Abstract
Introduction: An altered dental occlusion can also affect balance stability or mobility. Thus, the aim of this study was to examine whether wearing a mandibular splint, which retains the occlusion close to the centric occlusion, can increase or decrease balance stability and the range of motion (ROM) of the cervical spine as opposed to the habitual occlusion, and if there is a difference between men and women. Material and methods: In this study, 41 male (34.7 ± 11.4 years) and 50 female subjects (29.3 ± 12.7 years) participated. Cervical spine ROM was recorded using the Zebris CMS 70P system. For balance stability, a pressure measuring platform integrated into the treadmill system (FDM-T) of the company Zebris® Medical GmbH was used. Here, the area of the ellipse and the length of the Center of Pressure (CoP) was recorded whilst in the bipedal and unipedal stance. Results: The sex comparison showed significant differences for the area of the ellipse of the right leg and ROM extension in the habitual occlusion: females showed a better balance stability and a larger ROM extension. When wearing the splint, only the CoP of the left leg was significant with a better balance stability in female subjects. Within the male subjects, the ellipse area in the bipedal and unipedal (left/right) stance showed mostly significant reductions, while the rotation left and right as well as the lateral flexion (left/right) improved when wearing the splint. Female subjects, when wearing the splint, showed a significant decrease of the ellipse area and the CoP length when standing on either leg. Flexion, rotation to the right and lateral flexion to the left/right, all increased significantly. Conclusion: Wearing a splint that keeps the jaw close to the centric relation improved balance stability and increased the ROM of the cervical spine for both male and female subjects. Women may have marginally different basic balance stability strategies than men, with regard to bipedal and unipedal standing. Nevertheless, there are scarcely any differences between the two sexes in the adaptation when wearing a splint. Changing the jaw relation in healthy adults can possibly support the release of movement potentials that simplify the performance of everyday activities or sports movements.
1. Introduction
For the performance of any activity, be it leisure, business or sports, it is an advantage to have good coordination and physical condition [1,2,3]. In this context, balance stability is a major coordination skill [4,5]; through balance stability, it is possible to maintain an upright balanced stance while executing movements. Balance stability can be assessed, among other things, by the equal percentage distribution of body weight on the right and left forefoot and rearfoot, but also by the movement of the center of pressure (COP) over time; here, shorter distances correspond to smaller fluctuations. The length of the center of pressure (CoP) [6] as well as the distribution of body weight [6] are two frequently used evaluation parameters as they can be reliably measured and validated [6], and are also repeatable [7]. Here, components such as the vestibular system, the visual system and proprioception must interact together with the skeletal musculature where everything is under the control of the central nervous control [8,9]. As well as maintaining postural balance, the position and the mobility of the cervical spine also play important roles in order to consistently direct the head position and, more precisely, to direct the view to the place of action.
However, increasing evidence has come to light that the changing of the dental occlusion position has a sensorimotor effect on structures located more caudally [10,11,12,13,14]. In particular, the wearing of a splint has been found to harmonize the structures of the temporomandibular system (TMS) leading to a curative balancing effect of possible neuromuscular imbalances [15,16]. By changing the jaw relation via a custom-made splint, the effect may be twofold: an improvement in ventilation can be achieved, and the prevailing dysfunctions in the TMS can be regulated [17,18]. Thus, Garner and Lamira [17] have concluded that the design of the oral appliance causes an effect on the genioglossus; this results in a lowered respiratory rate and ventilation while showing no negative effects on oxygen uptake during exercise. This is also an important factor for athletes performing at a high level [19]. In their systematic review, Ferrillo et al. [20] examined the effects of occlusal splints on spinal posture in patients with temporomandibular disorders (TMD) and concluded that, for these individuals, occlusal splinting might be considered as a non-invasive therapeutic approach. However, they also criticized the low number of high-quality methodologies in the studies and recommended that, in the future, the combination of platform stabilometry and kinematic evaluation should be used to examine the effect of occlusal splints on posture. Thus, Zhang et al. [21] concluded in their review that an occlusal splint can be used as a non-invasive treatment approach for patients with TMD, especially in those individuals with signs and symptoms of mandibular movement limitation and pain. In women with TMD, wearing an occlusal splint has been found to be associated with an improvement in postural balance (sway area and sway length) [22]. Furthermore, postural sway was observed to significantly increase in subjects with TMD compared to healthy subjects when the mandible was in maximum intercuspidation or the dental occlusion was in the rest position [23]. It is also important to consider that cervical spine movements may be limited by factors such as TMD or TMD in combinationwith headache [18]. Since balance stability and cervical mobility represent the basic components of both daily and athletic performance and may also be influenced by the temporomandibular system, as described above, in this study we analyzed the possible influence of two different dental occlusion conditions (habitual occlusion, or wearing a splint) on the aforementioned parameters. However, a gender comparison was also given special consideration in this investigation since different postural balance responses have been observed in other studies [24,25,26].
