Gummy Smile Improvement during Growth Period Using a Simple Bite Jumping Appliance and High-Pull J-Hook HeadGear: A Case Series Study
Abstract
1. Introduction
2. Methods
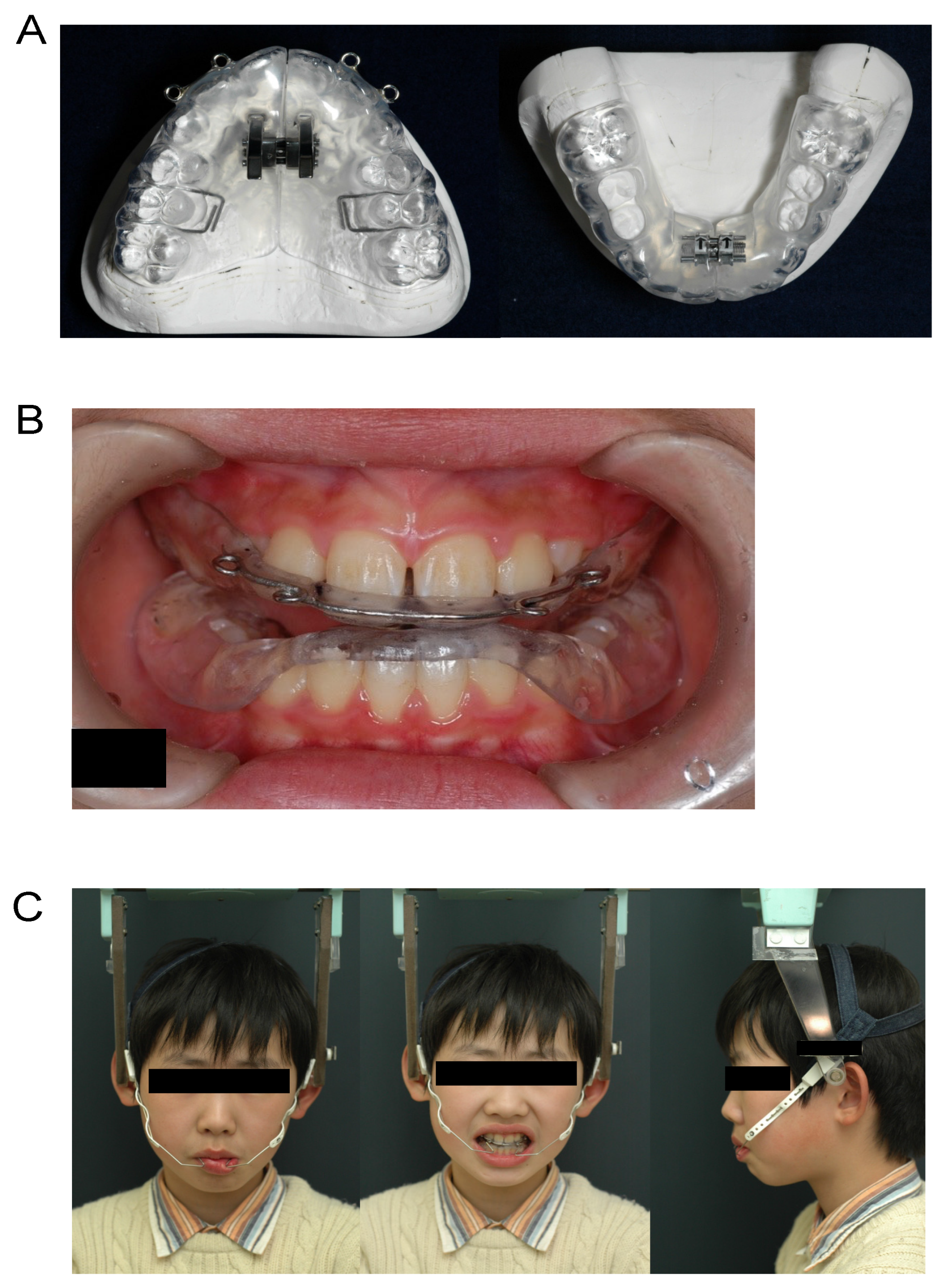
2.1. Differences between Simple Bite Jumping Appliance (SBJA) and BJA
2.2. Attachment of Loop to SBJA
2.3. Combined Use of SBJA and High-Pull J-Hook Headgear
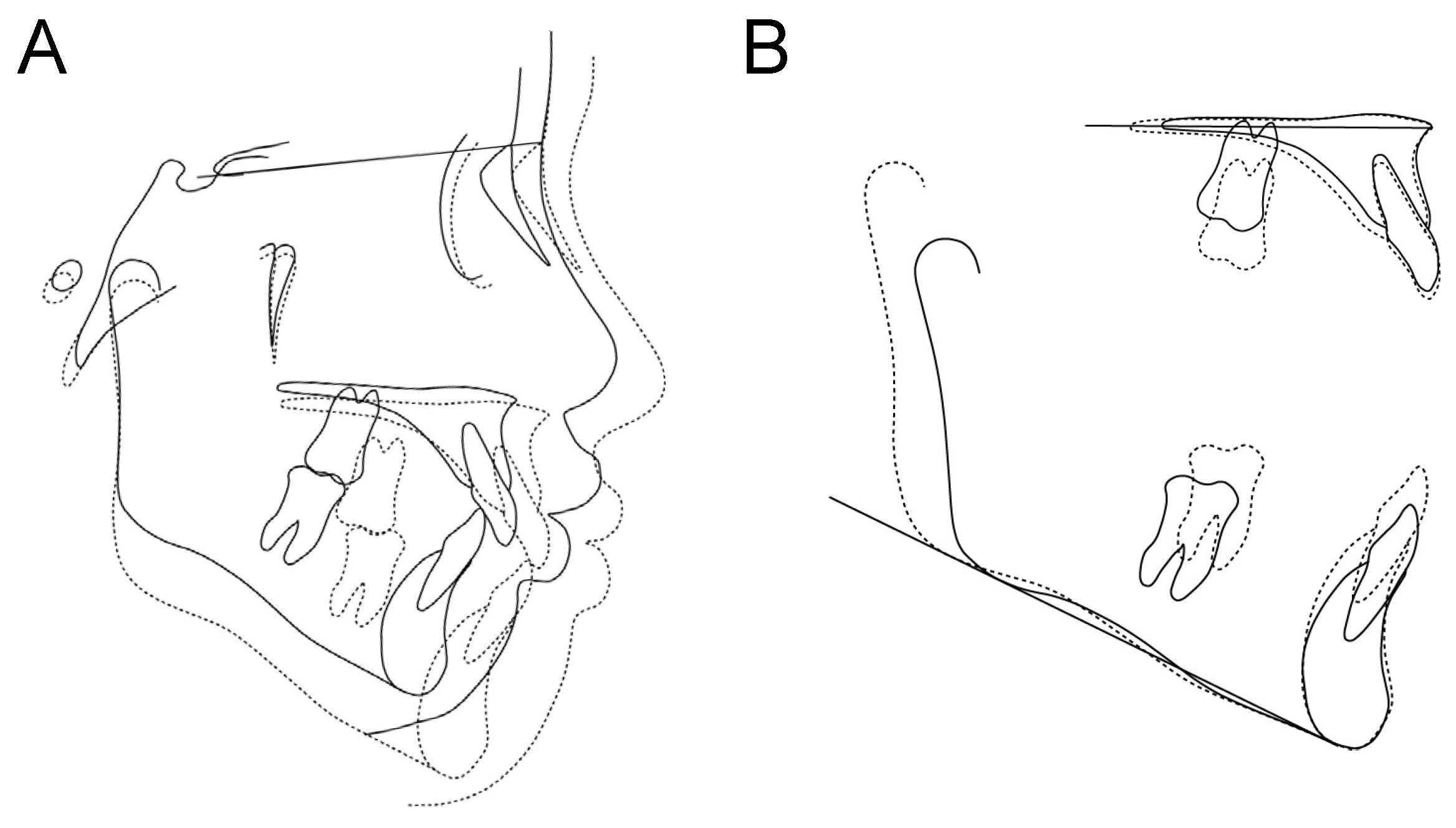
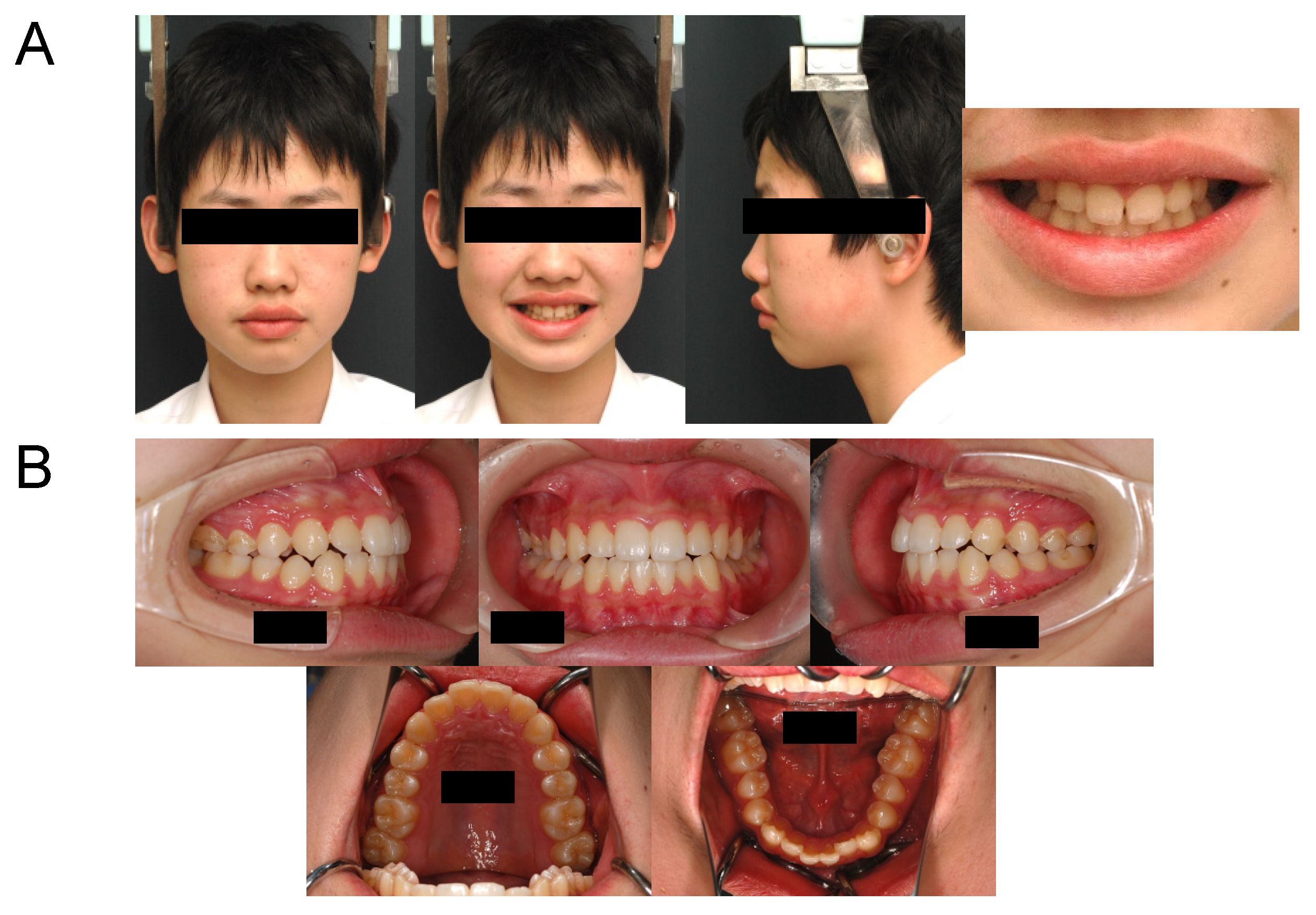
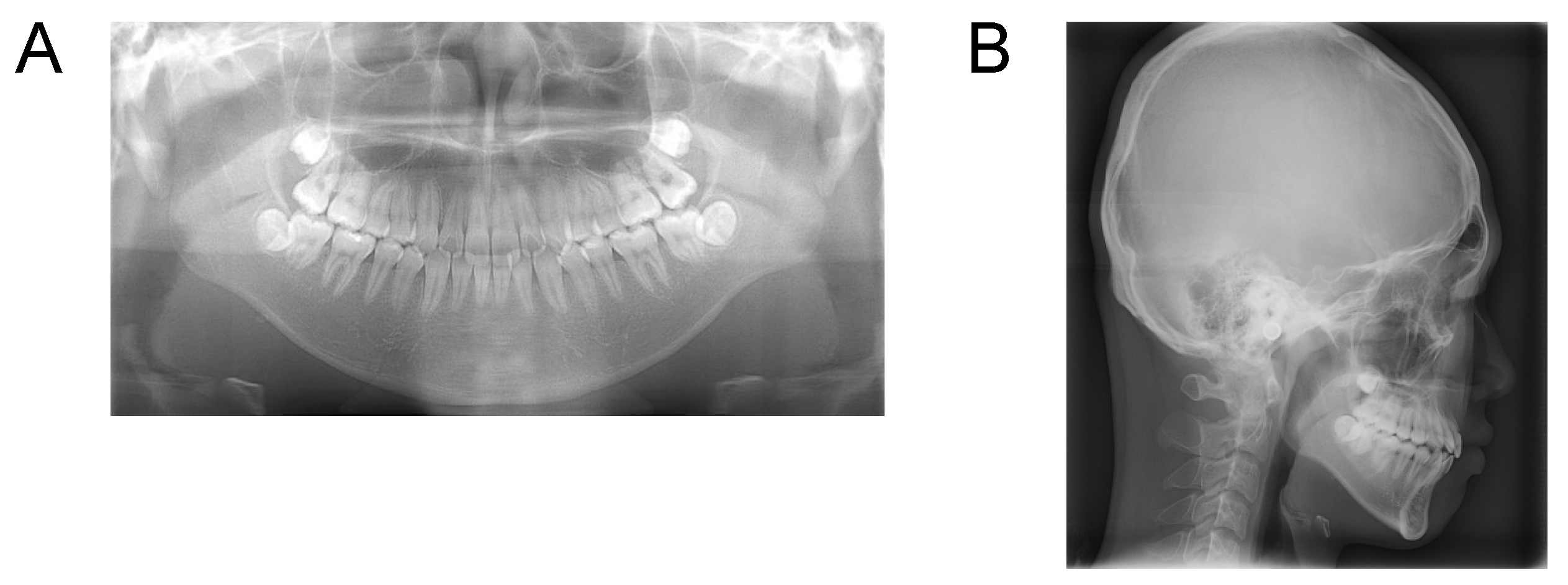
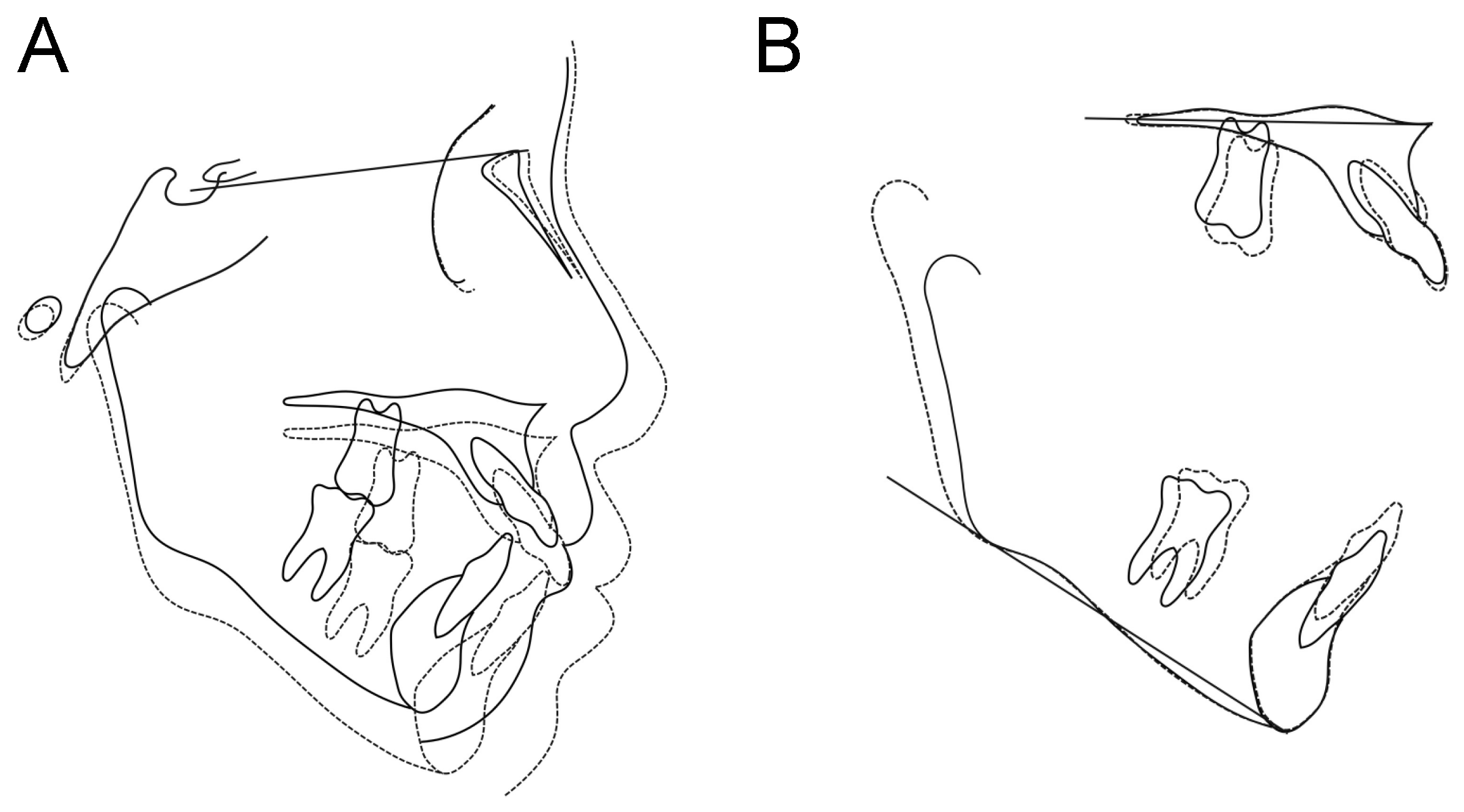
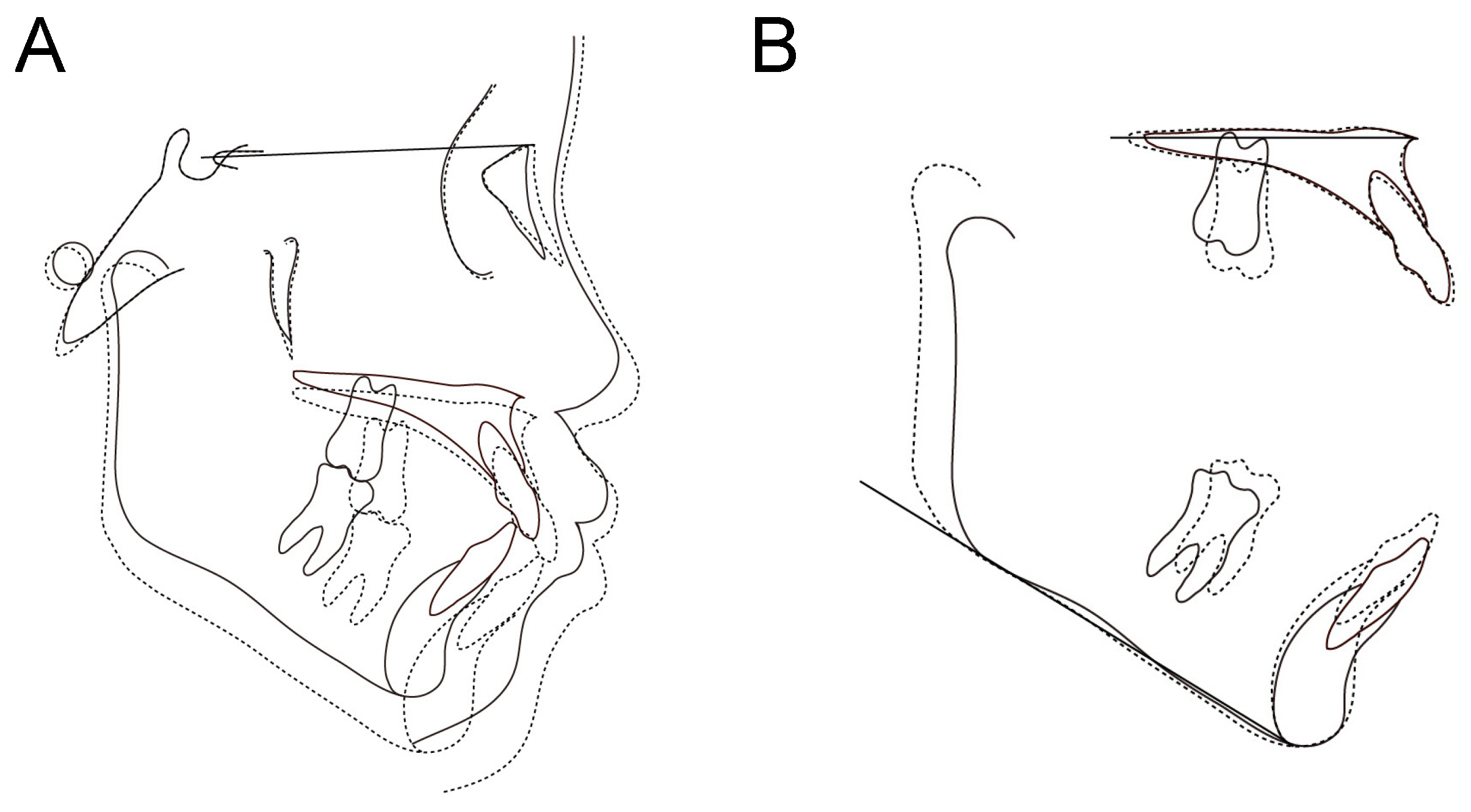
Case 1. Findings from initial examination
Case 2. Findings from initial examination
Case 3. Findings from initial examination
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kokich, V.O.; Kokich, V.G.; Kiyak, H.A. Perceptions of dental professionals and laypersons to altered dental esthetics: Asymmetric and symmetric situations. Am. J. Orthod. Dentofacial. Orthop. 2006, 130, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics; Mosby Year Book: St. Louis, MO, USA, 2007. [Google Scholar]
- Hunt, O.; Johnston, C.; Hepper, P.; Burden, D.; Stevenson, M. The influence of maxillary gingival exposure on dental attractiveness ratings. Eur. J. Orthod. 2002, 24, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Robbins, J.W. Differential diagnosis and treatment of excess gingival display. Pract. Periodontontics Aesthet. Dent. 1999, 11, 265–272. [Google Scholar]
