Abstract
This study aimed to analyze the treatment effects of miniscrew-assisted rapid palatal expansion using dental cone-beam computed tomography (CT) in adolescents. The study group comprised 20 patients who underwent cone-beam CT before and after miniscrew-assisted rapid palatal expansion (MARPE). Paired t-test and analysis of variance were used to analyze significant differences before and after treatment. Skeletal and dentoalveolar measurements indicated highly significant differences, with these expansions increasing progressively in the downward direction. The extent of anterior midpalatal suture expansion was significantly greater than that of the posterior part. Significant expansion was observed at the nasal width and inter-zygomaticomaxillary suture distance. MARPE can expand the craniofacial skeletal structure to the uppermost nasal bone and lateral to the zygomaticomaxillary sutures. The expansion was greater in the lower maxillary part, demonstrating an overall triangular maxillary expansion. The midpalatal suture opening was greater in the anterior than in the posterior side, whereas the posterior suture opening proportion was higher than that of the conventional rapid palatal expansion previously reported.
1. Introduction
Among the many factors contributing to malocclusion, anatomical factors can be broadly categorized as skeletal and dental. Skeletal elements include the relative anteroposterior, vertical, and transverse positioning of the maxilla and mandible. The diagnostic and treatment methods for defining and determining these elements have been the subject of much research and discussion. A constricted maxilla is one of the most frequent skeletal components of malocclusions. Narrow maxilla can cause arch length discrepancy resulting in crowding of the dentition and also can cause functional problems resulting from deficient posterior overjet or even posterior crossbite [1]. It is said that narrow maxilla is not only limited to transverse dimensional problem but is also related to the sagittal (i.e., Class II malocclusion) component of malocclusion [1]. Clinicians can resolve this skeletal malocclusion by applying a rapid palatal expander (RPE) in young patients and surgical options in adult patients. The treatment effect of a conventional RPE incudes skeletal and dental expansion with more tendency of dental expansion [2]. To increase the skeletal expansion effect of the RPE, a combination of skeletal anchorage to the RPE has been proposed and is now widely accepted in clinical orthodontics [3].
Skeletal anchorage-assisted RPE has two types: tooth-bone-borne and bone-borne. The tooth-bone-borne type RPE is not only assisted by skeletal anchorage but also supported by teeth [3]. Meanwhile, the bone-borne RPE type receives support solely from skeletal anchorage and is expected to exert only skeletal effects [4,5]. Although results among studies and arguments among clinicians are conflicting, tooth-bone-borne expander treatment effects are mainly skeletal with some dental effects [3,6,7]. The tooth-bone-borne type is the addition of skeletal anchorage, mostly the miniscrew type, to the conventional RPE design and may be more familiar to clinicians who are used to it. Most types of tooth-bone-borne RPE use miniscrews for skeletal anchorage, which is called miniscrew-assisted RPE (MARPE).
Reports on the treatment effect of MARPE have demonstrated its capability of more skeletal expansion of the maxilla than conventional RPE [8]. Furthermore, some reports have claimed that the mode of expansion is different from that of conventional RPE in that MARPE results in more parallel expansion between the palatal processes of the maxilla, whereas conventional RPE expands the maxilla more anteriorly than posteriorly [9]. Moreover, the age limitation has been extended using MARPE [10]. The age limitation of conventional RPE was considered 15 years after long-term clinical experience and anatomical studies; however, several reports have indicated that MARPE is capable of opening the palatal sutures in adults [11].
Despite the increasing popularity of MARPE in clinical orthodontics and published studies, more data are needed to elucidate its therapeutic effects. However, no consensus on the activation mode of MARPE, its optimal design, assisted miniscrews, or retention protocols has been established. The reported treatment effects of MARPE differ between studies, which may be because of different MARPE designs, numbers, and sizes of miniscrews used as well as different modes of activation among clinicians. More data should be accumulated to establish the application method of MARPE and understand and predict the results of MARPE applications. Therefore, the purpose of this study was to investigate the skeletal and dental effects of miniscrew-assisted rapid palatal expansion (MARPE) in adolescents using cone-beam computed tomography (CBCT). Changes in zygomatic width and nasal bone deviation were also evaluated.
