Evaluation of Skeletal, Dentoalveolar, and Sagittal Airway Changes Induced by the Mandibular Anterior Repositioning Appliance (MARA) in Class II Malocclusion: A Retrospective Controlled Study on Lateral Cephalograms
Abstract
:1. Introduction
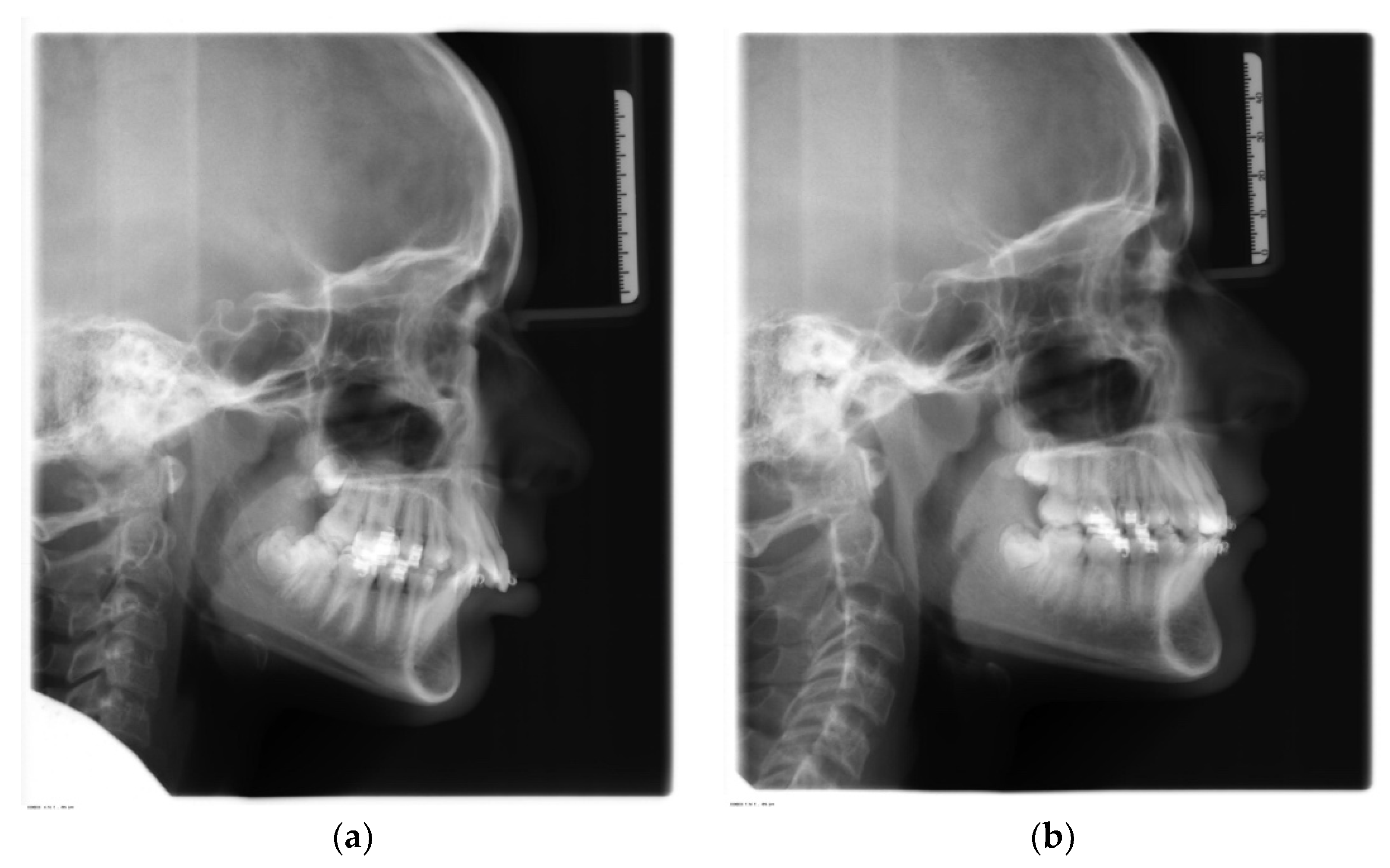
2. Materials and Methods
2.1. Cephalometric Analysis
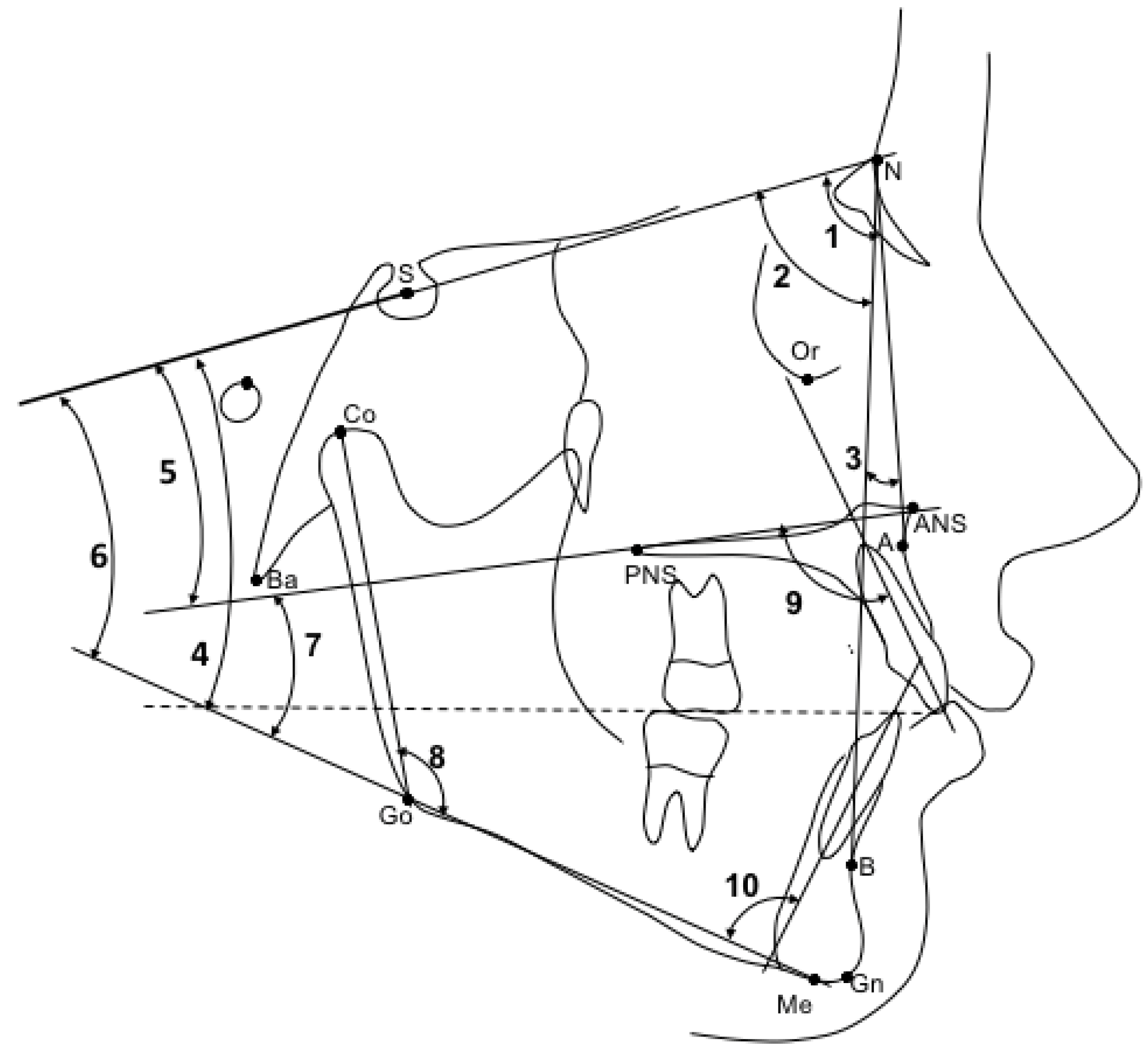
- SNA (°): angle between sella, nasion, and subspinale point A. It indicates the antero-posterior position of the maxilla relative to anterior cranial base (Figure 1, 1);
- SNB (°): angle between sella, nasion, and supramentale point B. It indicates the antero-posterior position of the mandible to anterior cranial base (Figure 1, 2);
- ANB (°): angle resulting from the difference between the SNA and SNB angles, which provide an indication of the sagittal skeletal relationships (Figure 1, 3);
- Wits (mm): is the measure of the segment Ao-Bo where Ao and Bo indicate respectively the projection of point A and point B on the occlusal plane (Figure 2, a);
- SN-Occlusal Plane (°): angle between the cranial base (SN) and the occlusal plane (Figure 1, 4);
- SN-Palatal Plane (°): angle between the cranial base (SN) and the palatal plane (Figure 1, 5);