- Silberberg, N.; Goldstein, M.; Smidt, A. Excessive gingival display—Etiology, diagnosis, and treatment modalities. Quintessence Int. 2009, 40, 809–818. [Google Scholar] [PubMed]
- Monaco, A.; Streni, O.; Marci, M.C.; Marzo, G.; Gatto, R.; Giannoni, M. Gummy smile: Clinical parameters useful for diagnosis and therapeutical approach. J. Clin. Pediatr. Dent. 2005, 29, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Evian, C.I.; Cutler, S.A.; Rosenberg, E.S.; Shah, R.K. Altered passive eruption: The undiagnosed entity. J. Am. Dent. Assoc. 1993, 124, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.A.; McGuire, M. The diagnosis and treatment of the gummy smile. Compend. Contin. Educ. Dent. 1997, 18, 757–762. [Google Scholar]
- Ohnishi, H.; Yagi, T.; Yasuda, Y.; Takata, K. A mini-implant for orthodontic anchorage in a deep overbite case. Angle Orthod. 2005, 75, 444–452. [Google Scholar] [CrossRef]
- Lin, J.C.Y.; Yeh, C.L.; Liou, E.J.W.; Bowman, S.J. Treatment of skeletal-origin gummy smiles with miniscrew anchorage. J. Clin. Orthod. 2008, 42, 285–296. [Google Scholar]
- Kokich, V. Esthetic and anterior tooth position: An orthodontic perspective. Part II: Vertical position. J. Esthet. Restor. Dent. 1993, 5, 200–207. [Google Scholar] [CrossRef]
