Featured Application
Opportunistic CBCT scans may be used to assess bone mineral density and fracture risk, improving the ability to track disease progression and helping clinicians to provide better care as osteoporosis can be detected early.
Abstract
Dual-energy X-ray absorptiometry is used to determine bone density in several pathologies, namely osteoporosis and fracture risk in post-menopausal women. The aim of this study was to identify, appraise and synthesize all available evidence about the correlation between Dual Energy X-ray Absorptiometry (DEXA) and Cone Beam Computed Tomography (CBCT) techniques through a systematic review. A systematic literature search was conducted in the following databases: PubMed via MEDLINE, Cochrane Library, EMBASE and Web of Science Core Collection, along with several sources of grey literature. The Cochrane Risk of Bias Tools were used to perform the qualitative assessment of the selected studies. A total of 913 articles were initially scrutinized and 11 were included for qualitative analysis, of which 3 were included in a meta-analysis. Most of the included studies revealed a low risk of bias (7 out of 11). A strong correlation (min r = 0.46 max r = 0.62) between DEXA and CBCT values were found. Thus, opportunistic CBCT scans may be used to assess the bone mineral density and fracture risk, improving the ability to track disease progression and providing better care.
1. Introduction
Osteoporosis is the most common bone disorder worldwide affecting over 27 million people in Europe alone. This disease is associated with decreased bone density, structural bone changes and an increased fracture risk [1]. During the last 30 years, osteoporosis prevalence has increased and with it, the capability of imaging technologies used for clinical assessment [2].
Dual-energy X-ray absorptiometry (DEXA or DXA) is used to determine bone density by combining two X-ray beans with different energy levels [3,4,5,6]. DEXA is used to monitor osteoporosis and assess fracture risk in mostly post-menopausal women [7]. From 1994 on, T-score (standard deviations compared with a young adult—reference population) has been used as a scale to classify bone mineral density (BMD) measurements in postmenopausal women. The T-scores evaluated were: (1) health: T-score value greater or equal to −1; (2) osteopenia: T-score value between −2.5 and −1; (3) osteoporosis: T-score value less or equal to −2.5. This classification was later adopted for all men, women and children by the International Society for Clinical Densitometry [7]. DEXA is regarded as the gold standard technique to assess BMD and despite being widely disseminated; it is scarcely used in Dentistry [7].
Computed Tomography (CT) has several uses in bone analysis and has been used in healthcare and diagnostic investigation, so it may be used to evaluate osteoporosis [1]. In dentistry, Cone Beam Computed Tomography (CBCT) scanners are increasingly used to evaluate morphologic information [8]. CBCT can additionally aid in bone density estimations through a linear correlation between CBCT voxels values (usually in Hounsfield units) and bone mineral content [8]. Knowing bone mineral density is crucial in some fields of dentistry such as Implantology [9]. To use CBCT for bone mineral density assessment, this exam must present with equal accuracy to the gold-standard technique (DEXA) [3].
If a strong correlation coefficient is established between DEXA and CBCT, this suggests that a CBCT can be used to evaluate patients with low BMD with the same level of assurance as DEXA. In dentistry the CBCT is commonly used to more accurately help plan future interventions, but it can be additionally used to detect low bone density without additional scans (e.g., DEXA), thus avoiding exposure to any additional radiation whilst reducing costs and saving time. The opportunity for osteoporosis diagnosis using CBCT has been reported in literature, albeit sparsely.
The aim of this systematic review is to identify, appraise and synthesize all available evidence regarding the correlation between Dual Energy X-ray Absorptiometry and Cone Beam Computed Tomography techniques in the evaluation of bone mineral density.
2. Materials and Methods
2.1. Protocol
The proposed systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The present systematic review aims to answer the following question according to the PICO model (P—population; I—intervention; C—Comparative Intervention; O—Outcome): “What is the correlation coefficient between DEXA and CBCT technologies in the determination of bone mineral density in osteoporosis patients?”. The protocol for this systematic review was registered on PROSPERO with CRD42018100209 number.