In our measurements, the habitual occlusal position was contrasted with an occlusal position that was maintained with a splint having an idealized condylar position, close to the centric position. This study design has already been used in a previous study of male athletes [27].
The following hypotheses to be tested were:
- Cervical spine movements differ between men and women wearing a splint.
- The quality of the change in balance stability between habitual occlusion (HO) and wearing a splint (S) differs between men and women.
- Both men and women show decreased balance stability and an increased range of motion (ROM) of the cervical spine as a result of wearing the splint.
2. Material and Methods
2.1. Subjects
All subjects were patients of the Edel and Weiß dental practice in Nuremberg (Germany) and were asked to participate in this prospective cross-sectional study during their routine dental consultation.
In the present study, 91 (41 m/50 f) subjects aged 18 to 68 years (31.7 ± 12.4 years) participated. Of these, 41 were male subjects (34.7 ± 11.4 years) and 50 were female subjects (29.3 ± 12.7 years). The following inclusion criteria applied to this study: all participants were between 18–68 years old and subjectively confirmed as feeling healthy. Thus, they neither suffered from peripheral, central vestibular or somatosensory disorders or from disorders of the vestibular organ, nor had they had injuries to the musculoskeletal system (such as bone fractures or muscle strains) and the temporomandibular system within the last 2 years prior to the study. All subjects took part in recreational sports with a maximal training load of 3x/week, each session lasting approximately 30 to 60 min. The following exclusion criteria were defined: (1) current or chronic musculoskeletal injuries, (2) acute temporomandibular joint disorders, (3) orthodontic or orthopedic treatment at the time of the study, (4) use of muscle relaxants, (5) acute infection and (6) genetic muscle diseases.
A TMD screening form of the German Society for Functional Diagnostics and Therapy (DGFDT) [28] was used in order to exclude such participants with pain in the temporomandibular joint or in the masticatory muscles, or those with temporomandibular joint noises or clicking, occlusion disorders, or limitations in the opening or closing of the mouth.
An approved ethics application from the medical faculty of the Goethe University Frankfurt is available for the conduct of the study (ethics vote no. 331/2011). All procedures were performed in accordance with the relevant guidelines of the declaration of Helsinki. An adequate sample size calculation has been performed for the approved ethics application. The global error probability is set at α = 0.05 and a test power of at least 0.8 is required.
2.2. Measuring Systems
2.2.1. Mobility Measurement of the Cervical Spine
Cervical spine movements were recorded using the Zebris CMS 70P (Zebris® Medical GmbH, Isny im Allgäu, Germany). This system uses the transit time determination of ultrasound pulses and has a measurement rate of 180 Hz and a sampling rate of 20 Hz. Inter-rater reliability and validity can be classified as good to excellent [29]. A special head attachment with integrated triple markers was used to register cervical spine movements. In addition, a reference triple marker was attached to the subject to compensate for upper body movements.
The data obtained in this process were displayed using the associated WinSpine 2.2.x computer program.
2.2.2. Analysis of the Balance Stability
By means of the pressure sensor matrix with 10,240 calibrated capacitive sensors, which were integrated into the treadmill system (FDM-T) of the company Zebris® Medical GmbH (Isny im Allgäu, Germany), the area of the ellipse and the length of the CoP was recorded. The measurement area employed was 170 cm × 65 cm. The measuring frequency was 300 Hz, while the pressure was measured in the measuring unit “Pascal” (force/area unit).
2.3. Splint Production
In order to produce an individually custom-made mandibular splint for each athlete, impressions of the upper (maxillary) and lower (mandibular) jaws were taken from the subjects using alginate (HS-Ortho Alginate, Henry Schein Dental International, Langen, Germany) and casts were made from superhard plaster (HS-Superhard Plaster Natur, Henry Schein DENTAL, Langen, Germany). A cast analysis was performed and each maxilla was articulated according to the Plane System (Plane Finder according to Udo Plaster®, Nuremberg, Germany). The mandible was then articulated in centric relation to the maxilla. The centric bite required for this was taken by each athlete after wearing an Aqualazier for at least 20 min in order to deprogram the neurophysiological system [30,31,32,33,34,35,36,37]. With the aid of a custom-made anterior jig made of millable, autopolymerizing plastic (LuxaBite, DMG Chemisch-Pharmazeutische Fabrik GmbH, Hamburg, Germany) and a suitable material for injecting under the teeth (VPS Hydro Bite, Henry Schein UK, Gillingham, UK), a centric bite registration was performed.
An individual mandibular splint was then fabricated in this determined position of the casts in relation to each other. After reduction of the milled splint, an adhesive (Mollosil, Detax, Ettlingen, Germany) was applied to create a bond between the splint and the Odontosil silicone (Shore hardness 50; Henry Schein DENTAL, Langen, Germany). Using this splint base made of polymethylmetachrylate (PMMA), the surface of the splint was reduced in the milling unit via the software program to such an extent that an approximately 2 mm layer of Odontosil could be applied to the splint base without increasing the registered vertical.