2. Materials and Methods
This retrospective study was approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (KHNMC 2023-01-031). Patients who underwent orthodontic treatment at the Department of Orthodontics, Kyung Hee University Hospital at Gangdong from 1 March 2017 to 31 December 2022 and in whom MARPE was used as the first treatment device were enrolled in this study (Figure 1 and Figure 2). Based on previous studies, the number of participants per group should be 15–20 [9,12]. A minimum sample size of 15 patients was required (G*Power 3.1.9.6, Dusseldorf, Germany), considering an alpha of 0.05, power of 80%, and effect size of 0.80 to detect differences in palatal expansion using a paired t-test [13].

Figure 1.
Clinical application of miniscrew-assisted rapid palatal expansion (MARPE). (A) before MARPE expansion; (B) after RPE expansion; (C) removal of dental connections after a month of expansion completion.
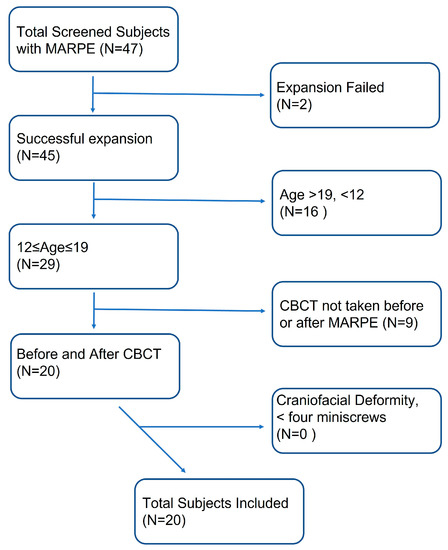
Figure 2.
Flowchart of participant recruitment.
The inclusion criteria were as follows: (1) CBCT was performed before expansion (T1) and after palatal expansion treatment (T2); (2) adolescent patients aged 12–19 years; and (3) four miniscrews without failure during treatment were used with the same MARPE appliance. The exclusion criteria were as follows: (1) craniofacial deformity, such as a cleft palate; (2) palatal expansion that did not occur as planned after MARPE; and (3) history of orthodontic treatment and/or orthognathic surgery.
The study group comprised 20 patients (7 male and 13 female patients) with a mean age of 15.40 ± 2.07 years. In this study, the same type of MARPE appliance was used in all patients for rapid palatal expansion. The MARPE device (MSE; BioMaterials Korea, Seoul, Republic of Korea) has four screw holes in the jackscrew body and four retention arms soldered to the maxillary first molars. Following MARPE cementation, four self-drilling bone screws (1.5 mm diameter and 9–11 mm length) were inserted perpendicularly under local infiltration anesthesia, and the miniscrew lengths were determined considering the palatal bone depth for fenestration of the palatal bone to facilitate greater expansion forces. The 9–11 mm length was selected by considering the 2 mm height of the insertion slots, 1–2 mm space between the appliance and the palatal surface, 1–2 mm gingival thickness, and 5–6 mm bone engagement. The antero-posterior position of the MARPE was set the same as the maxillary first molar in all patients. Activation was two turns per day for 2 weeks or one turn per day for 4 weeks. Patients below age 12 received one turn per day activation protocol. Additionally, with the patients who complained about much pain when activating MARPE, one turn per day activation protocol was applied even though the patient was older than the age 12. In our samples, only one patient received one turn per day expansion protocol while all the other patients received two turns per day expansion protocol. Both one turn and two turns per day activation protocols fall in rapid expansion, and it was assumed that there might be no significant difference between the two protocols. The expansion continued until the palatal cusps of the maxillary first molars were in contact with the buccal cusps of the mandibular molars. If there was hard resistance against activation, a 2-week rest was provided, and activation was resumed. After completion of the expansion, the expansion screw was fixed with flowable resin to secure its expanded state. One month after the completion of the expansion, four dental connections of the MARPE were removed, and CBCT was taken to ensure the expansion of the midpalatal suture. In this study, the mean duration of expansion was 22 ± 3.1 days (range, 13–63 days). The mean duration from completion of palatal expansion to CBCT taking at T2 stage was 44.6 ± 4.0 days (range, 27–97 days).
