Abstract
Current gait rehabilitation strategies rely heavily on motor learning principles, which involve facilitating active patient participation, high-doses of biomechanical task-related motor activities and accurate feedback. Furthermore, appropriate muscle groups need to be recruited for the joint movements that constitute the biomechanical task-related activities in order to effectively promote motor learning. Recently, exoskeleton-type robots utilizing crutches have been incorporated into overground gait rehabilitation programs. However, it is unclear which gait-related tasks are being trained because the joint movements and muscle recruitment patterns deviate from those of natural gait. This raises concerns because repetitive training with these devices may not lead to desirable rehabilitative gains. In this study, we compare the lower limb joint angles and electromyography patterns of healthy subjects walking with and without ReWalk in accordance with the three major biomechanical tasks required by bipedal gait: weight acceptance (WA), single-limb support, and limb advancement. Furthermore, we investigate whether the physical constraints of ReWalk, most noticeably the use of crutches and fixed ankle joints, were responsible for the specific changes by conducting additional walking sessions with either crutches or ankle foot orthoses. The results from the six healthy male volunteers suggest that the gait patterns observed with ReWalk deviate significantly from those of natural gait, particularly during the WA, and closely resemble those of crutch gait.
1. Introduction
Bipedal gait is the primary method of ambulation during everyday life. While most people can walk without much effort, the underlying mechanism requires intricate control of the individual muscles, the ensuing joint movements, and, moreover, whole-body balance [1,2,3]. What is interesting is that energy consumption is optimized during this complex process because of an inherent motor program shared by the general population [2,4,5]. Thus, a common repetition of sequential patterns can be observed during natural gait [1,6]. These patterns exist, in part, to execute specific biomechanical tasks, namely, weight acceptance, single-limb support, and limb advancement [1,7]. Constraints that limit the execution of certain motor programs not only affect the pertinent biomechanical task but, because of the reciprocity, also elicit compensation patterns that can be observed throughout the gait cycle. These compensation patterns can be found in abnormal gaits and, moreover, are indicative of innate pathological conditions [1,8].
Current gait rehabilitation strategies are based on motor learning principles, which require active patient participation and accurate feedback via intense training of biomechanical task-related motor activities [9,10,11,12,13,14]. When circumstances such as injuries or diseases inhibit the patients’ ability to independently perform gait, physical therapists are burdened with biomechanical tasks such as supporting bodyweight, moving the extremities, and maintaining balance during rehabilitation sessions [15,16]. This is not only physically demanding but, due to limited human resources and facilities, also impacts the patients’ training frequency and duration negatively.
Robot-assisted gait training (RAGT) has been proposed to alleviate this predicament and further promote quantitative rehabilitation sessions [17,18,19,20,21]. Contrary to high expectations, studies report that the full-bodyweight-supporting RAGTs, compared to conventional methods, fall short regarding rehabilitative efficacy [22,23]. It is widely accepted that this was due to a lack of patient participation, which was evident from diminished electromyography (EMG) signals [3,24]. More recently, exoskeleton-type robots, initially developed to assist with the ambulation of spinal cord injury (SCI) patients, have been proposed for RAGT. It was postulated that patient participation could be further facilitated because sensors were incorporated to identify gait intent and the patient controlled one’s own weight [22,25]. These studies indeed report a significant increase in EMG activity. However, it is of particular concern that the EMG patterns do not well match those of natural gait [3,26,27]. It is vital that the biomechanical task-related activities incorporated during RAGT promote the recruitment of appropriate muscle groups because rigorous training with deviant patterns may elicit non-physiological gait characteristics [10,11,13].
In this paper, we investigate how gait patterns change with ReWalk, an FDA-approved exoskeleton-type robot previously reported to improve quality of life for SCI patients [28], in order to investigate its potential use as a gait rehabilitation robot. Given that it is vital that specific interventions directly train the biomechanical tasks, we examine the gait patterns according to the three major gait-related biomechanical tasks, which are identifiable by three separate stages of the gait cycle [1]: weight acceptance (WA), single limb support (SS), and limb advancement (LA). We hypothesize that the use of elbow crutches and the immobilized ankle conformation of ReWalk, change the user’s natural gait patterns. The comparison was made by evaluating the lower limb kinematics as well as the EMG patterns during overground gait with ReWalk, elbow crutches, and AFOs. We find, from six healthy subjects that participated in this experiment, that walking with ReWalk closely resembles that of crutch gait, and, more importantly, deviates considerably from that of natural gait.