2.4. Examination Procedure
Firstly, all subjects were measured in habitual occlusion (HO) without a splint and then again with the splint (S). There was always a break of at least 15 min between the two measurement conditions. After splint insertion, measurements were started after 20 min to ensure adaptation to the temporary situation by the temporomandibular system. Either the recording of balance stability or the measurement of cervical mobility was made, depending on the outcome of tossing a coin. Prior to data recording, several test measurements of both measurement systems were completed. Both measurement series were repeated three times. The mean value was calculated from each of these measurements.
2.4.1. Cervical Spine Mobility
After fixing the head attachment and upper body reference markers, the subject sat on a chair with an approximately 90° angle between the upper and lower legs in an upright upper body position, with the arms or hands resting evenly on the thighs and the subject’s gaze directed straight ahead at eye level. The settings of the chair were as follows: inclination of the backrest 70°, length of the backrest 45 cm, inclination of the seat 5°, length of the seat 40 cm, height of the seat 45 cm. Before the three movement executions could be recorded, a calibration was performed in a neutral position. A ‘neutral position’ means in a given sitting position with the gaze directed straight ahead, fixing a point at eye level. The bite was either in habitual occlusion or with the splint which was lightly fixed.
Three different directions of the ROM were measured for each of the five repetitions:
- -
- Movement 1: flexion and extension of the cervical spine in the sagittal plane. The head was flexed as far as possible to the chest or extended to the neck without interrupting the movement (5 repetitions).
- -
- Movement 2: axial rotation, i.e., the movement function of the cervical spine in the transversal plane. The head was rotated five times maximally to the left side and to the right side.
- -
- Movement 3: frontal movement function of the cervical spine (lateral flexion). This involved the alternating sideward movement of the head to the right or left shoulder.
2.4.2. Balance Stability
Balance stability was measured barefoot in the bipedal stance and in the unipedal stance, on the left and right leg, respectively. For the bipedal stance, the subject was asked to place the feet hip-width apart in a habitual posture and to focus with the eyes on a point on the wall. The same visual focusing was also employed for the unipedal measurements.
Each measurement was of 10 s duration; the measurement was started and stopped by an acoustic signal. For the data evaluation of the “Center of Pressure” path length (mm) (total length of the CoP path movements to the anterior and posterior) and the ellipse sway area (mm2) (95% confidence ellipse for the mean of the CoP anterior, posterior, medial and lateral coordinates) were included. The shorter the distance covered by the CoP path length and the smaller the confidence ellipse was, the greater was the stance stability [38].
2.5. Statistical Evaluation Procedures
All measurements per condition were repeated three times, which were then averaged for evaluation. In order to evaluate the parameters statistically, the software program BIAS (Version 11.8; Epsilon-Verlag, Darmstadt, Germany) was used. The data were first tested for normal distribution using the Kolmogorov-Smirnov adjustment test. As the collected measurement data were not normally distributed, non-parametric tests, such as the Wilcoxon matched-pairs test to compare the two measurement conditions or the Wilcoxon-Man-Whitney U test to compare the men and women, were used. Subsequently, the data were subjected to Bonferroni-Holm correction. The significance level was 5%.
3. Results
3.1. Sex Comparison in Habitual Occlusion and Splint Wearing
The comparison between men and women (Table 1, Figure 1 and Figure 2) showed significant differences in habitual occlusion for the area of the ellipse while standing on the right leg (p ≥ 0.001; Ø♂: 695.50 mm2; Ø♀: 478.00 mm2) and the ROM in cervical extension (p ≥ 0.001; Ø♂: 58°; Ø♀: 62°). All other parameters of both the balance control and cervical spine movements were not significant.

Table 1.
Median, 1st and 3rd quartiles of all parameters for men and women. A comparison between men and women in the habitual occlusal position (HO) and the splint (S) condition. Significant p-values are marked in bold following Bonferroni-Holm correction.
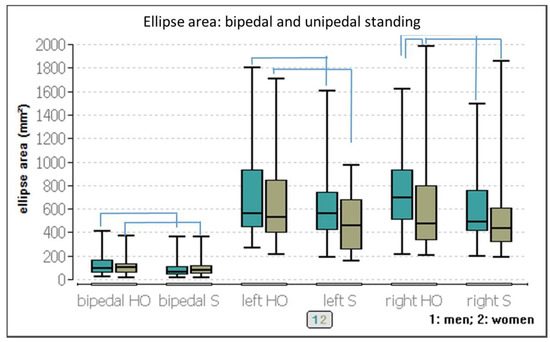
Figure 1.
Ellipse of CoP while bipedal and unipedal standing (left/right leg) with either habitual occlusion or splint, separated into male and female subjects.