- Peck, S.; Peck, L.; Kataja, M. The gingival smile line. Angle Orthod. 1992, 62, 92–100. [Google Scholar] [CrossRef]
- Kim, T.W.; Kim, H.; Lee, S.J. Correction of deep overbite and gummy smile by using a mini-implant with a segmented wire in a growing Class II Division 2 patient. Am. J. Orthod. Dentofacial Orthop. 2006, 130, 676–685. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.W.; Freitas, B.V. Orthodontic treatment of gummy smile by using mini-implants (part I): Treatment of vertical growth of upper anterior dentoalveolar complex. Dental Press J. Orthod. 2010, 15, 42.e1–42.e9. [Google Scholar] [CrossRef]
- Miyazawa, K.; Sakai, N.; Tsutsui, T.; Tabuchi, M.; Goto, S. The simplified bite jumping appliance: An improved functional appliance. Orthod. Waves 2015, 74, 18–21. [Google Scholar] [CrossRef]
- Sander, F.G.; Lassak, C. The modification of growth with the Jumping-the-Bite plate compared to other functional orthodontic appliances. J. Orofac. Orthop. 1990, 51, 155–164. [Google Scholar] [CrossRef]
- Martina, R.; Cioffi, I.; Galeotti, A.; Tagliaferri, R.; Cimino, R.; Michelotti, A.; Valletta, R.; Farella, M.; Paduano, S. Efficacy of the Sander bite-jumping appliance in growing patients with mandibular retrusion: A randomized controlled trial. Orthod. Craniofacial Res. 2013, 16, 116–126. [Google Scholar] [CrossRef]