- SN-Mandibular Plane (°): angle between the cranial base (SN) and the mandibular plane (Figure 1, 6);
- Palatal Plane-Mandibular Plane (°): angle between the bispinal plane and the mandibular plane, expressing intermaxillary divergence (Figure 1, 7);
- Co-Gn (mm): distance from condylion to anatomic gnathion, expressing total mandibular length (Figure 2, b);
- Co-Go (mm): distance from condylion to gonion, expressing the height of the mandibular ramus (Figure 2, c);
- Co-Go-Me (°): mandibular angle (Figure 1, 8);
- Overjet (mm): parameter indicating the measurement of the distance in the sagittal plane between the incisal margin of the upper incisors and the vestibular surface of the lower incisors (Figure 2, d);
- Overbite (mm): distance in the vertical plane between the incisal margin of the upper and lower central incisors (Figure 2, e);
- Molar relationship (mm): distance between the projections in the occlusal plane of the point of contact between the first permanent molars and the adjacent mesial tooth (second deciduous molar or second premolar) (Figure 2, f);
- Inc. Sup.-Pal. Pl. (°): angle expressing the inclination of the axis of the upper central incisor relative to the palatal plane (Figure 1, 9);
- Inc. Inf.-Mand. Pl. (°): angle expressing the inclination of the axis of the lower central incisor relative to the mandibular plane (Figure 1, 10);
- PNS-AD1 (mm): lower airway dimension; distance between the PNS and the nearest adenoid tissue measured through the PNS-Ba line (AD1) (Figure 3, g);
- AD1-Ba (mm): lower adenoid size; defined as the soft tissue thickness at the posterior nasopharynx wall through the PNS-Ba line (Figure 3, h);
- PNS-AD2 (mm): upper airway dimension; distance between the PNS and the nearest adenoid tissue measured through a perpendicular line to S-Ba from PNS (AD2) (Figure 3, i);
- AD2-H (mm): upper adenoid size; defined as the soft tissue thickness at the posterior nasopharynx wall through the PNS-H line (H, Hormion, point located at the intersection between the perpendicular line to S-Ba from PNS and the cranial base) (Figure 3, I);
- McNamara’s upper pharynx dimension (mm): the minimum distance between the upper soft palate and the nearest point on the posterior pharynx wall (Figure 3, m);
- McNamara’s lower pharynx dimension (mm): the minimum distance between the point where the posterior tongue contour crosses the mandible and the nearest point on the posterior pharynx wall (Figure 3, n).