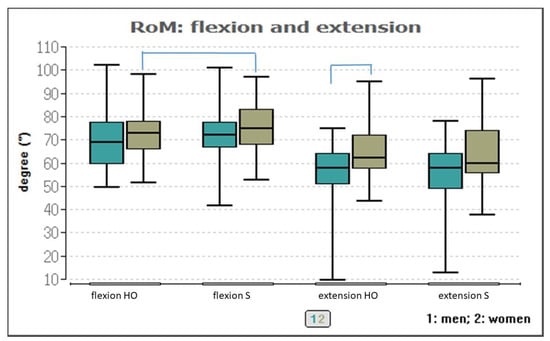
Figure 2.
Range of cervical motion with either habitual occlusion or splint, separated into male and female subjects.
Apart from the CoP length when standing on the left leg (p ≤ 0.01; Ø♂: 366.5 mm2; Ø♀: 292.0 mm2), all other parameters were non-significant in the sex comparison when wearing the splint (Table 1, Figure 3). For the cervical ROM, it can be seen that the male subjects had approximately 74.5 mm more anterior-posterior CoP sway on the left-legged single leg stance than the women.
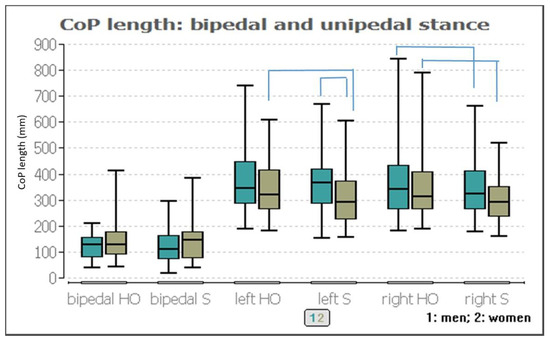
Figure 3.
Center of pressure length with either habitual occlusion or splint, separated into male and female subjects.
3.2. Condition Comparison Per Sex
Both conditions (HO and S) were compared within one sex (Table 2).

Table 2.
Median, 1st and 3rd quartiles of all parameters for men and women. A comparison between the habitual occlusal position (HO) and the splint (S) condition for both men and women. Significant p-values are marked in bold following Bonferroni-Holm correction.
Men: While the ellipse areas when in the bipedal stance and unipedal right-legged stance (p ≤ 0.01 and p ≤ 0.001, respectively, Figure 1) showed significant reductions when wearing the splint, the ellipse areas while standing on the left leg (p ≤ 0.04) showed a significant increase. The reduction of the sway area was much stronger for the right unipedal stance (approximately 202 mm2) than for the bipedal stance (approximately 31 mm2). In contrast, the ellipse area was 4 mm larger in the left-legged stance when wearing the splint. However, this reduction of the ellipse area significantly affected the length of the right-legged stance CoP (approximately 19 mm2), although it did not significantly affect the bipedal and left-legged stance (Figure 4).
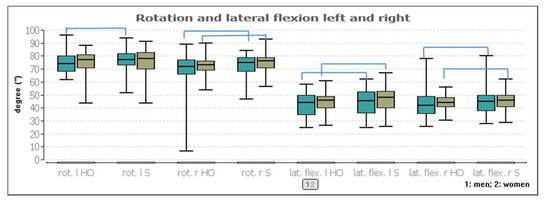
Figure 4.
Rotation and lateral flexion to the left and right body side with either habitual occlusion or splint, separated into male and female subjects.
With respect to cervical spine movements, rotation as well as lateral flexion to the left and right improved marginally by up to 3° by wearing the splint (p ≤ 0.001 and p ≤ 0.01, respectively, Figure 3).
Women: Women showed a significant improvement when wearing the splint while in the right- or left-legged stance (p ≤ 0.001 and 0.04, respectively, Figure 1). Wearing the splint reduced the area of the left ellipse by approximately 70 mm2 and by about 45 mm2 in the right- legged stance. These reductions were also visible in the CoP length, with 29 mm for the left leg and 20 mm for the right leg (Figure 3).
3.3. Quality of the Change between the Conditions
Finally, the extent or quality of the change between the two occlusion positions was considered by calculating the difference of the two measurement conditions per sex which were compared afterwards (Table 3). For balance stability, there was no significance observed. For the cervical spine ROM, significant ROM flexion, right rotation and lateral flexion to the left and right could be observed (p ≤ 0.001).

Table 3.
Differences between habitual occlusion and splint (median, 1st and 3rd quartiles) of all parameters for men and women as well as the p-value of the comparison between the men and women. Significant p-values are marked in bold following Bonferroni-Holm correction.