All CBCT scans were performed using CS9600 (Carestream Dental LLC, Atlanta, Georgia) before treatment (T1) and after expansion (T2); it was set at 100–150 kVp, and the slice thickness was 0.3 mm in the cranial mode. Digital Imaging and Communications in Medicine file image reconstruction and analysis were performed with InVivo5® (Anatomage, San Jose, CA, USA).
2.1. Reference Planes and Measurements
All CBCTs were aligned in InVivo5® (Anatomage, San Jose, CA, USA) so that the plane through the nasion, basion, and anterior nasal spine (ANS) was the midsagittal plane, and the transverse plane was perpendicular to the midsagittal plane and through the posterior nasal spine (PNS). The coronal plane was perpendicular to the mid-sagittal and transverse planes.
Skeletal (ANS-Ex, amount of expansion of the midpalatal suture at the ANS site; Mx6-Ex, amount of expansion of the midpalatal suture at the maxillary first molar area; PNS-Ex, amount of expansion of the midpalatal suture at the PNS site; UNW, anterior nasal width at the level of the buccal bone vertically; IZW, inter-zygomatic width; NSdev, nasal septum deviation; NW-lower, lower nasal width; NW-upper, upper nasal width; MxBBW, maxillary basal bone width), and dentoalveolar (Mx6W, maxillary intermolar width; Mx6Ax, maxillary first molar axis) measurements were analyzed. The landmarks, reference planes, and measurements used for CBCT in this study are depicted in Table 1 and Figure 3, Figure 4 and Figure 5.

Table 1.
Definition of landmarks, reference planes, and measurements used in this study.
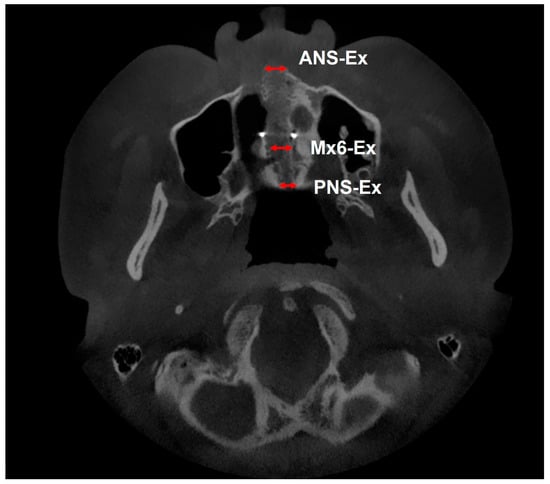
Figure 3.
Measurements in a cross-sectional slice of the palatal root apex of the maxillary left first molar: ANS-Ex, amount of expansion of the midpalatal suture at the anterior nasal spine (ANS) site; Mx6-Ex, amount of expansion of the midpalatal suture at the maxillary first molar area; PNS-Ex, amount of expansion of the midpalatal suture at the posterior nasal spine (PNS) site.
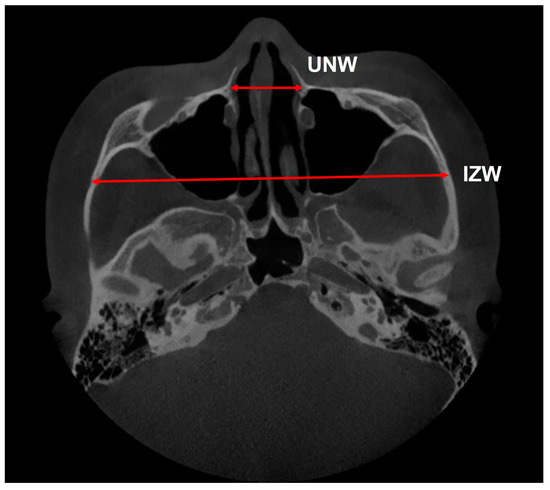
Figure 4.
Measurements in a cross-sectional slice of the zygomaticomaxillary suture: UNW, anterior nasal width at the level of the buccal bone vertically; IZW, inter-zygomatic width.
