Investigating the Mediating Role of Pain in the Relationship between Ankle Joint Position Sense and Balance Assessed Using Computerized Posturography in Individuals with Unilateral Chronic Ankle Instability: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Ethics, and Participants
2.2. Pain Intensity Assessment
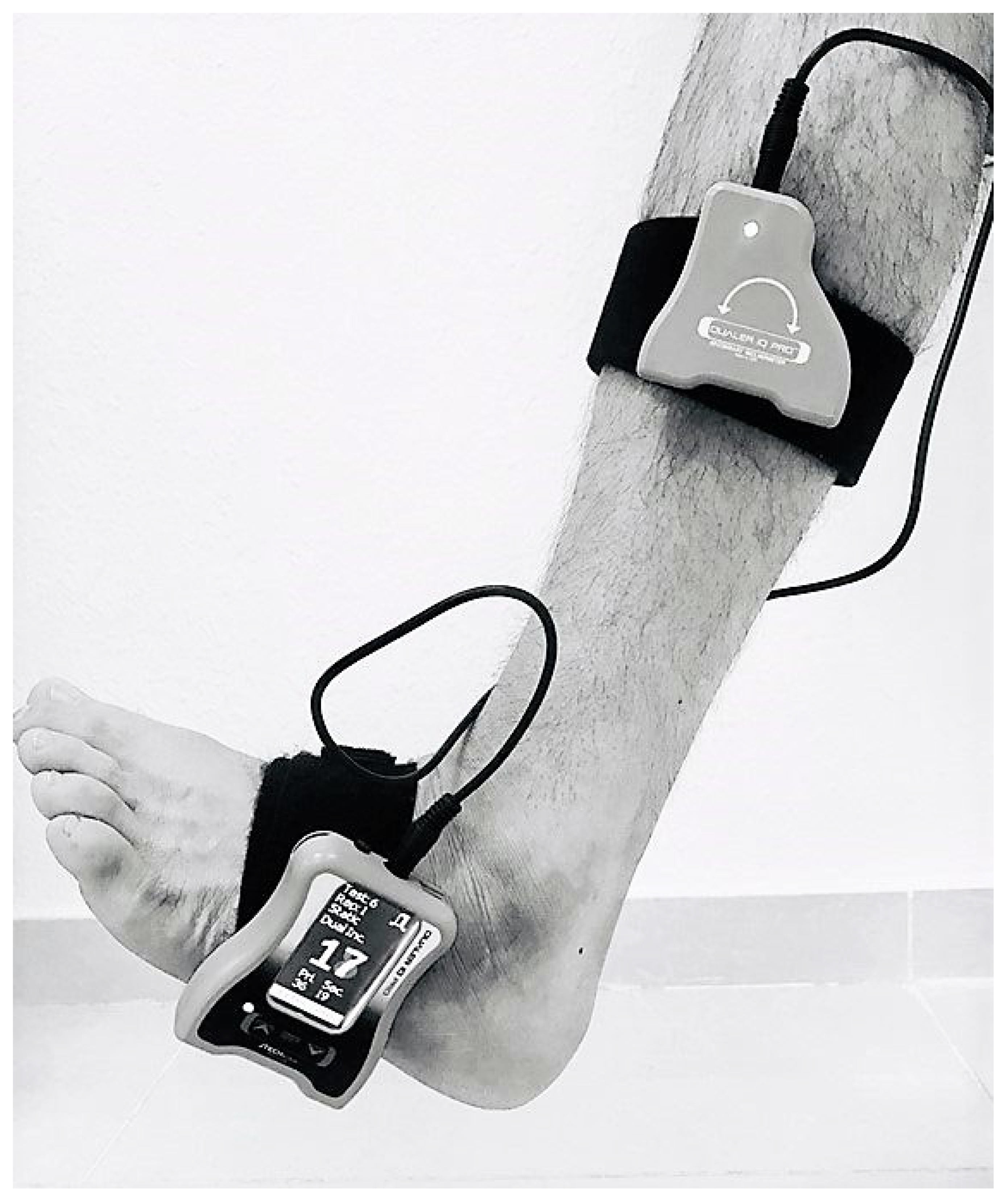
2.3. Ankle Joint Position Sense Assessment
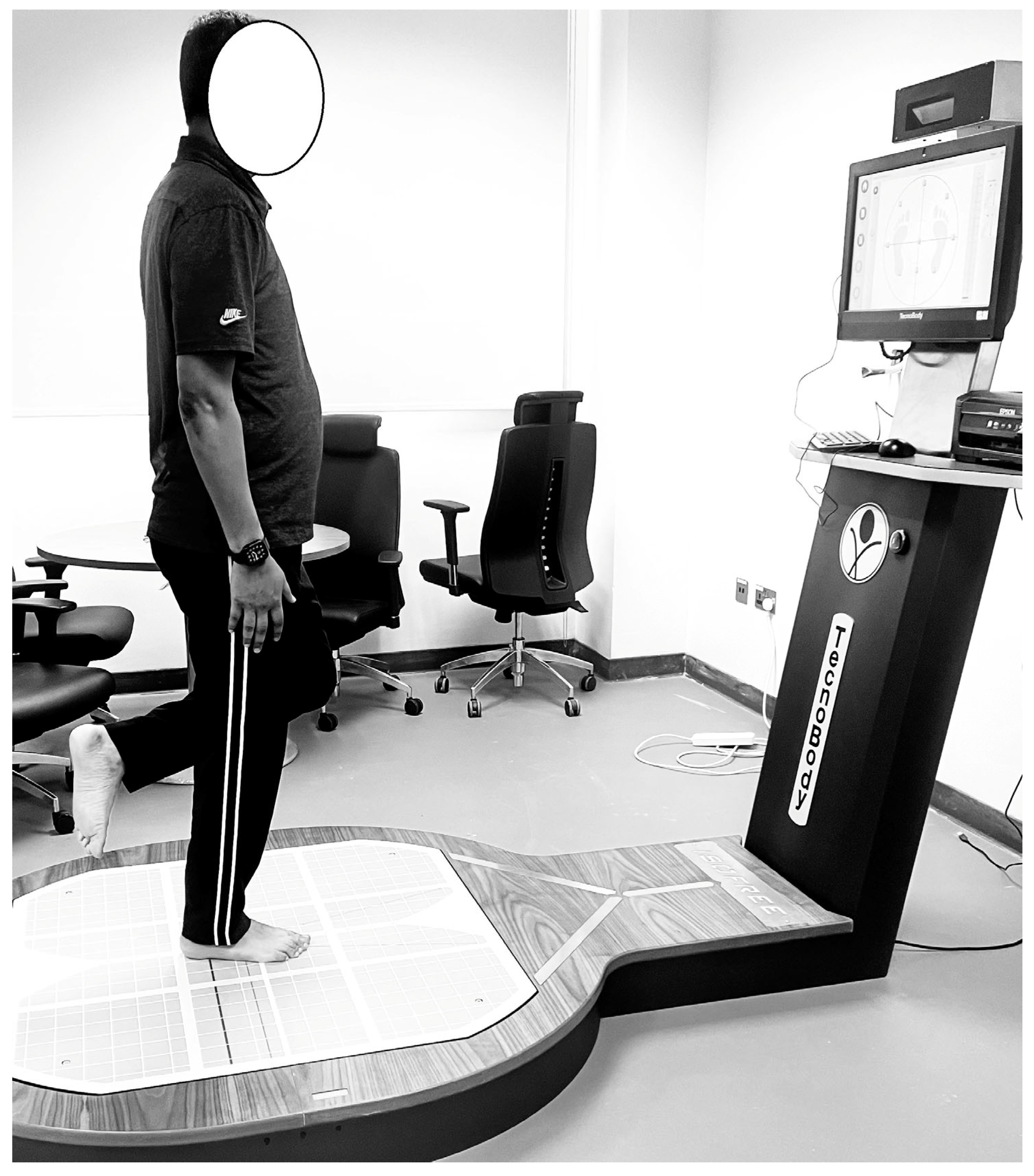
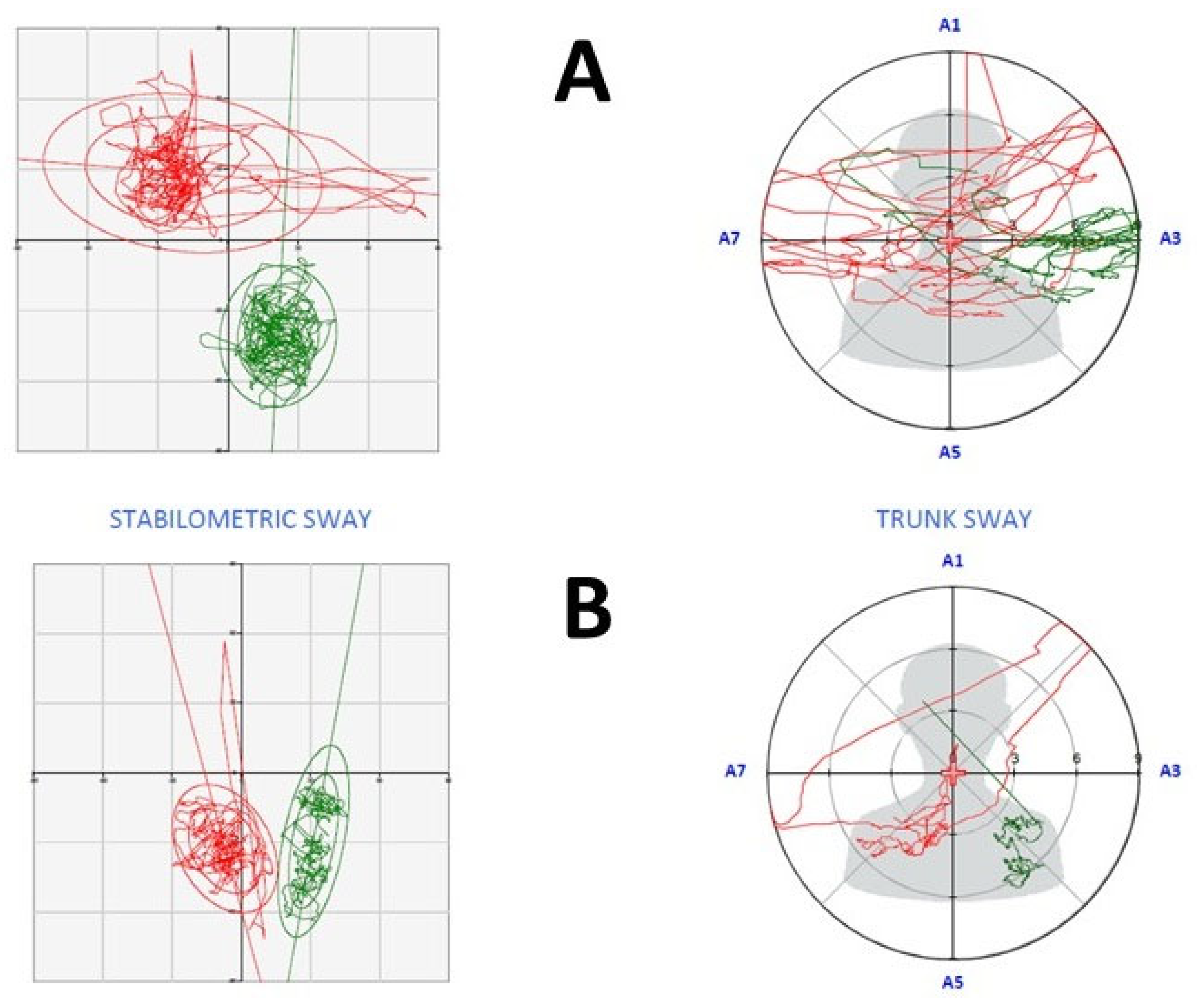
2.4. Balance Assessment
2.5. Sample Size Calculation
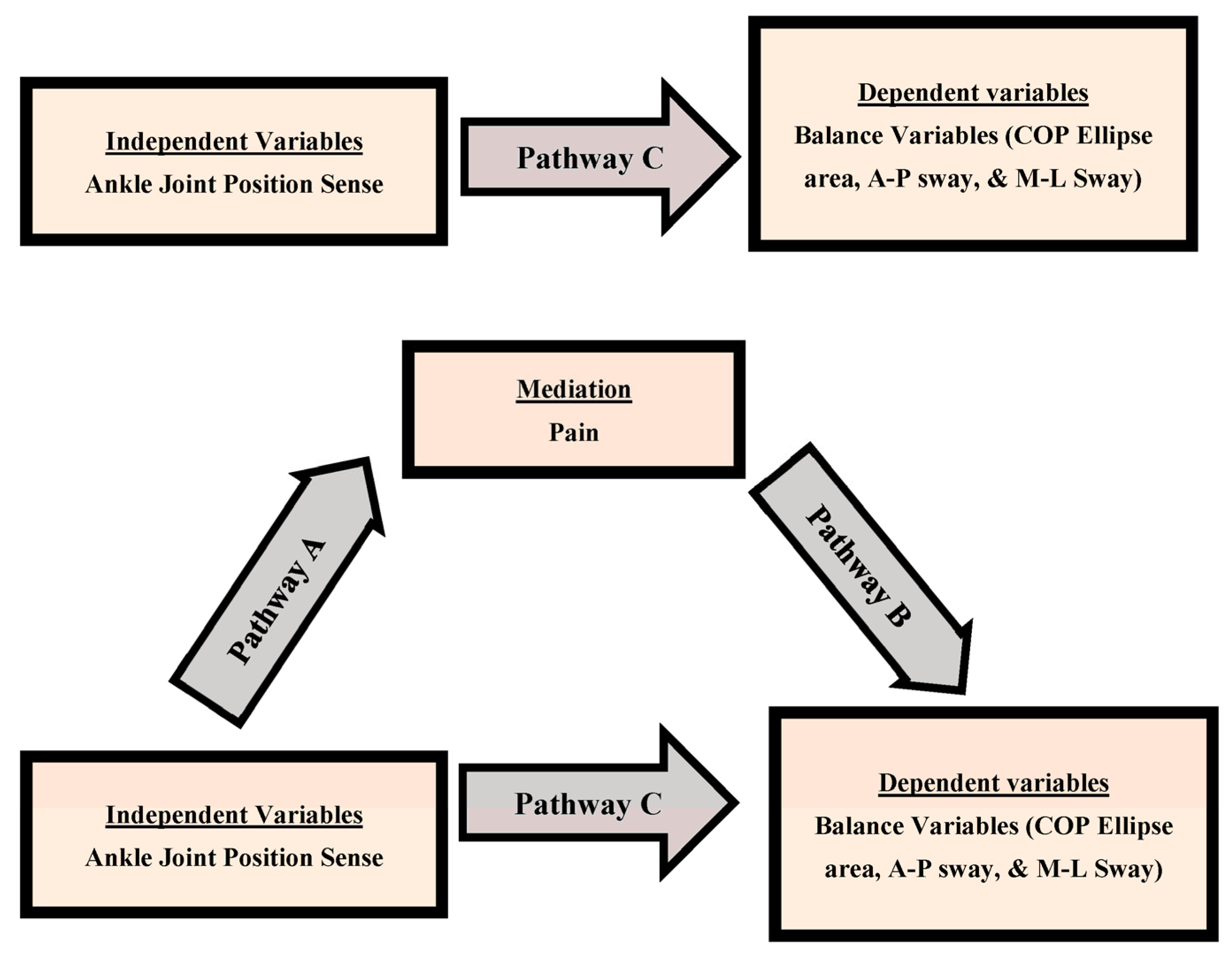
2.6. Statistical Analysis
3. Results
4. Discussion
4.1. Clinical Implications
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Delahunt, E.; Remus, A. Risk factors for lateral ankle sprains and chronic ankle instability. J. Athl. Train. 2019, 54, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J.; Corbett, R.O. An updated model of chronic ankle instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [PubMed]
- Di Maria, S. Effects of External Biofeedback Interventions in Individuals with Chronic Ankle Instability: A Scoping Review. Padua Thesis, Dipartimento di Neuroscienze, Torino, Italy, 2021. [Google Scholar]
- Lin, J.-Z.; Lin, Y.-A.; Tai, W.-H.; Chen, C.-Y. Influence of Landing in Neuromuscular Control and Ground Reaction Force with Ankle Instability: A Narrative Review. Bioengineering 2022, 9, 68. [Google Scholar] [CrossRef]
- Shirzadfar, H. The Structure and Function of Nervous System and Skeletal Muscle: A Review. Curr. Neuropsychiatry Clin. Neurosci. Rep. 2021, 3, 1–25. [Google Scholar]
- Banks, R.W.; Ellaway, P.H.; Prochazka, A.; Proske, U. Secondary endings of muscle spindles: Structure, reflex action, role in motor control and proprioception. Exp. Physiol. 2021, 106, 2339–2366. [Google Scholar] [CrossRef] [PubMed]
- Khorjahani, A.; Mirmoezzi, M.; Bagheri, M.; Kalantariyan, M. Effects of trx suspension training on proprioception and muscle strength in female athletes with functional ankle instability. Asian J. Sports Med. 2021, 12, 107042. [Google Scholar] [CrossRef]
- Ma, T.; Li, Q.; Song, Y.; Hua, Y. Chronic ankle instability is associated with proprioception deficits: A systematic review and meta-analysis. J. Sport Health Sci. 2021, 10, 182–191. [Google Scholar]