4. Discussion
The aim of this study was to identify possible differences in the balance stability and cervical ROM between men and women with respect to their reaction on wearing a splint. Descriptive differentiation characteristics for both occlusal conditions could be recognized. While the men had a slightly smaller ellipse area and length of CoP in the bipedal stance, the women performed better in the single-legged stance (whether on the right or left leg). The ROM in all three planes of the cervical spine was higher in women by up to 4° (Table 1, Figure 2 and Figure 4). In the habitual occlusion condition (HO), the women had a significantly greater cervical spine extension with a median difference of 4° and a significantly better balance stability (217 mm2).
However, only the CoP length for the right-legged single leg stance was significantly lower (75.5 mm) in women than in men when wearing a splint (S). There were no evident differences with regard to cervical spine movements, therefore, Hypothesis 1 must be falsified. Why only three parameters were found to be significant in the gender comparison (HO and S) should be investigated in more detail in further studies. This was also confirmed by the extent or quality of the change (difference of HO and S) in balance stability, thus, Hypothesis 2 can also be falsified.
Hypothesis 3 contains the evaluation of the comparison of the two measurement conditions (HO) and (S) per sex. Most of the men and women showed an increased ROM of the cervical spine and a reduced ellipse area at the same length of the CoP due to wearing the splint, although there were sex-specific differences. In men, lateral flexion to the left and right as well as rotation to the left and right increased when wearing the splint. Similarly, the unipedal and bipedal stance stability on the left and right leg improved significantly according to the ellipse area. In women, cervical spine rotation to the right, lateral flexion to the left and right, and flexion increased when wearing the splint. In contrast to the men, only the unipedal stance stability on the right and left leg improved in the women. Consequently, Hypothesis 3 can be verified.
In addition, almost all other parameters showed the same small improvements when wearing the splint, however, these were not significant. Moreover, due to the majority of right-sided dominance, the factor of the dominant leg side did not seem to have a major influence, although this should be investigated more explicitly in further studies.
The improvement of the cervical ROM could be attributed to the fact that the splint causes a different position of the mandible in the temporomandibular joint than is originally the case [39]. Furthermore, it can be assumed that the actual mandibular advancement is correlated to changes in the mechanical properties of the upper airways, resulting in an improvement of their stability and a reduction of their collapsibility. Consequently, this would also affect the position of the cervical spine which may be reflected in improvements in the ROM. Since there was an increase in ROM in the present case, the splint seems to keep the jaw in a better relation than is the case with HO. Due to the small magnitude of the cervical spine ROM, these improvements should be considered as a tendency rather than a clinical relevance.
Furthermore, since the balance stability (CoP area) improved but the length of the CoP reduced less markedly, the CoP apparently moves within a smaller ellipse area. Accordingly, in order to reach the same length within a smaller area for the same measurement time, the frequency of the fluctuations must have been increased. Whether or not this is a habitual pattern when fluctuations reduce, the reason for this potential change as well as its (long-term) effects should be investigated in further studies. Another fact to be investigated further in the future is that women have poorer balance stability when in the bipedal stance (ellipse area and CoP length), but are much more stable when in the single-legged stance in both occlusion conditions than men.
Muscularly-induced shifts in equilibrium compensate for anterior and posterior deviations of the body’s center of gravity through regulation of the “upper ankle strategy” and for frontal deviations through regulation of the “hip strategy” [40]. In accordance with Debrunner [40], the assumption results that the musculature of the lower extremity compensates differently in men and women. It is, thus, possible that men and women use different strategies in maintaining their balance stability; this would then also support the present results as well as other studies [24,25,26]. It is notable that Sell et al. [24] proved that female soldiers had significantly better static postural stability. These authors also found sex-specific differences in balance stability. Ingel et al. [25] also showed that women have better postural stability than men. They also pointed out that the complex nature of postural stability should be further investigated. For these investigations, all systems of postural stability maintenance, such as visual, somatosensory and vestibular systems, should be included as either one or a combination of these systems may be inherently different between the sexes or contribute to the observed differences in postural stability.
The reduction of the sway area and the resulting improvement of stance stability by wearing the splint, which places the occlusion in centric-like jaw relation, were also confirmed by Kim et al. [38]. Oliveira et al. [41] have also proved the influence of a splint by demonstrating a significant increase in the anterior-posterior speed of the CoP in TMD patients.
The improved ROM of the cervical spine in the present study contrasts with that of adolescent dancers analyzed by Klemm [42]. Here, Klemm [42] could not detect any changes in cervical mobility by means of a temporarily generated occlusion block. Furthermore, De Giorgi et al. [43] could not prove any influence of wearing a splint for a period of six months on the cervical spine position in women with TMD. However, a divergent subject collective (women, TMD and no athletes) as well as other measurement systems have to be considered here.
Consequently, it would be interesting to analyze in a follow-up study whether changes in balance and movement of the cervical spine are due to changes in the mechanical properties of the upper airway and, thus, still a lowered respiratory rate and ventilation.