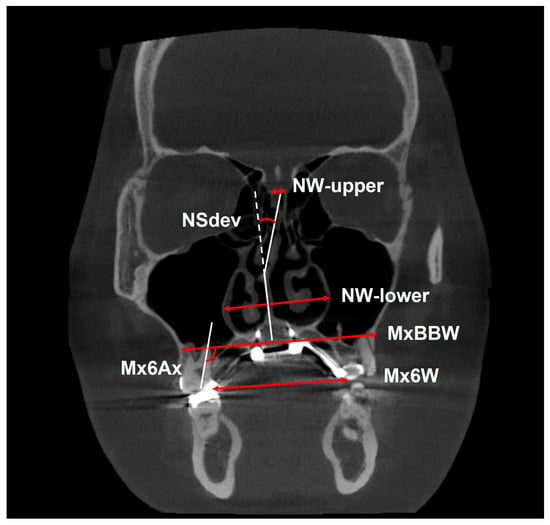
Figure 5.
Measurements in a slice of the root apex of the palatal side of the left maxillary first molar in the coronal plane: Nsdev, nasal septum deviation; NW-lower, lower nasal width; NW-upper, upper nasal width; MxBBW, maxillary basal bone width; Mx6W, maxillary intermolar width; Mx6Ax, maxillary first molar axis.
2.2. Statistical Analysis
All statistical analyses were performed using the IBM SPSS Statistics software for Windows (version 15.0; IBM Corp., Armonk, NY, USA). Descriptive statistics were used to analyze the variables. The Shapiro–Wilk test was used to confirm the normality of the data distribution. An independent t-test was performed to assess age differences according to sex. A χ2 test was performed to evaluate sex differences in the measurement before palatal expansion at T1 stage. Paired t-tests or Wilcoxon signed-rank tests were used to compare differences before and after expansion within each group. A one-way analysis of variance (ANOVA) with Bonferroni post-hoc test was performed to compare the three groups (ANS-Ex, Mx6-Ex, and PNS-Ex).
Significance was set at p < 0.05. The orientation and measurements were performed by a single experienced examiner (H.R. Kim). The same examiner remeasured 20 randomly selected CBCTs scans after a 2-week interval to determine intra-examiner reliability. The resulting intraclass correlation coefficient (ICC) indicated a high reliability (ICC > 0.98).
3. Results
This study group comprised 20 patients (7 male and 13 female patients) with a mean age of 15.40 ± 2.07 years (Table 2 and Table 3). No significant differences in age and sex distributions were observed between patients in the study group. Descriptive statistics and comparisons between mean values are listed in Table 2. The χ2 test revealed no significant differences in the pre-treatment measurements between sexes (Table 3). None of the miniscrews were failed during expansion, but several miniscrews’ axes were found to be changed after expansion (miniscrew head to the lateral side).

Table 2.
Demographic features of the subjects.

Table 3.
Comparison of the skeletal and dental changes during the treatment period.
Skeletal (ANS-Ex, Mx6-Ex, PNS-Ex, UNW, NW-lower, NW-upper, MxBBW, and IZW) and dentoalveolar (Mx6W and Mx6Ax) measurements demonstrated highly significant differences (p < 0.001 ***). Only the NSdev indicated no significant difference. Significant basal bone expansion was observed in the NW-lower, NW-upper, and MxBBW groups (p < 0.001) (Table 3).
After expansion (T2–T1), the amount of expansion of ANS-Ex in the left maxillary first molar region was significantly higher than that of Mx6-Ex and PNS-Ex in the ANOVA (p < 0.01). Post-hoc tests showed no differences between the Mx6-Ex and PNS-Ex groups. The amount of expansion was 4.41 ± 1.34 mm in the anterior region (ANS-Ex) and 3.44 ± 0.94, 3.55 ± 0.98 mm in the posterior region (Mx6-Ex and PNS-Ex), respectively (Table 3).
Significant dentoalveolar expansion was noted at the Mx6W and Mx6Ax (p < 0.001). The amount of expansion was 5.25 ± 1.81 mm at the Mx6W, and a significant increase of 2.97 ± 2.49° at the Mx6Ax was observed. Therefore, the buccal tipping of the maxillary molars was observed (Table 3).
