An Orthodontic Treatment Case of a TMD Patient with Maxillary Posterior Intrusion Using TSADs
Abstract
1. Introduction
2. Materials and Methods
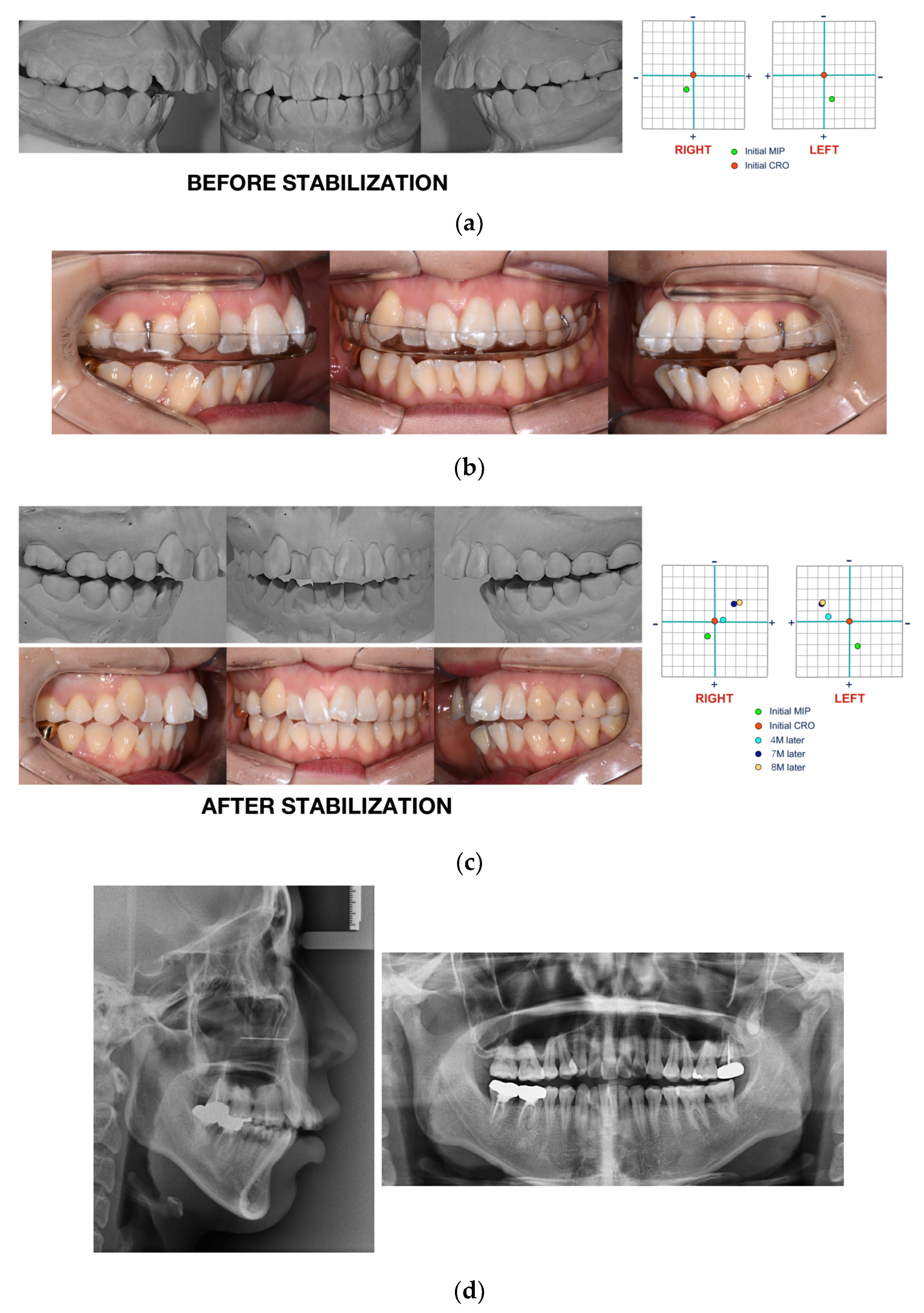
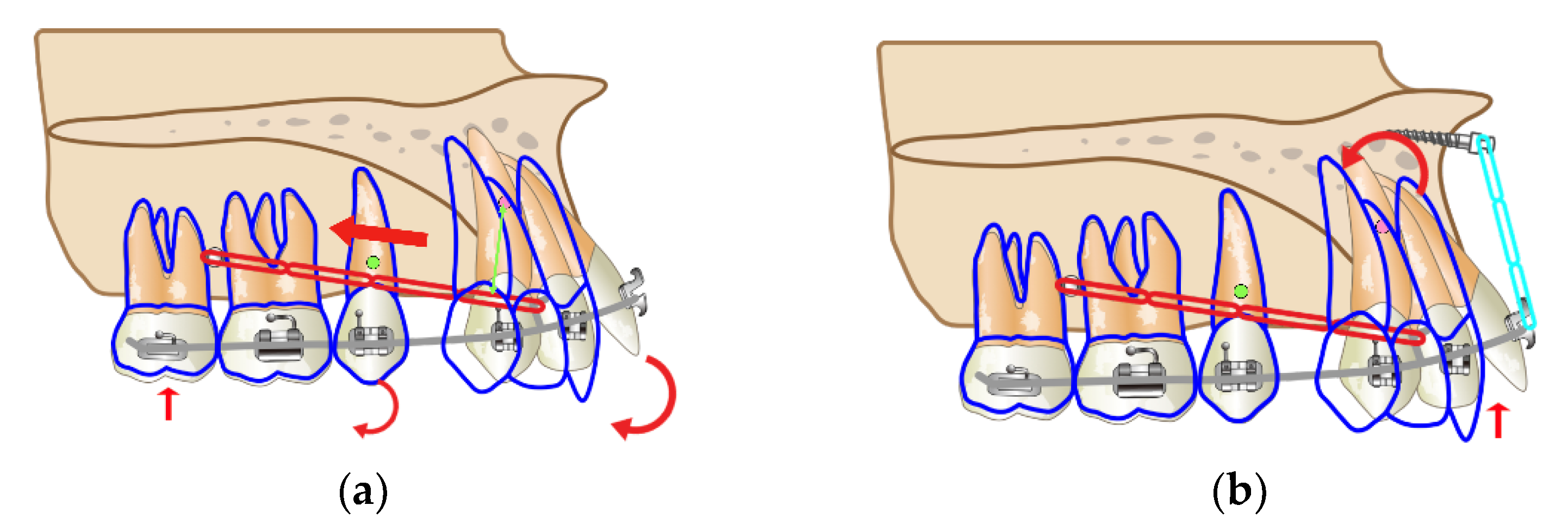
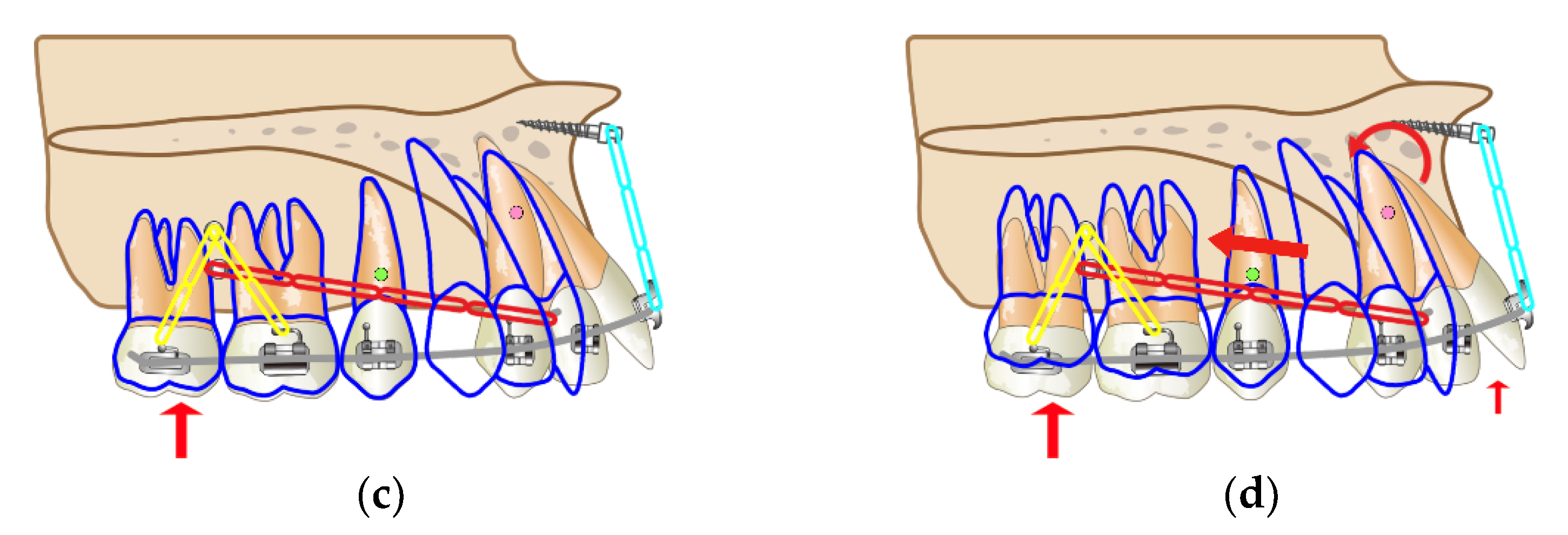
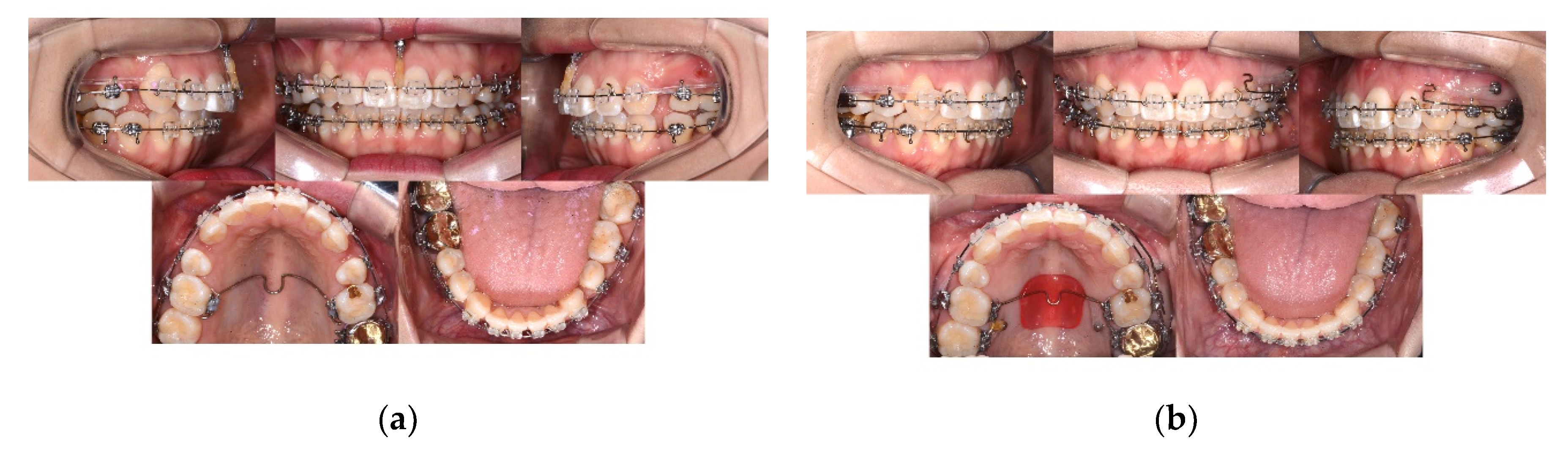
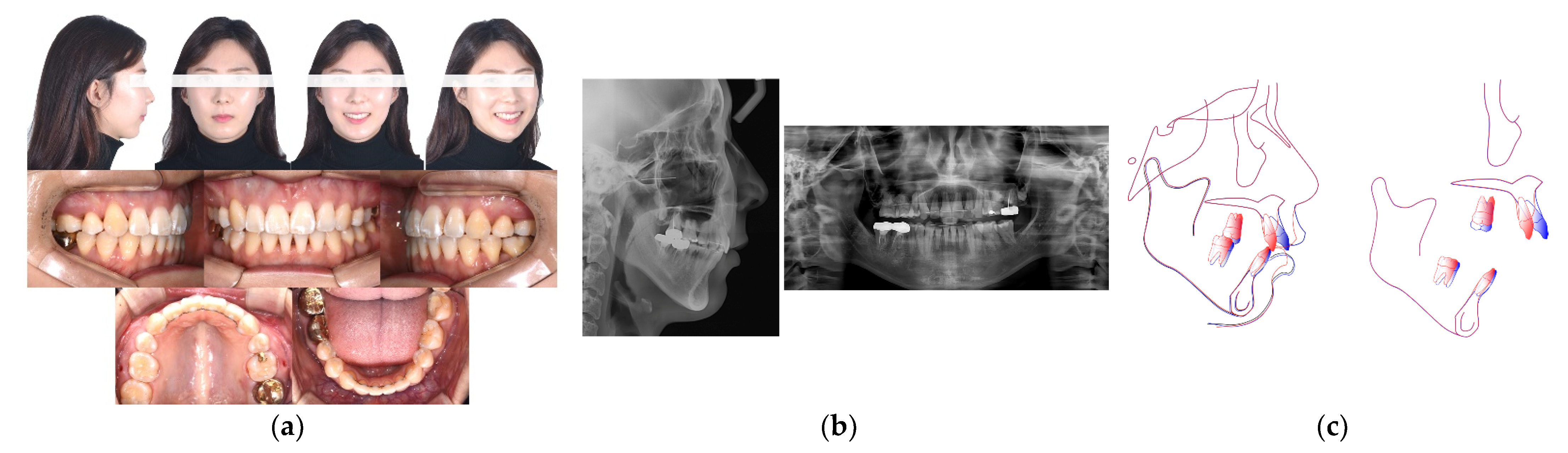
Case Report
3. Discussion
3.1. Importance of Condylar Position
3.2. Considerations for Orthodontic Tooth Movement after Stabilization
4. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, G.H.; Park, J.H.; Moon, D.; Lee, S. Protocols for orthodontic treatment of patients with temporomandibular joint disorders. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Moon, D.; Park, J.H.; Lee, G.H. Orthodontic treatment for a patient with anterior open bite and severe condylar resorption. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 392–407.e2. [Google Scholar] [CrossRef] [PubMed]
- Cordray, F.E. Three dimensional analysis of models articulated in the seated condylar position from a deprogrammed asymptomatic population: A prospective study. Part I. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 619–630. [Google Scholar] [CrossRef] [PubMed]
- Cordray, F.E. Articulated dental cast analysis of asymptomatic and symptomatic populations. Int. J. Oral Sci. 2016, 8, 126–132. [Google Scholar] [CrossRef]
- Lim, W.H.; Choi, B.T.; Lee, J.Y.; Ahn, S.J. Dentofacial characteristics in orthodontic patients with centric relation–maximum intercuspation discrepancy. Angle Orthod. 2014, 84, 939–945. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, S.M.; Moon, D.N.; Lee, G.H. Clinical application of a maximum intercuspal position-centric relation occlusion conversion of a lateral cephalogram in the treatment of orthodontic patients. Am. J. Orthod. Dentofac. Orthop. Clin. Companion 2021, 1, 127–135. [Google Scholar] [CrossRef]