Thus, it becomes clear that the analysis of the use of splints is not only the subject of scientific research in the field of sports, but also in rehabilitation, such as in the therapy of CMD or Pediatric Obstructive Sleep Apnea Syndrome. The possible treatment goals of a centric relation occlusal splint in case of rehabilitation are stabilization of the orofacial system; improvement and relief of temporomandibular dysfunctions, such as temporomandibular joint clicking and muscular pain, abnormal loading of the condyle and bilaminar zone. A good functional pre-treatment with a splint is also crucial for forensic reasons before large extensive restorations and tooth replacements.
The study also has limitations which are indicated in the following.
Likewise, only ad-hoc effects have been presented in the current cross-sectional study where the subjects wore the splint, for the first time, 20 min before the measurement. Whether these can still be preserved within a longitudinal study cannot be answered in the present study and, so, this would be desirable to investigate in future studies. Another limitation of this study is the fact that the measurements were taken while standing and not while moving. Whether the improvements of wearing a splint found here can also be positively demonstrated during the performance of daily or sport-related activities remains unclear, however, it could potentially be a very important factor, especially in competitive sports. Furthermore, the effect of wearing a splint on unathletic people or patients with TMD using the same study design has not been investigated. In addition, correlation calculations between the cervical spine movements and balance stability do not appear to be appropriate because the cervical spine movements were measured while sitting and the balance stability was measured while standing. Furthermore, the effect of past (sports) injuries were not considered. Past unilateral injuries, for example, to the lower extremity, could potentially result in compensatory mechanisms that may affect balance stability. Therefore, recovered past injuries should also be considered in future studies. Here, it should be examined whether these possibly affect either the postural control or movement motor control, or both sequentially, and if they can extend their effects beyond one body area [44].
Accordingly, it remains to be stated that the present results suggest that wearing a splint could possibly be beneficial for injury prevention as one would potentially have better cervical spine movement and increased balance stability, although the neurophysiological mechanisms underlying these results should be further investigated. Furthermore, available findings have shown that noteworthy negative effects do not occur with the parameters analyzed here.
5. Conclusions
In summary, it can be concluded that for both men and women, the wearing of a splint that keeps the jaw close to the centric relation improves their balance stability and increases the ROM of the cervical spine. Women may have marginally different basic balance stability strategies than men with regard to bipedal and unipedal standing. At the same time, there were barely any differences between the two sexes in adaptation when wearing a splint. Thus, changing the jaw relation in men and women can possibly favor and support movement potentials.
Author Contributions
Investigation, F.G. and J.H.; Resources, C.M.-G.; Formal analysis, F.G., J.H., C.M.-G. and D.O.; Writing review & editing, G.O., F.H., D.A.G., F.G. and D.O.; Project admin-istration, D.O.; Writing original draft, F.G. and D.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The APC was funded by MDPI.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by Ethics Committee of the medical faculty of the Goethe University Frankfurt (No. 331/2011).
Informed Consent Statement
All participants signed an informed consent to take part in the study in advance.
Data Availability Statement
All relevant data are within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| ROM | Range of motion |
| TMD | Temporomandibular disorder |
| CoP | Center of pressure |
References
- Wanke, E.M.; Schreiter, J.; Groneberg, D.A.; Weisser, B. Muscular imbalances and balance capability in dance. J. Occup. Med. Toxicol. 2018, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wanke, E.M.; Gabrys, L.; Leslie-Spinks, J.; Ohlendorf, D.; Groneberg, D.A. Functional muscle asymmetries and laterality in Latin American formation dancers. J. Back Musculoskelet. Rehabil. 2018, 31, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Wanke, E.M.; Mill, H.; Arendt, M.; Wanke, A.; Koch, F.; Groneberg, D.A. Occupational accidents in professional dancers with regard to different professional dance styles. Work 2014, 49, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Hrysomallis, C. Balance Ability and Athletic Performance. Sports Med. 2011, 41, 221–232. [Google Scholar] [CrossRef] [PubMed]
- Saleh AAl Attar, W.; Faude, O.; Husain, M.A.; Soomro, N.; Sanders, R.H. Combining the Copenhagen Adduction Exercise and Nordic Hamstring Exercise Improves Dynamic Balance Among Male Athletes: A Randomized Controlled Trial. Sports Health 2021, 13, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Amaricai, E.; Onofrei, R.R.; Suciu, O.; Marcauteanu, C.; Stoica, E.T.; Negruțiu, M.L.; David, V.L.; Sinescu, C. Do different dental conditions influence the static plantar pressure and stabilometry in young adults? PLoS ONE 2020, 15, e0228816. [Google Scholar] [CrossRef]
