Abstract
Background: We investigated the relationship between the mandibular Curve of Spee (COS) and a persisting primary second mandibular molar (ppM2) due to an agenesis of the second mandibular premolar, using a digital software technique. Methods: Digital dental casts were obtained from 200 patients at the Department of Orthodontics in Innsbruck and Vienna, Austria. Patients (age-, gender-, and malocclusion-matched) were equally divided into two groups (n = 100) according to the existence of a ppM2. COS depth, overjet, overbite, and angle-classification were measured digitally using the OnyxCeph3TM (version 3.2.147) software. ANOVA and Kruskal–Wallis tests were used to analyze relationships. For statistical analyses, p < 0.05 was considered as statistically significant, p < 0.01 as highly significant. Results were visualized with box plots and bar charts. Results: The deepest COS was present in patients with a ppM2. Furthermore, a positive correlation was shown between COS depth and angle-class II, between COS depth and age, as well as between COS depth and overbite. No gender differences could be observed. Conclusions: In our study population the COS depth was dependent on whether there is a ppM2 due to an agenesis of a second mandibular premolar or not, as well as on the malocclusion in sagittal direction.
Keywords:
curve of spee; tooth agenesis; persisting primary tooth; orthodontics; overbite; overjet; age; gender 1. Introduction
The Curve of Spee (COS) is a naturally occurring concave mandibular and convex maxillary line (i.e., compensating curve), and should in continuation be directly related to the anterior border of the jaw condyle. It was first described by F. Graf von Spee in 1890 [1].
Today, the COS is an important reference plane for occlusion in the field of Orthodontics; it is defined clinically as a sagittal occlusal line between the incisal edges of permanent mandibular incisors and the buccal cusp tips of the molar teeth [2].
With permanent incisor and mandibular first molar eruption, the COS develops and deepens when the second mandibular molar erupts [3]. Despite the relation to tooth eruption, underlying mechanisms of the curve’s formation and maintenance remain unknown.
With the six keys of occlusion, Andrews [4] stated in 1972 that the presence of a deep COS is associated with post orthodontic treatment relapse, concluding a flat plane as treatment goal in the field of Orthodontics.
The functional significance of the COS consecutively considers importance for maintenance of maximum tooth contacts during mastication [5], and further initiates a protrusive contact of the incisors without tooth interferences in the posterior section [6]. Taken together, a physiological COS is required for an efficient masticatory system [7]. Its proper management is critical for the construction of stable complete dentures, both in Dentistry and Orthodontics [3,4,8]. In complete denture prosthodontics, establishing a COS in harmony with the condylar guidance, incisal guidance, plane of occlusion, and prosthetic tooth cusp height is essential for developing a bilaterally balanced articulation, believed to maintain optimal denture stability [3]. It might also play a role in the success of implant-supported restorations [3,9].
Especially in the field of Orthodontics, the COS is an important diagnostic tool for treatment planning. Since Andrews proposed the flattening of the occlusal plane as a treatment goal, COS levelling is an everyday practice in orthodontic offices. Few studies suggested that levelling the COS leads to a prolonged dental arch, indicating a relationship between arch length and amount of levelling [10,11]. Otherwise, Braun et al. [11] disagreed, considering the lower incisors as an independent segment, which can be intruded for COS levelling without prolonging the dental arch. More recently, Afzal et al. [12] showed that levelling one millimetre of the COS increases mandibular arch length by 0.8 mm. In any case, depth measurement of the COS is a key part of space analysis, needed for every single planning of orthodontic patients [13].
As part of the masticatory system, the COS is likely to change individually with age or due to pathophysiological situations [7,13].
The most prevalent craniofacial malformation in humans is tooth agenesis [14]. Except the third molars, mandibular second premolars and maxillary lateral incisors are most likely to be missing [15]. The prevalence of a missing lower second premolar is about 3% [16,17]. For the second mandibular premolar, a unilateral agenesis was reported to occur more often [17]. Without a normal root resorption, the deciduous teeth may stay up to 40 or 50 years [18]. Hypodontia patients present dentofacial changes, such as a smaller lower anterior face hight [19] and angle-class III tendency [20].
Taking this into consideration, it can be hypothesised that the presence of a persisting primary second mandibular molar (ppM2), due to the agenesis of the second mandibular premolar, has an influence on the COS depth as well.
