Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia
Abstract
:1. Introduction
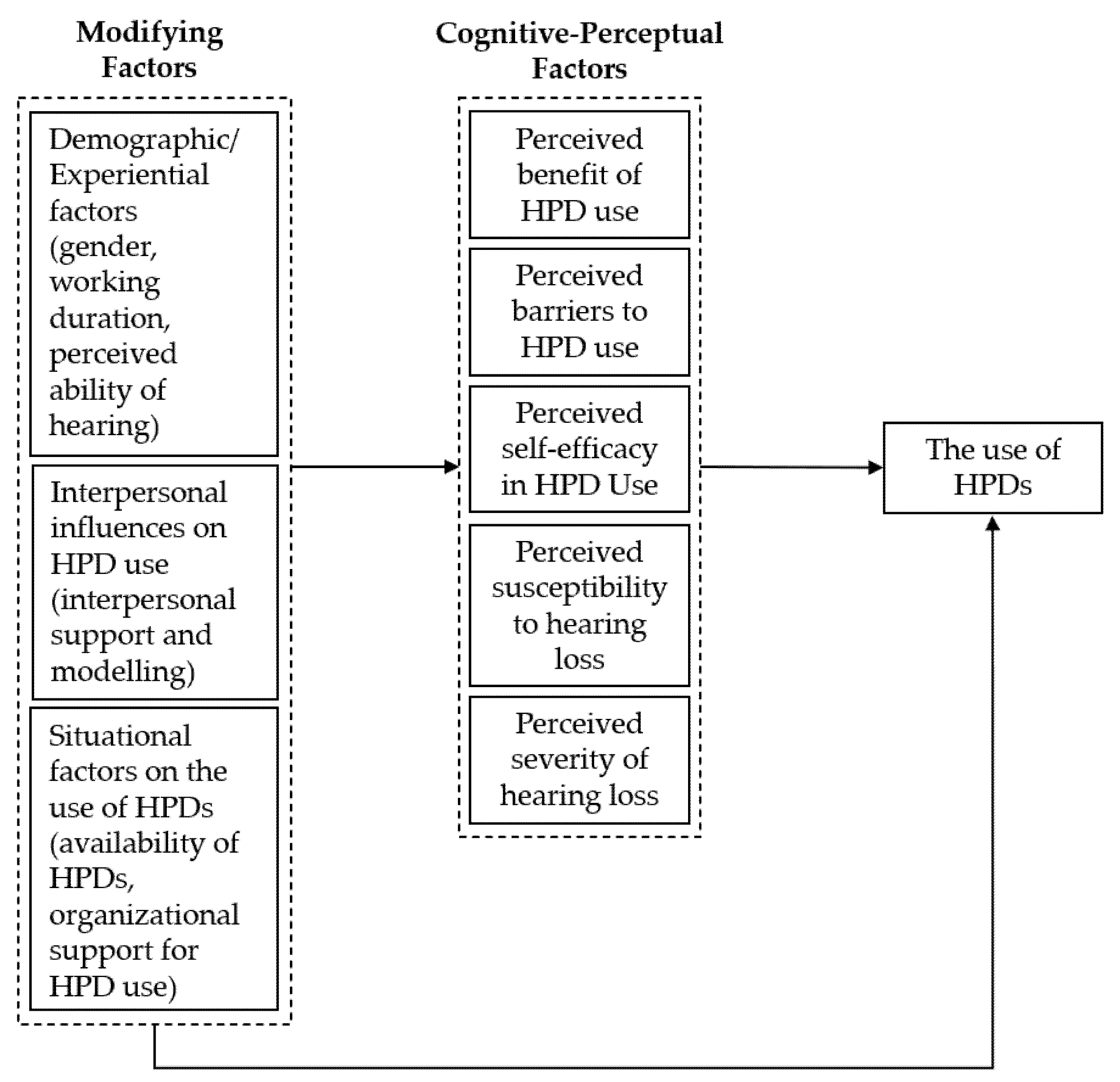
2. Materials and Methods
2.1. Study Design
2.2. Study Subjects
2.3. Research Tools
2.3.1. Sociodemographic and Perceived Hearing Questionnaire
2.3.2. Outcome Measurements: HPD Use and the Intention to Use HPD
2.3.3. Questionnaire on the Predictors of HPD Use
2.3.4. Module A—Intervention Group
- (i)
- Settings and durationThe training session was conducted in a classroom setting, accommodating thirty workers at a time. A presenter delivered the module in the form of presentation slides. The session lasted one hour.
