Abstract
This was an in vitro study that aimed to evaluate the antimicrobial effect of the propolis extract caffeic acid phenethyl ester (CAPE) on four different oral microorganisms. Seven different concentrations of CAPE (0.2, 0.5, 1, 1.5, 2, 3, and 4 mg/mL) for use against Staphylococcus aureus, Streptococcus mutans, Streptococcus oralis, and Streptococcus salivarius were determined using minimum inhibition concentration (MIC), minimum bactericidal concentration (MBC), broth microdilution, and well diffusion tests over 1, 3, 6, 12, and 24 h, while NaF at 0.05 percent was used as a positive control. Staphylococcus aureus was most affected by CAPE’s inhibitory effect on bacterial growth, whereas S. mutans was the least affected. S. mutans and S. oralis had similar CAPE MIC and MBC values of 1 mg/mL and 1.5 mg/mL, respectively. The most resistant bacteria to CAPE were S. salivarius and S. aureus, with MIC and MBC values of 3 mg/mL and 4 mg/mL, respectively. S. oralis, followed by S. salivarius, S. mutans, and S. aureus, had the highest viable count following exposure to CAPE’s MBC values, while S. aureus had the lowest. The current results of the inhibitory effect of CAPE on bacterial growth are promising, and the values of both CAPE MBC and MIC against the related four cariogenic bacterial organisms are significant. CAPE can be employed as an adjunct dental hygiene substance for maintaining good oral hygiene, and has a potential therapeutic effect in the field of oral health care.
1. Introduction
Approximately 80% of the world’s population have untreated dental caries, and almost all age groups are affected [1]. Although improvements have been made in raising dental public health awareness, dental caries is to date a serious disease, particularly in developing countries. The prevalence of dental caries in children is high, as seen in South Africa (49%), India (53%), and China (85%), as opposed to the prevalence of dental caries in developed countries such as Italy (16%) and England (32%) [2,3,4,5,6].
Dental caries is a microbial infection that initially manifests through a structural and functional organized biofilm called dental plaque. The development of dental caries is primarily dependent on bacteria, fermentable sugars, host factors, and other environmental conditions [7]. Evidence has identified Streptococcus mutans as the predominant cariogenic. Other factors that contribute to the development of caries are poor oral hygiene, decreased salivary flow and composition, and insufficient exposure to fluoride [7,8].
Due to public concern about the side effects of synthetic medications, organic products have recently gained popularity and attention [8,9]. Organic therapy is undergoing extensive research and has proven to be effective in treating and preventing a variety of illnesses and medical disorders [10,11,12]. Propolis, often known as bee glue, has traditionally been applied in a wide variety of cultural herbal remedies. It has been used to cure a variety of ailments, including cold sores, burns, diabetes, and skin conditions. It has been proven that propolis extract improves oral health and reduces dental cavities, gingivitis, and periodontitis [12]. One of the medicinal propolis extracts, caffeic acid phenethyl ester (CAPE), is a combination of bee-released and plant-derived substances. Generally, pure propolis is made up of approximately 50% resins, 30% paraffin, 10% essential oils, 5% pollen, and 5% other natural substances. Some of the chemicals contained in propolis are amino acids; terpenes; flavonoids including flavones, flavonols and flavanones; vanillin; isalpinin pinocembrin chrysin galangin; tectochrysin; caffeic acid; ferulic acid; caffeic acid phenethyl ester; cinnamic acid, and cinnamyl alcohol [12].
Caffeic acid has been significantly utilized as an alternative remedy to battle microbial pathogenesis and chronic infections caused by microbes such as bacteria, viruses, and fungi [13,14].
Most published experiments concentrate on CAPE’s antimicrobial efficacy against a particular bacteria species or on a certain type of analysis. There has been no comprehensive research on the antibacterial impact of CAPE on a variety of dental bacteria. Therefore, the goal of this study was to assess the antibacterial effect of CAPE (concentration and time of exposure) against different oral microbes.