- Sakamoto, T.; Miura, F.; Iizuka, T. Linear Analyses on the Developmental Changes of Dentofacial Complex of Japanese by Means of Roentgenographic. Cephalometry. J. Stomatol. Soc. 1963, 30, 169–182. [Google Scholar] [CrossRef]
- Bergman, R.T.; Waschak, J.; Borzabadi-Farahani, A.; Murphy, N.C. Longitudinal study of cephalometric soft tissue profile traits between the ages of 6 and 18 years. Angle Orthod. 2014, 84, 48–55. [Google Scholar] [CrossRef]
- Burstone, C.J. Deep overbite correction by intrusion. Am. J. Orthod. 1977, 72, 1–22. [Google Scholar] [CrossRef]
- Janzen, E.K. A balanced smile—A most important treatment objective. Am. J. Orthod. 1977, 72, 359–372. [Google Scholar] [CrossRef]
- Deguchi, T.; Murakami, T.; Kuroda, S.; Yabuuchi, T.; Kamioka, H.; Takano-Yamamoto, T. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J-hook headgear. Am. J. Orthod. Dentofacial Orthop. 2008, 133, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Burhan, A.S.; Nawaya, F.R. Dentoskeletal effects of the Bite-Jumping Appliance and the Twin-Block Appliance in the treatment of skeletal Class II malocclusion: A randomized controlled trial. Eur. J. Orthod. 2015, 37, 330–337. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sakai, N.; Miyazawa, K.; Tsutsui, T.; Tabuchi, M.; Shibata, M.; Goto, S. Comparative study of the treatment effects off bionator and bite jumping appliances on Cllass II malocclusions. Orthod. Waves 2016, 75, 1–9. [Google Scholar] [CrossRef]
- Van Diepenbeek, A.F.; Buschang, P.H.; Prahl-Andersen, B. Age-dependant cephalometric standards as determined by multilevel modeling. Am. J. Orthod. Dentofacial Orthop. 2009, 135, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Motoyoshi, M.; Matsuoka, M.; Shimizu, N. Application of orthodontic miniimplants in adolescents. Int. J. Oral Maxillofac. Surg. 2007, 36, 695–699. [Google Scholar] [CrossRef] [PubMed]










| Pre-Treatment | Post SBJA + High-Pull Headgear | |
|---|---|---|
| (10 y 7 m) | (14 y 4 m) | |
| Measurements (°) | Value | Value |
| SNA | 85.0 | 85.0 |
| SNB | 78.5 | 80.5 |
| ANB | 6.5 | 4.5 |
| FMA | 30.5 | 30.5 |
| U-1 to SN | 103.0 | 103.0 |
| FMIA | 62.0 | 61.0 |
| L-1 to mand.pl. | 87.5 | 88.5 |
| Interincisal Angle | 126.0 | 126.0 |
| SN to Nasal floor | 9.0 | 7.5 |
| Occ.pl.to FH | 19.0 | 11.5 |
| Pre-Treatment | Post SBJA + High-Pull Headgear | |||||
|---|---|---|---|---|---|---|
| (10 y 7 m) | (14 y 4 m) | |||||
| Measurements (mm) | Value | Mean | Deviation | Value | Mean | Deviation |
| N-ANS | 55.0 | 51.5 ± 3.1 | X | 58.0 | 57.0 ± 3.5 | N |