- Espeland, L.; Dowling, P.A.; Mobarak, K.A.; Stenvik, A. Three-year stability of open-bite correction by 1-piece maxillary osteotomy. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 60–66. [Google Scholar] [CrossRef]
- Park, Y.C.; Kim, J.K.; Lee, J.S. Biomechanical considerations with temporary anchorage devices. In Orthodontics: Current Principles and Techniques, 5th ed.; Graber, L.W., Vanasdall, R.L., Jr., Vig, K.W., Eds.; Elsevier/Mosby: St. Louis, MO, USA, 2011; pp. 381–419. [Google Scholar]
- Lee, G.H.; Lee, S.M.; Yoo, S.K.; Park, J.H. Orthodontic treatment of TMD patients with posterior intrusion using TADs. In Temporary Anchorage Devices in Clinical Orthodontics, 1st ed.; Park, J.H., Ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2020; pp. 415–431. [Google Scholar]
- Lee, G.H.; Park, J.H.; Moon, D.; Lee, S.M. Use of temporary skeletal anchorage devices for intrusive root movement of maxillary incisors in adult patients with Class II Division 2 malocclusion. Am. J. Orthod. Dentofac. Orthop. Clin. Companion 2022, 2, 151–165. [Google Scholar] [CrossRef]
- Okeson, J.P. Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future. Am. J. Orthod. Dentofac. Orthop. 2015, 147, S216–S223. [Google Scholar] [CrossRef]
- Okeson, J.P. Chapter 5: Management of Temporomandibular Disorders and Occlusion, 7th ed.; Elsevier/Mosby: St. Louis, MO, USA, 2013; pp. 73–85. [Google Scholar]
- Ferro, K.J.; Morgano, S.M.; Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; Twain, M. The Glossary of Prosthodontic Terms, 9th ed. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar]
- Dawson, P.E. A classification system for occlusions that relates maximal intercuspation to the position and condition of the TM joints. J. Prosthet. Dent. 1996, 75, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Crawford, S.D. The relationship between condylar axis position as determined by the occlusion and measured by the CPI instrument and signs and symptoms of TM joint dysfunction. Angle Orthod. 1999, 69, 103–115. [Google Scholar] [PubMed]