- Martin, R.L.; Davenport, T.E.; Fraser, J.J.; Sawdon-Bea, J.; Carcia, C.R.; Carroll, L.A.; Kivlan, B.R.; Carreira, D. Ankle stability and movement coordination impairments: Lateral ankle ligament sprains revision 2021: Clinical practice guidelines linked to the international classification of functioning, disability and health from the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2021, 51, CPG1–CPG80. [Google Scholar]
- Alshahrani, M.S.; Reddy, R.S. Relationship between Kinesiophobia and Ankle Joint Position Sense and Postural Control in Individuals with Chronic Ankle Instability—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2792. [Google Scholar] [CrossRef]
- Efstathiou, M.A.; Giannaki, C.D.; Roupa, Z.; Hadjisavvas, S.; Stefanakis, M. Evidence of distorted proprioception and postural control in studies of experimentally induced pain: A critical review of the literature. Scand. J. Pain 2022, 22, 445–456. [Google Scholar] [CrossRef]
- Azadinia, F.; Kingma, I.; Mazaheri, M. Effect of external lumbar supports on joint position sense, postural control, and postural adjustment: A systematic review. Disabil. Rehabil. 2023, 45, 753–771. [Google Scholar] [CrossRef] [PubMed]
- Wagemans, J.; Bleakley, C.; Taeymans, J.; Schurz, A.P.; Kuppens, K.; Baur, H.; Vissers, D. Exercise-based rehabilitation reduces reinjury following acute lateral ankle sprain: A systematic review update with meta-analysis. PLoS ONE 2022, 17, e0262023. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; Waddington, G.; Adams, R.; Han, J. Joint position reproduction and joint position discrimination at the ankle are not related. Somatosens. Mot. Res. 2020, 37, 97–105. [Google Scholar] [CrossRef]
- Alsakhawi, R.S.; Elshafey, M.A. Effect of core stability exercises and treadmill training on balance in children with Down syndrome: Randomized controlled trial. Adv. Ther. 2019, 36, 2364–2373. [Google Scholar] [CrossRef]
- Han, J.; Luan, L.; Adams, R.; Witchalls, J.; Newman, P.; Tirosh, O.; Waddington, G. Can therapeutic exercises improve proprioception in chronic ankle instability? A systematic review and network meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 2232–2244. [Google Scholar] [CrossRef] [PubMed]
