Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam
Abstract
:1. Introduction
2. Materials and Methods
2.1. Implant Characteristics
- (a)
- Shorts: 6.0 mm;
- (b)
- Longs: 13.0 mm.
2.2. Polyurethane Foam Blocks
2.3. Drilling Protocol
- Insertion Torque value (ITV) in Ncm;
- Resonance frequency analysis (RFA) in implant stability quotient score (ISQ);
- Removal Torque (RT) in Ncm.
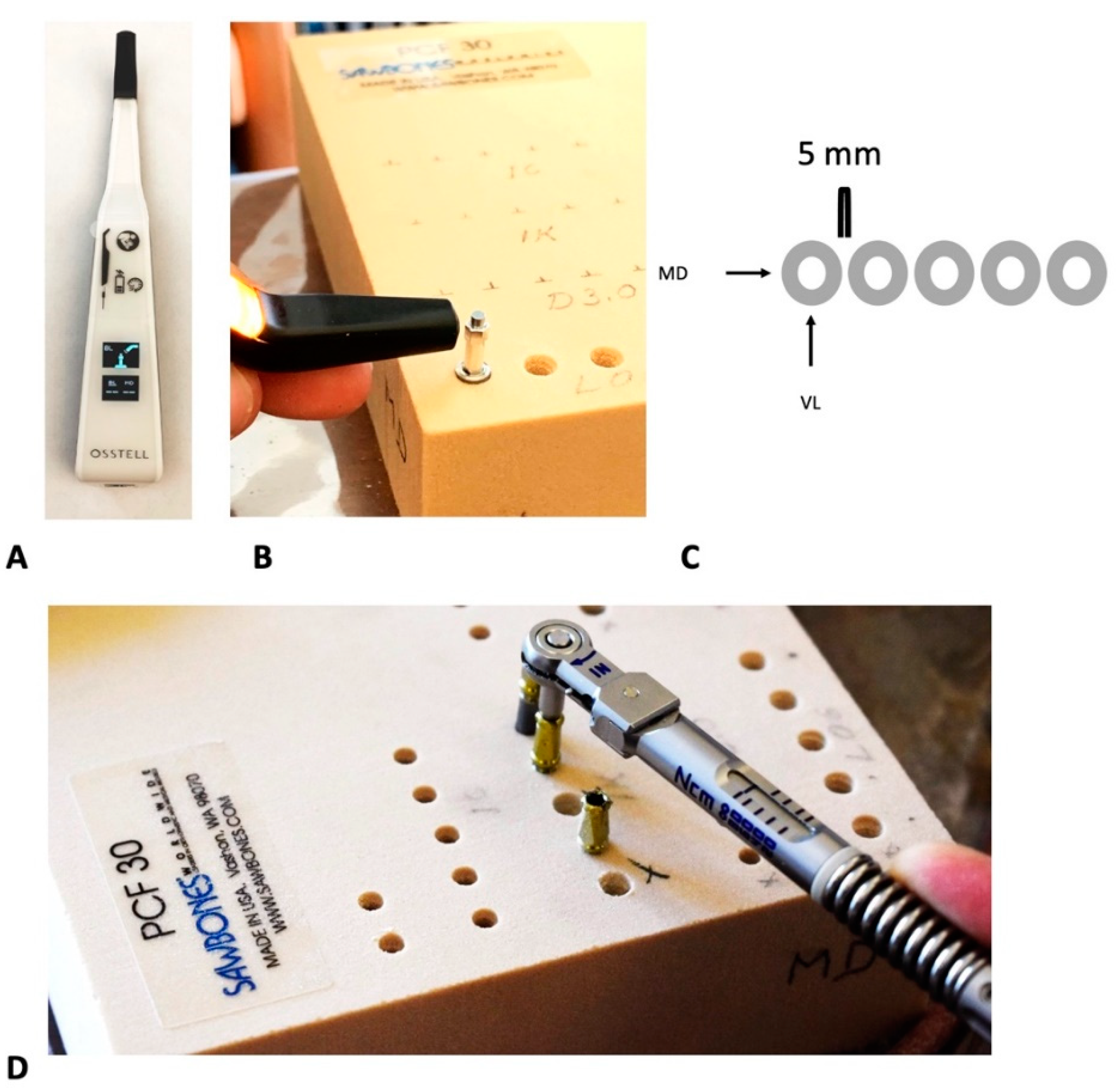
2.4. RFA Stability Measurement
- -
- Mesio-distal (MD);
- -
- Vestibulo-lingual (VL).