- Karl, P.J.; Foley, T.F. The use of a deprogramming appliance to obtain centric relation records. Angle Orthod. 1999, 69, 117–125. [Google Scholar] [PubMed]
- Capp, N.J.; Clayton, J.A. A technic for evaluation of centric relation tooth contacts: Part II: Following use of an occlusal splint for treatment of TMJ dysfunction. J. Prosthet. Dent. 1985, 54, 697–705. [Google Scholar] [CrossRef] [PubMed]
- Mahan, P.E.; Wilkinson, T.M.; Gibbs, C.H.; Mauderli, A.; Brannon, L.S. Superior and inferior bellies of the lateral pterygoid muscle EMG activity at basic jaw positions. J. Prosthet. Dent. 1983, 50, 710–718. [Google Scholar] [CrossRef]
- Ramfjord, S.P. Dysfunctional temporomandibular joint and muscle pain. J. Prosthet. Dent. 1961, 11, 353–374. [Google Scholar] [CrossRef]
- Bakke, M.; Moller, E. Distortion of maximum elevator activity by unilateral tooth contact. Scand. J. Dent. Res. 1980, 88, 67–75. [Google Scholar]
- Riise, C.; Sheikholeslam, A. The influence of experimental interfering occlusal contacts on the postural activity of the anterior temporal and masseter muscles in young adults. J. Oral Rehabil. 1982, 9, 419–425. [Google Scholar] [CrossRef]
- Williamson, E.H.; Lundquist, D.O. Anterior guidance: Its effect on electromyographic activity of the temporal and masseter muscles. J. Prosthet. Dent. 1983, 49, 816–823. [Google Scholar] [CrossRef]
- Hannam, A.G.; DeCow, R.E.; Scott, J.D.; Wood, W.W. The relationship between dental occlusion, muscle activity and associated jaw movement in man. Arch. Oral Biol. 1977, 22, 25–32. [Google Scholar] [CrossRef]
- Girardot, R.A. The nature of condylar displacement in patients with temporomandibular pain-dysfunction. Orthod. Rev. 1987, 1, 16–23. [Google Scholar] [PubMed]