- Heller, D.P. The Effect of a Specialized Yoga Intervention on Characteristics of Functional Ankle Instability. Master’s Thesis, University of Kansas, Lawrence, KS, USA, 2020. [Google Scholar]
- Alahmari, K.A.; Kakaraparthi, V.N.; Reddy, R.S.; Silvian, P.; Tedla, J.S.; Rengaramanujam, K.; Ahmad, I. Combined effects of strengthening and proprioceptive training on stability, balance, and proprioception among subjects with chronic ankle instability in different age groups: Evaluation of clinical outcome measures. Indian J. Orthop. 2021, 55, 199–208. [Google Scholar] [CrossRef]
- Thompson, C.S. Sensorimotor Adaptations in Chronic Ankle Instability. Ph.D. Thesis, Western Sydney University, Penrith, Australia, 2020. [Google Scholar]
- Johnson, J.J. Active and Passive Joint Position Sense on Healthy Hips. Master’s Thesis, Western Washington University, Bellingham, WA, USA, 2020. [Google Scholar]
- Peeters, G.; Bennett, M.; Donoghue, O.A.; Kennelly, S.; Kenny, R.A. Understanding the aetiology of fear of falling from the perspective of a fear-avoidance model—A narrative review. Clin. Psychol. Rev. 2020, 79, 101862. [Google Scholar] [CrossRef]
- Tito, N.; Porter, E.; Castonguay, T.; Dover, G. Longitudinal Validation of a Specific Measure of Fear Avoidance in Athletes: Predicting Time from Injury to Return to Sports Competition. J. Pain Res. 2023, 16, 1103–1114. [Google Scholar] [CrossRef]
- Zhao, X.; Boersma, K.; Gerdle, B.; Molander, P.; Hesser, H. Fear network and pain extent: Interplays among psychological constructs related to the fear-avoidance model. J. Psychosom. Res. 2023, 167, 111176. [Google Scholar] [CrossRef]
- Mullins, J.F.; Hoch, M.C.; Kosik, K.B.; Heebner, N.R.; Gribble, P.A.; Westgate, P.M.; Nitz, A.J. Effect of Dry Needling on Spinal Reflex Excitability and Postural Control in Individuals with Chronic Ankle Instability. J. Manip. Physiol. Ther. 2021, 44, 25–34. [Google Scholar] [CrossRef]
- Mullins, J.F.; Nitz, A.J.; Hoch, M.C. Dry needling equilibration theory: A mechanistic explanation for enhancing sensorimotor function in individuals with chronic ankle instability. Physiother. Theory Pract. 