2. Materials and Methods
2.1. CAPE Preparation
The methodology used for this study was similar to previously published investigations on the antibacterial effect of thymoquinone against different oral microorganisms [15]. CAPE was obtained as a dry powder extract (100% purity from Biosynth Carbosynth Ltd., Compton, UK) where 500 mg of CAPE powder was dissolved in 1 mL of methanol. Seven different concentrations of the tested compounds were prepared by diluting the methanol-dissolved CAPE powder in 1 mL of sterile brain heart infusion broth (BHIB) (0.2, 0.5, 1, 1.5, 2, 3 and 4 mg/mL). Two control groups were used, one positive control (1 mL Listerine containing 0.05% NaF, Johnson & Johnson Middle East, Dubai, UAE) and one negative control (1 mL broth of BHIB containing methanol with no added CAPE).
2.2. Microorganism
Bacterial strains were grown on Mueller–Hinton agar containing 5% Sheep Blood at 37 °C for 48 h with 5% CO2 (HiMedia Laboratories Pvt. Ltd., Maharashtra, India) [16]. S. salivarius (ATCC 13419), S. oralis (ATCC 6249), S. mutans (ATCC 25175), and S. aureus (ATCC 25923) were the four Gram-positive strains received from Microbiologics, St. Cloud, MN, USA. Colonies of the tested bacteria were taken from the fresh culture and then soaked in 2 mL distilled sterile water, before being diluted serially five times from 1:10 to 1:10.5.
2.3. CAPE Antibacterial Effectiveness against Tested Organisms
By combining the methanol-dissolved CAPE powder with 1 mL of sterile BHIB and 0.1 mL of tested organisms, seven different concentrations of CAPE (0.2, 0.5, 1, 1.5, 2, 3 and 4 mg/mL) were created and then stored under dry conditions at 4 °C.
As a negative control, 0.9 mL sterile BHIB was mixed with methanol and 0.1 mL of tested organisms, and, as a positive control, 0.9 mL NaF. Following this, they were mixed with 0.1 mL of tested organisms. Later, for each of the CAPE concentrations, 250 µL was cultured on Mueller–Hinton agar containing 5% Sheep Blood and incubated at 37 °C for 48 h, using a microaerophilic (10% CO2) candle jar technique for S. Salivarius, S. oralis, S. mutans and, in aerophilic circumstances, for S. aureus. The CAPE concentrations and each of the control solutions were tested in triplicate in this investigation.
2.4. Minimum Inhibitory Concentration (MIC) Test
The number of colonies growing in units per millimeter for each concentration was assessed after 24 h of incubation in order to establish the minimal inhibitory concentration (MIC). The MIC is the lowest concentration of CAPE that prevents bacteria from growing. The CAPE MIC for all of the microorganisms studied was calculated using a broth microdilution technique [17], as recommended by the Institute of Laboratory and Clinical Standards.
2.5. Minimum Bactericidal Concentration (MBC) Test
An amount of 250 µL was taken from all test tubes used for the MIC that showed no growth, then inoculated onto 5% Sheep Blood plates with new Mueller–Hinton agar and cultured for 48 h under the appropriate conditions for the tested microorganism. The minimum bactericidal concentration (MBC) was calculated by watching the bacterial growth. MBC was defined as the concentration of antimicrobial agents that eradicate more than 99.9% of bacteria after 24 h.
The following calculation was used to compute the percentage reduction in bacterial count for each concentration:
The colonies were counted after 48 h of incubation.
2.6. MBC Values for Bacterial Count throughout Various Periods
In sterile Eppendorf tubes containing 1 mL of BHIB, the MBC value for CAPE was inculcated with each bacterial inoculum (~10−5 CFU/mL). In addition, 1 mL of positive control was added to the examined organisms (NaF). At 37 °C, the tested and controlled groups were incubated for 24 h. Then, after 1, 3, 6, 12, and 24 h of inoculum, 0.1 mL of each group was tested using serial dilutions in sterile saline solution (0.9%). Then, 250 ul of each of these dilutions was added to Mueller–Hinton agar containing 5% Sheep Blood in duplicate, and then incubated following the recommended conditions for each of the tested bacterial strains requirements, as reported before.