2.5. Insertion and Removal Torque Values
2.6. Statistical Analysis
- -
- Long vs. short implants in 20 PCF;
- -
- Long vs. short implants in 30 PCF.
- -
- Long implants in 20 PCF vs. 30 PCF;
- -
- Short implants in 20 PCF vs. 30 PCF.
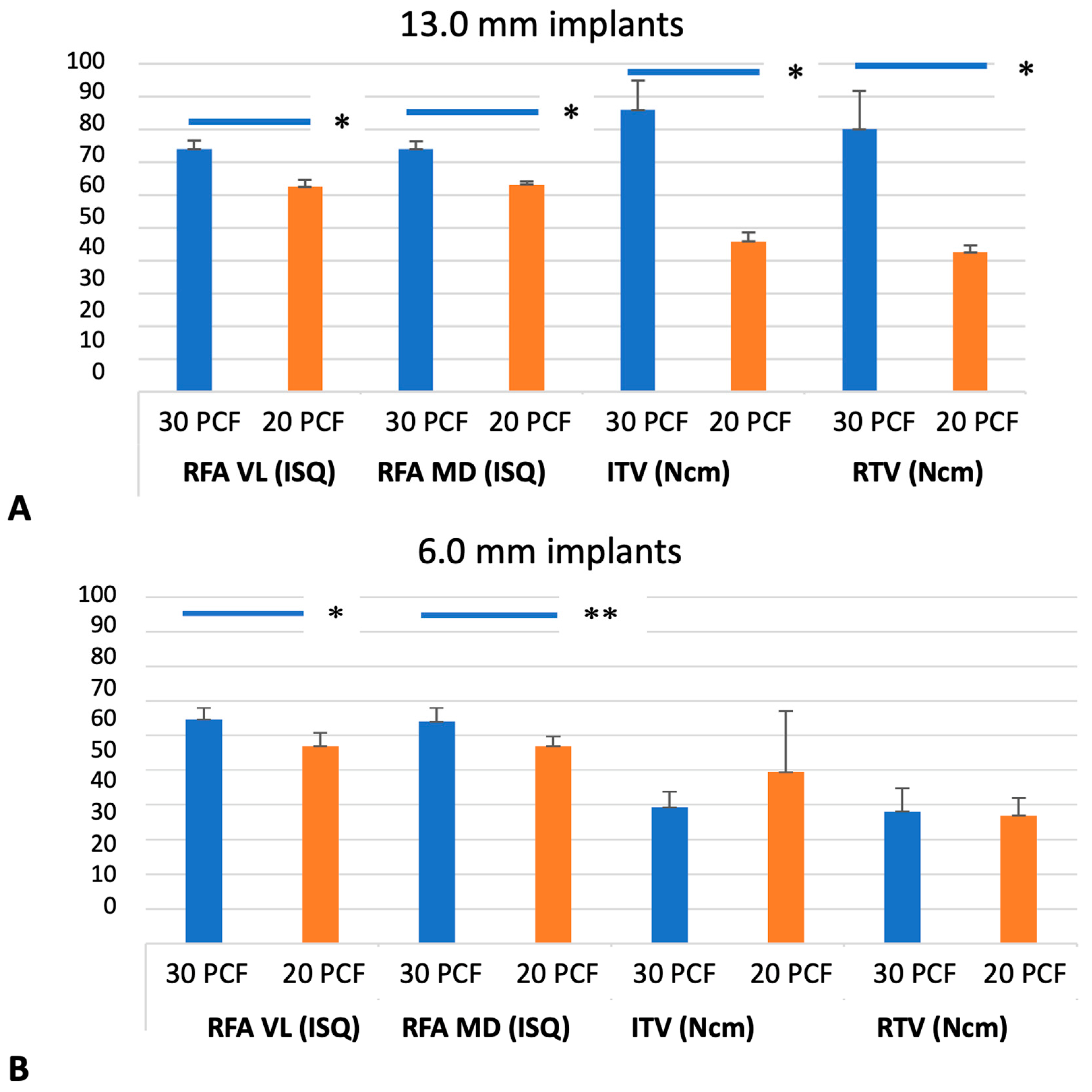
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.-S.; Zhang, Y.-R.; Zhu, Z.-L.; Yu, H.-Y. Micromotions and combined damages at the dental implant/bone interface. Int. J. Oral Sci. 2012, 4, 182–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wazen, R.M.; Currey, J.A.; Guo, H.; Brunski, J.B.; Helms, J.A.; Nanci, A. Micromotion-induced strain fields influence early stages of repair at bone–implant interfaces. Acta Biomater. 2013, 9, 6663–6674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sghaireen, M.G.; Alduraywish, A.A.; Srivastava, K.C.; Shrivastava, D.; Patil, S.R.; Al Habib, S.; Hamza, M.; Ab Rahman, S.; Lynch, E.; Alam, M.K. Comparative Evaluation of Dental Implant Failure among Healthy and Well-Controlled Diabetic Patients—A 3-Year Retrospective Study. Int. J. Environ. Res. Public Health 2020, 17, 5253. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Coulthard, P.; Worthington, H.V. Different loading strategies of dental implants: A Cochrane systematic review of randomised controlled clinical trials. Eur. J. Oral Implantol. 2008, 1, 259–276. [Google Scholar]
- Ledermann, P.D.; Schenk, R.K.; Buser, D. Long-Lasting Osseointegration of Immediately Loaded, Bar-Connected TPS Screws after 12 Years of Function: A Histologic Case Report of a 95-Year-Old Patient. Int. J. Periodontics Restor. Dent. 1998, 18, 552–563. [Google Scholar]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef]
- Aldahlawi, S.; Demeter, A.; Irinakis, T. The effect of implant placement torque on crestal bone remodeling after 1 year of loading. Clin. Cosmet. Investig. Dent. 2018, 10, 203–209. [Google Scholar] [CrossRef] [Green Version]
- Sierra-Rebolledo, A.; Allais-Leon, M.; Maurette-O’Brien, P.; Gay-Escoda, C. Primary Apical Stability of Tapered Implants through Reduction of Final Drilling Dimensions in Different Bone Density Models. Implant Dent. 2016, 25, 775–782. [Google Scholar] [CrossRef]
- Swami, V.; Vijayaraghavan, V. Current trends to measure implant stability. J. Indian Prosthodont. Soc. 2016, 16, 124–130. [Google Scholar] [CrossRef]
- Cobo-Vázquez, C.; Reininger, D.; Molinero-Mourelle, P.; González-Serrano, J.; Guisado-Moya, B.; López-Quiles, J. Effect of the lack of primary stability in the survival of dental implants. J. Clin. Exp. Dent. 2017, 10, e14–e19. [Google Scholar] [CrossRef] [PubMed]