2021, 37, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Raizah, A.; Reddy, R.S.; Alshahrani, M.S.; Gautam, A.P.; Alkhamis, B.A.; Kakaraparthi, V.N.; Ahmad, I.; Kandakurti, P.K.; ALMohiza, M.A. A Cross-Sectional Study on Mediating Effect of Chronic Pain on the Relationship between Cervical Proprioception and Functional Balance in Elderly Individuals with Chronic Neck Pain: Mediation Analysis Study. J. Clin. Med. 2023, 12, 3140. [Google Scholar] [CrossRef] [PubMed]
- Asiri, F.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Alshahrani, A.; Gular, K.; Raizah, A. Mediation Effect of Pain on the Relationship between Kinesiophobia and Postural Control: Comparison and Correlations in Individuals with Fibromyalgia Syndrome and Asymptomatic Individuals—A Cross-Sectional Study. Life 2023, 13, 175. [Google Scholar] [CrossRef]
- Paap, D.; Krops, L.A.; Schiphorst Preuper, H.R.; Geertzen, J.H.; Dijkstra, P.U.; Pool, G. Participants’ unspoken thoughts and feelings negatively influence the therapeutic alliance; a qualitative study in a multidisciplinary pain rehabilitation setting. Disabil. Rehabil. 2022, 44, 5090–5100. [Google Scholar] [CrossRef]
- Petrini, L.; Arendt-Nielsen, L. Understanding pain catastrophizing: Putting pieces together. Front. Psychol. 2020, 11, 603420. [Google Scholar] [CrossRef]
- Wright, C.J.; Arnold, B.L.; Ross, S.E.; Linens, S.W. Recalibration and validation of the Cumberland Ankle Instability Tool cutoff score for individuals with chronic ankle instability. Arch. Phys. Med. Rehabil. 2014, 95, 1853–1859. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Preuper, H.R.S.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Bergquist, R.; Weber, M.; Schwenk, M.; Ulseth, S.; Helbostad, J.L.; Vereijken, B.; Taraldsen, K. Performance-based clinical tests of balance and muscle strength used in young seniors: A systematic literature review. BMC Geriatr. 2019, 19, 9. [Google Scholar] [CrossRef]
- Henry, M.; Baudry, S. Age-related changes in leg proprioception: Implications for postural control. J. Neurophysiol. 2019, 122, 525–538. [Google Scholar] [CrossRef]
- Mosca, M.; Caravelli, S.; Massimi, S.; Fuiano, M.; Catanese, G.; Barone, G.; Bragonzoni, L.; Benedetti, M.G. Evaluation of proprioception and postural control at a minimum 1 year follow-up after ankle capsuloligamentous lateralplasty with Brostrom technique: A cohort study. Medicine 2020, 99, e19862. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Hertel, J.; Denegar, C.R.; Buckley, W.E. The effects of fatigue and chronic ankle instability on dynamic postural control. J. Athl. Train. 2004, 39, 321. [Google Scholar] [PubMed]