2.7. Well Diffusion Test
Blood Muller-Hinton agar (BMHA) was used for the well diffusion method [18]. Where the plates were inoculated for a specific volume of all isolates tested, a sterile cotton swab was utilized across the whole BMHA plate surface. A 6 mm diameter hole was punched in the agar gel, then each well was filled with 100 mL of one of the four CAPE concentrations (12.5, 25, 50, 75, and 100 mg/mL). In this work, for the positive control the NaF was selected and for the negative control the BMHA was mixed with methanol. All tested groups were incubated following the appropriate settings for the examined microorganism. Each antimicrobial agent was tested in duplicate in each experiment. Following the incubation, the bacterial growth inhibition (the clear zone diameter endpoint) was determined in millimeters.
2.8. Statistical Analysis
The collected CFU data were assembled for the different tested time periods and processed with Log10 transformation. Then, a comparison between the tested material (caffeic acid phenethyl ester) and the control material (sodium fluoride) was conducted for each microorganism strain with an independent t-test. The IBM SPSS® Statistic software (Version 25) was used for statistical analysis. Dot plots were used to show CFU results with individual measurements and means ± standard error. Tables were used to show the microbial inhibition zone results and the minimum inhibitory and bactericidal concentrations.
3. Results
Table 1 demonstrates the antibacterial potency of CAPE at various doses, in comparison to NaF mouthwash (positive control). The findings revealed that CAPE’s antibacterial action was concentration-dependent, albeit only at low concentrations. S. aureus had the greatest impact in preventing bacterial growth, followed by S. salivarius and S. oralis, and S. mutans had the least effect.

Table 1.
Microbial inhibition zone in millimeters produced by the addition of CAPE at different concentrations compared to the NaF (positive control).
To ensure consistency, the four bacterial strains colonies were counted. Following this, the identical CAPE dosages were applied, and cell-culture counts were used to calculate the MBC and MIC. With findings of 1 mg/mL and 1.5 mg/mL, respectively, the minimum concentration of CAPE required for the inhibition (MIC) or killing (MBC) of S. mutans and S. oralis was the most sensitive to CAPE. On the other hand, both S. salivarius and S. aureus, were more resistant to CAPE, with MBC and MIC values of 4 mg/mL and 3 mg/mL, respectively. The NaF control exhibited slightly different antibacterial activity when compared to CAPE for the four cariogenic bacteria. The MIC for NaF was lower in the bacterial strains S. salivarius, S. aureus, and S. oralis, while it was higher for S. mutans as compared to results of the MIC for CAPE. On the other hand, The MBC for NaF was lower in S. aureus, higher in S. oralis and S. mutans, and similar in S. salivarius as compared to results of the MBC for CAPE (Table 2).

Table 2.
Bactericidal concentration and minimum inhibitory (mg/mL) of positive control NaF and CAPE against the four bacterial strains.
As seen in Figure 1, the viable count of the tested microorganisms after exposure to the MBC values of CAPE was the highest detected with S. oralis, followed by S. salivarius, and S. mutans while the least detected was with S. aureus. The viable count of bacterial strains after exposure to the MBC concentrate of the CAPE was most effective after 12 h, where no bacterial growth was detected for all bacterial strains except for S. aureus. However, the results showed no bacterial growth for all different strains after 24 h. No difference was detected between the MBC values of CAPE and NaF among different strains after 24 h.