2.2. Strategy and Study Selection
A systematic literature search was conducted on the following databases: MEDLINE via PubMed via MedLine, Cochrane Library, EMBASE and Web of Science Core Collection (All databases). The search for grey literature included ProQuest (Database, EBooks and Technology for Research), HSRProj and Onegrey. The search was performed until 6 March 2023, independently by two reviewers. The Search Strategies are detailed in Table S1. No restrictions on publication date were applied but language filters (English, Portuguese, and Spanish) were considered. A manual search of the reference list of the retrieved studies selected for critical appraisal was also conducted.
Results of all database searches were collated and uploaded to Mendeley v1.19.5 (Mendeley Ltd., Elsevier, Amsterdam, The Netherlands), and all duplicates were removed. Subsequently, the titles and abstracts were independently screened by two reviewers and assessed according to the eligibility criteria. Any disagreements were resolved by a third review author. If the article did not have the information for the authors to make the decision, the article was collected for reading the full text.
The following inclusion criteria were used: (1) Participants: adults (aged 18 years and over), male or female, with or without a diagnosis of osteoporosis, and with or without bone fractures; (2) papers where a correlation coefficient was calculated to assess the relationship between BMD measured with CBCT and the lumbar spine or femoral neck BMD measured by DEXA; (3) Study design: randomized controlled trials (RCTs), controlled clinical trials (CCTs) and cohort studies that show the correlation coefficient between DEXA and CBCT; 4) studies in humans. The following exclusion criteria were considered: (1) Participants: children or animal studies; (2) papers where a correlation coefficient between DEXA and CBCT technologies was not calculated; (3) Study design: case reports, case series, editorials, conference abstracts, opinion letters, book chapters; (4) studies with missing data.
The full text of relevant papers was screened by two independent reviewers and whenever a consensus was not reached, a third researcher was consulted.
2.3. Data Extraction
The data gathered from the papers included in this review was the following: author and year of publication, size and type of samples analyzed (experimental/control group, sex, age, pathologies), description of DEXA and CBCT equipment, locations analyzed by DEXA and CBCT, software used to analyze CBCT images, field of view (FOV) and Voxel size used, the correlation coefficients between BMD values obtained with DEXA and CBCT, and the main conclusions of each study). Authors of papers were contacted to request missing or additional data when required. Any disagreements between the reviewers were solved by a third reviewer.
2.4. Risk of Bias
Selected papers were assessed by two independent reviewers for methodological quality. The Cochrane Risk of Bias Tools were used to perform the qualitative assessment of the selected studies. Depending on the type of study, the corresponding Cochrane Risk of Bias Tool was chosen, and the quality assessment was performed independently by two review authors. Any disagreements between the reviewers were solved by a third reviewer. The overall risk of individual bias studies was categorized into three categories: low- all domains evaluated with low risk of bias; moderate- low or moderate risk of bias for all domains; severe if at least one domain presents a severe risk assessment bias.
2.5. Statistical Analysis
Based on the coefficients of correlation between BMD values obtained with DEXA and CBCT extracted from the included papers, a meta-analysis was conducted to determine the strength of correlation between the two imaging techniques regarding their ability for measuring BMD. The summary measure adopted for the meta-analysis was the correlation coefficient between CBCT and DEXA values. As some of the studies acquired images in more than one location showing various correlation values, it was decided that two meta-analysis studies would be persormed: one with the minimum correlation value and one with the maximum value. A forest-plot was produced for each study. The summary measure was calculated using the random effects model, and heterogeneity was assessed using Cochran’s Q test and the I2 statistic. Meta-analysis was performed in R using the metafor package and a 5% significance level was adopted.
3. Results
In the first stage of this study, a total of 913 articles were identified from the electronic databases. A total of 11 papers met the eligibility criteria and were included in this Systematic Review. Figure 1 shows the flowchart that illustrates the references search and selection process.
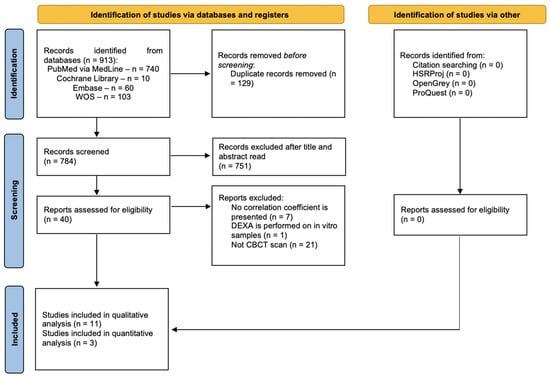
Figure 1.