- De Oliveira, M.R.; Fabrin, L.F.; de Oliveira Gil, A.W.; Benassi, G.H.; Camargo, M.Z.; da Silva, R.A.; de Lima, R.R. Acute effect of core stability and sensory-motor exercises on postural control during sitting and standing positions in young adults. J. Bodyw. Mov. Ther. 2021, 28, 98–103. [Google Scholar] [CrossRef]
- Esteves, J.; Dinis, R.; Fernandes, O.; Castro, M.A.; Oliveira, R.; Pezarat-Correia, P. Differences in postural control between healthy and subjects with chronic ankle instability. Phys. Ther. Sport 2022, 56, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Qu, X.; Hu, X.; Zhao, J.; Zhao, Z. The roles of lower-limb joint proprioception in postural control during gait. Appl. Ergon. 2022, 99, 103635. [Google Scholar] [CrossRef] [PubMed]
- Basta, D.; Rossi-Izquierdo, M.; Soto-Varela, A.; Ernst, A. Mobile posturography: Posturographic analysis of daily-life mobility. Otol. Neurotol. 2013, 34, 288–297. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Gonzalez, A. The Effects of Foot Intrinsic Strengthening Compared to Balance Training on Self-Perceived Function in Patients with Chronic Ankle Instability: A Meta-Analysis. Ph.D. Thesis, California State University, Fresno, CA, USA, 2023. [Google Scholar]
- Shi, X.; Han, J.; Witchalls, J.; Waddington, G.; Adams, R. Does treatment duration of manual therapy influence functional outcomes for individuals with chronic ankle instability: A systematic review with meta-analysis? Musculoskelet. Sci. Pract. 2019, 40, 87–95. [Google Scholar] [CrossRef]
- Helly, K.L.; Bain, K.A.; Hoch, M.C.; Heebner, N.R.; Gribble, P.A.; Terada, M.; Kosik, K.B. The effect of attending physical rehabilitation after the first acute lateral ankle sprain on static postural control in patients with chronic ankle instability. J. Sport Rehabil. 2021, 30, 1000–1007. [Google Scholar] [CrossRef]