- Bayarchimeg, D.; Namgoong, H.; Kim, B.K.; Kim, M.D.; Kim, S.; Kim, T.-I.; Seol, Y.J.; Lee, Y.M.; Ku, Y.; Rhyu, I.-C.; et al. Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J. Periodontal Implant Sci. 2013, 43, 30–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamatsu, Y.; Kaimoto, K.; Arai, M.; Ide, Y. Properties of the elastic modulus from buccal compact bone of human mandible. Bull. Tokyo Dent. Coll. 1996, 37, 93–101. [Google Scholar] [PubMed]
- Misch, C.E.; Qu, Z.; Bidez, M.W. Mechanical properties of trabecular bone in the human mandible: Implications for dental implant treatment planning and surgical placement. J. Oral Maxillofac. Surg. 1999, 57, 700–706. [Google Scholar] [CrossRef]
- Miyashiro, M.; Suedam, V.; Moretti Neto, R.; Ferreira, P.M.; Rubo, J.H. Validation of an experimental polyurethane model for biomechanical studies on implant supported prosthesis—Tension tests. J. Appl. Oral Sci. 2011, 19, 244–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An In vitro evaluation, on polyurethane foam sheets, of the insertion torque (IT) values, pull-out torque values, and resonance frequency analysis (RFA) of NanoShort dental implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanali, S.; Tumedei, M.; Pignatelli, P.; Inchingolo, F.; Pennacchietti, P.; Pace, G.; Piattelli, A. Implant primary stability with an osteocon-densation drilling protocol in different density polyurethane blocks. Comput. Methods Biomech. Biomed. Eng. 2020, 24, 14–20. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary stability of dental implants in low-density (10 and 20 pcf) polyurethane foam blocks: Conical vs. cylindrical implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [Green Version]
- Davies, J.E. Mechanisms of endosseous integration. Int. J. Prosthodont. 1998, 11, 391–401. [Google Scholar]
- Petrini, M.; Giuliani, A.; Di Campli, E.; Di Lodovico, S.; Iezzi, G.; Piattelli, A.; D’Ercole, S. The Bacterial Anti-Adhesive Activity of Double-Etched Titanium (DAE) as a Dental Implant Surface. Int. J. Mol. Sci. 2020, 21, 8315. [Google Scholar] [CrossRef]
- Del Giudice, R.; Piattelli, A.; Grande, N.M.; Cataneo, E.; Crispino, A.; Petrini, M. Implant insertion torque value in immediate loading: A retrospective study. Med. Oral Patol. Oral Y Cirugía Bucal 2019, 24, e398–e403. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; Cellini, L.; Pilato, S.; Di Lodovico, S.; Iezzi, G.; Piattelli, A.; Petrini, M. Material characterization and Streptococcus oralis adhesion on Polyetheretherketone (PEEK) and titanium surfaces used in implantology. J. Mater. Sci. Mater. Med. 2020, 31, 84. [Google Scholar] [CrossRef] [PubMed]
