Three-Dimensional Cephalometric Analysis of Skeletal and Dental Effects in Patients Undergoing Transpalatal Distraction
Abstract
:1. Introduction
2. Material and Methods
2.1. Surgical Procedure
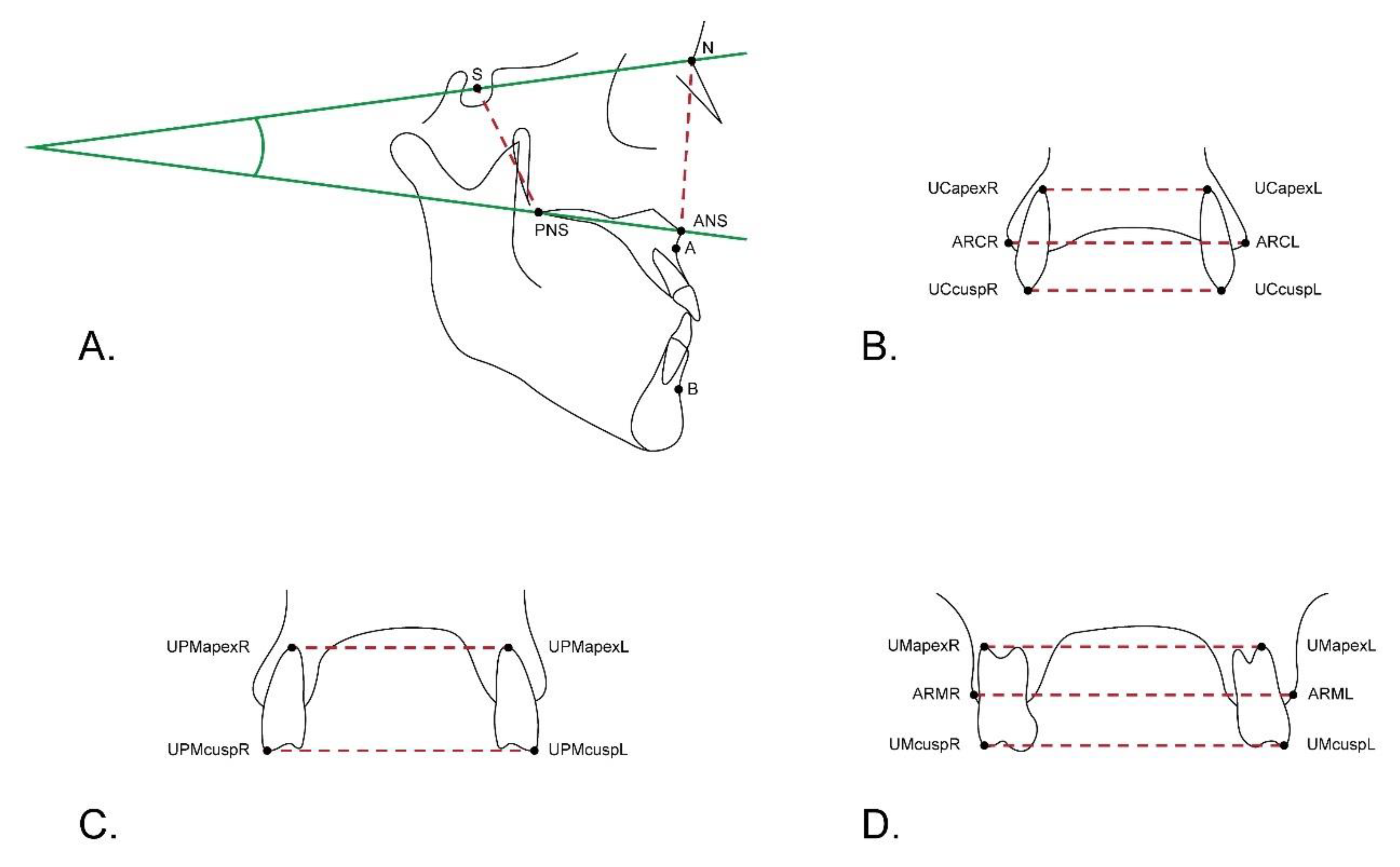
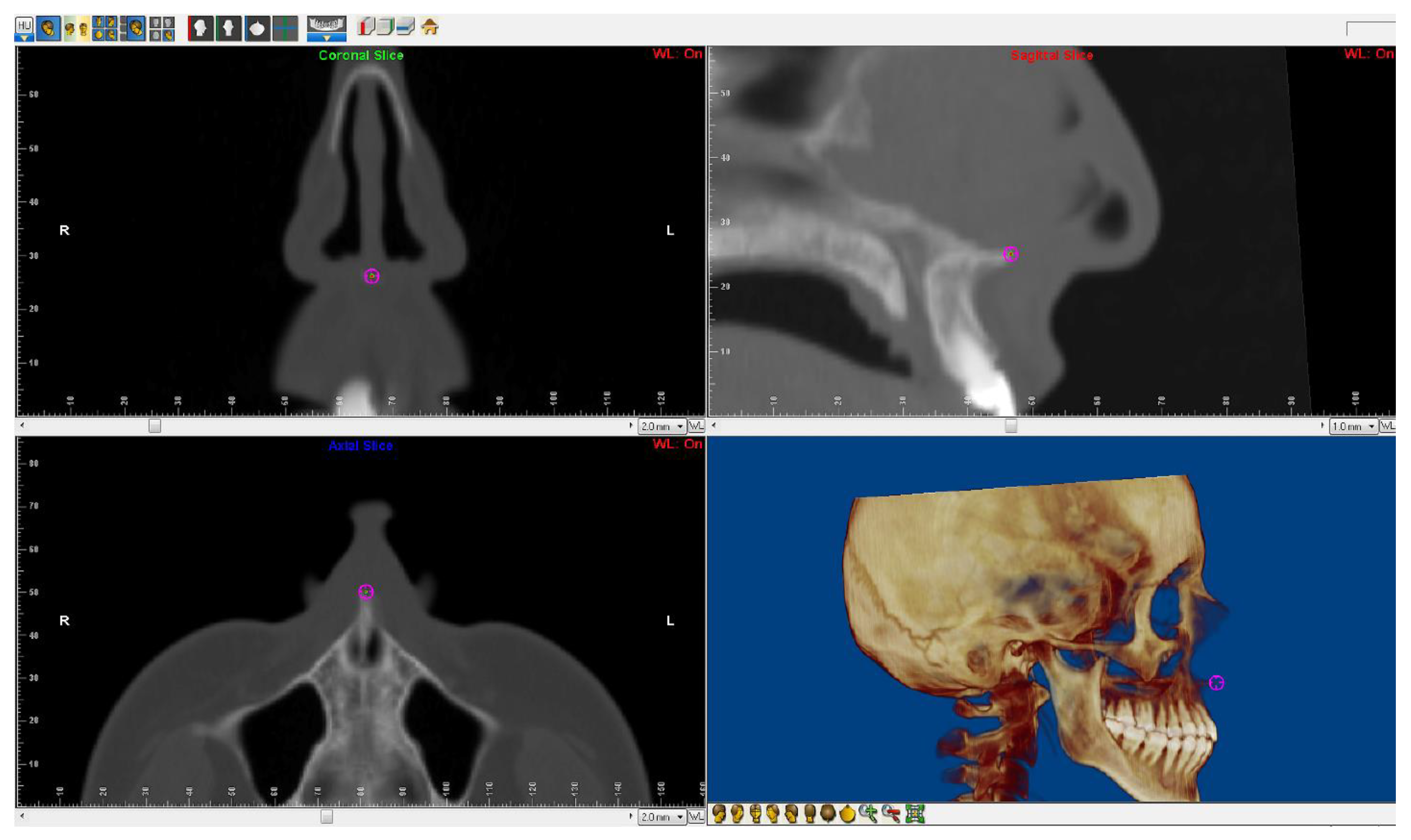
2.2. 3D Cephalometric Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
- The clear advantage of 3D analysis over 2D analysis is that the former allows the determination of changes in all planes of space using only one radiological exposure.
- TPD does not produce a significant anteroposterior displacement of the maxilla. However, factors such as surgical technique, distraction protocol, as well as individual anatomical differences may have an impact on the outcome.
- TPD causes transverse and vertical changes useful in the treatment of an open bite caused by maxillary constriction and anterior rotation of the palatal plane.