Significant expansion was observed at the NW-upper (0.47 ± 0.36 mm), NW-lower (3.0 ± 1.16 mm), MxBBW (3.58 ± 1.18 mm), and Mx6W (5.25 ± 1.81 mm), with these expansions increasing progressively in the order listed above, suggesting an overall triangular maxillary expansion (Table 3 and Figure 6).
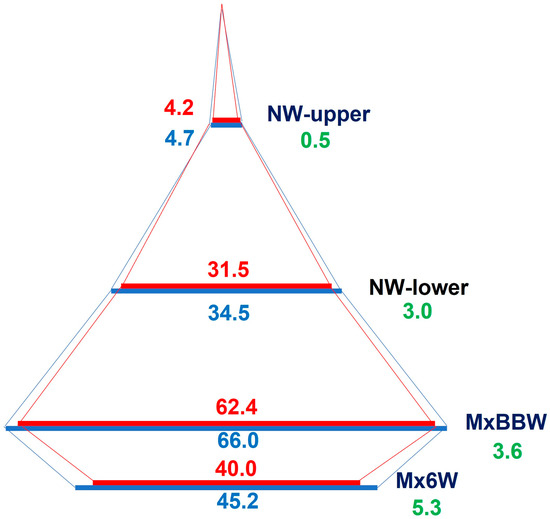
Figure 6.
Diagram of transverse change of the left maxillary first molar in the coronal section. Values are the mean differences (mm); red line, T1, before treatment (red); T2, after expansion (blue); ∆T2–T1, difference between before and after expansion (green).
4. Discussion
Dental clinicians frequently encounter the need for palatal appliances for transverse maxillary correction. The use of RPE or MARPE can promote skeletal and alveolar bone changes, with the most studied aspects being the opening of the midpalatal suture, changes in the position of the basal bone, and tilting of the molars [15,16,17]. One of the objectives of miniscrew-assisted maxillary expansion is to secure alveolar bone coverage along with lateral expansion of the maxillary buccal segment for proper transverse maxillary dimensions. According to a previous study, MARPE has demonstrated favorable skeletal and dentoalveolar expansion even in young adults, thus expanding the age limit for nonsurgical maxillary expansion [10]. This study aimed to analyze the effects of miniscrew-assisted rapid palatal expansion using dental cone-beam CT in adolescents who, as they age, are likely to receive orthodontic treatment the most. A comprehensive three-dimensional view of the maxilla is required to analyze the changes during the expansion period, and evaluating the changes using CBCT is important.
In this study, the expansion pattern was triangular in both the coronal and axial planes. Extension of the entire craniofacial structure can be depicted in the coronal plane as a triangular pattern based on the maxillary dental arch. In our study, significant expansion was observed at the NW-upper (0.47 ± 0.36 mm), NW-lower (3.0 ± 1.16 mm), MxBBW (3.58 ± 1.18 mm), and Mx6W (5.25 ± 1.81 mm), with these expansions increasing progressively in the order listed above. Hence, we observed a decreasing amount of upward and skeletal expansion ranging from 25% to 61%, which is consistent with that reported in previous research [7,18,19]. This triangular expansion pattern enlarges the alveolar bone area to a greater extent, thereby allowing greater alveolar bone enlargement relative to the basal bone. Although not reported in the Section 2 and Section 3, correlation analysis between the amounts of hard tissue expansion and patients’ characteristics (sex and age) was performed. The results of this analysis showed no significant correlation between the amounts of hard tissue expansion and patients’ characteristics (sex and age). This can be interpreted as MARPE being able to expand hard tissues to similar extents regardless of age and sex. However, it is important to note that only successfully expanded patients were enrolled in this study, so this interpretation should be accepted with caution. Additionally, the small sample size of the study makes the correlation analysis result less reliable.
Buccal tipping of the anchor teeth owing to the maxillary expansion is consistent with the results in previous studies [5,7,18]. Inclination of the maxillary first molars increased significantly after expansion (2.97° ± 2.49°) in this study. Although MARPE was designed to maximize skeletal expansion while keeping the teeth in the original alveolar bone position, the current results indicate some expansions in the anchored posterior teeth. This mean increase in buccal inclination may be clinically insignificant. The largest change identified in our sample was 9.6°, which was clinically significant. Clinicians must be aware of the possibility of significant buccal tipping of the anchored maxillary molar, even when MARPE is used. This buccal tipping may cause loss of the buccal alveolar bone in the corresponding maxillary molar [5]. The whole palatal segment may possibly rotate after expansion, resulting in buccal tipping of the alveolar bone and posterior teeth in a mass without the so-called sole dental expansion. However, this hypothesis should be evaluated using more sophisticated measurements in these areas, which was beyond the scope of this study.