- (ii)
- Language and complexity of contentMost of the participants only received formal education up to secondary school. Hence, the module content was written in plain and straightforward Malay, minimising unnecessary technical terms. The participants were briefed on the following topics: sound and noise, the hearing system, health effects of noise, hearing conservation programme, and noise hazard control. Diagrams and analogies were used to explain relevant concepts. None of the participants were in managerial or administrative positions. Rather, they were all stationed along the mill’s production line and were constantly exposed to excessive noise during working hours. Hence, when explaining noise-hazard control, we focused on the appropriate actions at the personal level (wearing HPD) instead of elaborating on engineering and administrative control measures.
- (iii)
- Emphasis on relevant pointsThe participants’ questionnaire responses provided insight into the factors that affected their use of HPD. The main barriers to compliance were the lack of comfort and difficulties in communicating when wearing the devices. While most of them agreed that they were susceptible to hearing loss due to their working environment, 1 in 6 participants was unaware of the irreversibility of noise-induced hearing loss. Interpersonal and situational influences did not hinder their use of HPD. Based on these responses, we fine-tuned the module content to emphasise the hazardous effects of noise on workers’ health, notably the permanent nature of noise-induced hearing loss, and hence the need to use HPD at all times when working in noisy environments. We also stressed the importance of preserving any remaining hearing capability for those who had already developed hearing loss.
- (iv)
- Noise mapThe mill conducts yearly noise-risk assessments as part of its hearing-conservation programme. We obtained the noise map of the mill from the latest noise-risk assessment report and presented it in one of the slides to improve the workers’ understanding of the noise hazard present at their workstations.
- (v)
- Audiogram readingsParticipants were handed a copy of their latest audiometric test results during the session. As the presenter explained the audiogram interpretations, the participants could compare their audiograms with the examples shown on the slides. This method made the session more interactive for the participants.
- (vi)
- Technique demonstrationThe final part of the training session included a demonstration of the correct technique for wearing HPD.
2.3.5. Module B—Control Group