PRISMA flowchart diagram. This diagram represents all the information during the different phases, from identification, screnning and inclusion of studies.
3.1. Description of the Included Studies
Only one study mentions a random patient sample, and the sample group sizes varied from 23 to 81 individuals [10]. Out of the 11 studies that were assessed, five contained sample groups solely comprised of female individuals [10,11,12,13,14,15], another five studies analyzed samples with both male and female individuals [10,16,17,18,19], and only one study assessed an exclusively male group [20]. Four of the eleven studies specifically evaluated post-menopausal females [11,13,14,15], one study evaluated acromegaly patients [20] and one study evaluated diabetic patients [20].
Radiomorphometric analysis were used to assess BMD from CBCT images in several of the included studies. One author was involved in 3 studies [13,14,15] using the same sample comprised of 38 post-menopausal female patients. Although it is the same sample, the analyzes performed are from different bone zones and therefore were included as independent studies. The main results of both studies concluded that CBCT-derived radiographic density (RD) measurements of the body and ramus of the mandible and cervical vertebrae could help predict osteoporosis with an accuracy of 75% for lumbar vertebrae (LV) and 78.4% for femoral neck(FN) [15], accuracy of 90.8% for LV and 86.4% [13]. A strong correlation with LV and FN in trabecular bone structure of jawbones and odontoid process comparision, thus the authors concluded the dens-derived measures can accurately predict osteoporosis [14].
The majority of the studies chose the lumbar spine as the preferred structure to assess BMD and to posteriorly compare the results to the CBCT of the mandibular cortical and cancellous bone. Four of the included studies compared the mandibular cortical bone with the lumbar spine DEXA obtaining an r value that fluctuated from 0.411 to 0.857 [12,16,17,19,20]. The highest correlation value that was observed among all the selected articles was of r = 0.924 and it was attained when comparing the cortical foramen and the femoral neck [17], in contrast, the lowest correlation value was observed between the distal epiphysis border of the radius and the femoral neck with an r = 0.17 [19]. In general, it was concluded that BMD presents lower values in osteoporotic groups when compared to osteopenia and/or control groups.
Regarding the software used [16,17] of the eleven studies made no mention of the chosen software to analyze CBCT images. Three of the studies by the same author used the WhiteFox ® Imaging v.3 (Acteon Group Ltd., Milan, Italy) software [13,14,15]. The i-Cat vision (Imaging Sciences International Inc., Hatfield, PA, USA) software was only used in oneof the studies [10]. Two out of the 11 studies assessed used Planmeca Romexis (Helsinki, Finland), another two [11,18] used the OnDemand 3-D Dental Software (CyberMed, Seoul, Republic of Korea) and only one studyused the BoneJ 1.3.9 program, (U.S. National Institutes of Health, Bethesda, MD, USA) [19].
FOV and voxel size are also important factors to take into account and two studies [16,17] did not provide any information about these variables. Shokri et al. [11] provided information regarding the FOV: 13 × 14 cm and Sghaireen et al. [18] only provided information about the Voxel Size: 0.2 mm. Three studies [13,14,15] used values of FOV: 13 × 15 cm and Voxel size: 0.25 mm. All other studies used different FOV and voxel values with one of these using FOV: 13 × 15 cm and Voxel size: 0.25 mm [10], another using FOV: 8 × 8 cm and Voxel size: 0.2 mm [12]; an additional one using FOV: 8 × 8 cm and Voxel Size: 0.75 mm [19] and lastly, another one using FOV: 4 × 4 cm and Voxel size: 0.4 mm [20]. Table 1 summarize the characteristics of the articles included.

Table 1.
Characteristics of included studies in the qualitative analysis.
The coefficients values found within the studies are described in Table 2. The highest value was r = 0.924 [17] and the lower value was r = 0.08 [19], with a discrepancy of 0.8 values between the higher and the lower values.

Table 2.
Coefficients of correlation between BMD values obtained with DEXA and CBCT technologies.