2.2. Method Error
2.3. Statistical Analyses
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- McNamara, J.A. Components of class II malocclusion in children 8–10 years of age. Angle Orthod. 1981, 51, 177–202. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.; Tang, Z.; Gao, X.; Zeng, X.L. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod. 2010, 80, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; Stahl, F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: A double-blind study of consecutively treated patients at puberty. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 698.e1–698.e10. [Google Scholar] [CrossRef] [PubMed]
- Katyal, V.; Pamula, Y.; Martin, A.J.; Daynes, C.N.; Kennedy, J.D.; Sampson, W.J. Craniofacial and upper airway morphology in pediatric sleep-disordered breathing: Systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 20–30. [Google Scholar] [CrossRef] [PubMed]
- El, H.; Palomo, J.M. Airway volume for different dentofacial skeletal patterns. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e511–e521. [Google Scholar] [CrossRef] [PubMed]
- Banabilh, S.M.; Samsudin, A.R.; Suzina, A.H.; Dinsuhaimi, S. Facial profile shape, malocclusion and palatal morphology in Malay obstructive sleep apnea patients. Angle Orthod. 2010, 80, 37–42. [Google Scholar] [CrossRef]
- Carroll, J.L. Obstructive sleep-disordered breathing in children: New controversies, new directions. Clin. Chest Med. 2003, 24, 261–282. [Google Scholar] [CrossRef]
- Kaditis, A.G.; Alonso Alvarez, M.L.; Boudewyns, A.; Alexopoulos, E.I.; Ersu, R.; Joosten, K.; Larramona, H.; Miano, S.; Narang, I.; Trang, H.; et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: Diagnosis and management. Eur. Respir. J. 2016, 47, 69–94. [Google Scholar] [CrossRef]
- Li, Y. Early orthodontic treatment of skeletal Class II malocclusion may be effective to prevent the potential for OSAHS and snoring. Med. Hypotheses 2009, 73, 594–595. [Google Scholar] [CrossRef]
- Xiang, M.L.; Hu, B.; Liu, Y.; Sun, J.; Song, J. Changes in airway dimensions following functional appliances in growing patients with skeletal class II malocclusion: A systematic review and meta-analysis. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 170–180. [Google Scholar] [CrossRef]
- Mohamed, R.N.; Basha, S.; Al-Thomali, Y. Changes in upper airway dimensions following orthodontic treatment of skeletal Class II malocclusion with twin block appliance: A systematic review. Turk. J. Orthod. 2020, 33, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Rizk, S.; Kulbersh, V.P.; Al-Qawasmi, R. Changes in the oropharyngeal airway of Class II patients treated with the mandibular anterior repositioning appliance. Angle Orthod. 2016, 86, 955–961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baccetti, T.; Franchi, L.; McNamara, J.A. The Cervical Vertebral Maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar] [CrossRef]