The understanding of the COS and its consequences for patients’ orthodontic therapy is very important and may lead to individualized treatment planning.
The aim of the study was to compare the depth of the COS between patients with a ppM2 due to an agenesis of the second mandibular premolar and patients with no agenesis. Further, a potential association between COS depth and age, gender, and angle-classification should be disclosed.
The null hypothesis is that the depth of COS does not change, regardless of ppM2, age, gender, or malocclusion.
2. Materials and Methods
This study was designed as a bicentric retrospective archive research in which pre-treatment samples were evaluated. The study was approved by the Ethics Committee of the Medical University Innsbruck, Austria (Studies no. 1136/2021), the Ethics Committee of the Medical University Vienna, Austria (2136/2018), and was conducted in accordance with the Declaration of Helsinki of 1975 as revised in 2013.
Patients’ records were collected at the Departments of Orthodontics in Innsbruck and Vienna, Austria.
Inclusion criteria for the experimental group (n = 100) were agenesis of the second mandibular premolar (unilateral agenesia or bilateral), a ppM2, and a fully erupted dentition. Experimental group included 58 females and 42 males, with a mean age of 18.9 years.
The control group (n = 100) consisted of age-, sex- and malocclusion-matched patients and inclusion criterion was a fully erupted dentition.
Exclusion criteria for both groups were previous orthodontic treatment, craniofacial disorders, syndromes, and agenesis of other teeth except the second mandibular premolar.
The demographic information for the experimental and control group is shown in Table 1.

Table 1.
Descriptive Statistics.
All dental casts were available digitally after intraoral scanning during general diagnostics and were analyzed by one experienced investigator using OnyxCeph3TM (version 3.2.147; Image Instruments, Chemnitz, Germany) software.
To measure the COS depth, a horizontal reference plane was drawn from the mandibular incisor cusp tip to the distobuccal cusp tip of the second molar, and a perpendicular distance was measured from the buccal cusp tip of the second premolar or the buccal cusp tip of the ppM2, respectively (Figure 1). In case of bilateral agenesia, values were averaged.
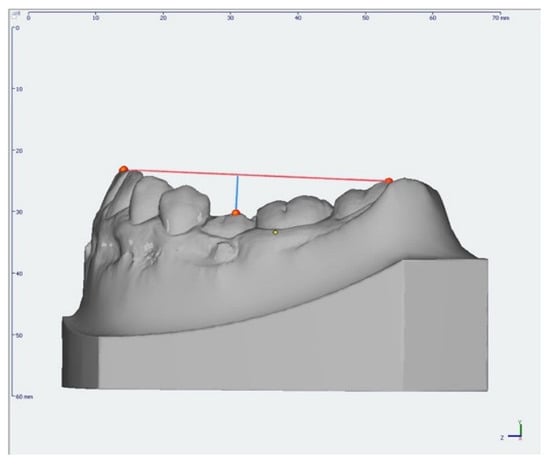
Figure 1.
Digital measurement of the Curve of Spee in a dental arch with a persisting primary second molar.
In addition, dental parameters like overjet (OJ), overbite (OB), and angle-classification were recorded.
Measurements were transferred in an Excel spreadsheet and SPSS (v. 26; IBM SPSS Inc., Armonk, NY, USA) was used for statistical analyses. A Shapiro–Wilk test was used to check for normal distribution and Levene’s test for homogeneity of variance, displaying the variables with means and standard deviation. If variables failed to confirm homogeneity, median and interquartile range were showed. Additionally, method error was evaluated by calculating standard error (SE).
ANOVA and—in case of non-normality—a Kruskal–Wallis Test were used to analyse differences in the COS depths between the dental casts with and without ppM2, regarding sex, age, and angle-class.
Bar charts and boxplots were used to display results. The relationship between age and COS depth was visualized by a scatter blot.
Differences emerging from any of these statistical tests were regarded as significant at p < 0.05, or as highly significant at p < 0.01.
3. Results
3.1. Descriptive Statistics
A total of 200 study models from 116 women and 84 men were included in this study and were equally divided into two groups (n = 100). Groups were sex-, age-, and angle-class-matched. The average age of the patients in the experimental group was 18.9 years and in the control group 19.7 years. In both groups, 25 patients were recorded with angle-class I, 61 with angle-class II, and 14 with angle-class III (Table 1).