3.2. Quantitative Analysis
A meta-analysis was conducted to determine the strength of correlation between the two imaging techniques regarding their ability for measuring BMD. Of the included articles, three were chosen for the quantitative assessment of the results given that these are the ones that establish a correlation between the CBCT/CT and DEXA values and presented eligibility to compare the results. The remaining articles use measures that do not allow this comparison since they use t-scores to measure the relationships between cortical bone and trabecular bone.
The following forest-plots illustrate the results for the minimum values of correlation (Figure 2).
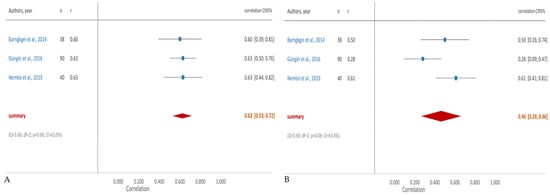
Figure 2.
Forest plot of quantitative analysis between the CBCT/CT and DEXA: (A) minimum correlation value; (B) maximum correlation value [10,15,20].
3.3. Risk of Bias
The risk of bias in randomized and non-randomized studies is summarized in Table 3 and Table 4, respectively. The only randomized trial included had a low risk of bias [11]. Regarding non-randomized studies, most of the included studies revealed a low risk of bias (6 out of 10). The remaining four have methodological flaws, 2 of them in the domain of bias due to confounding [20,21], 1 in deviations from intended interventions domain [16], and 1 with a methodologic flaw in the missing data domain [12].

Table 3.
Risk of bias in randomized trials with the analysis of the parameters: randomization process, deviations from the intended, missing outcome data, measurement of outcome, selection of the reported result and overall bias (Y green—Yes).

Table 4.
Risk of bias in non-randomized trials with the analysis of the parameters: randomization process, deviations from the intended, missing outcome data, measurement of outcome, selection of the reported result and overall bias. (Y green—Yes; N red—No).
4. Discussion
The use of CBCT scans daily in dentistry practices has increased in recent years. Dental CBCT have lower radiologic dosages relative to traditional CT scans and comparable precision CBCT scans could be used to detect patients with low BMD without additional scans (e.g., DEXA) and help refer those patients to further follow-up. The studies in this Systematic Review intended to study the possibility of using CBCT images to identify and differentiate patients with low BMD, patients with risk of developing osteoporosis and patients who had already recovered from this illness, from healthy individuals.
In this study, we intended to determinate the correlation coefficient between DEXA and CBCT derived values. In 2017 a systematic review was published, investigating the opportunist capability of CBCT to identify patients with low BMD [21]. This systematic review did not identify the correlation coefficient between DEXA and CBCT, and, consequently, did not had quantitative analysis of their results. The authors concluded that the evidence was restricted to endorse the use of CBCT derived images as a mean to diagnostic low BMD [21]. Meanwhile, new publications in recent years justify the elaboration of a new Systematic Review, particularly, with a quantitative analysis that allows the extraction of a correlation coefficient.
All included articles in this Systematic Review concluded that CBCT derived images can be used to estimate BMD and refer patients at risk of osteoporosis. However, the methodology of the included papers was different, different indices (qualitative and linear) were used in the included studies as an opportunist diagnostic tools for low BMD. Furthermore, seven of the included papers in this review, resorted to those indices to differentiate patients with low BMD from patients with normal BMD, according to DEXA results [10,11,12,16,17,18,19]. Relatively to the studies who performed their analysis in the jaw bones: Güngör et al. [10] study, assessed CT values and radio morphometric index measurements, and concluded that those values can evaluated the changes associated to osteoporosis and referred those patients for further treatment. Shokri et al. [11]. study calculated mean gray values of CBCT cross-sectional images and concluded that those where lower in post-menopausal osteoporotic and osteopenic females, than in postmenopausal normal BMD females. Furthermore, Mostafa et al. [12] analyzed the mandible CBCT derived images of normal BMD and osteoporotic females and calculated radio morphometric index measurements, concluding those were lower in osteoporotic patients, and so, could be used to refer patients in risk of osteoporosis. Sghaireen et al. [18] used CBCT-derived grayscale values (GS) from jawbones to discriminate normal BMD patients and osteoporotic BMD patients and concluded that CBCT GS values are able to predict the presence of osteoporosis and DXA T-score values. Therefore, based in the results of the aforementioned studies, we can conclude that radio morphometric measurements are a capable tool for the identification of low BMD patients.