| ANS-Me | 68.5 | 66.2 ± 3.7 | N | 77.5 | 73.0 ± 4.6 | N |
| Is-Is’ | 31.5 | 28.5 ± 2.1 | X | 33.0 | 30.7 ± 2.8 | N |
| Mo-Ms | 17.5 | 19.1 ± 1.7 | N | 25.5 | 23.7 ± 2.2 | N |
| Ii-Ii’ | 42.0 | 41.4 ± 1.5 | N | 47.5 | 46.0 ± 1.9 | N |
| Mo-Mi | 29.0 | 29.9 ± 2.3 | N | 35.5 | 34.1 ± 2.9 | N |
| Wits appraisal | 0.0 | −2.0 | ||||
| N: Within one standard deviation of the mean | ||||||
| X: Outside one standard deviation of the mean | ||||||
| Pre-Treatment | Post SBJA + High-Pull Headgear | |
|---|---|---|
| (10 y 0 m) | (13 y 10 m) | |
| Measurements (°) | Value | Value |
| SNA | 85.0 | 85.0 |
| SNB | 77.0 | 80.0 |
| ANB | 8.0 | 5.0 |
| FMA | 33.5 | 33.5 |
| U-1 to SN | 118.5 | 110.0 |
| FMIA | 53.5 | 53.5 |
| L-1 to mand.pl. | 92.5 | 93.0 |
| Interincisal Angle | 117.0 | 125.0 |
| SN to Nasal floor | 7.0 | 4.0 |
| Occ.pl.to FH | 15.0 | 10.5 |
| Pre-Treatment | Post SBJA + High-Pull Headgear | |||||
|---|---|---|---|---|---|---|
| (10 y 0 m) | (13 y 10 m) | |||||
| Measurements (mm) | Value | Mean | Deviation | Value | Mean | Deviation |
| N-ANS | 55.5 | 51.5 ± 3.1 | X | 58.5 | 57.0 ± 3.5 | N |
| ANS-Me | 66.5 | 66.2 ± 3.7 | N | 71.0 | 73.0 ± 4.6 | N |
| Is-Is’ | 31.0 | 28.5 ± 2.1 | X | 32.5 | 30.7 ± 2.8 | N |
| Mo-Ms | 18.0 | 19.1 ± 1.7 | N | 25.0 | 23.7 ± 2.2 | N |
| Ii-Ii’ | 40.0 | 41.4 ± 1.5 | N | 45.0 | 46.0 ± 1.9 | N |