- Slavicek, R.J. Clinical and instrumental functional analysis for diagnosis and treatment planning, Part IV: Instrumental analysis of mandibular casts using the mandibular position indicator. J. Clin. Orthod. 1988, 22, 566–575. [Google Scholar] [PubMed]
- Hicks, S.T.; Wood, D.P. Recording condylar movement with two face-bow systems. Angle Orthod. 1996, 66, 293–300. [Google Scholar] [PubMed]
- Lavine, D.; Kulbersh, R.; Bonner, P.; Pink, F.E. Reproducibility of the Condylar Position Indicator. Semin. Orthod. 2003, 9, 96–101. [Google Scholar] [CrossRef]
- Wassell, R.W. Do Occlusal factors play a part in temporomandibular dysfunction? J. Dent. 1989, 17, 101–110. [Google Scholar] [CrossRef]
- Greene, C.S.; Laskin, D.M. Splint therapy for the myofascial pain-dysfunction (MPD) syndrome: A comparative study. J. Am. Dent. Assoc. 1972, 84, 624–628. [Google Scholar] [CrossRef]
- Clark, G.T. A critical evaluation of orthopedic interocclusal appliance therapy: Design, theory, and overall effectiveness. J. Am. Dent. Assoc. 1984, 108, 359–364. [Google Scholar] [CrossRef]
- Sarver, D.M.; Janyavula, S.; Cron, R.Q. Condylar degeneration and diseases, local and systemic etiologies. Semin. Orthod. 2013, 19, 89–96. [Google Scholar] [CrossRef]
- Choi, B.T.; Baik, S.H. Effect of anterior guidance change on the condylar path in skeletal Class I young adult women using a splint with flat or steep anterior guidance. J. Korean Dent. Sci. 2012, 5, 29–36. [Google Scholar] [CrossRef]
- Ekberg, E.C.; Vallon, D.; Nilner, M. Occlusal appliance therapy in patients with temporomandibular disorders. A double-blind controlled study in a short-term perspective. Acta Odontol. Scand. 1998, 56, 122–128. [Google Scholar] [CrossRef]
- Dylina, T.J. A common-sense approach to splint therapy. J. Prosthet. Dent. 2001, 86, 539–545. [Google Scholar] [CrossRef]