- ALMohiza, M.A.; Reddy, R.S.; Asiri, F.; Alshahrani, A.; Tedla, J.S.; Dixit, S.; Gular, K.; Kakaraparthi, V.N. The Mediation Effect of Pain on the Relationship between Kinesiophobia and Lumbar Joint Position Sense in Chronic Low Back Pain Individuals: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 5193. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S. Mediation Effect of Kinesiophobia on the Relationship between Cervical Joint Position Sense and Limits of Stability in Individuals with Fibromyalgia Syndrome: A Cross-Sectional Study Using Mediation Analysis. J. Clin. Med. 2023, 12, 2791. [Google Scholar] [CrossRef]
- Kędziorek, J.; Błażkiewicz, M. Nonlinear measures to evaluate upright postural stability: A systematic review. Entropy 2020, 22, 1357. [Google Scholar] [CrossRef] [PubMed]
- Kantak, S.S.; Johnson, T.; Zarzycki, R. Linking pain and motor control: Conceptualization of movement deficits in patients with painful conditions. Phys. Ther. 2022, 102, pzab289. [Google Scholar] [CrossRef] [PubMed]
- Viseux, F.J.; Simoneau, M.; Billot, M. A Comprehensive Review of Pain Interference on Postural Control: From Experimental to Chronic Pain. Medicina 2022, 58, 812. [Google Scholar] [CrossRef] [PubMed]


| Variables | Functional Ankle Instability Group | p-Value |
|---|---|---|
| Age in years (Mean ± SD) | 23.11 ± 1.85 | - |
| Gender: Male: Female (%) | 29 (63):17 (37) | - |
| BMI (kg/m2) (Mean ± SD) | 24.26 ± 2.69 | - |
| Ankle Sprain duration in months (Mean ± SD) | 12.41 ± 3.88 | - |
| Pain Intensity (VAS score) (Mean ± SD) | 5.89 ± 1.34 | - |
Joint position sense at 10 degrees of dorsiflexion (Mean ± SD)
| 4.88 ± 1.44 1.30 ± 0.64 | <0.001 |
Joint position sense at 15 degrees of dorsiflexion (Mean ± SD)
| 4.72 ± 1.57 1.30 ± 0.16 | <0.001 |
Joint position sense at 10 degrees of plantarflexion (Mean ± SD)
| 4.75 ± 1.56 1.08 ± 0.79 | <0.001 |
Joint position sense at 15 degrees of plantarflexion (Mean ± SD)
| 4.77 ± 1.63 1.30 ± 0.70 | <0.001 |
COP Ellipse area (mm2) (Mean ± SD)
| 948.04 ± 172.09 462.22 ± 155.53 | <0.001 |
Anterior–posterior sway (mm) (Mean ± SD)
| 8.41 ± 3.08 3.67 ± 1.80 | <0.001 |
Medial–lateral sway (mm) (Mean ± SD)
| 6.45 ± 2.10 3.57 ± 1.07 | <0.001 |
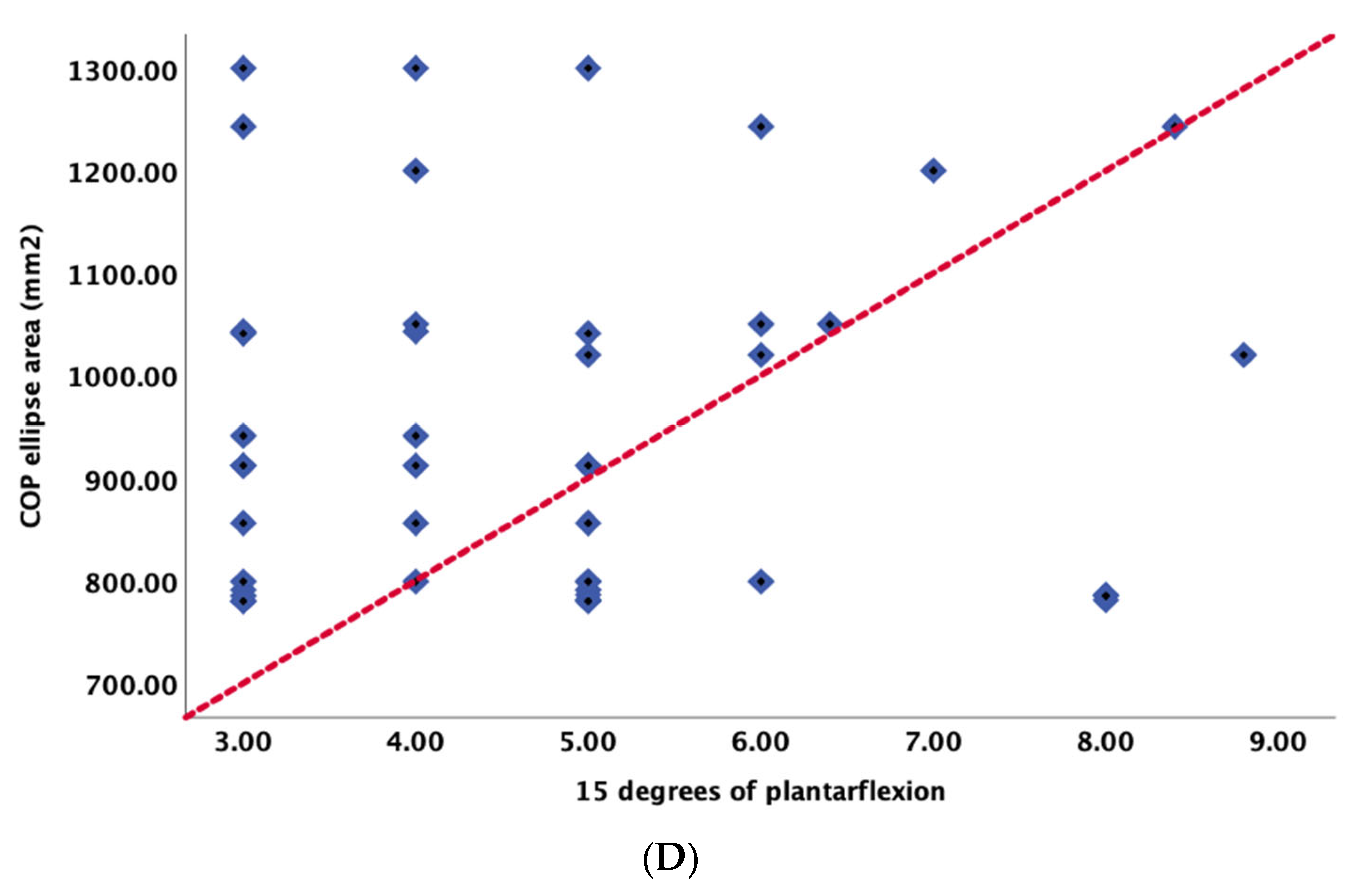
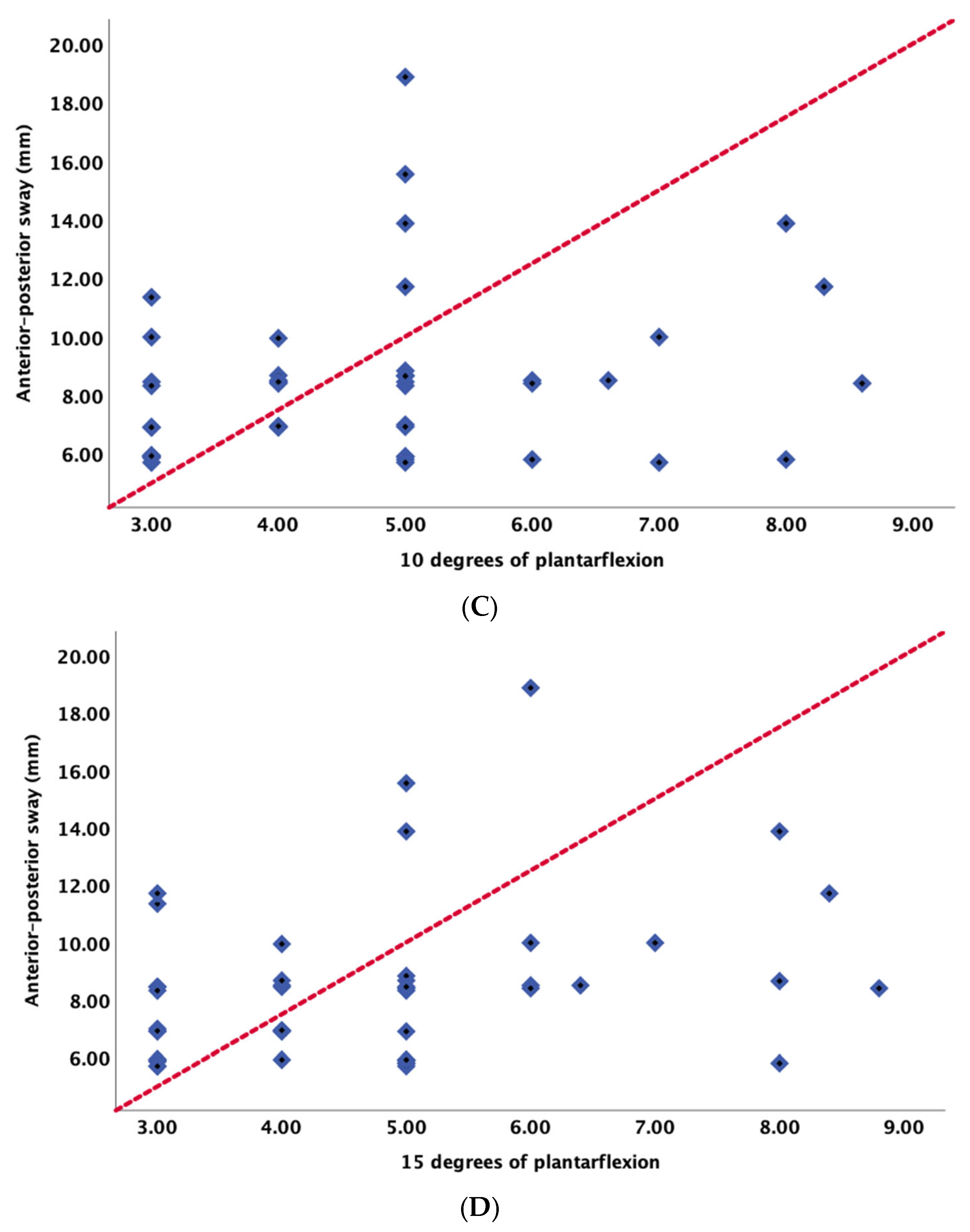
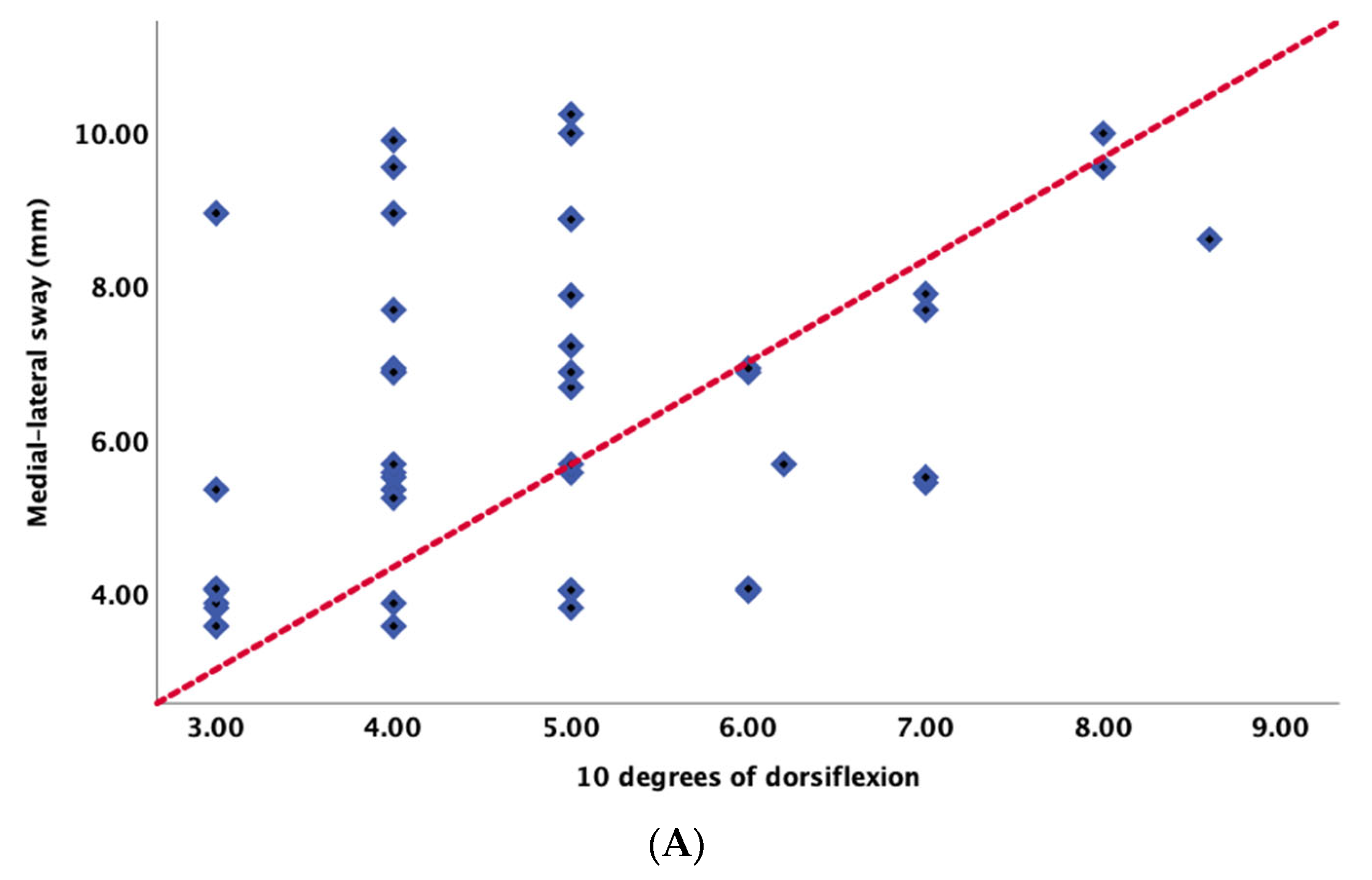
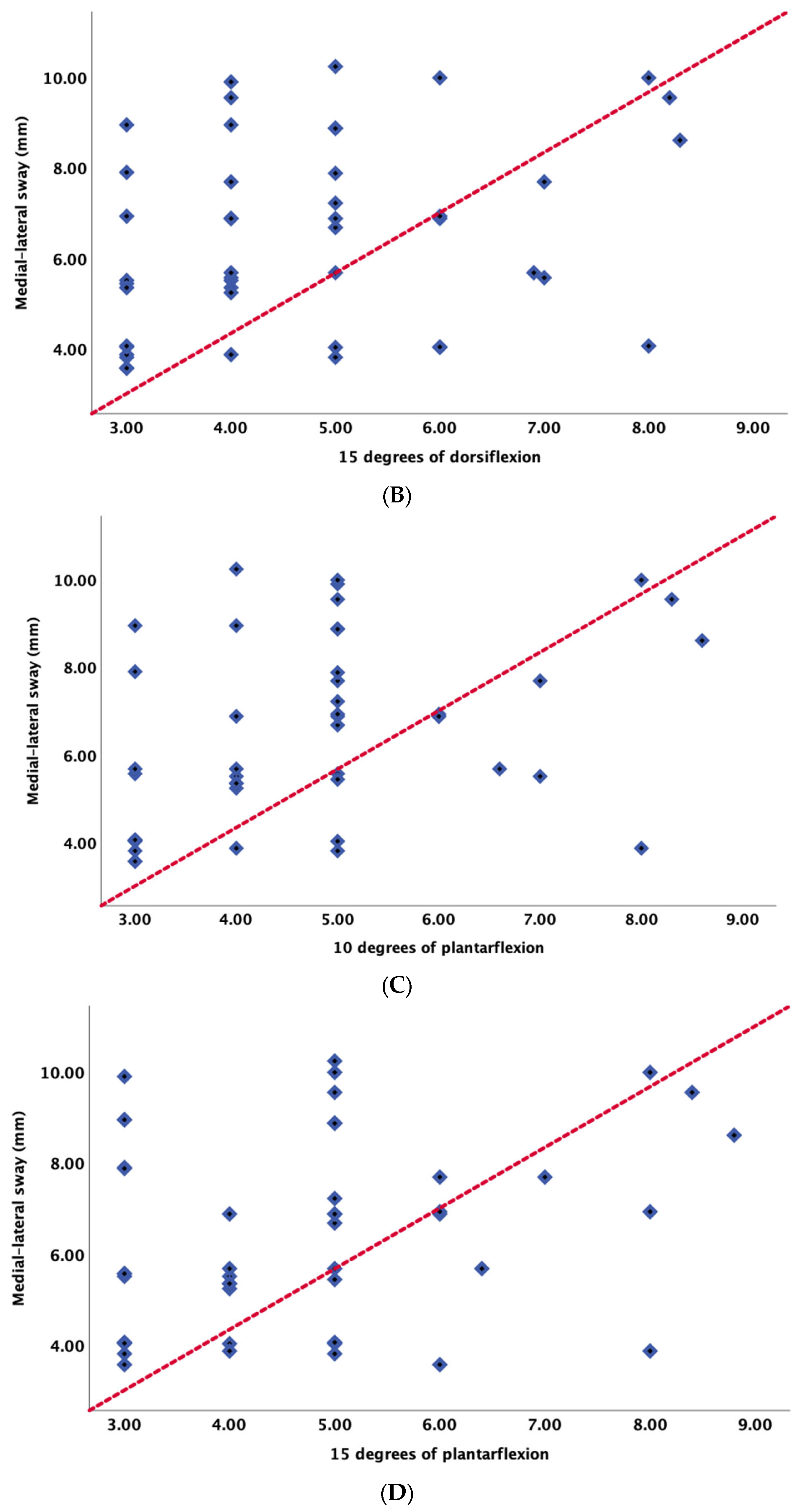