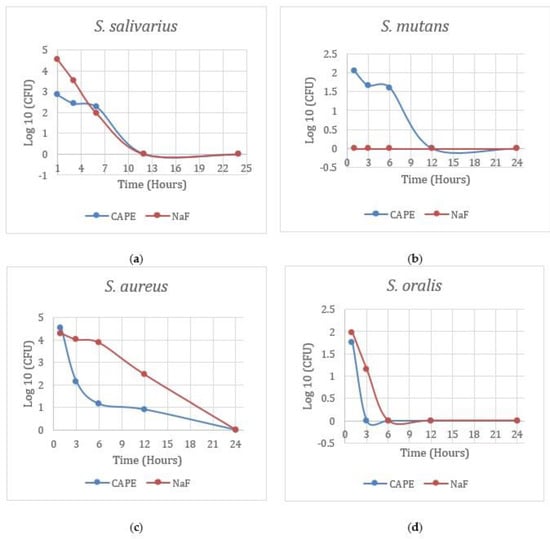
Figure 1.
Viable bacterial count using Log10 transformation CAPE (caffeic acid) vs. NaF (sodium fluoride).
The colony-forming units reflect the microorganisms’ growth after exposure to the MIC concentrate; the CAPE was less potent against S. salivarius, S oralis, and S. aureus compared to the control NaF. According to the Log10 transformation, only S. mutans was significantly different from the control NaF (p = 0.04).
4. Discussion
One of the most common worldwide dental problems is dental caries. Dental caries starts with dental plaque formation that leads to cariogenic bacteria colonization. In previous years, numerous studies have been carried out to try and control dental caries by inhibiting bacterial growth, as well as bacterial colonization. Many clinical studies have proven the direct and indirect relationship between cariogenic bacteria and systemic diseases such as peritonitis, atherosclerosis, ulcerative colitis, and infective endocarditis [19,20]. Recently, a variety of organic natural materials have been tested in vitro to prevent cariogenic bacterial growth [9]. Furthermore, organic materials have been employed as remedies for thousands of years due to their ease of accessibility, extraction, and use [21].
Propolis is a natural material synthesized by bees to disinfect the hive. The antimicrobial effect of propolis has been investigated extensively in the medical field. Many cultures have used propolis extract (caffeic acid phenethyl ester) for many years due to its significant effects in different areas of medicine [22]. A review of the literature has shown many studies proving the antibiotic potency of CAPE against various bacteria. It has been proposed that CAPE can modify the dental pellicle favorably to prevent or even reverse the process of caries by eliminating the cariogenic bacteria. Propolis and its extract (CAPE) have many benefits in managing multiple pathogens such as bacterial, fungal and viral infections, cancer, and inflammatory diseases [23].
The results of this study displayed a promising effect of propolis in terms of antibacterial activity against four different types of bacteria. The minimal bactericidal concentration (MBC) and minimal inhibitory concentration (MIC) are the gold standards for evaluating an agent’s antimicrobial efficacy against bacteria and are thus used to appraise alternative antimicrobial evaluation procedures [24].
Interestingly, CAPE showed promising effects in preventing the growth and flourishing of oral bacteria. The null hypothesis was disproved since CAPE was most effective against S. oralis, S. mutans had a MIC of 1 mg/mL and MBC of 1.5 mg/mL, and S. salivarius and S. aureus had a MIC of 3 mg/mL and MBC of 4 mg/mL. When employing the control NaF, all tested microorganisms showed a slightly similar resistance pattern, with S. mutans and S. oralis exhibiting the least resistance and S. aureus and S. salivarius exhibiting the greatest.
The differing reports on the chemical nature and antimicrobial ability of the propolis extract, specifically CAPE, and the significant antimicrobial activity presented in the current results, incited systematic chemical characterization and antibacterial testing to categorize the antimicrobial components present, and to further investigate their properties for possible use as therapeutic antimicrobials [25,26]. In fact, one of the microorganisms that causes tooth caries is S. mutans. In an earlier investigation, while the role of S. Salivarius is more apparent in active carious lesions, it aids in the progression of caries in the teeth [27].
This study’s findings are consistent with prior studies that have found CAPE to be bactericidal as well as growth-inhibiting for all cariogenic bacteria [28,29]. Furthermore, S. oralis was found to be the dominant microorganism in the active carious lesion. It is thought to play a role in the progression and long-term viability of the caries’ progression [25,28]. The findings are in line with a study that found S. salivarius, S. aureus, and S. mutans to be sensitive to CAPE, with substantial MIC and MBC values [26,28].