- Forsman, P.; Haeggström, E.; Wallin, A.; Toppila, E.; Pyykkö, I. Daytime Changes in Postural Stability and Repeatability of Posturographic Measurements. J. Occup. Environ. Med. 2007, 49, 591–596. [Google Scholar] [CrossRef]
- Schiebler, T.H.; Korf, H.W. Anatomie: Histologie, Entwicklungsgeschichte, Makroskopische und Mikroskopische Anatomie, Topographie; Steinkopff: Heidelberg, Germany, 2007. [Google Scholar]
- Schünke, M. Topografie und Funktion des Bewegungssystems: Funktionelle Anatomie; Thieme: Stuttgart, Germany, 2014. [Google Scholar]
- Manni, E.; Palmieri, G.; Marini, R.; Pettorossi, V.E. Trigeminal influences on extensor muscles of the neck. Exp. Neurol. 1975, 47, 330–342. [Google Scholar] [CrossRef]
- Maurer, C.; Heller, S.; Sure, J.-J.; Fuchs, D.; Mickel, C.; Wanke, E.M.; Groneberg, D.A.; Ohlendorf, D. Strength improvements through occlusal splints? The effects of different lower jaw positions on maximal isometric force production and performance in different jumping types. PLoS ONE 2018, 13, e0193540. [Google Scholar] [CrossRef]
- Maurer, C.; Holzgreve, F.; Erbe, C.; Wanke, E.; Kopp, S.; Groneberg, D.; Ohlendorf, D. Influence of dental occlusion conditions on plantar pressure distribution during standing and walking—A gender perspective. Med. Eng. Phys. 2021, 88, 47–53. [Google Scholar] [CrossRef]
- Michelotti, A.; Buonocore, G.; Manzo, P.; Pellegrino, G.; Farella, M. Dental occlusion and posture: An overview. Prog. Orthod. 2011, 12, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Melvin, M.; Sylvia, M.; Udo, W.; Helmut, S.; Paletta, J.R.; Adrian, S. Reproducibility of rasterstereography for kyphotic and lordotic angles, trunk length, and trunk inclination: A reliability study. Spine 2010, 35, 1353–1358. [Google Scholar] [CrossRef] [PubMed]
- Leroux, E.; Leroux, S.; Maton, F.; Ravalec, X.; Sorel, O. Influence of dental occlusion on the athletic performance of young elite rowers: A pilot study. Clinics 2018, 73, e453. [Google Scholar] [CrossRef] [PubMed]
- Grosdent, S.; O’Thanh, R.; Domken, O.; Lamy, M.; Croisier, J.L. Dental Occlusion Influences Knee Muscular Performances in Asymptomatic Females. J. Strength Cond. Res. 2014, 28, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Garner, D.P.; Lamira, J. Respiratory outcomes with the use of a lower custom fit genioglossal-effecting oral appliance. Clin. Exp. Dent. Res. 2019, 6, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Grondin, F.; Hall, T.; Ella, B.; Laurentoye, M.; Laurentjoye, M. Upper cervical range of motion is impaired in patients with temporomandibular disorders. Cranio® 2014, 33, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Baldini, A.; Cravino, G. Occlusione dentale e prestazione sportiva: Revisione della letteratura. Mondo Ortodon. 2011, 36, 131–141. [Google Scholar] [CrossRef]
- Ferrillo, M.; Marotta, N.; Giudice, A.; Calafiore, D.; Curci, C.; Fortunato, L.; Ammendolia, A.; de Sire, A. Effects of Occlusal Splints on Spinal Posture in Patients with Temporomandibular Disorders: A Systematic Review. Healthcare 2022, 10, 739. [Google Scholar] [CrossRef]
- Zhang, S.-H.; He, K.-X.; Lin, C.-J.; Liu, X.-D.; Wu, L.; Chen, J.; Rausch-Fan, X. Efficacy of occlusal splints in the treatment of temporomandibular disorders: A systematic review of randomized controlled trials. Acta Odontol. Scand. 2020, 78, 580–589. [Google Scholar] [CrossRef]
- Hobeiche, J.; el Zoghbi, A.; Halimi, M.; Haddad, C. Effect of Occlusal Splints on Posture Balance in Patients with Temporomandibular Joint Disorder: A Prospective Study. J. Contemp. Dent. Pract. 2021, 22, 615–619. [Google Scholar] [CrossRef]
- Nota, A.; Tecco, S.; Ehsani, S.; Padulo, J.; Baldini, A. Postural stability in subjects with temporomandibular disorders and healthy controls: A comparative assessment. J. Electromyogr. Kinesiol. 2017, 37, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Sell, T.C.; Lovalekar, M.T.; Nagai, T.; Wirt, M.D.; Abt, J.P.; Lephart, S.M. Gender Differences in Static and Dynamic Postural Stability of Soldiers in the Army’s 101st Airborne Division (Air Assault). J. Sport Rehabil. 2018, 27, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Ingel, N.; Vice, V.; Dommer, C.; Csonka, J.; Moore, T.; Zaleski, A.; Killelea, C.; Faherty, M.; Feld, J.; Sell, T. Examining Sex Differences in Visual Reliance During Postural Control in Intercollegiate Athletes. Int. J. Sports Phys. Ther. 2021, 16, 1273–1277. [Google Scholar] [CrossRef] [PubMed]
- Nakhostin-Ansari, A.; Naghshtabrizi, N.; Naghdi, S.; Ghafouri, M.; Khalifeloo, M.; Mohammadzadeh, M.; Vezvaei, P.; Ansari, N.N. Normative values of functional reach test, single-leg stance test, and timed “UP and GO” with and without dual-task in healthy Iranian adults: A cross-sectional study. Ann. Med. Surg. 2022, 80, 104053. [Google Scholar] [CrossRef]
- Herzog, J.; Göttfert, F.; Maurer-Grubinger, C.; Holzgreve, F.; Oremek, G.; Groneberg, D.A.; Ohlendorf, D. Improvement of cervical spine mobility and stance stability by wearing a custom-made mandibular splint in male recreational athletes. PLoS ONE 2022. accepted for publication. [Google Scholar]
- Deutsche Gesellschaft für Funktionsdiagnostik und -Therapie in der Zahn-, Mund und Kieferheilkunde. Richtlinien und Formulare. Available online: https://www.dgfdt.de/richtlinien_formulare (accessed on 17 August 2022).