Several studies have reported on the parallel expansion of the midpalatal suture with MARPE [9]. The current study identified a greater expansion in the ANS area than in the posterior (first molar and PNS) area. This inconsistency may be due to the differences in the position of the MARPE jackscrew, length of the anchor screws, age of the study participants, etc. [20,21]. In this study, the mean expansion in the ANS and PNS regions was 4.41 ± 1.34 mm and 3.55 ± 0.98 mm, respectively. The percentage ratio of posterior to anterior expansion was approximately 80%. Compared to the conventional RPE without skeletal anchorage reinforcement, which demonstrated expansion in the anterior region by 2.42 to 4 mm while the expansion in the posterior region was 0.84 to 2.88 mm, the percentage of posterior suture opening is still larger with the MARPE in this study [22].
Cantarella et al. have reported that MARPE can alter the zygomaticomaxillary complex by rotating the zygomatic process [8]. Their study demonstrated that the extent of skeletal changes in the craniofacial complex after MARPE was significantly greater than that after conventional RPE. Similarly, we attempted to determine any change in the inter-zygomaticomaxillary suture distance for maxillary expansion which may cause changes in this distance. The statistical results indicated a significant increase in the zygomaticomaxillary suture distance, with a mean of 1.49-mm increase. All the participants in this study demonstrated an increase in this measurement at T2 compared to that at T1. Thus, the expanding ability of MARPE reaches the zygoma. However, many of the participants were growing adolescents, and establishing control groups with the same age range is necessary to fully confirm this expansion effect in the zygomaticomaxillary suture. Although we cannot fully rule out the possibility of a growing effect on the inter-zygomaticomaxillary suture distance, the time differences between T1 and T2 were relatively short (4.4 ± 2.1 months), and little growth effect was expected.
Increased nasal airway dimensions after palatal expansion have been reported in previous studies [23,24]. The current study results demonstrated increased dimensions of the nasal width not only in the lower part, which is structurally near the palate, but also in the upper nasal width, which was significantly increased. These results indirectly support the hypothesis that the nasal airway volume increases with MARPE treatment. We also evaluated changes in nasal septum deviation after palatal expansion. Nasal septal deviation is associated with nasal obstruction, which leads to nasal breathing difficulties [25]. Therefore, relieving nasal septum deviation after MARPE would be another explanation for better nasal breathing after palatal expansion as reported in the literature [23,26,27]. However, few studies have been conducted on this issue, and the results are conflicting [28,29]. Meanwhile, no significant change in the nasal septum deviation angle measured before and after palatal expansion was observed in this study, indicating that the nasal septum deviation did not improve after MARPE expansion. However, this measurement represented only the coronal plane and did not evaluate the horizontal plane. Furthermore, this study did not evaluate long-term changes. Further investigation is required to address this issue.
5. Conclusions
The CBCT images of the 20 patients who underwent MARPE were investigated to detect the skeletal and dental effects of MARPE.
- Significant skeletal expansion in the palate and nasal bones and dental expansion of the anchored maxillary first molars were observed.
- Splitting of the midpalatal suture was greater in the anterior than the posterior region. However, the midpalatal suture splitting pattern of the MARPE was more parallel than that of the conventional RPE, as reported in previous studies.
- A significant inter-zygomaticomaxillary suture width was identified, but this needs to be interpreted carefully because of possible growth effects.
- Changes in the nasal septum deviation were not observed in this study; however, further studies are needed to fully address this issue.
Author Contributions
Conceptualization, J.J.P. and Y.-G.K.; methodology, K.-A.K. and H.-R.K.; formal analysis, J.J.P., S.O.H. and H.-R.K.; writing of the original draft, J.J.P. and Y.-G.K.; writing, review, and editing, S.O.H. and Y.-G.K.; supervision, K.-A.K.; funding acquisition, S.O.H. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the National Research Foundation of Korea (NRF) and by the Korea government (MSIT; Ministry of Science and ICT) (No. 2021R1F1A1049784).