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Themann, C.L.; Masterson, E.A. Occupational Noise Exposure: A Review of Its Effects, Epidemiology, and Impact with Recommendations for Reducing Its Burden. J. Acoust. Soc. Am. 2019, 146, 3879–3905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuente, A.; Hickson, L. Noise-Induced Hearing Loss in Asia. Int. J. Audiol. 2011, 50, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Engdahl, B.; Tambs, K. Occupational Noise Exposure and Hearing: A Systematic Review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Occupational Safety and Health. Laporan Tahunan JKKP (DOSH Annual Report) 2020; Department of Occupational Safety and Health: Putrajaya, Malaysia, 2021. [Google Scholar]
- Sam, W.Y.; Anita, A.R.; Hayati, K.S.; Haslinda, A.; Lim, C.S. Shift Work As a Predictor of Hearing Protection Devices Use Among Manufacturing Workers in Selangor, Malaysia. Int. J. Public Health Clin. Sci. 2016, 3, 2289–7577. [Google Scholar]
- Ismail, A.F.; Daud, A.; Ismail, Z.; Abdullah, B. Noise-Induced Hearing Loss Among Quarry Workers in a North-Eastern State of Malaysia: A Study on Knowledge, Attitude and Practice. Oman Med. J. 2013, 28, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Factories and Machinery Act 1967. Factories and Machinery (Noise Exposure) Regulations 1989; Ministry of Labour: Kuala Lumpur, Malaysia, 1989. [Google Scholar]
- Haron, Z.; Abidin, M.Z.; Lim, M.H.; Yahya, K.; Jahya, Z.; Mohd, S.K.; Saim, A.A. Noise Exposure among Machine Operators on Construction Sites in South Johor, Malaysia. Adv. Mater. Res. 2014, 838–841, 2507–2512. [Google Scholar] [CrossRef]
- Mohd Rus, R.; Daud, A.; Musa, K.I.; Naing, L. Knowledge, Attitude and Practice of Sawmill Workers Towards Noise-Induced Hearing Loss in Kota Bharu, Kelantan. Malays. J. Med. Sci. 2008, 15, 28–34. [Google Scholar]
- El Dib, R.; Mathew, J.L.; Martins, R.H.G. Interventions to Promote the Wearing of Hearing Protection. Cochrane Database Syst. Rev. 2012, 4, 1–44. [Google Scholar] [CrossRef] [Green Version]
- Kreuter, M.W.; Lukwago, S.N.; Bucholtz, D.C.; Clark, E.M.; Sanders-Thompson, V. Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches. Health Educ. Behav. 2003, 30, 133–146. [Google Scholar] [CrossRef]
- Kerr, M.J.; Savik, K.; Monsen, K.A.; Lusk, S.L. Effectiveness of Computer-Based Tailoring Versus Targeting to Promote Use of Hearing Protection. Can. J. Nurs. Res. 2007, 39, 80–97. [Google Scholar]
- Lusk, S.L.; Ronis, D.L.; Kazanis, A.S.; Eakin, B.L.; Hong, O.S.; Raymond, D.M. Effectiveness of a Tailored Intervention to Increase Factory Workers’ Use of Hearing Protection. Nurs. Res. 2003, 52, 289–295. [Google Scholar] [CrossRef]
- Hong, O.S.; Ronis, D.L.; Lusk, S.L.; Kee, G.S. Efficacy of a Computer-Based Hearing Test and Tailored Hearing Protection Intervention. Int. J. Behav. Med. 2006, 13, 304–314. [Google Scholar] [CrossRef]