2. Materials and Methods
2.1. Experimental Setup
Six healthy male volunteers (age: 28.7 ± 1.2 years, height: 176.2 ± 3.3 cm, weight: 77.8 ± 8.9 kg) participated in this study. Each subject performed four gait conditions: with ReWalk (ReWalk Robotics Ltd., Yokneam Illit, Israel), with elbow crutches (ErgoBaum Comfortable Crutches, Ergoactives LLC, Miami, FL, USA), with ankle foot orthoses (AFO; Ottobock, Duderstadt, Germany) to immobilize the ankle, and unassisted natural overground gait. Participants were each asked to walk once in a straight line along a 20 m overground walkway for all conditions at a self-selected comfortable speed except for ReWalk sessions, where the default speed was selected, which is approximately 1.6 km/h. In order to investigate muscle recruitment patterns, EMG signals were obtained from the rectus femoris (RF), biceps femoris (BF), tibialis anterior (TA), and soleus (SL) of the right leg (Figure S1a) using wireless EMG sensors (TrignoTM wireless system, Delsys Inc.,Boston, MA, USA). In addition, inertial measurement unit (IMU) sensors placed on the waist and thigh, shank, and foot of both limbs were used to estimate hip, knee, and ankle joint angles along with foot contact (FC) and lift-off (LO) events (Figure 1). The EMG, acceleration, angular velocity, and orientation signals were sampled at approximately 1777, 148, 148, and 74 Hz, respectively.
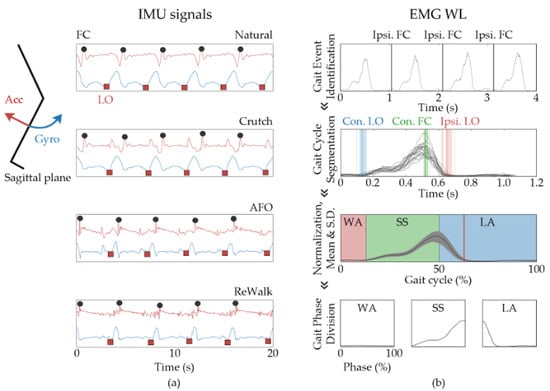
Figure 1.
Signal processing and representation of data acquired during gait sessions. (a) Gait event detection via acceleration (red lines) and angular velocity (blue lines) obtained from IMU sensors placed on the shank. The IMU data obtained from the shank of subject 1 is shown for each gait condition. The points at which the foot makes initial contact and leaves the ground are marked with black circles and red squares, respectively. (b) The top panel shows the EMG WL of soleus muscle during three gait cycles. Using the ipsilateral FC position (black lines), the SL EMG WL can be segmented into gait cycles (second panel). The blue, green, and red lines depict contralateral limb LO, contralateral limb FC, and ipsilateral limb LO, respectively. The third panel shows the ensemble-mean and SD of the SL EMG WL within a gait cycle with a black line and grey area, respectively. In addition, the red, green, and blue stages depict the WA, SS, and LA phases, respectively. The bottom panel depicts the mean SL EMG WL normalized against the respective phase progression.
All participants signed a written consent form, and the research ethics of human experiments were ensured by the approval of the gait sessions by the Institutional Review Board of Korea University (IRB No. 2021-0120-01).
2.2. Gait Cycle Event Identification
The gait cycle events, FC and LO, were identified by analyzing data obtained from an IMU sensor positioned on the shank via a method similar to what was described by Gottlieb et al. Jasiewicz et al. [29,30]. The heel contact events were identifiable by the local maximum following the global minimum of the acceleration signal and LO as the local minimum preceding the local maximum of the angular velocity (Figure 1a and Figure S1b).
2.3. Signal Processing
A band-pass filter (4th order Butterworth; 20 to 500 Hz) was applied to the EMG data, then we obtained the envelope function, a common approach [31,32,33] when comparing muscle activation levels, by calculating the waveform length (WL) [32,34]. The merits of the EMG WL reside in the fact that both amplitude and frequency are taken into account, as shown in Equation (1) below:
where n is the current sample and N is the window size.