- Cretella Lombardo, E.; Franchi, L.; Lione, R.; Chiavaroli, A.; Cozza, P.; Pavoni, C. Evaluation of sagittal airway dimensions after face mask therapy with rapid maxillary expansion in Class III growing patients. Int. J. Pediatr. Otorhinolaryngol. 2020, 130, 109794. [Google Scholar] [CrossRef]
- Springate, S. The effect of sample size and bias on the reliability of estimates of error: A comparative study of Dahlberg’s formula. Eur. J. Orthod. 2012, 34, 158–163. [Google Scholar] [CrossRef] [Green Version]
- Ghislanzoni, L.T.H.; Toll, D.E.; Defraia, E.; Baccetti, T.; Franchi, L. Treatment and posttreatment outcomes induced by the mandibular advancement repositioning appliance; A controlled clinical study. Angle Orthod. 2011, 81, 684–691. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.V.; Sparrow, S.A. Developing criteria for establishing interrater reliability of specific items: Applications to assessment of adaptive behavior. Am. J. Ment. Defic. 1981, 86, 127–137. [Google Scholar]
- Gönner, U.; Özkan, V.; Jahn, E.; Toll, D.E. Effect of the MARA appliance on the position of the lower anteriors in children, adolescents and adults with Class II malocclusion. J. Orofac. Orthop. 2007, 68, 397–412. [Google Scholar] [CrossRef]
- Pandis, N. Use of controls in clinical trials. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 250–251. [Google Scholar] [CrossRef]
- Vogler, R.C.; Wippold, F.J.; Pilgram, T.K. Age-specific size of the normal adenoid pad on magnetic resonance imaging. Clin. Otolaryngol. Allied Sci. 2000, 25, 392–395. [Google Scholar] [CrossRef]
- Songu, M.; Adibelli, Z.H.; Tuncyurek, O.; Adibelli, H. Age-specific size of the upper airway structures in children during development. Ann. Otol. Rhinol. Laryngol. 2010, 119, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Cozza, P.; Baccetti, T.; Franchi, L.; De Toffol, L.; McNamara, J.A. Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 599.e1–599.e12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arens, R.; McDonough, J.M.; Corbin, A.M.; Hernandez, M.E.; Maislin, G.; Schwab, R.J.; Pack, A.I. Linear dimensions of the upper airway structure during development: Assessment by magnetic resonance imaging. Am. J. Respir. Crit. Care Med. 2002, 165, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Perinetti, G.; Primožič, J.; Furlani, G.; Franchi, L.; Contardo, L. Treatment effects of fixed functional appliances alone or in combination with multibracket appliances: A systematic review and meta-analysis. Angle Orthod. 2015, 85, 480–492. [Google Scholar] [CrossRef] [PubMed]
- Huanca Ghislanzoni, L.T.; Baccetti, T.; Toll, D.; Defraia, E.; McNamara, J.A.; Franchi, L. Treatment timing of MARA and fixed appliance therapy of Class II malocclusion. Eur. J. Orthod. 2013, 35, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Cortese, M.; Pigato, G.; Casiraghi, G.; Ferrari, M.; Bianco, E.; Maddalone, M. Evaluation of the oropharyngeal airway space in class II malocclusion treated with mandibular activator: A retrospective study. J. Contemp. Dent. Pract. 2020, 21, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Chiqueto, K.; Henriques, J.F.C.; Barros, S.E.C.; Janson, G. Angle Class II correction with MARA appliance. Dent. Press J. Orthod. 2013, 18, 35–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Variables | MARA Group (n = 24) | Control Group (n = 20) | Diff. | p-Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Age at T1 (years) | 13.8 | 2.0 | 13.8 | 1.8 | 0.0 | 0.902 |