3.2. COS Depth in the Experimental and Control Group
Patients with a ppM2 showed a statistically significant deeper COS (p < 0.01; 3.57 mm) in contrast to the control group (Figure 2 and Table 2).
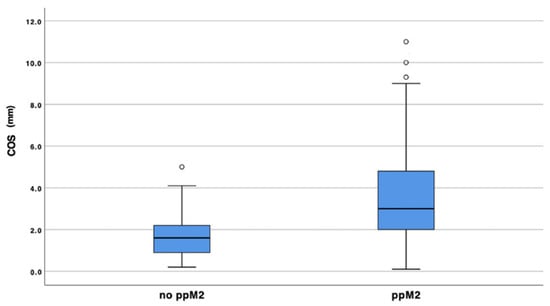
Figure 2.
COS depth experimental versus control group.

Table 2.
COS depth experimental versus control group.
Furthermore, the SD showed higher values in casts with a ppM2 (2.44 mm). In the control group, mean depth of the COS was 1.66 mm with a SD of 0.95 mm. SE values were lower in the control group (Table 2).
3.3. Gender
Comparing the COS between males and females, differences could be observed as not statistically significant with p = 0.68 (Figure 3 and Table 3).
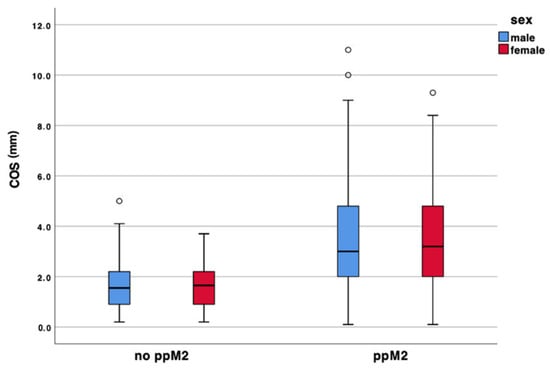
Figure 3.
COS depth and gender.

Table 3.
COS depth and gender.
Regardless of male or female, COS mean depth was deeper in the experimental group with 3.73 mm in men and 3.44 mm in women, respectively. COS mean depth in the control group counted 1.67 mm for males and 1.65 mm for females. Method error showed minor values in the control group (Table 3).
3.4. Age
Figure 4 shows the COS depth depend on age. It can be observed that the COS depth flattened in patients without ppM2 and deepened in patients with a primary tooth in situ.
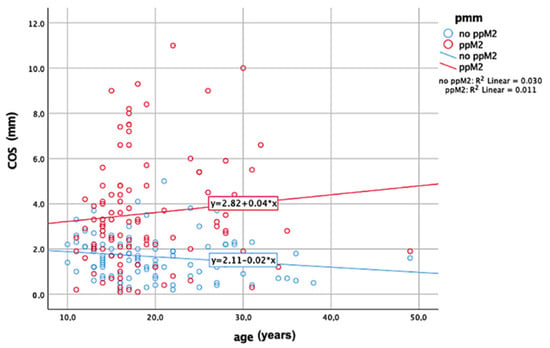
Figure 4.
COS depth depending on age.
No statistical significance (p = 0.8) was determined regarding the relationship between a ppM2 and age (Table 4).

Table 4.
COS depth and age.
3.5. Angle-Classification
Figure 5 shows the COS depth separately for each angle-class (class I, class II, class III). As it can clearly be seen, COS is deeper in the experimental group regardless of the malocclusion. However, analysis of variance showed that there was no statistical significance (p = 0.29) between COS, a ppM2, and angle-class (Table 5).
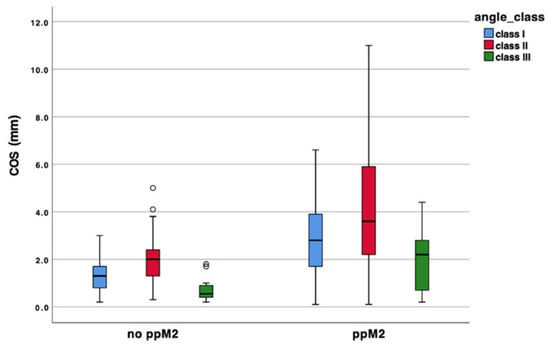
Figure 5.