- Dawson, P.E. Occlusal splints. In Functional Occlusion: From TMJ to Smile Design, 1st ed.; Mosby: St. Louis, MO, USA, 2007; pp. 69–73. [Google Scholar]
- Okeson, J.P. Chapter 13: Management of Temporomandibular Disorders and Occlusion, 7th ed.; Elsevier/Mosby: St. Louis, MO, USA, 2013; p. 358. [Google Scholar]
- Lundh, H.; Westesson, P.L.; Kopp, S.; Tillstrom, B. Anterior repositioning splint in the treatment of temporomandibular joints with reciprocal clicking: Comparison with a flat occlusal splint and an untreated control group. Oral Surg. Oral Med. Oral Pathol. 1985, 60, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.H.; Evans, D.L.; Barton, W.A.; Williams, B.H. The effect of biteplane use on terminal hinge axis location. Angle Orthod. 1977, 47, 25–33. [Google Scholar] [PubMed]
- Roth, R.H. Gnathologic considerations for orthodontic therapy editor. In Science and Practice of Occlusion, 1st ed.; Charles, M., Ed.; Quintessence Publishing: Chicago, IL, USA, 1997; pp. 502–514. [Google Scholar]
- Scheerlinck, J.P.; Stoelinga, P.J.; Blijdorp, P.A. Sagittal split advancement osteotomies stabilized with miniplates. 2-5 Years follow-up. Int. J. Oral Maxillofac. Surg. 1994, 23, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Arnett, G.W.; Tamborello, J.A.; Rathbone, J.A. Temporomandibular joint ramifications of orthognathic surgery. In Modem Practice in Orthognathic and Reconstructive Surgery, 1st ed.; Bell, W.H., Ed.; WB Saunders: Philadelphia, PA, USA, 1992; pp. 523–593. [Google Scholar]
- Hoppenreijs, T.J.; Freihofer, H.P.; Stoelinga, P.J.; Tuinzing, D.B.; van’t Hof, M.A. Condylar remodeling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite. A clinical and radiological study. Int. J. Oral Maxillofac. Surg. 1998, 27, 81–91. [Google Scholar]