The samples of the included studies were very distinct. Considering sex and health status, seven studies compared osteoporotic men and women, with healthy men and women with normal BMD, according to DEXA results [10,11,12,16,17,18,19]. Pathophysiology, aged-bone loss in women is related with a combination of a negative remodeling balance and an increase of bone remodeling (both in cortical and cancellous bone), and in men, the aged-related bone loss is mostly related with reduction of bone formation, and reduction of bone turnover, however, the World Health Organization and the International Society for Clinical Densitometry stated, recently, that risk of fracture in men and females occurs proximally at the same BMD [22]. Still on the issue of samples of the included studies, one study [20] performed their analysis in a group of diabetic patients (type I and II patients were analyzed). The neuropathy of diabetes mellitus (DM) amplified severally the possibility of developing osteoporosis, and consequently, the likelihood of disease-related fractures, morbidity, and mortality [23]. However, the risk of osteoporosis and the values of BMD in DM patients are not well described, and although most papers stated a lower BMD in DM type I patients, other studies claimed that BMD may be greater, similar or lower in DM type II patients [20]. Another study performed their analysis in acromegaly patients [19], and according to recent data, although BMD in acromegaly patients may be higher, similar or lower and there is no agreement of BMD and the appearance of fractures, a lower hip BMD founded in acromegaly patients has been related to the presence vertebral fractures in those patients [24].
Regarding to the coefficient values, we can state that Ko et al. [17] obtained the highest coefficient values, (r = 0.924). However, this study had a small sample of people included with 14 on the case group and 14 in the control group [17].
The present study has some limitations namely the discrepancy in anatomical structures chosen to perform the DEXA which can introduce a bias due to possible variations in DEXA values in different structures [25]. Also, several studies obtained radiographic density though grey values derived from CBCT images, and those values change with FOV and Voxel size [26]. In addition, BMD in some mandibular areas can be affected by local conditions, which must be taken into account.
Other limitations can be scrutinized such as the CBCT equipment used to evaluate BMD which was not the same for all studies and when technical parameters change (like FOV and voxel size), the quality of the image also changes, especially spatial resolution [27]. Five studies [10,11,13,14,15] used the similar FOV and voxel size, however 3 studies had different FOV and voxel sizes, and two studies [16,17] did not have any information about FOV and voxel size. In this study local factors such as occlusal forces and masseter muscle tensions were not considered despite their possible influence on the mandibular bony areas, constituting an additional limitation. Further investigation is mandatory to understand if these different technical parameters may change aforementioned results. Also, all included studies had a small and heterogenic sample of individuals analyzed. Control groups were quite diverse and some disagreement: some studies included only healthy normal BMD patients, but others included osteoporotic patients, and some studies included normal BMD and osteopenic patients in the control group.
Future studies should be performed in order to obtain further evidence, with standardized protocols taking into account the chosen structures for analysis, a more robust sample group and more homogenous in terms of heal status, sex, age and health characteristics.
5. Conclusions
A strong correlation (min r = 0.46 max r = 0.62) between DEXA and CBCT values were found. Thus, opportunistic CBCT scans may be used to assess the bone mineral density and fracture risk, improving the ability to track disease progression and providing better care.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app13105962/s1, Table S1: Search Strategies.