The knee, hip, and ankle joint angles on the sagittal plane were also estimated so that changes due to different gait conditions could be evaluated. The IMU sensors used in this study provide 3D orientation data using information from the built-in acceleration, rotation, and earth magnetic field sensors. The joint angles were estimated by calculating the relative orientation of the IMU sensors, on the sagittal plane, that reside on each side of the respective joint. For instance, the knee joint angle was calculated by subtracting the orientation of the tibia from that of the thigh [35]. Once the FC and LO events were identified, the signals were segmented into gait cycles. We then normalized the signals along the time axis for each gait cycle, and the data was further represented as ensemble averages and standard deviation (S.D.). The data was further divided into the three gait-related biomechanical phases: WA, SS, and LA [1]. The WA phase begins with the FC of the ipsilateral limb and lasts until the LO of the contralateral limb. The subsequent SS phase ends with the FC of the contralateral limb, followed by the LA phase, which lasts until termination of the gait cycle (Figure 1b). All data processing was performed using a custom-built MATLAB (Mathworks Inc, Natick, MA, USA) code, and Wilcoxon signed rank tests were performed to assert any statistical significance.
3. Results
In order to investigate changes in muscle activation patterns elicited by ReWalk, we evaluated four lower-limb muscles (RF, BF, TA, and SL) that have well-documented functions during gait. The EMG WL during natural and ReWalk gaits depict significantly different patterns, as shown in the first and second columns of Figure 2, respectively. During the initial WA phase of natural gait, the BF, RF, and TA are known to coactivate in order to facilitate the loading response and ensure stability of the ipsilateral limb [1,36]. Furthermore, SL should be inactive to ensure proper heel striking. However, a completely altered pattern can be observed with ReWalk. The EMG signal from the RF has significantly decreased compared to the previous LA phase, and BF is activated after the WA phase has started. We also note that SL EMG signals start to increase upon FC, but TA is not activated.
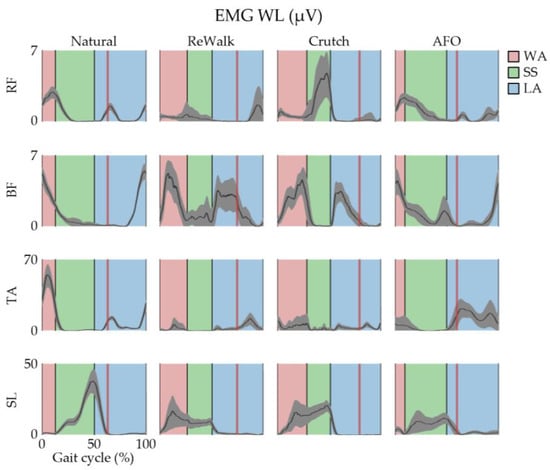
Figure 2.
Lower-limb EMG patterns within the gait cycle obtained during the gait sessions performed by subject 1. The gait cycle is further divided into three biomechanical task-related phases, where red, green, and blue stages represent the WA, SS, and LA phases, respectively. The red vertical line represents the ipsilateral foot’s LO position. The data are represented as mean ± SD via black lines and grey areas, respectively.
The differences in EMG patterns are not as drastic for the SS phase. During natural gait, a marked increase in SL and diminished BF, RF, and TA EMG levels can be observed. While a continuous increase of SL EMG is not observed during ReWalk gait, possibly due to early activation during the WA phase or that the body weight is partially supported via crutches, considerable levels are still observable, and the absence of TA activation suggests plantar flexion intent. Also, the other evaluated muscle sites had diminished EMG levels, which is consistent with natural gait. Lastly, other than the differences observed in the late LA phase that elicited the previously mentioned WA phase discrepancies, one notable characteristic of ReWalk gait is the significant increase in BF EMG in the early LA phase, which would result in either knee flexion or hip extension.
We now examine whether the form factor, most noticeably crutches and ankle immobilization, is responsible for the changes in gait patterns by investigating EMG patterns during gait with either crutches or an AFO, shown in the third and fourth columns of Figure 2, respectively. It is clearly observable that coactivation of BF and RF is absent at the start of the WA phase during crutch gait, much like what was observed with ReWalk. Furthermore, SL is actively involved and TA is absent during the WA phase. What is interesting is that the waveforms of RF and BF EMG WL during AFO gait, despite some differences in amplitude, resemble that of natural gait. The differences found with SL and TA occur in the early WA and LA phases, respectively. However, the changes in EMG patterns observed with AFO gait were not present during ReWalk gait. Taken together, the results suggest that the changes in muscle activation patterns may have been elicited by the use of crutches.