- Zachrisson, B.U. Esthetic factors involved in anterior tooth display and the smile: Vertical dimension. J. Clin. Orthod. 1998, 32, 432–445. [Google Scholar]
- Sabri, R. The eight components of a balanced smile. J. Clin. Orthod. 2005, 39, 155–167. [Google Scholar]
- McHorris, W.H. Occlusion with particular emphasis on the functional and parafunctional role of anterior teeth. Part 2. J. Clin. Orthod. 1979, 13, 684–701. [Google Scholar]
- Ahn, S.J.; Baek, S.H.; Kim, T.W.; Nahm, D.S. Discrimination of internal derangement of temporomandibular joint by lateral cephalometric analysis. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 331–339. [Google Scholar] [CrossRef]
- Mackley, R.J. An evaluation of smiles before and after orthodontic treatment. Angle Orthod. 1993, 63, 183–189. [Google Scholar]
- Choi, B.; Baek, S.H.; Yang, W.S.; Kim, S. Assessment of the relationships among posture, maxillomandibular denture complex, and soft- tissue profile of aesthetic adult Korean women. J. Craniofac. Surg. 2000, 11, 586–594. [Google Scholar] [CrossRef]
- Gurbanov, V.; Bas, B.; Oz, A. Evaluation of stresses on temporomandibular joint in the use of Class II and III orthodontic elastics: A three-dimensional finite element study. J. Oral Maxillofac. Surg. 2020, 78, 705–716. [Google Scholar] [CrossRef]
- Park, Y.C.; Lee, H.A.; Choi, N.C.; Kim, D.H. Open bite correction by intrusion of posterior teeth with miniscrews. Angle Orthod. 2008, 78, 699–710. [Google Scholar] [CrossRef]
- Scheffler, N.R.; Proffit, W.R.; Phillips, C. Outcomes and stability in patients with anterior open bite and long anterior face height treated with temporary anchorage devices and a maxillary intrusion splint. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 594–602. [Google Scholar] [CrossRef]
- Arriola-Guillen, L.E.; Flores-Mir, C. Molar heights and incisor inclinations in adults with Class II and Class III skeletal open-bite malocclusions. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 325–332. [Google Scholar] [CrossRef]
