and Wellness in Healthcare Workers: Identifying Risks, Prevention, and Treatment; IGI Global: Hershey, PA, USA, 2022; pp. 82–104. [Google Scholar]
- Terry, D.L.; Mathews, D.P. Social Norms and Engagement in Protective Health Behaviors Among Rural Health Providers. J. Clin. Psychol. Med. Settings 2022, 29, 384–390. [Google Scholar] [CrossRef]
- Bartosiewicz, A.; Łuszczki, E.; Nagórska, M.; Oleksy, Ł.; Stolarczyk, A.; Dereń, K. Risk Factors of Metabolic Syndrome among Polish Nurses. Metabolites 2021, 11, 267. [Google Scholar] [CrossRef]
- Chappel, S.E.; Verswijveren, S.J.J.M.; Aisbett, B.; Considine, J.; Ridgers, N.D. Nurses’ Occupational Physical Activity Levels: A Systematic Review. Int. J. Nurs. Stud. 2017, 73, 52–62. [Google Scholar] [CrossRef]
- Forcada-Parrilla, I.; Reig-Garcia, G.; Serra, L.; Juvinyà-Canal, D. The Influence of Doing Shift Work on the Lifestyle Habits of Primary Care Nurses. Nurs. Rep. 2022, 12, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Panczyk, M.; Woynarowska-So\ldan, M.; Żmuda-Trzebiatowska, H.; Gotlib, J. Health-Enhancing Behaviours of Nurses in Poland and Their Association with Shift Work and Age. Collegian 2018, 25, 255–261. [Google Scholar] [CrossRef]
- Priano, S.M.; Hong, O.S.; Chen, J.-L. Lifestyles and Health-Related Outcomes of U.S. Hospital Nurses: A Systematic Review. Nurs. Outlook 2018, 66, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Scheit, L.; Schröder, J.; Wolf, K.H.; Richter, T.H.; Busch, C.; Beer, R. Fitness and Activity Levels of German Military Medical Personnel at the Bundeswehr Hospital Hamburg. Wehrmed. Mon. 2022, 66, 1–7. [Google Scholar]
- Woynarowska-Sołdan, M.; Panczyk, M.; Iwanow, L.; Gałązkowski, R.; Wójcik-Fatla, A.; Panasiuk, L.; Gotlib, J. Associations between Overweight and Obesity and Health Enhancing Behaviours among Female Nurses in Poland. Ann. Agric. Environ. Med. 2018, 25, 714–719. [Google Scholar] [CrossRef]
- Biernat, E.; Piątkowska, M. Overestimation of Physical Activity by Long IPAQ in a Polish Nationwide Study. Hygeia Public Health 2016, 51, 87–95. [Google Scholar]
- Makarewicz, A.; Jamka, M.; Wasiewicz-Gajdzis, M.; Bajerska, J.; Miśkiewicz-Chotnicka, A.; Kwiecień, J.; Lisowska, A.; Gagnon, D.; Herzig, K.-H.; Mądry, E.; et al. Comparison of Subjective and Objective Methods to Measure the Physical Activity of Non-Depressed Middle-Aged Healthy Subjects with Normal Cognitive Function and Mild Cognitive Impairment-A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 8042. [Google Scholar] [CrossRef]
- Seo, K.; Jung, M.O.; Suh, M. Agreement of Physical Activity Measured Using Self-Reporting Questionnaires with Those Using Actigraph Devices, Focusing on the Correlation with Psychological State. J. Korean Biol. Nurs. Sci. 2021, 23, 287–297. [Google Scholar] [CrossRef]
- Sundarapperuma, T.D.; Wasalathanthri, S.; Wijesinghe, C.; Hettiarachchi, P. Assessment of Energy Expenditure in Postpartum Women with Prior Gestational Diabetes Mellitus: Subjective versus Objective Methods. Asian J. Med. Sci. 2022, 13, 29. [Google Scholar] [CrossRef]
- Deenik, J.; Koomen, L.E.; Scheewe, T.W.; van Deursen, F.P.; Cahn, W. Cardiorespiratory fitness and self-reported physical activity levels of referring mental healthcare professionals, and their attitudes and referral practices related to exercise and physical health. J. Psychiatr. Res. 2022, 154, 19–27. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Kamarudin, K.S.; Wan Muda, W.A.M. Associations between Self-Reported and Objectively Measured Physical Activity and Overweight/Obesity among Adults in Kota Bharu and Penang, Malaysia. BMC Public Health 2019, 19, 621. [Google Scholar] [CrossRef]
- Finn, M.; Sherlock, M.; Feehan, S.; Guinan, E.M.; Moore, K.B. Adherence to Physical Activity Recommendations and Barriers to Physical Activity Participation among Adults with Type 1 Diabetes. Ir. J. Med. Sci. 2022, 191, 1639–1646. [Google Scholar] [CrossRef]
- Gudnadottir, U.; Cadmus-Bertram, L.; Spicer, A.; Gorzelitz, J.; Malecki, K. The Relationship between Occupational Physical Activity and Self-Reported vs Measured Total Physical Activity. Prev. Med. Rep. 2019, 15, 100908. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Taylor, K.; Vella, C.A. Comparison of Self-Reported and Objectively Measured Sedentary Behavior and Physical Activity in Undergraduate Students. Meas. Phys. Educ. Exerc. Sci. 2019, 23, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Neupane, S.; Karstad, K.; Hallman, D.M.; Rugulies, R.; Holtermann, A. Objectively Measured versus Self-Reported Occupational Physical Activity and Multisite Musculoskeletal Pain: A Prospective Follow-up Study at 20 Nursing Homes in Denmark. Int. Arch. Occup. Environ. Health 2020, 93, 381–389. [Google Scholar] [CrossRef]
- Cuthbertson, C.C.; Moore, C.C.; Evenson, K.R. Paradox of Occupational and Leisure-Time Physical Activity Associations with Cardiovascular Disease. Heart 2023, 109, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka, A.; Garbaciak, W.; Cholewa, J.; Mynarski, W. The Relationship between Meeting of Recommendations on Physical Activity for Health and Perceived Work Ability among White-Collar Workers. Eur. J. Sport Sci. 2018, 18, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Skarpsno, E.S.; Mork, P.J.; Nilsen, T.I.L.; Jørgensen, M.B.; Holtermann, A. Objectively Measured Occupational and Leisure-Time Physical Activity: Cross-Sectional Associations with Sleep Problems. Scand. J. Work. Environ. Health 2018, 44, 202–211. [Google Scholar] [CrossRef]
- Wolff, M.B.; O’Connor, P.J.; Wilson, M.G.; Gay, J.L. Associations Between Occupational and Leisure-Time Physical Activity With Employee Stress, Burnout and Well-Being Among Healthcare Industry Workers. Am. J. Health Promot. 2021, 35, 957–965. [Google Scholar] [CrossRef]
- Abu Saad, H.; Low, P.K.; Jamaluddin, R.; Chee, H.P. Level of Physical Activity and Its Associated Factors among Primary Healthcare Workers in Perak, Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 5947. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Nam, S.; Buss, J.; Lee, S.-J. Assessing the Prevalence of Meeting Physical Activity Recommendations among U.S. Healthcare Workers: Data from the 2015 National Health Interview Survey. Arch. Environ. Occup. Health 2020, 75, 422–430. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).