- If the SARME protocol does not involve pterygoid disjunction and the TPD is placed at the level of second premolars, more skeletal and dental expansion occurs at the anterior than at the posterior part of the maxilla, which may be beneficial in the treatment of anterior transverse maxillary deficiency.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koudstaal, M.J.; Wolvius, E.B.; Schulten, A.J.M.; Hop, W.C.J.; van der Wal, K.G.H. Stability, tipping and relapse of bone-borne versus tooth-borne surgically assisted rapid maxillary expansion; a prospective randomized patient trial. Int. J. Oral Maxillofac. Surg. 2009, 38, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Mommaerts, M.Y. Transpalatal distraction as a method of maxillary expansion. Br. J. Oral Maxillofac. Surg. 1999, 37, 268–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matteini, C.; Mommaerts, M.Y. Posterior transpalatal distraction with pterygoid disjunction: A short-term model study. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 498–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinto, P.X.; Mommaerts, M.Y.; Wreakes, G.; Jacobs, W.V.G.J.A. Immediate postexpansion changes following the use of the transpalatal distractor. J. Oral Maxillofac. Surg. 2001, 59, 994–1000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ramieri, G.A.; Spada, M.C.; Austa, M.; Bianchi, S.D.; Berrone, S. Transverse maxillary distraction with a bone-anchored appliance: Dento-periodontal effects and clinical and radiological results. Int. J. Oral Maxillofac. Surg. 2005, 34, 357–363. [Google Scholar] [CrossRef]
- Asscherickx, K.; Govaerts, E.; Aerts, J.; Vande Vannet, B. Maxillary changes with bone-borne surgically assisted rapid palatal expansion: A prospective study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 374–383. [Google Scholar] [CrossRef]
- Major, P.W.; Johnson, D.E.; Hesse, K.L.; Glover, K.E. Landmark identification error in posterior anterior cephalometrics. Angle Orthod. 1994, 64, 447–454. [Google Scholar]
- Scarfe, W.C.; Farman, A.G.; Sukovic, P. Clinical applications of cone-beam computed tomography in dental practice. J. Can. Dent. Assoc. 2006, 72, 75–80. [Google Scholar]
- Bayome, M.; Park, J.H.; Kook, Y.-A. New three-dimensional cephalometric analyses among adults with a skeletal Class I pattern and normal occlusion. Korean J. Orthod. 2013, 43, 62–73. [Google Scholar] [CrossRef] [Green Version]
- Periago, D.R.; Scarfe, W.C.; Moshiri, M.; Scheetz, J.P.; Silveira, A.M.; Farman, A.G. Linear Accuracy and Reliability of Cone Beam CT Derived 3-Dimensional Images Constructed Using an Orthodontic Volumetric Rendering Program. Angle Orthod. 2008, 78, 387–395. [Google Scholar] [CrossRef]
- Chien, P.; Parks, E.; Eraso, F.; Hartsfield, J.; Roberts, W.; Ofner, S. Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional cone beam computed tomography in vivo. Dentomaxillofac. Radiol. 2009, 38, 262–273. [Google Scholar] [CrossRef]