In order to identify the similarities between the ReWalk and crutch gaits, we overlay and present the EMG WL data normalized to 100% of each gait-related biomechanical phase (Figure 3) before proceeding with our qualitative analysis. We can roughly categorize each time trace within the gait-related biomechanical phase as either dormant, increasing, decreasing, leveling, peaking, or a combination of the above. During the WA gait stage, both ReWalk and crutch gait exhibit dormant, peak, dormant, and increase followed by leveling for RF, BF, TA, and SL, respectively. There are no coinciding patterns for natural gait during the WA gait stage. For the SS gait stage, BF, TA, and SL all match for ReWalk and crutch gait but the RF muscle shows different patterns, as RF is dormant for ReWalk but a peak is observed for crutch gait. As we move on to the LA gait stage, the patterns for all of the observed muscles (RF, BF, TA, and SL) seem to match pretty well for ReWalk and crutch gait, at least compared to natural gait. Collectively, other than RF during the SS gait stage, we do not observe any significant qualitative differences in time-trace patterns within the biomechanical phases. We also obtained the average EMG WL of all steps performed during each gait session in order to quantitatively evaluate our previous analysis (Figure 3b). Each gait condition was performed at different speeds and different weight-bearing conditions; thus, we would like to point out that careful interpretation is warranted. Specifically, the absence of activation, such as, missing activation of RF, and TA and the activation of SL in the WA phase, was observed and should be investigated further. However, because the difference observed with BF was not in EMG levels but rather a delay in timing, the mean EMG WL values alone do not exhibit as drastic changes. Thus, examination of EMG levels as well as time trace patterns seems necessary when evaluating EMG patterns.
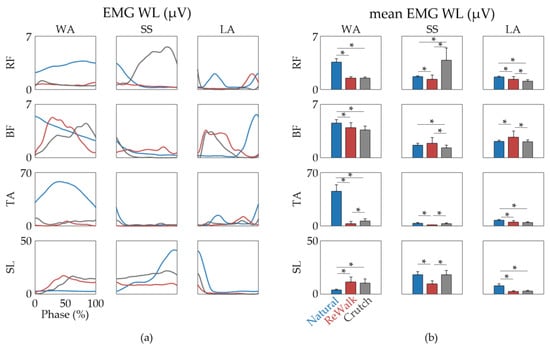
Figure 3.
Comparison of EMG patterns in subject 1 divided according to the gait-related biomechanical phases. (a) Overlay of mean EMG WL during WA, SS, and LA phases obtained from ReWalk (red lines), natural (blue lines), and crutch (grey lines) gait conditions. (b) Bar graph representing the average EMG WL over the WA, SS, and LA phase periods. The data are shown as mean ± SD. Statistical significance was assessed by the Wilcoxon signed rank test (* denotes p < 0.05).
We also analyzed the hip, knee, and ankle joint angles during the gait sessions (Figure 4). Both ReWalk and crutch gait show similar hip angles, which display noticeably more flexion compared to natural gait throughout the entire gait cycle. However, this is not observed with the AFO gait (Figure S2). This is somewhat expected considering the subject leans forward at the hips when using crutches. The knee joint angles, on the other hand, are relatively comparable during the WA and SS phases for all gait conditions, while some discrepancies are apparent in the LA phase. The maximum knee flexion angles of the crutch and ReWalk gaits are similar; however, the point at which this angle occurs is delayed. This may be due to the ReWalk’s “pre-programmed” slight pause before the start of the swing motion. Lastly, ReWalk and crutch gait both lack dorsiflexion during the early WA phase, just as the EMG pattern analysis suggested. Thus, taking the EMG and joint angle pattern analysis together, our results suggest that ReWalk and crutch gait are similar to each other and significantly different from natural gait, particularly during the WA phase.

Figure 4.
Comparison of joint angles in subject 1 divided according to the gait-related biomechanical phases. (a) Overlay of mean hip, knee, and ankle joint angles during WA, SS, and LA phases obtained from ReWalk (red lines), natural (blue lines), and crutch (grey lines) gait conditions. (b) Bar graph representing the average joint angles over the WA, SS, and LA phase periods. The data are shown as mean ± SD. Statistical significance was assessed by independent two sample t-tests (* denotes p < 0.05).
We have made several postulations regarding how crutches are mainly responsible for changes in gait patterns observed with ReWalk by examining EMG patterns and joint angles acquired from one subject. To further substantiate our postulations, we investigate whether these observations are consistent throughout the participant group.