| Mo-Mi | 28.0 | 29.9 ± 2.3 | N | 31.5 | 34.1 ± 2.9 | N |
| Wits appraisal | 2.0 | −0.5 | ||||
| N: Within one standard deviation of the mean | ||||||
| X: Outside one standard deviation of the mean | ||||||
| Pre-Treatment | Post SBJA + High-Pull Headgear | |
|---|---|---|
| (8 y 10 m) | (13 y 5 m) | |
| Measurements (°) | Value | Value |
| SNA | 84.5 | 84.5 |
| SNB | 78.5 | 80.5 |
| ANB | 6.0 | 4.0 |
| FMA | 26.0 | 26.0 |
| U-1 to SN | 109.0 | 115.5 |
| FMIA | 52.0 | 49.5 |
| L-1 to mand.pl. | 102.0 | 104.5 |
| Interincisal Angle | 116.0 | 107.0 |
| SN to Nasal floor | 8.5 | 7.5 |
| Occ.pl.to FH | 15.5 | 11.0 |
| Pre-Treatment | Post SBJA + High-Pull Headgear | |||||
|---|---|---|---|---|---|---|
| (8 y 10 m) | (13 y 5 m) | |||||
| Measurements (mm) | Value | Mean | Deviation | Value | Mean | Deviation |
| N-ANS | 51.0 | 47.0 ± 2.5 | X | 52.5 | 53.3 ± 2.8 | N |
| ANS-Me | 62.5 | 62.1 ± 2.9 | N | 69.0 | 70.4 ± 3.8 | N |
| Is-Is’ | 29.5 | 26.3 ± 2.1 | X | 30.0 | 30.5 ± 2.1 | N |
| Mo-Ms | 18.5 | 17.3 ± 1.5 | N | 24.0 | 22.6 ± 1.7 | N |
| Ii-Ii’ | 39.0 | 37.8 ± 1.6 | N | 44.0 | 43.2 ± 1.6 | N |
| Mo-Mi | 29.0 | 27.5 ± 1.7 | N | 33.0 | 31.9 ± 2.1 | N |
| Wits appraisal | −0.5 | −1.5 | ||||
| N: Within one standard deviation of the mean | ||||||