COS depth and angle-classification.

Table 5.
COS depth and angle-classification in experimental and control group.
Table 5 summarizes the mean values and standard deviations for measurements of the COS for each angle-class. Patients with a class II malocclusion showed the deepest COS (4.24 mm), and patients with a class III malocclusion the lowest (2.03 mm), respectively. Kruskal–Wallis revealed a statistical significance regarding COS depth and each angle-class specifically (class I p < 0.01; class II p < 0.01; class III p < 0.05).
3.6. Overjet
There was no statistically significant dependency (p = 0.17) between a ppM2, angle-class, and OJ (Figure 6 and Table 6).
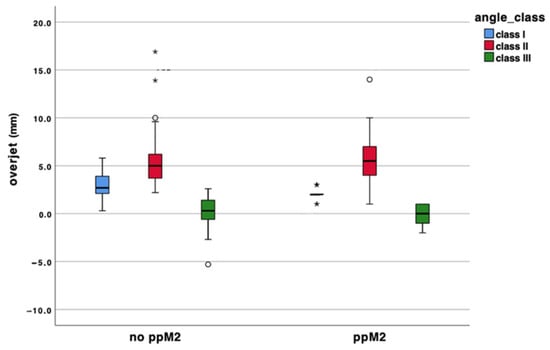
Figure 6.
Relationship between overjet and angle-classification in the experimental and control group.

Table 6.
Overjet in experimental and control group.
Angle-class II showed the biggest OJ in both groups (5.5 mm and 5.33 mm) and angle-class III the lowest (0 mm and 0.3 mm). A statistical significance was shown between OJ and angle-class I (p < 0.05) (Table 6).
3.7. Overbite
Figure 7 shows the relationship between a ppM2, angle-class, and OB in the present study population. ANOVA revealed a statistically significance (p < 0.05). (Table 7).
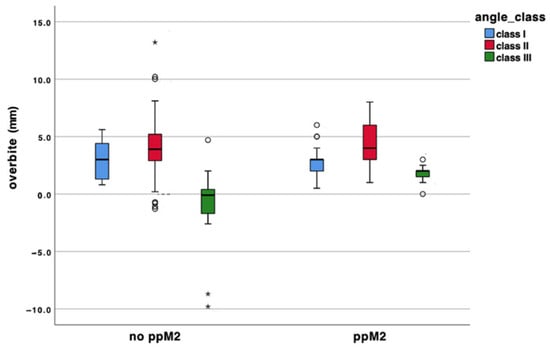
Figure 7.
Relationship between overbite and angle-classification in the experimental and control group.

Table 7.
Overbite in experimental and control group.
Table 7 displays means and SDs, median and IQR of OB measurements for each angle-class. OB values showed a positive correlation with class II in the experimental and in the control group (4 mm and 4.05 mm). General low values for OB can be observed for angle-class III (1.97 mm and −1.18 mm). the conjunction between OB and angle-class III was calculated as highly significant (p < 0.01).
4. Discussion
A stable occlusion with the highest number of required interactions of the masticatory system is the foundation for clinical success. This study was conducted to discover the effects of a persisting primary second mandibular molar on the COS depth, considering that a severe COS is accompanied by a wide range of orthodontic problems, such as a deep bite [21].
As already found in few studies, there was no relevant difference in COS depth between the oral left and right side [3,22,23]. Therefore, in the present study mean values of measurements from both sides were examined for the control group.
Our findings showed that the COS is deepened in the presence of a deciduous tooth (ppM2). Thus, clinicians should keep in mind that neighboring teeth may tip towards the primary tooth in consequence of its lower marginal ridges, which deepens the COS. As the first primary molar is determined as the most affected tooth affected by ankylosis [24], the presence of a deep COS might be the first sign which must be followed in a timely manner to prevent further complications.
Furthermore, patients with tooth agenesis not only show tooth related changes which can be orthodontically treated, but also morphometrical changes in the mandible. Bertl et al. [25] concluded that in consequence of a missing lower second premolar, a reduced mandible length and shape differences might be expected. The study compared the morphology of the mandible between patients with agenesis of the second lower premolar and patients without agenesis. In the treatment of patients with an agenesis, the orthodontist has to deal with a reduced dimension of the mandible due to the absence of sagittal growth. In consequence, the reduced sagittal dimension of the mandible may lead to an increased OJ, though our study collective misses to prove.