Table 1 shows that the changes in subject #1′s gait patterns when walking with ReWalk were also observed with most of the subjects that participated in this study. We note that both increased hip flexion during the SS phase and decreased knee flexion during the LA phase are observed throughout the group, which is not surprising considering that it is only natural when negotiating balance with partial body weight supported by crutches. Also, because delayed activation is not well represented via mean EMG WL values, we only present those of RF, SL, and TA during the WA phase in Table 2, Table 3, and Table 4, respectively. The mean and SD are presented with the difference (%) between one another. Furthermore, the statistical significance was assessed using the Wilcoxon signed rank test because, when confirmed with the Shapiro-Wilk test, less than half of the data followed a normal distribution (Table S1). The results show that the EMG WL levels of ReWalk and crutch gait are closer to each other than those of natural gait, although this was not systematically the case for each subject and EMG. However, absence of a statistically significant EMG WL difference was most often found in the Crutch-ReWalk comparison (Table 2, Table 3 and Table 4).

Table 1.
Changes in gait patterns due to ReWalk that were commonly observed with crutch gait.

Table 2.
Comparison of mean RF EMG WL during the WA phase.

Table 3.
Comparison of mean TA EMG WL during the WA phase.

Table 4.
Comparison of mean SL EMG WL during the WA phase.
4. Discussion
In this study, we present an in-depth investigation of lower-limb EMG and joint angle patterns while walking with ReWalk. Analysis of EMG obtained from four muscles involved with controlling the hip, knee, and ankle joints was executed hand in hand with the joint angles. Because gait is a series of reciprocal events that require specific biomechanical tasks in order to maintain balance and forward progression, we investigated the gait patterns by segmenting the signals into WA, SS, and LA phases. We find that with ReWalk, significant deviation from natural gait can be observed in the WA and LA phases. By further examining crutch- and AFO-gait experiments collectively, our results suggest that ReWalk gait patterns closely follow crutch gait rather than that of natural gait.
Throughout this paper, we have painted the fact that ReWalk gait resembles that of crutch gait rather than a natural gait with a rather negative brush. However, this is not always the case, as with some patients, it might be too optimistic to expect full recovery and achieve a bipedal, natural gait. These patients need a means to increase quality of life, which is not confined to rehabilitative gains but also includes feasibility, costs, and assistance with activities of everyday life [37,38,39,40].
It is our belief that conventional comparisons of average EMG levels during stance and swing phases, or sometimes even cruder entire gait cycles, may be sufficient for measuring volitional intent but do not come close when describing gait patterns. For instance, while the average BF EMG WL during the WA phase from ReWalk, crutch, and natural gait are comparable, the elicited time trace patterns and the underlying functions are significantly different. Thus, a thorough comparison of the time traces is warranted. However, precaution must be taken when comparing time traces, especially with unconventional gait patterns, as the relative timing of each biomechanical task within the gait cycle may be significantly different. This is most evident with the different relative LO positions within a single gait cycle that can be clearly observed from our gait sessions. Taken together, we would like to emphasize that our data analysis within the corresponding gait-related biomechanical phases played an important role in elucidating gait patterns elicited via ReWalk.
Even though our results were presented with quantitative data, we do note that our analysis of the time traces is somewhat qualitative and might be susceptible to individual perception. This is in part, due to the inherent difficulties of quantitative assessment of similarity between two graphs. Some studies have proposed employing methods such as LFM and cross-correlation [41,42,43], however, precaution is warranted as slight phase shifts in parabolic traces can elicit very low similarity values. This predicament could be alleviated and might even be necessitated, when analyzing data from large populations, by employing artificial intelligence-based pattern recognition techniques.
To summarize this study, we have demonstrated that our gait phase analysis method is essential when analyzing gait patterns and assessing biomechanical task-related gait activities that are facilitated by interventions. By comparing the gait patterns elicited by ReWalk with that of natural, crutch-, and AFO gait, future investigations may be able to improve RAGT by shying away from crutches in cases where loading response training is essential and focus on control systems that enable proper promotion of natural gait.
We would like to point out that the size of our participant group is of particular concern. The fact that we have only enrolled 6 participants is much too small to reach any definitive conclusions. Moreover, the participants are all healthy males in their late 20s, thus the observations made in this study would in fact be confined to this demographic group. This warrants further studies that include a wider demographic of participants and we currently in preparation of a follow up study with a wider weight, sex, and age group.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/app122412574/s1, Figure S1: The EMG and IMU sensor positions; Figure S2. Lower-limb joint angles within the gait cycle obtained during the gait sessions performed by subject 1. Table S1. Shapiro-Wilks test p-values for RF, TA, and SL EMG WL during WA phase.