| Age at T2 (years) | 15.7 | 1.9 | 15.4 | 1.6 | 0.3 | 0.517 |
| T1-T2 interval (years) | 1.9 | 0.4 | 1.6 | 0.5 | 0.3 | 0.071 |
| CVM at T1 | CS1 = 4; CS2 = 3; CS3 = 2; CS4 = 6; CS5 = 6; CS6 = 2 | CS1 = 3; CS2 = 3; CS3 = 1; CS4 = 4; CS5 = 7; CS6 = 2 | 0.980 | |||
| CVM at T2 | CS2 = 2; CS3 = 4; CS4 = 7; CS5 = 5; CS6 = 5 | CS2 = 1; CS3 = 4; CS4 = 5; CS5 = 7; CS6 = 3 | 0.862 | |||
| Variables | MARA Group (n = 24) | Control Group (n = 20) | Diff. | p-Value | 95% CI of the Difference | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Lower | Upper | |||
| Age (years) | 13.8 | 2.0 | 13.8 | 1.8 | 0.0 | 0.902 | −1.1 | 1.2 |
| SNA (deg) | 80.3 | 4.2 | 81.1 | 3.2 | −0.8 | 0.517 | −3.0 | 1.5 |
| SNB (deg) | 75.4 | 3.2 | 75.9 | 2.8 | −0.5 | 0.632 | −2.3 | 1.4 |
| ANB (deg) | 4.9 | 2.4 | 5.2 | 1.6 | −0.3 | 0.638 | −1.6 | 1.0 |
| Wits (mm) | 2.7 | 2.5 | 2.3 | 3.1 | 0.4 | 0.591 | −1.3 | 2.2 |
| SN-Occ. Pl. (deg) | 17.2 | 3.6 | 17.8 | 3.8 | −0.6 | 0.551 | −2.9 | 1.6 |
| SN-Pal. Pl. (deg) | 7.8 | 2.9 | 7.8 | 2.9 | 0.0 | 0.974 | −1.7 | 1.8 |
| SN-Mand. Pl. (deg) | 31.8 | 6.1 | 30.5 | 4.7 | 1.3 | 0.424 | −2.0 | 4.7 |
| Pal. Pl. to Mand. Pl. (deg) | 24.0 | 5.7 | 22.7 | 5.0 | 1.3 | 0.431 | −2.0 | 4.6 |
| Co-Gn (mm) | 103.5 | 12.8 | 102.7 | 5.9 | 0.8 | 0.175 | ||
| Co-Go (mm) | 52.6 | 7.6 | 52.2 | 4.5 | 0.4 | 0.465 | ||
| Co-Go-Me (deg) | 121.6 | 6.2 | 121.5 | 5.4 | 0.1 | 0.948 | −3.5 | 3.7 |
| Overjet (mm) | 4.9 | 2.0 | 4.9 | 1.3 | 0.0 | 0.936 | −1.1 | 1.0 |
| Overbite (mm) | 2.9 | 1.8 | 4.1 | 2.2 | −1.2 | 0.062 | −2.4 | 0.1 |
| Molar Relationship (mm) | −0.1 | 1.5 | −0.6 | 1.7 | 0.5 | 0.338 | −0.5 | 1.5 |
| Upper Inc. to Pal. Pl. (deg) | 111.2 | 7.3 | 107.4 | 7.6 | 3.8 | 0.099 | −0.7 | 8.3 |
| Lower Inc. to Mand. Pl. (deg) | 102.0 | 6.5 | 103.5 | 7.8 | −1.5 | 0.495 | −5.8 | 2.9 |
| PNS-AD1 (mm) | 22.9 | 4.8 | 23.7 | 3.3 | −0.8 | 0.536 | −3.3 | 1.8 |
| AD1-Ba (mm) | 20.6 | 4.3 | 18.5 | 4.3 | 2.1 | 0.115 | −0.5 | 4.7 |
| PNS-AD2 (mm) | 18.1 | 3.9 | 18.7 | 4.1 | −0.6 | 0.649 | −3.0 | 1.9 |
| AD2-H (mm) | 11.3 | 3.7 | 10.6 | 3.8 | 0.7 | 0.529 | −1.6 | 3.0 |
| McNa Upper Pharinx (mm) | 12.4 | 3.9 | 12.6 | 3.4 | −0.2 | 0.809 | −2.5 | 2.0 |
| McNa Lower Pharinx (mm) | 9.4 | 2.6 | 10.2 | 2.8 | −0.8 | 0.297 | −2.5 | 0.8 |
| Variables | MARA Group (n = 24) | Control Group (n = 20) | Diff. | p-Value | 95% CI of the Difference | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Lower | Upper | |||
| SNA (deg) | −0.3 | 1.1 | 0.0 | 1.2 | −0.3 | 0.301 | −1.1 | 0.3 |
| SNB (deg) | 0.4 | 1.0 | 0.1 | 1.3 | 0.3 | 0.476 | −0.4 | 0.9 |
| ANB (deg) | −0.7 | 1.0 | −0.1 | 0.9 | −0.6 | 0.038 | −1.2 | 0.0 |