- Bataineh, A.B.; Al-Dakes, A.M. The influence of length of implant on primary stability: An in vitro study using resonance frequency analysis. J. Clin. Exp. Dent. 2016, 9, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Balaji, V.R.; Lambodharan, R.; Manikandan, D.; Deenadayalan, S. Pterygoid implant for atrophic posterior maxilla. J. Pharm. BioAllied Sci. 2017, 9, S261–S263. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, C.; Manresa, C.; Francisco, K.; Claros, P.; Alández, J.; Gonzalez-Martin, O.; Albrektsson, T. Zygomatic implants: Indications, techniques and outcomes, and the Zygomatic Success Code. Periodontology 2000 2014, 66, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Wang, X.; Qiu, L. Outcomes of 6.5-mm Hydrophilic Implants and Long Implants Placed with Lateral Sinus Floor Elevation in the Atrophic Posterior Maxilla: A Prospective, Randomized Controlled Clinical Comparison. Clin. Implant Dent. Relat. Res. 2016, 19, 111–122. [Google Scholar] [CrossRef]
- Jung, R.E.; Al-Nawas, B.; Araujo, M.; Avila-Ortiz, G.; Barter, S.; Brodala, N.; Chappuis, V.; Chen, B.; De Souza, A.; Faria-Almeida, R.; et al. Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient-reported outcomes. Clin. Oral Implant. Res. 2018, 29, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Tumedei, M.; Petrini, M.; Cipollina, A.; Di Carmine, M.; Piattelli, A.; Cucurullo, A.; Iezzi, G. Comparative Evaluation of Primary Stability between Different Diameters Multi-Scale Roughness Dental Implant by Solid Rigid Polyurethane Simulation. Osteology 2021, 1, 62–72. [Google Scholar] [CrossRef]
- Misch, C.E. Bone classification, training keys to implant success. Dent. Today 1989, 8, 39–44. [Google Scholar]
- Schouten, C.; Meijer, G.J.; Van Den Beucken, J.J.; Leeuwenburgh, S.C.; de Jonge, L.T.; Wolke, J.G.; Spauwen, P.H.; Jansen, J.A. In vivo bone response and mechanical evaluation of electrosprayed CaP nanoparticle coatings using the iliac crest of goats as an implantation model. Acta Biomater. 2010, 6, 2227–2236. [Google Scholar] [CrossRef]
- Hernandez, C.; Beaupre, G.; Keller, T.; Carter, D. The influence of bone volume fraction and ash fraction on bone strength and modulus. Bone 2001, 29, 74–78. [Google Scholar] [CrossRef]
- Keaveny, T.M.; Morgan, E.F.; Niebur, G.L.; Yeh, O.C. Biomechanics of trabecular bone. Annu. Rev. Biomed. Eng. 2001, 3, 307–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ASTM F1839-01; Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments. American Society for Testing and Materials: West Conshohocken, PA, USA, 2001.