| Joint Position Sense | COP Ellipse Area (mm2) | Anterior–Posterior Sway (mm) | Medial–Lateral Sway (mm) |
|---|---|---|---|
| r | r | r | |
| 10 degrees of dorsiflexion | 0.31 ** | 0.42 ** | 0.38 ** |
| 15 degrees of dorsiflexion | 0.32 ** | 0.38 ** | 0.43 ** |
| 10 degrees of plantarflexion | 0.35 ** | 0.43 ** | 0.48 ** |
| 15 degrees of plantarflexion | 0.37 ** | 0.49 ** | 0.47 ** |
| Test Variables | Total Effect—Direct and Indirect (c + a × b) | Direct Effect (c-Path) | Indirect Effect (b-Path) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | p-Value | B | SE | p-Value | B | SE | p-Value | |
| Pain × JPS − 10° of DF × A-P sway (mm) | 0.42 | 0.12 | 0.001 | 0.13 | 0.02 | <0.001 | 0.05 | 0.01 | 0.002 |
| Pain × JPS − 15° of DF × A-P sway (mm) | 0.43 | 0.14 | 0.001 | 0.20 | 0.01 | <0.001 | 0.04 | 0.01 | 0.002 |
| Pain × JPS − 10° of PF × A-P sway (mm) | 0.58 | 0.11 | 0.011 | 0.16 | 0.01 | <0.001 | 0.09 | 0.02 | 0.003 |
| Pain × JPS − 15° of PF × A-P sway (mm) | 0.46 | 0.12 | 0.012 | 0.14 | 0.01 | <0.001 | 0.11 | 0.02 | 0.004 |
| Pain × JPS − 10° of DF × M-L sway (mm) | 0.42 | 0.14 | 0.001 | 0.31 | 0.02 | <0.001 | 0.05 | 0.01 | 0.002 |
| Pain × JPS − 15° of DF × M-L sway (mm) | 0.53 | 0.13 | 0.001 | 0.30 | 0.01 | <0.001 | 0.04 | 0.01 | 0.002 |
| Pain × JPS − 10° of PF × M-L sway (mm) | 0.48 | 0.12 | 0.011 | 0.26 | 0.01 | <0.001 | 0.09 | 0.02 | 0.003 |
| Pain × JPS − 15° of PF × M-L sway (mm) | 0.46 | 0.13 | 0.012 | 0.24 | 0.01 | <0.001 | 0.11 | 0.02 | 0.004 |
| Pain × JPS − 10° of DF × COP Ellipse area (mm2) | 0.48 | 0.09 | 0.011 | 0.16 | 0.01 | <0.001 | 0.09 | 0.02 | <0.001 |
| Pain × JPS − 15° of DF × COP Ellipse area (mm2) | 0.46 | 0.08 | 0.012 | 0.14 | 0.01 | <0.001 | 0.11 | 0.02 | <0.001 |
| Pain × JPS − 10° of PF × COP Ellipse area (mm2) | 0.42 | 0.08 | 0.001 | 0.31 | 0.02 | <0.001 | 0.05 | 0.01 | <0.001 |
| Pain × JPS − 15° of PF × COP Ellipse area (mm2) | 0.53 | 0.07 | 0.001 | 0.30 | 0.01 | <0.001 | 0.04 | 0.01 | <0.001 |
| Test Variables | Sobel Test | SE | p-Value |
|---|---|---|---|
| Pain × JPS − 10° of DF × A-P sway (mm) | 0.34 | 0.04 | 0.040 |
| Pain × JPS − 15° of DF × A-P sway (mm) | 0.44 | 0.03 | 0.030 |
| Pain × JPS − 10° of PF × A-P sway (mm) | 0.26 | 0.02 | 0.028 |
| Pain × JPS − 15° of PF × A-P sway (mm) | 0.36 | 0.04 | 0.029 |