- Tantranont, K.; Codchanak, N. Predictors of Hearing Protection Use among Industrial Workers. Work. Health Saf. 2017, 65, 365–371. [Google Scholar] [CrossRef]
- Hong, O.S.; Lusk, S.L.; Ronis, D.L. Ethnic Differences in Predictors of Hearing Protection Behavior Between Black and White Workers. Res. Theory Nurs. Pract. 2005, 19, 63–76. [Google Scholar] [CrossRef]
- Lusk, S.L.; Ronis, D.L.; Baer, L.M. A Comparison of Multiple Indicators—Observations, Supervisors Report, and Self-Report as Measures of Workers’ Hearing Protection Use. Eval. Health Prof. 1995, 18, 51–63. [Google Scholar] [CrossRef] [Green Version]
- Wilson, K.; Korn, J.H. Attention during Lectures: Beyond Ten Minutes. Teach. Psychol. 2007, 34, 85–89. [Google Scholar] [CrossRef]
- Yahya, S.N.; Rahman, N.A.A.; Razali, A.; Rahman, N.I.A.; Haque, M. Satisfaction Study of Using Hearing Protection Device among Sawmill Workers in Kuantan, Malaysia. Int. J. Pharm. Res. 2016, 8, 50–56. [Google Scholar]
- Reddy, R.K.; Welch, D.; Thorne, P.; Ameratunga, S. Hearing Protection Use in Manufacturing Workers: A Qualitative Study. Noise Health 2012, 14, 202–209. [Google Scholar] [CrossRef]
- Hong, O.S.; Chin, D.L.; Fiola, L.A.; Kazanis, A.S. The Effect of a Booster Intervention to Promote Hearing Protection Behavior in Operating Engineers. Am. J. Ind. Med. 2013, 56, 258–266. [Google Scholar] [CrossRef]
- Lusk, S.L.; Eakin, B.L.; Kazanis, A.S.; McCullagh, M.C. Effects of Booster Interventions on Factory Workers’ Use of Hearing Protection. Nurs. Res. 2004, 53, 53–58. [Google Scholar] [CrossRef]
- Occupational Safety and Health Act 1994. Occupational Safety and Health (Noise Exposure) Regulations 2019; Ministry of Human Resources: Putrajaya, Malaysia, 1994. [Google Scholar]
- Reddy, R.; Welch, D.; Ameratunga, S.; Thorne, P. An Ecological Approach to Hearing-Health Promotion in Workplaces. Int. J. Audiol. 2017, 56, 316–327. [Google Scholar] [CrossRef] [PubMed]
- McCullagh, M.C. Effects of a Low Intensity Intervention to Increase Hearing Protector Use among Noise-Exposed Workers. Am. J. Ind. Med. 2011, 54, 210–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neitzel, R.; Meischke, H.; Daniell, W.E.; Trabeau, M.; Somers, S.; Seixas, N.S. Development and Pilot Test of Hearing Conservation Training for Construction Workers. Am. J. Ind. Med. 2008, 51, 120–129. [Google Scholar] [CrossRef] [PubMed]
| Domain | Number of Items | Mean | SD | Cronbach’s Alpha |
|---|---|---|---|---|
| Benefit of HPD use | 5 | 3.31 | 0.4 | 0.9 |
| Barriers to HPD use | 10 | 2.18 | 0.41 | 0.84 |
| Self-efficacy in HPD use | 5 | 2.7 | 0.44 | 0.79 |