Previous studies have proven that CAPE is safe even in relatively large doses. Additionally, evidence has shown that CAPE is concentration dependent. For instance, at a CAPE dosage of 100 mg/mL, S. aureus displayed the most inhibition, followed by S. salivarius, S. oralis then S. mutans. [29,30].
When different CAPE concentrations were tested, a dose-dependent effect was verified. In prior investigation, CAPE showed a dose-dependent bactericidal action against S. mutans, which matches our findings. One of the most prevalent infections presented in clinical settings is S. aureus [31].
Although S. aureus has demonstrated resistance to conventional antimicrobial therapy, increasing the amount of CAPE has been proven to reduce bacterial growth and count; CAPE could be the key to addressing this microorganism’s high resistance.
A well diffusion test was performed to confirm the study findings versus standard laboratory testing. For S. aureus, S. oralis, and S. salivarius, the CAPE inhibitory effect was time-dependent, not just concentration-dependent. When it came to preventing the growth of microbes, CAPE outperformed the NaF control when used against S. salivarius, S. oralis and S. aureus. On the other hand, S. mutans was inhibited by using NaF at the first hour. When utilizing NaF, S. aureus was still present after 12 h, S. salivarius diminished after 6 h, S. oralis was eradicated after 3 h and showed no growth at all from the beginning. The viable count of different strains after exposure to the MBC values of CAPE was highest detectable. The viable count of bacterial strains after exposure to the MBC concentrate of CAPE was most effective after 1 h, where no bacterial growth was observed for S. oralis; after 6 h for S. salivarius and S. mutans; and after 12 h for S. aureus.
While NaF may have the same benefits as CAPE, this research implies that using CAPE infrequently can help prevent caries. Higher doses may be advantageous in preventing caries initiation. It has proved to have a prospective advantage similar to NaF in terms of effectiveness against cariogenic bacteria in regular-basis dental hygiene.
Other research has concentrated on MIC or MBC, the bacterial inhibition zone, or only one or two bacterial strains. The merit of this investigation is that it investigated a wider range of cariogenic bacteria, which play a major role in the initiation, maintenance, and progression of the caries’ progress. Concurrently addressing the inhibitory zone, MBC, and MIC are feasible tests in determining the antimicrobial activity of experimental drugs [32].
Numerous active compounds have been analyzed and found to be useful in controlling dental pellicle/plaque and lowering the number of cariogenic bacteria. Filogônio et al. supplemented a commercial products dentifrice with a natural South American nut extract. He claimed that the evaluated products were adequate in considerably improving dental biofilm control after 90 days [33]. Lobo et al. examined the effects of Lippia sidoides Cham essential oil and chlorhexidine in decreasing salivary S. mutans in children suffering from caries lesions. On the other hand, chlorhexidine decreased S. mutans after use of the mouth rinse, but the S. mutans numbers quickly reverted to baseline levels. The S. mutans number was lowered while using the Lippia sidoides Cham essential oil and remained low even after therapy [34].
Marya C M et al. compared the effect of CAPE added to chlorhexidine and fluoride mouth rinses in reducing dental plaque accumulation and gingivitis. In vitro, all three mouth rinses showed antimicrobial efficacy towards S. mutans and other microorganisms [35].
CAPE antibacterial action was tested against four microorganisms that are important for the initiation and maintenance of caries lesions in this study. On the other hand, dental caries begin with dental plaque, which forms a biofilm in the mouth. Additional clinical trials are needed to assess the impact against other biofilm bacteria, and to investigate the effect of CAPE on plaque pH after acidogenic challenge, plaque and gingival indices, and gingival inflammation. Thus, a corresponding study is required on patients with a variety of oral conditions. This study could disclose clinically relevant therapeutic effects as well as an in vitro assessment of CAPE’s antibacterial properties. More research with varied CAPE doses and intervals, as well as other natural products that could alter or amplify its impact, could be very useful in determining CAPE therapeutic and preventive significance.