- de Oliveira, A.E.F.; Cevidanes, L.H.S.; Phillips CMotta ABurke, B.; Tyndall, D. Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 256–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dowgierd, K.; Borowiec, M.; Kozakiewicz, M. Bone changes on lateral cephalograms and CBCT during treatment of maxillary narrowing using palatal osteodistraction with bone-anchored appliances. J. Craniomaxillofac. Surg. 2018, 46, 2069–2081. [Google Scholar] [CrossRef] [PubMed]
- Parhiz, A.; Schepers, S.; Lambrichts, I.; Vrielinck, L.; Sun, Y.; Politis, C. Lateral cephalometry changes after SARPE. Int. J. Oral Maxillofac. Surg. 2011, 40, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Hansen, L.; Tausche, E.; Hietschold, V.; Hotan, T.; Lagravère, M.; Harzer, W. Skeletally-anchored rapid maxillary expansion using the Dresden Distractor. J. Orofac. Orthop. 2007, 68, 148–158. [Google Scholar] [CrossRef]
- Günbay, T.; Akay, M.C.; Günbay, S.; Aras, A.; Koyuncu, B.Ö.; Sezer, B. Transpalatal Distraction Using Bone-Borne Distractor: Clinical Observations and Dental and Skeletal Changes. J. Oral Maxillofac. Surg. 2008, 66, 2503–2514. [Google Scholar] [CrossRef]
- Lee, S.C.; Park, J.H.; Bayome, M.; Kim, K.B.; Araujo, E.A.; Kook, Y.-A. Effect of bone-borne rapid maxillary expanders with and without surgical assistance on the craniofacial structures using finite element analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 638–648. [Google Scholar] [CrossRef]
- Krebs, A. Expansion of the Midpalatal Suture, Studied by Means of Metallic Implants. Acta Odontol. Scand. 1959, 17, 491–501. [Google Scholar] [CrossRef]
- Glassman, A.S.; Nahigian, S.J.; Medway, J.M.; Aronowitz, H.I. Conservative surgical orthodontic adult rapid palatal expansion: Sixteen cases. Am. J. Orthod. 1984, 86, 207–213. [Google Scholar] [CrossRef]
- Tausche, E.; Hansen, L.; Hietschold, V.; Lagravère, M.O.; Harzer, W. Three-dimensional evaluation of surgically assisted implant bone-borne rapid maxillary expansion: A pilot study. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S92–S99. [Google Scholar] [CrossRef]
- Landes, C.A.; Laudemann, K.; Schübel, F.; Petruchin, O.; Mack, M.; Kopp, S.; Sader, R.A. Comparison of Tooth- and Bone-Borne Devices in Surgically Assisted Rapid Maxillary Expansion by Three-Dimensional Computed Tomography Monitoring: Transverse Dental and Skeletal Maxillary Expansion, Segmental Inclination, Dental Tipping, and Vestibular Bone Resorption. J. Craniofac. Surg. 2009, 20, 1132–1141. [Google Scholar] [PubMed]
- Zandi, M.; Miresmaeili, A.; Heidari, A. Short-term skeletal and dental changes following bone-borne versus tooth-borne surgically assisted rapid maxillary expansion: A randomized clinical trial study. J. Craniomaxillofac. Surg. 2014, 42, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
| Measurement | N | Mean | SD | Min | Med | Max | p1 | p2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | ||||
| N-ANS (mm) | 50.29 | 51.34 | 51.55 | 4.10 | 3.81 | 3.97 | 42.70 | 42.30 | 42.60 | 49.70 | 50.85 | 50.95 | 57.70 | 58.20 | 58.80 | ||||
| 2-1 | 34 | 1.05 | 1.28 | −1.20 | 1.35 | 3.10 | <0.001 | 0.0001 | |||||||||||