Institutional Review Board Statement
This study was approved by the Institutional Review Board of the Kyung Hee University Hospital at Gangdong (approval no. KHNMC 2023-01-031).
Informed Consent Statement
The requirement for obtaining informed consent from the participants was waived owing to the retrospective nature of the study.
Data Availability Statement
The authors declare that the materials are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- McNamara, J.A. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef] [PubMed]
- Bucci, R.; D’Antò, V.; Rongo, R.; Valletta, R.; Martina, R.; Michelotti, A. Dental and skeletal effects of palatal expansion techniques: A systematic review of the current evidence from systematic reviews and meta-analyses. J. Oral Rehabilitation 2016, 43, 543–564. [Google Scholar] [CrossRef] [PubMed]
- Baik, H.-S.; Kang, Y.-G.; Choi, Y.J. Miniscrew-assisted rapid palatal expansion: A review of recent reports. J. World Fed. Orthod. 2020, 9, S54–S58. [Google Scholar] [CrossRef]
- Lin, L.; Ahn, H.-W.; Kim, S.-J.; Moon, S.-C.; Kim, S.-H.; Nelson, G. Tooth-borne vs. bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015, 85, 253–262. [Google Scholar] [CrossRef]
- Moon, H.-W.; Kim, M.-J.; Ahn, H.-W.; Kim, S.-J.; Kim, S.-H.; Chung, K.-R.; Nelson, G. Molar Inclination and Surrounding Alveolar Bone Change Relative to the Design of Bone-borne Maxillary Expanders: A CBCT study. Angle Orthod. 2020, 90, 13–22. [Google Scholar] [CrossRef]
- Jia, H.; Zhuang, L.; Zhang, N.; Bian, Y.; Li, S. Comparison of skeletal maxillary transverse deficiency treated by microimplant-assisted rapid palatal expansion and tooth-borne expansion during the post-pubertal growth spurt stage. Angle Orthod. 2021, 91, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Kapetanović, A.; I Theodorou, C.; Bergé, S.J.; Schols, J.G.J.H.; Xi, T. Efficacy of Miniscrew-Assisted Rapid Palatal Expansion (MARPE) in late adolescents and adults: A systematic review and meta-analysis. Eur. J. Orthod. 2021, 43, 313–323. [Google Scholar] [CrossRef]
- Cantarella, D.; Dominguez-Mompell, R.; Moschik, C.; Sfogliano, L.; Elkenawy, I.; Pan, H.C.; Mallya, S.M.; Moon, W. Zygomaticomaxillary modifications in the horizontal plane induced by micro-implant-supported skeletal expander, analyzed with CBCT images. Prog. Orthod. 2018, 19, 41. [Google Scholar] [CrossRef]
- Cantarella, D.; Dominguez-Mompell, R.; Mallya, S.M.; Moschik, C.; Pan, H.C.; Miller, J.; Moon, W. Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. Prog. Orthod. 2017, 18, 1–12. [Google Scholar] [CrossRef]
- Choi, S.-H.; Shi, K.-K.; Cha, J.-Y.; Park, Y.-C.; Lee, K.-J. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016, 86, 713–720. [Google Scholar] [CrossRef]
- de Jesus, A.S.; de Oliveira, C.B.; Murata, W.H.; Suzuki, S.S.; dos Santos-Pinto, A. Would midpalatal suture characteristics help to predict the success rate of miniscrew-assisted rapid palatal expansion? Am. J. Orthod. Dentofac. Orthop. 2021, 160, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Park, J.J.; Park, Y.-C.; Lee, K.-J.; Cha, J.-Y.; Tahk, J.H.; Choi, Y.J. Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study. Korean J. Orthod. 2017, 47, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Noh, Y.; Choi, Y.J.; Chung, C.; Lee, H.S.; Kim, K.-H. Dentofacial transverse development in Koreans according to skeletal maturation: A cross-sectional study. Korean J. Orthod. 2018, 48, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Canan, S.; Şenışık, N.E. Comparison of the treatment effects of different rapid maxillary expansion devices on the maxilla and the mandible. Part 1: Evaluation of dentoalveolar changes. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1125–1138. [Google Scholar] [CrossRef]