- Baek, E.S.; Hwang, S.; Kim, K.H.; Chung, C.J. Total intrusion and distalization of the maxillary arch to improve smile esthetics. Korean J. Orthod. 2017, 47, 59–73. [Google Scholar] [CrossRef]
- Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; Takano-Yamamoto, T. Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 599–605. [Google Scholar] [CrossRef]
- Deguchi, T.; Kurosaka, H.; Oikawa, H.; Kuroda, S.; Takahashi, I.; Yamashiro, T.; Takano-Yamamoto, T. Comparison of orthodontic treatment outcomes in adults with skeletal open bite between conventional edgewise treatment and implant-anchored orthodontics. Am. J. Orthod. Dentofac. Orthop. 2011, 139, S60–S68. [Google Scholar] [CrossRef]
- Park, H.S.; Kwon, T.G.; Kwon, O.W. Treatment of open bite with micro-screw implant anchorage. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 627–636. [Google Scholar] [CrossRef]
- Kuroda, S.; Katayama, A.; Takano-Yamamoto, T. Severe anterior open-bite case treated using titanium screw anchorage. Angle Orthod. 2004, 74, 558–567. [Google Scholar]
- Kuroda, S.; Sugawara, Y.; Tamamura, N.; Takano-Yamamoto, T. Anterior open bite with temporomandibular disorder treated with titanium screw anchorage: Evaluation of morphological and functional improvement. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 550–560. [Google Scholar] [CrossRef] [PubMed]

| Measurement | Korean Norm | Pretreatment | Post-stabilization | Posttreatment |
|---|---|---|---|---|
| SNA (°) | 81.5 | 83.0 | 83.0 | 81.5 |
| SNB (°) | 79.0 | 71.5 | 70.5 | 72.0 |
| ANB (°) | 2.5 | 11.5 | 12.5 | 8.5 |
| Saddle Angle (°) | 123.0 | 122.0 | 120.5 | 121.0 |
| Articular Angle (°) | 149.0 | 167.0 | 169.0 | 168.5 |
| Gonial Angle (°) | 121.0 | 119.0 | 119.0 | 119.0 |
| SUM (°) | 393.0 | 408.0 | 408.5 | 408.5 |