| X: Outside one standard deviation of the mean | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, T.; Tabuchi, M.; Kawaguchi, M.; Sekiya, T.; Takahashi, M.; Asaoka, R.; Miyazawa, K.; Goto, S. Gummy Smile Improvement during Growth Period Using a Simple Bite Jumping Appliance and High-Pull J-Hook HeadGear: A Case Series Study. Appl. Sci. 2022, 12, 12268. https://doi.org/10.3390/app122312268
Sato T, Tabuchi M, Kawaguchi M, Sekiya T, Takahashi M, Asaoka R, Miyazawa K, Goto S. Gummy Smile Improvement during Growth Period Using a Simple Bite Jumping Appliance and High-Pull J-Hook HeadGear: A Case Series Study. Applied Sciences. 2022; 12(23):12268. https://doi.org/10.3390/app122312268
Chicago/Turabian StyleSato, Takuma, Masako Tabuchi, Misuzu Kawaguchi, Takeo Sekiya, Mifumi Takahashi, Ryo Asaoka, Ken Miyazawa, and Shigemi Goto. 2022. "Gummy Smile Improvement during Growth Period Using a Simple Bite Jumping Appliance and High-Pull J-Hook HeadGear: A Case Series Study" Applied Sciences 12, no. 23: 12268. https://doi.org/10.3390/app122312268
APA StyleSato, T., Tabuchi, M., Kawaguchi, M., Sekiya, T., Takahashi, M., Asaoka, R., Miyazawa, K., & Goto, S. (2022). Gummy Smile Improvement during Growth Period Using a Simple Bite Jumping Appliance and High-Pull J-Hook HeadGear: A Case Series Study. Applied Sciences, 12(23), 12268. https://doi.org/10.3390/app122312268