Author Contributions
Conceptualization, J.K. and S.-J.K.; methodology, J.K. and Y.K.; software, J.K. and Y.K.; validation, J.K., Y.K. and S.-J.K.; formal analysis, J.K.; investigation, Y.K.; resources, S.-J.K.; data curation, J.K.; writing—original draft preparation, J.K.; writing—review and editing, J.K. and S.-J.K.; visualization, Y.K.; supervision, S.-J.K.; project administration, S.-J.K.; funding acquisition, S.-J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the National Research Council of Science and Technology (NST) grant by the Korea government (MSIT) (No. CAP20000-000) and by the Intramural Program (Project No. K1804361) of Korea University.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Korea University (IRB No. 2021-0120-01 on 1 April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Perry, J. Gait Analysis: Normal and Pathological Function; SLACK Incorporated: Thorofare, NJ, USA, 1992; pp. 3–16. [Google Scholar]
- Queralt, A.; Valls-Solé, J.; Castellote, J.M. Speeding up Gait Initiation and Gait-Pattern with a Startling Stimulus. Gait Posture 2010, 31, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Swank, C.; Wang-Price, S.; Gao, F.; Almutairi, S. Walking with a Robotic Exoskeleton Does Not Mimic Natural Gait: A within-Subjects Study. JMIR Rehabil. Assist. Technol. 2019, 6, e11023. [Google Scholar] [CrossRef] [PubMed]
- Park, K.; Roemmich, R.T.; Elrod, J.M.; Hass, C.J.; Hsiao-Wecksler, E.T. Effects of Aging and Parkinson’s Disease on Joint Coupling, Symmetry, Complexity and Variability of Lower Limb Movements during Gait. Clin. Biomech. 2016, 33, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Scafetta, N.; Marchi, D.; West, B.J. Understanding the Complexity of Human Gait Dynamics. Chaos 2009, 19, 026108. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, M.A.; Veicsteinas, A.; Rampichini, S.; Cé, E.; Nemni, R.; Riboldazzi, G.; Merati, G. Energy Cost of Spontaneous Walking in Parkinson’s Disease Patients. Neurol. Sci. 2012, 33, 779–784. [Google Scholar] [CrossRef]
- Kharb, A.; Saini, V.; Jain, Y.; Dhiman, S. A review of gait cycle and its parameters. IJCEM Int. J. Comput. Eng. Manag. 2011, 13, 78–83. [Google Scholar]
- Chen, C.L.; Chen, H.C.; Tang, S.F.T.; Wu, C.Y.; Cheng, P.T.; Hong, W.H. Gait performance with compensatory adaptations in stroke patients with different degrees of motor recovery. Am. J. Phys. Med. Rehabil. 2003, 82, 925–935. [Google Scholar] [CrossRef]
- Van Peppen, R.P.S.; Kwakkel, G.; Wood-Dauphinee, S.; Hendriks, H.J.M.; van der Wees, P.J.; Dekker, J. The Impact of Physical Therapy on Functional Outcomes after Stroke: What’s the Evidence? Clin. Rehabil. 2004, 18, 833–862. [Google Scholar] [CrossRef]
- Carr, J.H.; Shepherd, R.B. A Motor Learning Model for Stroke Rehabilitation. Physiotherapy 1989, 75, 372–380. [Google Scholar] [CrossRef]
- Bowles, A.O.; Kevorkian, C.G.; Rintala, D.H. Gender Differences Regarding Career Issues and Promotion in Academic Physical Medicine and Rehabilitation. Am. J. Phys. Med. Rehabil. 2007, 86, 918–925. [Google Scholar] [CrossRef]
- Daly, J.J.; Ruff, R.L. Construction of Efficacious Gait and Upper Limb Functional Interventions Based on Brain Plasticity Evidence and Model-Based Measures for Stroke Patients. Sci. World J. 2007, 7, 2031–2045. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.; Shepherd, R. Neurological Rehabilitation: Optimizing Motor Performance, 2nd ed.; Churchill Livingstone: Edinburgh, UK, 2010. [Google Scholar]