| Susceptibility to hearing loss | 2 | 3.12 | 0.5 | 0.86 |
| Severity of hearing loss | 6 | 3.25 | 0.61 | 0.78 |
| Interpersonal influences | 3 | 3.04 | 0.41 | 0.74 |
| Situational influences | 5 | 3.38 | 0.42 | 0.91 |
| Variables | Control (n = 30) | Intervention (n = 30) | p-Value |
|---|---|---|---|
| Age (years) | 41.43 (8.67) a | 40.2 (10.26) a | 0.617 b |
| 21–30 | 6 | 7 | 0.053 c |
| 31–40 | 7 | 10 | |
| 41–50 | 12 | 3 | |
| 51–60 | 5 | 10 | |
| Working duration (years) | 16.07 (9.32) a | 14.87 (10.94) a | 0.649 b |
| 1–10 | 9 | 11 | 0.349 d |
| 11–20 | 9 | 9 | |
| 21–30 | 11 | 6 | |
| 31–40 | 1 | 4 | |
| Education level | |||
| Primary school | 2 | 2 | 1d |
| Secondary school | 25 | 26 | |
| College/University | 3 | 2 | |
| Perceived hearing status | |||
| Poor | 9 | 5 | 0.494 d |
| Fair | 8 | 10 | |
| Good | 12 | 12 | |
| Excellent | 1 | 3 |
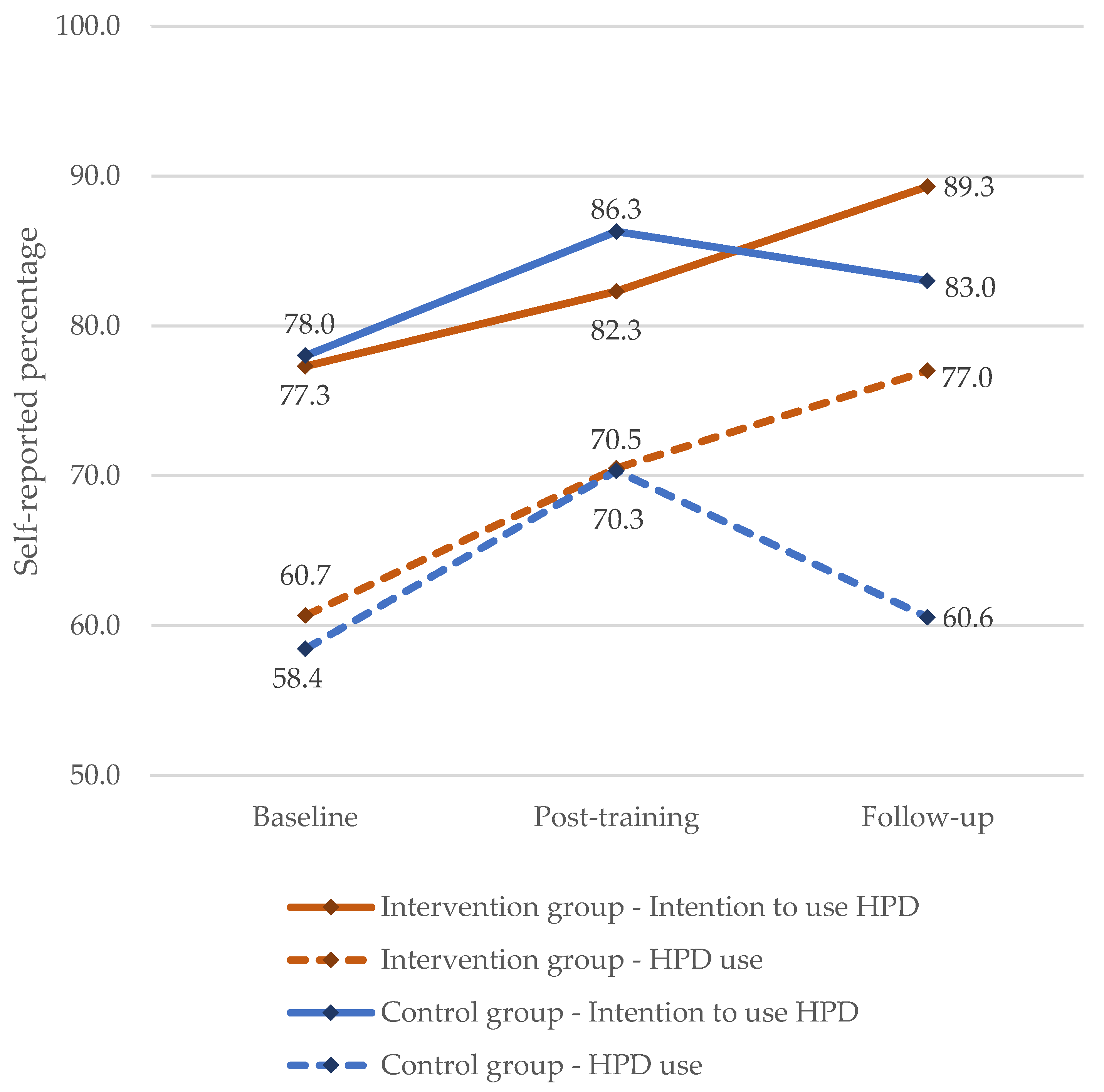
| Measures | Mean (SD) | Paired Analysis Baseline & Follow-Up p-Value | ||
|---|---|---|---|---|
| Baseline | Post-Training | Follow-Up | ||
| HPD use | ||||
| Intervention group | 60.67 (25.63) | 70.50 (25.81) | 77.00 (25.13) | <0.001 |
| Control group | 58.44 (22.40) | 70.33 (19.21) | 60.55 (27.62) | 0.675 |
| Intention to use HPD | ||||
| Intervention group | 77.33 (23.18) | 82.33 (22.39) | 89.33 (15.3) | 0.004 |
| Control group | 78.0 (12.43) | 86.33 (16.91) | 83.0 (23.8) | 0.247 |
| Measures | ANOVA | F (df) | ηp2 | p-Value |
|---|---|---|---|---|
| HPD use | ||||
| Time a | 7.14 (1.9, 110.4) | 0.11 | 0.001 c | |
| Training type b | 1.456 (1, 58) | 0.024 | 0.232 | |
| Time x Training type | 4.091 (1.9, 110.4) | 0.066 | 0.021 c | |
| Intention to use HPD | ||||
| Time a | 4.668 (2, 116) | 0.074 | 0.011 | |
| Training type b | 0.022 (1, 58) | <0.001 | 0.882 | |
| Time x Training type | 1.622 (2, 116) | 0.027 | 0.202 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ammar, S.; Daud, A.; Ismail, A.F.; Razali, A. Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia. Appl. Sci. 2022, 12, 2497. https://doi.org/10.3390/app12052497
Ammar S, Daud A, Ismail AF, Razali A. Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia. Applied Sciences. 2022; 12(5):2497. https://doi.org/10.3390/app12052497
Chicago/Turabian StyleAmmar, Sirri, Aziah Daud, Ahmad Filza Ismail, and Ailin Razali. 2022. "Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia" Applied Sciences 12, no. 5: 2497. https://doi.org/10.3390/app12052497
APA StyleAmmar, S., Daud, A., Ismail, A. F., & Razali, A. (2022). Efficacy of a Targeted Intervention Method to Improve the Use of Hearing Protection Devices among Agro-Industrial Workers in Malaysia. Applied Sciences, 12(5), 2497. https://doi.org/10.3390/app12052497