- Smolenski, U.C.; Endres, G.; Bocker, B. Untersuchung der Halswirbelsäulenbeweglichkeit mittels Bewegungsfunktionsanalysesystemzebris und Winkelmessung. Man. Med. 2003, 41, 365–373. [Google Scholar] [CrossRef]
- Azarbal, M. Comparison of Myo-Monitor centric position to centric relation and centric occlusion. J. Prosthet. Dent. 1977, 38, 331–337. [Google Scholar] [CrossRef]
- Dawson, P.E. Evaluation, Diagnosis, and Treatment of Occlusal Problems; Mosby: Maryland Heights, MO, USA, 1989. [Google Scholar]
- Dawson, P.E. Optimum TMJ condyle position in clinical practice. Int. J. Periodontics Restor. Dent. 1985, 5, 10–31. [Google Scholar]
- Dawson, P.E. A classification system for occlusions that relates maximal intercuspation to the position and condition of the temporomandibular joints. J. Prosthet. Dent. 1996, 75, 60–66. [Google Scholar] [CrossRef]
- Gelb, H. The optimum temporomandibular joint condyle position in clinical practice. Int. J. Periodontics Restor. Dent. 1985, 5, 34–61. [Google Scholar]
- Long, J.H. Locating centric relation with a leaf gauge. J. Prosthet. Dent. 1973, 29, 608–610. [Google Scholar] [CrossRef]
- Lucia, V.O. A technique for recording cen-tric relation. J. Prosthet. Dent. 1964, 14, 492–505. [Google Scholar] [CrossRef]
- McNeill, C. The optimum temporomandibular joint condyle position in clinical practice. Int. J. Periodontics Restor. Dent. 1985, 5, 52–76. [Google Scholar]
- Kim, K.J.; Lučarević, J.; Bennett, C.; Gaunaurd, I.; Gailey, R.; Agrawal, V. Testing the assumption of normality in body sway area calculations during unipedal stance tests with an inertial sensor. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 2016, 4987–4990. [Google Scholar]
- Kamal, A.T.; Fida, M. Evaluation of cervical spine posture after functional therapy with twin-block appliances: A retrospective cohort study. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 656–661. [Google Scholar] [CrossRef]
- Debrunner, H.U. Biomechanik des Fußes; Ferdinand Enke Verlag: Stuttgart, Germany, 1998. [Google Scholar]
- Oliveira, S.S.I.; Pannuti, C.M.; Paranhos, K.S.; Tanganeli, J.P.C.; Laganá, D.C.; Sesma, N.; Duarte, M.; Frigerio, M.L.M.A.; Cho, S. Effect of occlusal splint and therapeutic exercises on postural balance of patients with signs and symptoms of temporomandibular disorder. Clin. Exp. Dent. Res. 2019, 5, 109–115. [Google Scholar] [CrossRef]
- Klemm, S. Okklusionsstörungen und Beweglichkeit der HWS. Man. Med. 2009, 47, 255–260. [Google Scholar] [CrossRef]
- Ilaria De Giorgi, D.D.; Tommaso Castroflorio, D.D.; Andrea Deregibus, M.D. Does occlusal splint affect posture? A randomized controlled trial. Cranio 2020, 38, 264–272. [Google Scholar] [CrossRef]
- Salzer, S.; Heansel, R.; Rey, J.; Maltry, L.; Holzgreve, F.; Lampe, J.; Wanke, E.M.; Groneberg, D.A.; Ohlendorf, D. Injury Occurrence in Male Handball Players and its Impact on Physical Constitution. Endoscopy 2020, 41, 328–338. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).