| 3-2 | 34 | 0.22 | 0.81 | −1.30 | 0.20 | 2.10 | 0.52 | ||||||||||||
| 3-1 | 34 | 1.27 | 1.35 | −1.00 | 1.55 | 4.10 | 0.0001 | ||||||||||||
| S-PNS (mm) | 45.14 | 45.39 | 45.68 | 4.01 | 4.15 | 4.13 | 37.10 | 37.30 | 37.80 | 46.05 | 46.60 | 46.15 | 51.70 | 52.20 | 52.60 | ||||
| 2-1 | 34 | 0.24 | 0.56 | −1.10 | 0.25 | 1.40 | <0.001 | 0.0001 | |||||||||||
| 3-2 | 34 | 0.30 | 0.52 | −0.90 | 0.30 | 1.60 | 0.01 | ||||||||||||
| 3-1 | 34 | 0.54 | 0.68 | −0.90 | 0.60 | 1.80 | 0.045 | ||||||||||||
| ARMR-ARML (mm) | 51.87 | 57.82 | 56.68 | 4.69 | 4.88 | 4.47 | 41.90 | 47.00 | 47.30 | 51.40 | 56.80 | 56.25 | 64.00 | 68.50 | 67.50 | ||||
| 2-1 | 34 | 5.95 | 2.15 | 3.10 | 5.30 | 12.20 | <0.001 | <0.001 | |||||||||||
| 3-2 | 34 | −1.14 | 1.11 | −3.60 | −0.95 | 0.30 | <0.001 | ||||||||||||
| 3-1 | 34 | 4.81 | 2.41 | 1.00 | 5.00 | 12.10 | <0.001 | ||||||||||||
| ARCR-ARCL (mm) | 35.02 | 43.45 | 41.41 | 3.58 | 3.20 | 3.92 | 25.82 | 37.60 | 34.70 | 34.15 | 43.00 | 41.80 | 42.20 | 51.30 | 50.60 | ||||
| 2-1 | 34 | 8.43 | 2.38 | 3.90 | 8.25 | 17.40 | <0.001 | <0.001 | |||||||||||
| 3-2 | 34 | −2.04 | 1.45 | −4.80 | −2.15 | 0.50 | <0.001 | ||||||||||||
| 3-1 | 34 | 6.39 | 2.85 | 0.20 | 5.55 | 16.70 | <0.001 | ||||||||||||
| SNA (°) | 82.12 | 82.06 | 82.15 | 3.19 | 3.22 | 3.20 | 77.11 | 76.92 | 77.08 | 82.10 | 82.14 | 82.16 | 90.00 | 90.30 | 90.40 | ||||
| 2-1 | 34 | 0.06 | 0.65 | −2 | 0.23 | 1.17 | 0.23 | ||||||||||||
| 3-2 | 34 | 0.09 | 0.29 | −0.3 | 0.01 | 1.01 | |||||||||||||
| 3-1 | 34 | 0.15 | 0.50 | −1.12 | 0.12 | 1.06 | |||||||||||||
| SNB (°) | 80.77 | 80.53 | 80.62 | 4.80 | 4.98 | 4.95 | 72.06 | 72.1 | 72.14 | 80.12 | 80.06 | 79.95 | 92.95 | 93.12 | 93.17 | ||||
| 2-1 | 34 | −0.24 | 0.96 | −4.36 | 0.02 | 0.12 | 0.16 | ||||||||||||
| 3-2 | 34 | 0.09 | 0.29 | 0.12 | −0.01 | 1.32 | |||||||||||||
| 3-1 | 34 | −0.15 | 0.74 | −3.11 | 0.11 | 1.24 | |||||||||||||
| ANB (°) | 1.26 | 1.53 | 1.56 | 4.07 | 4.27 | 4.31 | −11.06 | −10.95 | −11.01 | 2.06 | 2.21 | 2.14 | 8.23 | 8.17 | 8.21 | ||||
| 2-1 | 34 | 0.26 | 0.62 | −1.03 | 0.2 | 2.12 | 0.35 | ||||||||||||
| 3-2 | 34 | 0.00 | 0.00 | 0.26 | 0.11 | 0.03 | |||||||||||||
| 3-1 | 34 | 0.26 | 0.62 | −1.11 | 0.11 | 2.03 | |||||||||||||
| S-N/PNS-ANS (°) | 0.21 | 0.48 | 0.57 | 4.89 | 4.51 | 4.45 | −9.68 | −8.20 | −7.78 | 1.35 | 1.42 | 1.36 | 8.12 | 7.55 | 8.06 | ||||
| 2-1 | 34 | 0.27 | 1.04 | −0.80 | −0.05 | 1.35 | 0.27 | ||||||||||||
| 3-2 | 34 | 0.09 | 0.36 | −0.70 | 0.10 | 1.74 | |||||||||||||
| 3-1 | 34 | 0.36 | 1.25 | −1.00 | 0.10 | 5.06 | |||||||||||||
| Measurement (mm) | T | N | Mean | SD | Min | Med | Max | p1 | p2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | T1 | T2 | T3 | |||||
| UMcuspR-UMcuspL | 48.09 | 54.85 | 53.19 | 5.99 | 6.16 | 5.77 | 32.40 | 40.10 | 39.40 | 48.45 | 55.00 | 53.60 | 57.30 | 69.20 | 64.80 | ||||
| T2-T1 | 34 | 6.76 | 3.27 | 2.00 | 6.15 | 16.80 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −1.66 | 1.41 | −5.20 | −1.25 | 0.50 | <0.001 | ||||||||||||
| T3-T1 | 34 | 5.10 | 3.14 | −0.50 | 5.40 | 16.90 | 0.001 | ||||||||||||