| Wits (mm) | −1.0 | 1.7 | 0.4 | 1.6 | −1.4 | 0.009 | −2.4 | −0.4 |
| SN-Occ. Pl. (deg) | 0.3 | 2.9 | −0.7 | 2.6 | 1.0 | 0.251 | −0.7 | 2.7 |
| SN-Pal. Pl. (deg) | 0.4 | 0.9 | 0.8 | 1.4 | −0.4 | 0.252 | −1.2 | 0.3 |
| SN-Mand. Pl. (deg) | −1.3 | 3.3 | −0.5 | 1.6 | −0.8 | 0.532 | ||
| Pal. Pl. to Mand. Pl. (deg) | −1.7 | 3.0 | −1.3 | 1.9 | −0.4 | 0.887 | ||
| Co-Gn (mm) | 3.2 | 2.4 | 3.0 | 2.3 | 0.2 | 0.732 | ||
| Co-Go (mm) | 2.3 | 1.7 | 2.2 | 1.7 | 0.1 | 0.785 | −0.9 | 1.2 |
| Co-Go-Me (deg) | −1.1 | 2.4 | −1.5 | 1.7 | 0.4 | 0.570 | −0.9 | 1.6 |
| Overjet (mm) | −2.2 | 2.2 | −0.3 | 0.9 | −1.9 | 0.001 | −3.0 | −0.8 |
| Overbite (mm) | −1.4 | 1.9 | 0.1 | 1.0 | −1.5 | 0.005 | ||
| Molar Relationship (mm) | 1.6 | 2.0 | −0.2 | 0.9 | 1.8 | 0.000 | 0.9 | 2.8 |
| Upper Inc. to Pal. Pl. (deg) | −1.4 | 7.2 | 0.6 | 2.9 | −2.0 | 0.249 | −5.5 | 1.5 |
| Lower Inc. to Mand. Pl. (deg) | 3.2 | 4.3 | 0.5 | 2.1 | 2.7 | 0.012 | 0.6 | 4.9 |
| PNS-AD1 (mm) | 0.6 | 2.2 | 0.4 | 3.5 | 0.2 | 0.855 | −1.6 | 1.9 |
| AD1-Ba (mm) | −0.1 | 2.3 | 0.3 | 3.0 | −0.4 | 0.211 | ||
| PNS-AD2 (mm) | 1.5 | 2.4 | 0.4 | 2.7 | 1.1 | 0.162 | −0.5 | 2.7 |
| AD2-H (mm) | −1.2 | 2.5 | 0.1 | 3.1 | −1.3 | 0.130 | −3.0 | 0.4 |
| McNa Upper Pharinx (mm) | 1.6 | 2.5 | 0.9 | 2.4 | 0.7 | 0.342 | −0.8 | 2.2 |
| McNa Lower Pharinx (mm) | 1.9 | 0.4 | 1.6 | 0.5 | 0.3 | 0.641 | −1.7 | 1.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Statie, M.D.; Franceschi, D.; Pierleoni, F.; Barone, V.; Popovic, N.; Nardi, C.; Franchi, L.; Giuntini, V. Evaluation of Skeletal, Dentoalveolar, and Sagittal Airway Changes Induced by the Mandibular Anterior Repositioning Appliance (MARA) in Class II Malocclusion: A Retrospective Controlled Study on Lateral Cephalograms. Appl. Sci. 2022, 12, 1484. https://doi.org/10.3390/app12031484
Statie MD, Franceschi D, Pierleoni F, Barone V, Popovic N, Nardi C, Franchi L, Giuntini V. Evaluation of Skeletal, Dentoalveolar, and Sagittal Airway Changes Induced by the Mandibular Anterior Repositioning Appliance (MARA) in Class II Malocclusion: A Retrospective Controlled Study on Lateral Cephalograms. Applied Sciences. 2022; 12(3):1484. https://doi.org/10.3390/app12031484
Chicago/Turabian StyleStatie, Maria Denisa, Debora Franceschi, Felicita Pierleoni, Valeria Barone, Nenad Popovic, Cosimo Nardi, Lorenzo Franchi, and Veronica Giuntini. 2022. "Evaluation of Skeletal, Dentoalveolar, and Sagittal Airway Changes Induced by the Mandibular Anterior Repositioning Appliance (MARA) in Class II Malocclusion: A Retrospective Controlled Study on Lateral Cephalograms" Applied Sciences 12, no. 3: 1484. https://doi.org/10.3390/app12031484
APA StyleStatie, M. D., Franceschi, D., Pierleoni, F., Barone, V., Popovic, N., Nardi, C., Franchi, L., & Giuntini, V. (2022). Evaluation of Skeletal, Dentoalveolar, and Sagittal Airway Changes Induced by the Mandibular Anterior Repositioning Appliance (MARA) in Class II Malocclusion: A Retrospective Controlled Study on Lateral Cephalograms. Applied Sciences, 12(3), 1484. https://doi.org/10.3390/app12031484