5. Conclusions
These findings suggest that propolis extract (CAPE) might positively contribute to the prevention of and reduction in dental caries. The current results obtained for CAPE’S inhibitory effects on bacterial growth are promising, and the values of both CAPE MBC and MIC against the related four cariogenic bacteria are significant. Therefore, current evidence highlights that CAPE can be employed as a dental hygiene substance for achieving and maintaining good oral hygiene, and it has a potential therapeutic effect in the field of oral health care; however, additional oral hygiene cleaning aids are needed in combination with CAPE application.
6. Further Perspectives
Further studies are necessary to explore and identify the effects of CAPE on dental bacteria. The fast and strong antimicrobial effect against the aforementioned bacteria types that have been identified as the most predominant cariogenic microbiota supports the need to investigate the potential of CAPE as an antimicrobial element for therapeutic use. The reported antibacterial character of CAPE might be beneficial when used in confined body spaces requiring antibacterial treatment. Studying a population with a high prevalence of caries and other infectious oral health conditions would be necessary to test the effectiveness of CAPE in the prevention and treatment of oral health diseases.
7. Recommendations
Based on the results of this study, clinical and laboratory investigations of antimicrobial activities, together with the effect on caries and gingival inflammation, need to be further investigated. The possible antiviral and antifungal effects of propolis extract, commonly known as CAPE, should also be investigated. However, the cytotoxic activities of CAPE need to be assessed before the development of oral applications becomes a reality.
Author Contributions
Conceptualization, K.S.A.-K. and R.A.; methodology, K.S.A.-K. and R.A.; software, K.S.A.-K. and A.M.A.; validation, K.S.A.-K. and R.A.; formal analysis, H.N.A., H.Z.; investigation, K.S.A.-K., R.A., H.N.A. and I.A.; resources, K.S.A.-K. and R.A.; data curation, K.S.A.-K. and R.A.; writing—original H.N.A., R.A. and H.Z. draft preparation, K.S.A.-K. and R.A.; writing—review and editing, K.S.A.-K., H.S.H. and R.A.; visualization, K.S.A.-K. and R.A.; supervision, K.S.A.-K.; project administration, K.S.A.-K. and R.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Hossam El-Sayyed for the microbiology tests involved in this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moynihan, P. Sugars and Dental Caries: Evidence for Setting a Recommended Threshold for Intake. Adv. Nutr. 2016, 7, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Liu, J.; Lo, E.C.; Chu, C.H. Dental caries status of Bulang preschool children in Southwest China. BMC Oral Health 2014, 14, 16. [Google Scholar] [CrossRef] [PubMed]
- Prakasha Shrutha, S.; Vinit, G.B.; Giri, K.Y.; Alam, S. Feeding practices and early childhood caries: A cross-sectional study of preschool children in kanpur district, India. ISRN Dent 2013, 2013, 275193. [Google Scholar] [CrossRef] [PubMed]
- Thekiso, M.; Yengopal, V.; Rudolph, M.J.; Bhayat, A. Caries status among children in the West Rand District of Gauteng Province, South Africa. SADJ 2012, 67, 318–320. [Google Scholar]
- Pitts, N.B.; Boyles, J.; Nugent, Z.J.; Thomas, N.; Pine, C.M. The dental caries experience of 5-year-old children in Great Britain (2005/6). Surveys co-ordinated by the British Association for the study of community dentistry. Community Dent Health 2007, 24, 59–63. [Google Scholar]