Author Contributions
Conceptualization, F.C. and F.V.; Data curation, F.C.; Formal analysis, C.N., F.P. and F.C.; Investigation, C.N., R.T. and C.M.M.; Methodology, I.F., F.P. and F.C.; Project administration, F.V.; Resources, C.M.M.; Supervision, I.F. and F.V.; Validation, M.M., M.S. and C.O.; Visualization, C.O.; Writing—original draft, F.P., F.M. and M.M.; Writing—review & editing, M.P.R., M.S. and A.B.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Grüneboom, A.; Kling, L.; Christiansen, S.; Mill, L.; Maier, A.; Engelke, K.; Quick, H.H.; Schett, G.; Gunzer, M. Next-Generation Imaging of the Skeletal System and Its Blood Supply. Nat. Rev. Rheumatol. 2019, 15, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Griffith, J.F.; Genant, H.K. New Advances in Imaging Osteoporosis and Its Complications. Endocrine 2012, 42, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.-T.; Chen, Y.-J.; Tsai, M.-T.; Lan, H.H.-C.; Cheng, F.-C.; Chen, M.Y.C.; Wang, S.-P. Predicting Cortical Bone Strength from DXA and Dental Cone-Beam CT. PLoS ONE 2012, 7, e50008. [Google Scholar] [CrossRef] [PubMed]
- Khoo, B.C.C.; Brown, K.; Cann, C.; Zhu, K.; Henzell, S.; Low, V.; Gustafsson, S.; Price, R.I.; Prince, R.L. Comparison of QCT-Derived and DXA-Derived Areal Bone Mineral Density and T Scores. Osteoporos. Int. 2009, 20, 1539–1545. [Google Scholar] [CrossRef] [PubMed]
- Bachrach, L.K.; Gordon, C.M.; Sills, I.N.; Lynch, J.L.; Casella, S.J.; DiMeglio, L.A.; Gonzalez, J.L.; Wintergerst, K.; Kaplowitz, P.B. Bone Densitometry in Children and Adolescents. Pediatrics 2016, 138, e20162398. [Google Scholar] [CrossRef] [PubMed]
- Crabtree, N.; Ward, K. Bone Densitometry: Current Status and Future Perspective. In Calcium and Bone Disorders in Children and Adolescents; Karger Publishers: Berlin, Germany, 2015; pp. 72–83. [Google Scholar]
- Link, T.M. Osteoporosis Imaging: State of the Art and Advanced Imaging. Radiology 2012, 263, 3–17. [Google Scholar] [CrossRef]
- Yepes, J.F.; Al-Sabbagh, M. Use of Cone-Beam Computed Tomography in Early Detection of Implant Failure. Dent. Clin. N. Am. 2015, 59, 41–56. [Google Scholar] [CrossRef]
- Jeong, K.-I.; Kim, S.-G.; Oh, J.-S.; Jeong, M.-A. Consideration of Various Bone Quality Evaluation Methods. Implant. Dent. 2013, 22, 55–59. [Google Scholar] [CrossRef]
- Güngör, E.; Yildirim, D.; Çevik, R. Evaluation of Osteoporosis in Jaw Bones Using Cone Beam CT and Dual-Energy X-ray Absorptiometry. J. Oral Sci. 2016, 58, 185–194. [Google Scholar] [CrossRef]
- Shokri, A.; Ghanbari, M.; Maleki, F.H.; Ramezani, L.; Amini, P.; Tapak, L. Relationship of Gray Values in Cone Beam Computed Tomography and Bone Mineral Density Obtained by Dual Energy X-ray Absorptiometry. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 319–331. [Google Scholar] [CrossRef]
- Mostafa, R.A.; Arnout, E.A.; Abo el-Fotouh, M.M. Feasibility of Cone Beam Computed Tomography Radiomorphometric Analysis and Fractal Dimension in Assessment of Postmenopausal Osteoporosis in Correlation with Dual X-ray Absorptiometry. Dentomaxillofac. Radiol. 2016, 45, 20160212. [Google Scholar] [CrossRef] [PubMed]
- Barngkgei, I.; Al Haffar, I.; Shaarani, E.; Khattab, R.; Mashlah, A. Assessment of Jawbone Trabecular Bone Structure amongst Osteoporotic Women by Cone-Beam Computed Tomography: The OSTEOSYR Project. J. Investig. Clin. Dent. 2016, 7, 332–340. [Google Scholar] [CrossRef]