- Patel, P.S.D.; Shepherd, D.E.T.; Hukins, D.W.L. Compressive properties of commercially available polyurethane foams as mechanical models for osteoporotic human cancellous bone. BMC Musculoskelet. Disord. 2008, 9, 137. [Google Scholar] [CrossRef] [Green Version]
- Calvert, K.L.; Trumble, K.P.; Webster, T.J.; Kirkpatrick, L.A. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J. Mater. Sci. Mater. Med. 2010, 21, 1453–1461. [Google Scholar] [CrossRef]
- Palissery, V.; Taylor, M.; Browne, M. Fatigue characterization of a polymer foam to use as a cancellous bone analog material in the assessment of orthopaedic devices. J. Mater. Sci. Mater. Med. 2004, 15, 61–67. [Google Scholar] [CrossRef]
- Ersanli, S.; Karabuda, C.; Beck, F.; Leblebicioglu, B. Resonance Frequency Analysis of One-Stage Dental Implant Stability during the Osseointegration Period. J. Periodontol. 2005, 76, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishna, R.; Nayar, S. Clinical assessment of primary stability of endosseous implants placed in the incisor region, using resonance frequency analysis methodology: An in vivo study. Indian J. Dent. Res. 2007, 18, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; De Angelis, F.; Lorusso, F.; Piattelli, A.; Iezzi, G. Influence of the dental implant macrogeometry and threads design on primary stability: An in vitro simulation on artificial bone blocks. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 1242–1250. [Google Scholar] [CrossRef]
- La Scala ISQ—Osstell®—Implant Stability. [Internet]. Available online: https://www.osstell.com/it/clinical-guidelines/the-isq-scale/ (accessed on 14 March 2021).
- Lemos, C.A.; Verri, F.R.; Neto, O.B.D.O.; Cruz, R.S.; Gomes, J.M.L.; Casado, B.G.D.S.; Pellizzer, E.P. Clinical effect of the high insertion torque on dental implants: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 126, 490–496. [Google Scholar] [CrossRef]
- Ottoni, J.M.P.; Oliveira, Z.F.L.; Mansini, R.; Cabral, A.M. Correlation between placement torque and survival of single-tooth implants. Int. J. Oral Maxillofac. Implant. 2005, 20, 769–776. [Google Scholar]
- Calandriello, R.; Tomatis, M.; Rangert, B. Immediate functional loading of Brånemark System® implants with enhanced initial stability: A prospective 1- to 2-year clinical and radiographic study. Clin. Implant Dent. Relat. Res. 2003, 5, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Piattelli, A. Immediate Functional and Non-Functional Loading of Dental Implants: A 2- to 60-Month Follow-Up Study of 646 Titanium Implants. J. Periodontol. 2003, 74, 225–241. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, M.; Pertl, C.; Zhang, K.; Wimmer, G.; Wegscheider, W.A. Immediate loading of single-tooth implants in the anterior maxilla. Preliminary results after one year. Clin. Oral Implant. Res. 2003, 14, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Meredith, N. A Review of Implant Design, Geometry and Placement. Appl. Osseointegration Res. 2008, 6, 6–12. [Google Scholar]
- Duyck, J.; Naert, I.; Ronold, H.J.; Ellingsen, J.E.; Van Oosterwyck, H.; Sloten, J.V. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study. Clin. Oral Implant. Res. 2001, 12, 207–218. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; Tripodi, D.; Ravera, L.; Perrotti, V.; Piattelli, A.; Iezzi, G. Bacterial leakage in Morse Cone internal connection implants using different torque values: An in vitro study. Implant Dent. 2014, 23, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, Y.; Shiota, M.; Munakata, M.; Kasugai, S.; Ozeki, M. Effect of implant design on primary stability using torque-time curves in artificial bone. Int. J. Implant Dent. 2015, 1, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrini, M.; Tumedei, M.; Cipollina, A.; D’Ercole, S.; Carmine, M.S.D.; Piattelli, A.; Re, M.; Iezzi, G. Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam. Appl. Sci. 2022, 12, 2683. https://doi.org/10.3390/app12052683
Petrini M, Tumedei M, Cipollina A, D’Ercole S, Carmine MSD, Piattelli A, Re M, Iezzi G. Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam. Applied Sciences. 2022; 12(5):2683. https://doi.org/10.3390/app12052683
Chicago/Turabian StylePetrini, Morena, Margherita Tumedei, Alessandro Cipollina, Simonetta D’Ercole, Maria Stella Di Carmine, Adriano Piattelli, Marco Re, and Giovanna Iezzi. 2022. "Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam" Applied Sciences 12, no. 5: 2683. https://doi.org/10.3390/app12052683
APA StylePetrini, M., Tumedei, M., Cipollina, A., D’Ercole, S., Carmine, M. S. D., Piattelli, A., Re, M., & Iezzi, G. (2022). Fixture Length and Primary Stability: An In Vitro Study on Polyurethane Foam. Applied Sciences, 12(5), 2683. https://doi.org/10.3390/app12052683