| Anterior Cranial Base Length (mm) | 71.0 | 65.3 | 65.3 | 65.3 |
| Posterior Cranial Base Length (mm) | 33.0 | 36.0 | 35.0 | 35.0 |
| Mandibular Body Length (mm) | 71.0 | 72.0 | 72.0 | 72.0 |
| Ramus Height (mm) | 44.0 | 39.6 | 40.5 | 40.5 |
| ACB: MBL | 1:1 | 1:1.1 | 1:1.1 | 1:1.1 |
| PCB: Ramus Height | 3:4 | 3:3.3 | 3:3.5 | 3:3.5 |
| Post.FH/Ant.FH (%) | 66.8 | 58.0 | 57.3 | 57.3 |
| SN-MP (°) | 33.5 | 48.0 | 50.0 | 49.0 |
| TVL to MxOP (°) | 100.0 | 95.0 | 95.0 | 101.5 |
| U1-FH (°) | 116.6 | 115.0 | 115.0 | 100.0 |
| IMPA (°) | 90.0 | 90.0 | 90.0 | 92.0 |
| U1 to Stms (mm) | 3.0 | 3.9 | 3.9 | 3.0 |
| U1/L1 (°) | 124.0 | 99.0 | 95.0 | 119.0 |
| Overjet (mm) | 2.8 | 11.5 | 11.5 | 3.0 |
| Overbite (mm) | 3.0 | 0.5 | 0.0 | 2.8 |
| Upper lip (mm) | 0.0 | 4.3 | 3.8 | 0.0 |
| Lower lip (mm) | 0.0 | 5.9 | 5.0 | 0.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, G.-H.; Park, J.H.; Lee, S.-M.; Kim, E.-J.; Lim, S.-W.; Moon, D. An Orthodontic Treatment Case of a TMD Patient with Maxillary Posterior Intrusion Using TSADs. Appl. Sci. 2022, 12, 12098. https://doi.org/10.3390/app122312098
Lee G-H, Park JH, Lee S-M, Kim E-J, Lim S-W, Moon D. An Orthodontic Treatment Case of a TMD Patient with Maxillary Posterior Intrusion Using TSADs. Applied Sciences. 2022; 12(23):12098. https://doi.org/10.3390/app122312098
Chicago/Turabian StyleLee, Gye-Hyeong, Jae Hyun Park, Sang-Mi Lee, Eun-Jeong Kim, Seung-Weon Lim, and Danal Moon. 2022. "An Orthodontic Treatment Case of a TMD Patient with Maxillary Posterior Intrusion Using TSADs" Applied Sciences 12, no. 23: 12098. https://doi.org/10.3390/app122312098
APA StyleLee, G.-H., Park, J. H., Lee, S.-M., Kim, E.-J., Lim, S.-W., & Moon, D. (2022). An Orthodontic Treatment Case of a TMD Patient with Maxillary Posterior Intrusion Using TSADs. Applied Sciences, 12(23), 12098. https://doi.org/10.3390/app122312098