- Lim, H.-M.; Park, Y.-C.; Lee, K.-J.; Kim, K.-H.; Choi, Y.J. Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. Korean J. Orthod. 2017, 47, 313–322. [Google Scholar] [CrossRef]
- Lee, R.J.; Moon, W.; Hong, C. Effects of monocortical and bicortical mini-implant anchorage on bone-borne palatal expansion using finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 887–897. [Google Scholar] [CrossRef]
- Haas, A.J. The Treatment of Maxillary Deficiency by Opening the Midpalatal Suture. Angle Orthod. 1965, 35, 200–217. [Google Scholar]
- Garib, D.G.; Henriques, J.F.C.; Janson, G.; Freitas, M.R.; Coelho, R.A. Rapid maxillary expansion—Tooth tissue-borne versus tooth-borne expanders: A computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005, 75, 548–557. [Google Scholar]
- Yoon, S.; Lee, D.-Y.; Jung, S.-K. Influence of changing various parameters in miniscrew-assisted rapid palatal expansion: A three-dimensional finite element analysis. Korean J. Orthod. 2019, 49, 150–160. [Google Scholar] [CrossRef]
- Seong, E.-H.; Choi, S.-H.; Kim, H.-J.; Yu, H.-S.; Park, Y.-C.; Lee, K.-J. Evaluation of the effects of miniscrew incorporation in palatal expanders for young adults using finite element analysis. Korean J. Orthod. 2018, 48, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Xu, T.; Zou, W. Effects of rapid maxillary expansion on the midpalatal suture: A systematic review. Eur. J. Orthod. 2015, 37, 651–655. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Wang, D.; Kuo, C.-L.; Mu, J.; Vich, M.L.; Allareddy, V.; Tadinada, A.; Yadav, S. Long-term effects of mini-screw–assisted rapid palatal expansion on airway. Angle Orthod. 2020, 91, 195–205. [Google Scholar] [CrossRef]
- Prévé, S.; Alcázar, B.G. Interest of miniscrew-assisted rapid palatal expansion on the upper airway in growing patients: A systematic review. Int. Orthod. 2022, 20, 100657. [Google Scholar] [CrossRef] [PubMed]
- Sooknundun, M.; Kacker, S.K.; Bhatia, R.; Deka, R. Nasal septal deviation: Effective intervention and long term follow-up. Int. J. Pediatr. Otorhinolaryngol. 1986, 12, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Brunetto, D.P.; Moschik, C.E.; Dominguez-Mompell, R.; Jaria, E.; Sant’anna, E.F.; Moon, W. Mini-implant assisted rapid palatal expansion (MARPE) effects on adult obstructive sleep apnea (OSA) and quality of life: A multi-center prospective controlled trial. Prog. Orthod. 2022, 23, 3. [Google Scholar] [CrossRef] [PubMed]
- Calvo-Henriquez, C.; Megias-Barrera, J.; Chiesa-Estomba, C.; Lechien, J.R.; Alvarado, B.M.; Ibrahim, B.; Suarez-Quintanilla, D.; Kahn, S.; Capasso, R. The Impact of Maxillary Expansion on Adults’ Nasal Breathing: A Systematic Review and Meta-Analysis. Am. J. Rhinol. Allergy 2021, 35, 923–934. [Google Scholar] [CrossRef] [PubMed]
- Aziz, T.; Wheatley, F.C.; Ansari, K.; Lagravere, M.; Major, M.; Flores-Mir, C. Nasal septum changes in adolescent patients treated with rapid maxillary expansion. Dent. Press J. Orthod. 2016, 21, 47–53. [Google Scholar] [CrossRef]
- Bruno, G.; De Stefani, A.; Benetazzo, C.; Cavallin, F.; Gracco, A. Changes in nasal septum morphology after rapid maxillary expansion: A Cone-Beam Computed Tomography study in pre-pubertal patient. Dent. Press J. Orthod. 2020, 25, 51–56. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).