| Pain × JPS − 10° of DF × M-L sway (mm) | 0.44 | 0.10 | 0.020 |
| Pain × JPS − 15° of DF × M-L sway (mm) | 0.53 | 0.12 | 0.010 |
| Pain × JPS − 10° of PF × M-L sway (mm) | 0.35 | 0.11 | 0.030 |
| Pain × JPS − 15° of PF × M-L sway (mm) | 0.47 | 0.09 | 0.019 |
| Pain × JPS − 10° of DF × COP Ellipse area (mm2) | 0.26 | 0.02 | 0.028 |
| Pain × JPS − 15° of DF × COP Ellipse area (mm2) | 0.36 | 0.04 | 0.029 |
| Pain × JPS − 10° of PF × COP Ellipse area (mm2) | 0.44 | 0.10 | 0.020 |
| Pain × JPS − 15° of PF × COP Ellipse area (mm2) | 0.53 | 0.12 | 0.010 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfaya, F.F.; Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Gular, K.; Mukherjee, D. Investigating the Mediating Role of Pain in the Relationship between Ankle Joint Position Sense and Balance Assessed Using Computerized Posturography in Individuals with Unilateral Chronic Ankle Instability: A Cross-Sectional Study. Appl. Sci. 2023, 13, 8169. https://doi.org/10.3390/app13148169
Alfaya FF, Reddy RS, Alshahrani MS, Tedla JS, Dixit S, Gular K, Mukherjee D. Investigating the Mediating Role of Pain in the Relationship between Ankle Joint Position Sense and Balance Assessed Using Computerized Posturography in Individuals with Unilateral Chronic Ankle Instability: A Cross-Sectional Study. Applied Sciences. 2023; 13(14):8169. https://doi.org/10.3390/app13148169
Chicago/Turabian StyleAlfaya, Fareed F., Ravi Shankar Reddy, Mastour Saeed Alshahrani, Jaya Shanker Tedla, Snehil Dixit, Kumar Gular, and Debjani Mukherjee. 2023. "Investigating the Mediating Role of Pain in the Relationship between Ankle Joint Position Sense and Balance Assessed Using Computerized Posturography in Individuals with Unilateral Chronic Ankle Instability: A Cross-Sectional Study" Applied Sciences 13, no. 14: 8169. https://doi.org/10.3390/app13148169
APA StyleAlfaya, F. F., Reddy, R. S., Alshahrani, M. S., Tedla, J. S., Dixit, S., Gular, K., & Mukherjee, D. (2023). Investigating the Mediating Role of Pain in the Relationship between Ankle Joint Position Sense and Balance Assessed Using Computerized Posturography in Individuals with Unilateral Chronic Ankle Instability: A Cross-Sectional Study. Applied Sciences, 13(14), 8169. https://doi.org/10.3390/app13148169