- Morone, G.; Paolucci, S.; Cherubini, A.; de Angelis, D.; Venturiero, V.; Coiro, P.; Iosa, M. Robot-Assisted Gait Training for Stroke Patients: Current State of the Art and Perspectives of Robotics. Neuropsychiatr. Dis. Treat. 2017, 13, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Sale, P.; Franceschini, M.; Waldner, A.; Hesse, S. Use of the robot assisted gait therapy in rehabilitation of patients with stroke and spinal cord injury. Eur. J. Phys. Rehabil. Med. 2012, 48, 111–121. [Google Scholar] [PubMed]
- Calabrò, R.S.; Cacciola, A.; Bertè, F.; Manuli, A.; Leo, A.; Bramanti, A.; Naro, A.; Milardi, D.; Bramanti, P. Robotic Gait Rehabilitation and Substitution Devices in Neurological Disorders: Where Are We Now? Neurol. Sci. 2016, 37, 503–514. [Google Scholar] [CrossRef]
- Gassert, R.; Dietz, V. Rehabilitation Robots for the Treatment of Sensorimotor Deficits: A Neurophysiological Perspective. J. Neuroeng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Poli, P.; Morone, G.; Rosati, G.; Masiero, S. Robotic Technologies and Rehabilitation: New Tools for Stroke Patients’ Therapy. BioMed Res. Int. 2013, 2013, 153872. [Google Scholar] [CrossRef] [PubMed]
- Dzahir, M.A.M.; Yamamoto, S.I. Recent Trends in Lower-Limb Robotic Rehabilitation Orthosis: Control Scheme and Strategy for Pneumatic Muscle Actuated Gait Trainers. Robotics 2014, 3, 120–148. [Google Scholar] [CrossRef]
- Goffredo, M.; Iacovelli, C.; Russo, E.; Pournajaf, S.; di Blasi, C.; Galafate, D.; Pellicciari, L.; Agosti, M.; Filoni, S.; Aprile, I.; et al. Stroke Gait Rehabilitation: A Comparison of End-Effector, Overground Exoskeleton, and Conventional Gait Training. Appl. Sci. 2019, 9, 2627. [Google Scholar] [CrossRef]
- Valè, N.; Gandolfi, M.; Vignoli, L.; Botticelli, A.; Posteraro, F.; Morone, G.; Dell’orco, A.; Dimitrova, E.; Gervasoni, E.; Goffredo, M.; et al. Electromechanical and Robotic Devices for Gait and Balance Rehabilitation of Children with Neurological Disability: A Systematic Review. Appl. Sci. 2021, 11, 12061. [Google Scholar] [CrossRef]
- Pennycott, A.; Wyss, D.; Vallery, H.; Klamroth-Marganska, V.; Riener, R. Towards More Effective Robotic Gait Training for Stroke Rehabilitation: A Review. J. Neuroeng. Rehabil. 2012, 9, 65. [Google Scholar] [CrossRef]
- Belda-Lois, J.M.; Mena-Del Horno, S.; Bermejo-Bosch, I.; Moreno, J.C.; Pons, J.L.; Farina, D.; Iosa, M.; Molinari, M.; Tamburella, F.; Ramos, A.; et al. Rehabilitation of Gait after Stroke: A Review towards a Top-down Approach. J. Neuroeng. Rehabil. 2011, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Israel, J.F.; Campbell, D.D.; Kahn, J.H.; Hornby, T.G. Metabolic Costs and Muscle Activity Patterns during Robotic- and Therapist-Assisted Treadmill Walking in Individuals with Incomplete Spinal Cord Injury. Phys. Ther. 2006, 86, 1466–1478. [Google Scholar] [CrossRef] [PubMed]
- Androwis, G.J.; Pilkar, R.; Ramanujam, A.; Nolan, K.J. Electromyography Assessment during Gait in a Robotic Exoskeleton for Acute Stroke. Front. Neurol. 2018, 9, 630. [Google Scholar] [CrossRef] [PubMed]
- Sylos-Labini, F.; la Scaleia, V.; d’Avella, A.; Pisotta, I.; Tamburella, F.; Scivoletto, G.; Molinari, M.; Wang, S.; Wang, L.; van Asseldonk, E.; et al. EMG Patterns during Assisted Walking in the Exoskeleton. Front. Hum. Neurosci. 2014, 8, 423. [Google Scholar] [CrossRef]
- De Luca, A.; Bellitto, A.; Mandraccia, S.; Marchesi, G.; Pellegrino, L.; Coscia, M.; Leoncini, C.; Rossi, L.; Gamba, S.; Massone, A.; et al. Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations. Appl. Sci. 2019, 9, 2868. [Google Scholar] [CrossRef]
- Van Nes, I.J.W.; van Dijsseldonk, R.B.; van Herpen, F.H.M.; Rijken, H.; Geurts, A.C.H.; Keijsers, N.L.W. Improvement of Quality of Life after 2-Month Exoskeleton Training in Patients with Chronic Spinal Cord Injury. J. Spinal Cord Med. 2022. [Google Scholar] [CrossRef]