| UMapexR-UMapexL | 48.17 | 52.81 | 51.79 | 5.31 | 5.21 | 50.08 | 340.10 | 38.30 | 37.30 | 48.00 | 51.45 | 51.00 | 58.00 | 62.10 | 60.60 | ||||
| T2-T1 | 34 | 4.64 | 1.77 | 1.70 | 4.55 | 9.20 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −1.02 | 1.45 | −3.50 | −0.85 | 2.50 | <0.001 | ||||||||||||
| T3-T1 | 34 | 3.62 | 2.71 | −1.80 | 3.70 | 8.10 | 0.004 | ||||||||||||
| UPMcuspR-UPMcuspL | 38.48 | 46.81 | 44.85 | 4.46 | 4.50 | 40.47 | 300.40 | 39.90 | 37.80 | 38.20 | 45.70 | 44.55 | 51.60 | 59.50 | 58.70 | ||||
| T2-T1 | 34 | 8.33 | 3.09 | 3.00 | 8.30 | 16.60 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −1.96 | 1.59 | −6.20 | −1.95 | 0.50 | <0.001 | ||||||||||||
| T3-T1 | 34 | 6.38 | 2.99 | 2.00 | 6.65 | 14.70 | <0.001 | ||||||||||||
| UPMapexR-UPMapexL | 34.72 | 40.77 | 39.40 | 3.99 | 4.30 | 40.52 | 270.60 | 31.70 | 31.70 | 33.65 | 41.55 | 39.30 | 40.60 | 49.40 | 47.60 | ||||
| T2-T1 | 34 | 6.05 | 2.56 | 0.30 | 6.50 | 10.90 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −1.37 | 1.24 | −4.40 | −1.30 | 0.40 | <0.001 | ||||||||||||
| T3-T1 | 34 | 4.68 | 2.78 | −0.70 | 4.20 | 8.90 | 0.003 | ||||||||||||
| UCcuspR-UCcuspL | 32.47 | 41.21 | 38.07 | 2.86 | 3.81 | 40.01 | 270.80 | 34.50 | 30.90 | 33.15 | 40.80 | 38.20 | 37.60 | 52.80 | 50.30 | ||||
| T2-T1 | 34 | 8.74 | 2.62 | 4.70 | 8.40 | 17.00 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −3.14 | 1.69 | −6.10 | −2.85 | −0.40 | <0.001 | ||||||||||||
| T3-T1 | 34 | 5.60 | 2.76 | 0.20 | 5.95 | 14.50 | <0.001 | ||||||||||||
| UCapexR-UCapexL | 26.29 | 33.28 | 32.47 | 3.36 | 3.23 | 30.94 | 190.50 | 26.60 | 23.50 | 26.20 | 33.85 | 33.80 | 31.30 | 42.00 | 41.30 | ||||
| T2-T1 | 34 | 6.99 | 1.84 | 3.90 | 7.50 | 10.70 | <0.001 | <0.001 | |||||||||||
| T3-T2 | 34 | −0.81 | 1.64 | −3.90 | −0.85 | 2.60 | <0.001 | ||||||||||||
| T3-T1 | 34 | 6.18 | 2.71 | 0.70 | 6.00 | 11.30 | 0.130 | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Żyła, T.; Kawala, B.; Nowak, R.; Kawala, M.; Halupczok-Żyła, J. Three-Dimensional Cephalometric Analysis of Skeletal and Dental Effects in Patients Undergoing Transpalatal Distraction. Appl. Sci. 2022, 12, 4273. https://doi.org/10.3390/app12094273
Żyła T, Kawala B, Nowak R, Kawala M, Halupczok-Żyła J. Three-Dimensional Cephalometric Analysis of Skeletal and Dental Effects in Patients Undergoing Transpalatal Distraction. Applied Sciences. 2022; 12(9):4273. https://doi.org/10.3390/app12094273
Chicago/Turabian StyleŻyła, Tomasz, Beata Kawala, Rafał Nowak, Maciej Kawala, and Jowita Halupczok-Żyła. 2022. "Three-Dimensional Cephalometric Analysis of Skeletal and Dental Effects in Patients Undergoing Transpalatal Distraction" Applied Sciences 12, no. 9: 4273. https://doi.org/10.3390/app12094273
APA StyleŻyła, T., Kawala, B., Nowak, R., Kawala, M., & Halupczok-Żyła, J. (2022). Three-Dimensional Cephalometric Analysis of Skeletal and Dental Effects in Patients Undergoing Transpalatal Distraction. Applied Sciences, 12(9), 4273. https://doi.org/10.3390/app12094273