- Congiu, G.; Campus, G.; Sale, S.; Spano, G.; Cagetti, M.G.; Lugliè, P.F. Early childhood caries and associated determinants: A cross-sectional study on Italian preschool children. J. Public Health Dent 2014, 74, 147–152. [Google Scholar] [CrossRef]
- Conrads, G.; About, I. Pathophysiology of Dental Caries. Monogr. Oral Sci. 2018, 27, 1–10. [Google Scholar] [CrossRef]
- LuIs, H.S.; Luis, L.S.; Bernardo, M. study of the effect of an essential oil and a delmopinol mouth rinse on dental plaque bacteria. Indian J. Dent. Res. 2016, 27, 648–651. [Google Scholar] [CrossRef]
- Iyer, M.; Gujjari, A.K.; Gowda, V.; Angadi, S. Antifungal response of oral-associated candidal reference strains (American Type Culture Collection) by supercritical fluid extract of nutmeg seeds for geriatric denture wearers: An. J. Indian Prosthodont. Soc. 2017, 17, 267–272. [Google Scholar] [CrossRef]
- Fong, H.H. Integration of herbal medicine into modern medical practices: Issues and prospects. Integr. Cancer Ther. 2002, 1, 287–293. [Google Scholar] [CrossRef]
- Dattner, A.M. From medical herbalism to phytotherapy in dermatology: Back to the future. Dermatol. Ther. 2003, 16, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Anjum, S.I.; Ullah, A.; Khan, K.A.; Attaullah, M.; Khan, H.; Ali, H.; Bashir, M.A.; Tahir, M.; Ansari, M.J.; Ghramh, H.A.; et al. Composition and functional properties of propolis (bee glue): A review. Saudi J. Biol. Sci. 2019, 26, 1695–1703. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Bamunuarachchi, N.I.; Tabassum, N.; Kim, Y.M. Caffeic Acid and Its Derivatives: Antimicrobial Drugs toward Microbial Pathogens. J. Agric. Food Chem. 2021, 69, 2979–3004. [Google Scholar] [CrossRef] [PubMed]
- Muhammad Abdul Kadar, N.N.; Ahmad, F.; Teoh, S.L.; Yahaya, M.F. Caffeic Acid on Metabolic Syndrome: A Review. Molecules 2021, 26, 5490. [Google Scholar] [CrossRef]
- Al-Khalifa, K.S.; AlSheikh, R.; Al-Hariri, M.T.; El-Sayyad, H.; Alqurashi, M.S.; Ali, S.; Bugshan, A.S. Evaluation of the Antimicrobial Effect of Thymoquinone against Different Dental Pathogens: An In Vitro Study. Molecules 2021, 26, 6451. [Google Scholar] [CrossRef]
- Niederstebruch, N.; Sixt, D.; Benda, B.I.; Banboye, N. A suitable blood agar containing human blood especially for the use in laboratories of developing countries. J. Infect. Dev. Ctries. 2017, 11, 399–406. [Google Scholar] [CrossRef]
- CLSI Document M07-A9; Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically. Approved Standard—Ninth Edition; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2012.
- Silva, F.R.G.; Matias, T.M.S.; Souza, L.I.O.; Matos-Rocha, T.J.; Fonseca, S.A.; Mousinho, K.C.; Santos, A.F. Phytochemical screening and in vitro antibacterial, antifungal, antioxidant and antitumor activities of the red propolis Alagoas. Braz. J. Biol. 2019, 79, 452–459. [Google Scholar] [CrossRef]
- Shakoor, S.; Fasih, N.; Jabeen, K.; Jamil, B. Rothia dentocariosa endocarditis with mitral valve prolapse: Case report and brief review. Infection 2011, 39, 177–179. [Google Scholar] [CrossRef]
- Kojima, A.; Nomura, R.; Naka, S.; Okawa, R.; Ooshima, T.; Nakano, K. Aggravation of inflammatory bowel diseases by oral streptococci. Oral Dis. 2014, 20, 359–366. [Google Scholar] [CrossRef]
- Haraszthy, V.I.; Reynolds, H.S.; Sreenivasan, P.K.; Subramanyam, R.; Cummins, D.; Zambon, J.J. Media- and method-dependent variations in minimal inhibitory concentrations of antiplaque agents on oral bacteria. Lett. Appl. Microbiol. 2006, 43, 256–261. [Google Scholar] [CrossRef]