- Gottlieb, U.; Balasukumaran, T.; Hoffman, J.R.; Springer, S. Agreement of Gait Events Detection during Treadmill Backward Walking by Kinematic Data and Inertial Motion Units. Sensors 2020, 20, 6331. [Google Scholar] [CrossRef]
- Jasiewicz, J.M.; Allum, J.H.J.; Middleton, J.W.; Barriskill, A.; Condie, P.; Purcell, B.; Li, R.C.T. Gait Event Detection Using Linear Accelerometers or Angular Velocity Transducers in Able-Bodied and Spinal-Cord Injured Individuals. Gait Posture 2006, 24, 502–509. [Google Scholar] [CrossRef]
- Nandedkar, S.D.; Sanders, D.B. Sanders. Measurement of the amplitude of the EMG envelope. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 1990, 13, 933–938. [Google Scholar] [CrossRef]
- Kim, J.; Chung, S.H.; Choi, J.; Lee, J.M.; Kim, S.J. Practical Method for Predicting Intended Gait Speed via Soleus Surface EMG Signals. Electron. Lett. 2020, 56, 528–531. [Google Scholar] [CrossRef]
- Barzilay, O.; Wolf, A. A Fast Implementation for EMG Signal Linear Envelope Computation. J. Electromyogr. Kinesiol. 2011, 21, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Englehart, K.; Hudgins, B. A Robust, Real-Time Control Scheme for Multifunction Myoelectric Control. IEEE Trans. Biomed. Eng. 2003, 50, 848–854. [Google Scholar] [CrossRef] [PubMed]
- Saito, A.; Kizawa, S.; Kobayashi, Y.; Miyawaki, K. Pose Estimation by Extended Kalman Filter Using Noise Covariance Matrices Based on Sensor Output. ROBOMECH J. 2020, 7, 36. [Google Scholar] [CrossRef]
- Boudarham, J.; Hameau, S.; Zory, R.; Hardy, A.; Bensmail, D.; Roche, N. Coactivation of Lower Limb Muscles during Gait in Patients with Multiple Sclerosis. PLoS ONE 2016, 11, e0158267. [Google Scholar] [CrossRef] [PubMed]
- Platz, T.; Gillner, A.; Borgwaldt, N.; Kroll, S.; Roschka, S. Device-Training for Individuals with Thoracic and Lumbar Spinal Cord Injury Using a Powered Exoskeleton for Technically Assisted Mobility: Achievements and User Satisfaction. BioMed Res. Int. 2016, 2016, 8459018. [Google Scholar] [CrossRef]
- Lajeunesse, V.; Vincent, C.; Routhier, F.; Careau, E.; Michaud, F. Exoskeletons’ Design and Usefulness Evidence According to a Systematic Review of Lower Limb Exoskeletons Used for Functional Mobility by People with Spinal Cord Injury. Disabil. Rehabil. Assist. Technol. 2016, 11, 535–547. [Google Scholar] [CrossRef]
- Tamburella, F.; Lorusso, M.; Tramontano, M.; Fadlun, S.; Masciullo, M.; Scivoletto, G. Overground Robotic Training Effects on Walking and Secondary Health Conditions in Individuals with Spinal Cord Injury: Systematic Review. J. Neuroeng. Rehabil. 2022, 19, 27. [Google Scholar] [CrossRef]
- Fritz, H.; Patzer, D.; Galen, S.S. Robotic Exoskeletons for Reengaging in Everyday Activities: Promises, Pitfalls, and Opportunities. Disabil. Rehabil. 2019, 41, 560–563. [Google Scholar] [CrossRef]
- Iosa, M.; Cereatti, A.; Merlo, A.; Campanini, I.; Paolucci, S.; Cappozzo, A. Assessment of Waveform Similarity in Clinical Gait Data: The Linear Fit Method. BioMed Res. Int. 2014, 2014, 214156. [Google Scholar] [CrossRef]
- Iosa, M.; Peppe, A.; Morone, G.; Bottino, S.; Bini, F.; Marinozzi, F.; Paolucci, S. Assessment of Waveform Similarity in Electromyographical Clinical Gait Data: The Linear Fit Method. J. Med. Biol. Eng. 2018, 38, 774–781. [Google Scholar] [CrossRef]
- Wren, T.A.L.; Patrick Do, K.; Rethlefsen, S.A.; Healy, B. Cross-Correlation as a Method for Comparing Dynamic Electromyography Signals during Gait. J. Biomech. 2006, 39, 2714–2718. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).