- Barngkgei, I.; Joury, E.; Jawad, A. An Innovative Approach in Osteoporosis Opportunistic Screening by the Dental Practitioner: The Use of Cervical Vertebrae and Cone Beam Computed Tomography with Its Viewer Program. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 651–659. [Google Scholar] [CrossRef]
- Barngkgei, I.; Al Haffar, I.; Khattab, R. Osteoporosis Prediction from the Mandible Using Cone-Beam Computed Tomography. Imaging Sci. Dent. 2014, 44, 263. [Google Scholar] [CrossRef] [PubMed]
- Jeong, K.; Ko, H.; Lee, C.-H.; Lee, M.; Yoon, K.-H.; Lee, J. A Novel Method for Estimation of Femoral Neck Bone Mineral Density Using Forearm Images from Peripheral Cone Beam Computed Tomography. Appl. Sci. 2016, 6, 113. [Google Scholar] [CrossRef]
- Ko, H.; Lee, C.H.; Jeong, K.; Lee, M.S.; Nam, Y.; Yoon, K.H.; Lee, J. A Pilot Study on Hip Bone Mineral Densities Estimation from Forearm CBCT Images. KSII Trans. Internet Inf. Syst. 2017, 11, 6054–6068. [Google Scholar] [CrossRef]
- Sghaireen, M.G.; Ganji, K.K.; Alam, M.K.; Srivastava, K.C.; Shrivastava, D.; Ab Rahman, S.; Patil, S.R.; Al Habib, S. Comparing the Diagnostic Accuracy of CBCT Grayscale Values with DXA Values for the Detection of Osteoporosis. Appl. Sci. 2020, 10, 4584. [Google Scholar] [CrossRef]
- Maffezzoni, F.; Maddalo, M.; Frara, S.; Mezzone, M.; Zorza, I.; Baruffaldi, F.; Doglietto, F.; Mazziotti, G.; Maroldi, R.; Giustina, A. High-Resolution-Cone Beam Tomography Analysis of Bone Microarchitecture in Patients with Acromegaly and Radiological Vertebral Fractures. Endocrine 2016, 54, 532–542. [Google Scholar] [CrossRef]
- Nemtoi, A.; Nemtoi, A.; Fochi, A.; Sirghe, A.E.; Preda, C.; Earar, K.; Beznea, A.; Onisor, C.; Iorgulescu, G.; Haba, D. CBCT Evaluation of the Mandibular Bone Quality in Relation to Skeletal Status after Treatment with Strontium Renelate in Diabetic Patients. Rev. Chim. 2019, 70, 4113–4118. [Google Scholar] [CrossRef]
- Guerra, E.N.S.; Almeida, F.T.; Bezerra, F.V.; Figueiredo, P.T.D.S.; Silva, M.A.G.; De Luca Canto, G.; Pachêco-Pereira, C.; Leite, A.F. Capability of CBCT to Identify Patients with Low Bone Mineral Density: A Systematic Review. Dentomaxillofac. Radiol. 2017, 46, 20160475. [Google Scholar] [CrossRef]
- Adler, R.A. Update on Osteoporosis in Men. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 759–772. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Lv, H.; Niu, P.; Tan, J.; Ma, Y. Association between Diabetic Neuropathy and Osteoporosis in Patients: A Systematic Review and Meta-Analysis. Arch. Osteoporos. 2020, 15, 125. [Google Scholar] [CrossRef] [PubMed]
- Anthony, J.R.; Ioachimescu, A.G. Acromegaly and Bone Disease. Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 476–482. [Google Scholar] [CrossRef]
- Eckstein, F.; Lochmüller, E.-M.; Lill, C.A.; Kuhn, V.; Schneider, E.; Delling, G.; Müller, R. Bone Strength at Clinically Relevant Sites Displays Substantial Heterogeneity and Is Best Predicted from Site-Specific Bone Densitometry. J. Bone Min. Res. 2002, 17, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.; Parsa, A.; Hassan, B.; van der Stelt, P.; Aartman, I.H.A.; Wismeijer, D. The Effect of Scan Parameters on Cone Beam CT Trabecular Bone Microstructural Measurements of the Human Mandible. Dentomaxillofac. Radiol. 2013, 42, 20130206. [Google Scholar] [CrossRef]
- Ibrahim, N.; Parsa, A.; Hassan, B.; van der Stelt, P.; Aartman, I.H.A.; Nambiar, P. Influence of Object Location in Different FOVs on Trabecular Bone Microstructure Measurements of Human Mandible: A Cone Beam CT Study. Dentomaxillofac. Radiol. 2014, 43, 20130329. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).