- Galeotti, F.; Maccari, F.; Fachini, A.; Volpi, N. Chemical Composition and Antioxidant Activity of Propolis Prepared in Different Forms and in Different Solvents Useful for Finished Products. Foods 2018, 7, 41. [Google Scholar] [CrossRef] [PubMed]
- Kuropatnicki, A.K.; Szliszka, E.; Krol, W. Historical aspects of propolis research in modern times. Evid Based Complement Altern. Med. 2013, 2013, 964149. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.M. Determination of minimum inhibitory concentrations. J. Antimicrob. Chemother. 2001, 48 (Suppl. 1), 5–16. [Google Scholar] [CrossRef] [PubMed]
- Duailibe, S.A.; Gonçalves, A.G.; Ahid, F.J. Effect of a propolis extract on Streptococcus mutans counts in vivo. J. Appl. Oral. Sci. 2007, 15, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Nazeri, R.; Ghaiour, M.; Abbasi, S. Evaluation of Antibacterial Effect of Propolis and its Application in Mouthwash Production. Front. Dent. 2019, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, G.L.S.; Bezerra, L.M.D.; Ribeiro, I.L.A.; Morais Júnior, R.C.D.; Castro, R.D. Susceptibility of cariogenic microorganisms to phytoconstituents. Braz. J. Biol. 2018, 78, 691–696. [Google Scholar] [CrossRef]
- Awawdeh, L.; Al-Beitawi, M.; Hammad, M. Effectiveness of propolis and calcium hydroxide as a short-term intracanal medicament against Enterococcus faecalis: A laboratory study. Aust. Endod. J. 2009, 35, 52–58. [Google Scholar] [CrossRef]
- Akca, A.E.; Akca, G.; Topçu, F.T.; Macit, E.; Pikdöken, L.; Özgen, I. The Comparative Evaluation of the Antimicrobial Effect of Propolis with Chlorhexidine against Oral Pathogens: An In Vitro Study. Biomed. Res. Int. 2016, 2016, 3627463. [Google Scholar] [CrossRef]
- Choo, S.W.; Mohammed, W.K.; Mutha, N.V.R.; Rostami, N.; Ahmed, H.; Krasnogor, N.; Tan, G.Y.A.; Jakubovics, N.S. Transcriptomic Responses to Coaggregation between Streptococcus gordonii and Streptococcus oralis. Appl. Environ. Microbiol. 2021, 87, e0155821. [Google Scholar] [CrossRef]
- Niu, Y.; Wang, K.; Zheng, S.; Wang, Y.; Ren, Q.; Li, H.; Ding, L.; Li, W.; Zhang, L. Antibacterial Effect of Caffeic Acid Phenethyl Ester on Cariogenic Bacteria and Streptococcus mutans Biofilms. Antimicrob. Agents Chemother. 2020, 64, E00251-20. [Google Scholar] [CrossRef]
- Balouiri, M.; Sadiki, M.; Ibnsouda, S.K. Methods for. J. Pharm. Anal. 2016, 6, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Filogônio, C.e.F.; Soares, R.V.; Horta, M.C.; Penido, C.V.; Cruz, R.e.A. Effect of vegetable oil (Brazil nut oil) and mineral oil (liquid petrolatum) on dental biofilm control. Braz. Oral. Res. 2011, 25, 556–561. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lobo, P.L.; Fonteles, C.S.; Marques, L.A.; Jamacaru, F.V.; Fonseca, S.G.; de Carvalho, C.B.; de Moraes, M.E. The efficacy of three formulations of Lippia sidoides Cham. essential oil in the reduction of salivary Streptococcus mutans in children with caries: A randomized, double-blind, controlled study. Phytomedicine 2014, 21, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Marya, C.M.; Oberoi, S.S.; Nagpal, R.; Dhingra, C. Comparison of Antimicrobial Efficacy of Brazilian Propolis With Chlorhexidine and Sodium Fluoride Against Common Oral Pathogens: An In Vitro Study. Jundishapur J. Nat. Pharm. Prod. 2015, 10, e19069. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).