As a deep COS may lead to masticatory problems or temporomandibular joint (TMJ) disorders [26,27], professional management of a ppM2 is crucial for dentists, as well as for orthodontists.
Xu et al. [9] reported that the depth of the COS (also obtained by digital methods) was approximately 1.8 mm to 1.9 mm, which is similar to the COS measurements in the control group of the present study (1.6 mm).
According to previous researchers [9,23,28], in our study population there are no significant differences in the COS depth between males and females.
The current study population consisted of patients with fully erupted teeth, as existing literature showed that there is no significant change in the COS depth between adolescence and adults [29,30].
However, in our study population, the COS depth decreased with age in the control group and deepened in patients with agenesis. One possible explanation is that the COS may be pathologically altered in situations resulting from tipping of neighboring teeth when there is no sufficient restauration on the deciduous one. In contrast, a recent study from Karani et al. [31] stated that the depth of the COS is maintained throughout life. However, orthodontists should be aware of individual occlusal adjustments with age, ending in a customized COS. Thus, if this individual COS got changed, the masticatory system and oral health of the patient may get damaged [32].
In our study population, COS is deepest in class II subjects (5.33 mm) and most levelled in class III subjects (0.3 mm), which is in accordance with other studies [13,23,33,34]. This also supports the hypothesis that arch length is associated with the COS depth [10,11], as a class III malocclusion is related to an exceeded lower arch length resulting in an anterior cross bite [35].
Furthermore, measurements of OJ did not show statistically significant dependencies relating to a ppM2 or angle-classification. It might be assumed that COS depth is not an issue when it comes to OJ measuring. Even though there is no statistical significance, OJ increased in class II subjects (5.5 mm) and is lowest in class III individuals (0 mm), leading to an assumption that an increased OJ is related to a deeper COS at least to a minimum. Studies evaluating this topic remain missing.
Further, results showed a highly positive correlation of OB depth, a ppM2, and angle-classification. These results confirmed existing literature, which has stated that an exaggerated OB could be associated with a deep COS [21], which runs hand-in-hand with a ppM2. A deep COS is frequently observed in dental malocclusions with deep OB [3,36,37].
Rozzi et al. [38,39] showed that skeletal vertical parameters influence dental movements during COS levelling. In these studies, it was observed that in brachyfacial patients COS levelling occurred through buccal inclination and intrusion of mandibular incisors, whereas in dolichofacial subjects COS was flattened through extrusion and up righting of mandibular posterior teeth. It was also shown that hypodivergent individuals presented a deeper COS than norm-divergent subjects. To what extend the COS depth is related to this topic should be an issue in future studies.
When discussing the results of the present study, some limitations must be mentioned. As the COS compensates individual craniofacial characteristics, data in relation to the craniofacial structures of the patients are missing. For COS depth measurement lower incisors were included, and as they can be over-erupted, COS depth might be overestimated. Evaluation of longitudinal changes in the depth of COS could give more detailed knowledge about this special topic. Furthermore, radiographic measurements could have been added to model measurements, increasing the study efficiency.
5. Conclusions
In our study population the COS depth is increased in patients with a persisting primary second mandibular molar, in patients with a class II malocclusion, and is positively correlated to a deep overbite. Examining the COS depth should be part of all patient-oriented orthodontic diagnostics, and orthodontists should consider these factors in treatment planning as a moderate COS is key to a stable occlusion and a proper biomechanical function in the past, today, and in the future.
Author Contributions
Conceptualization, A.G.C. and L.S.; methodology, L.S.; software, L.S.; validation, A.G.C. and L.S.; formal analysis, H.U.; investigation, A.G.C.; resources, A.G.C.; data curation, T.K.; writing—original draft preparation, L.S.; writing—review and editing, N.S.-S.; visualization, A.G.C.; supervision, A.G.C.; project administration, M.N.; funding acquisition, A.G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Medical University Innsbruck (studies no. 1136/2021; 2136/2018).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Spee, F.G.; Biedenbach, M.A.; Hotz, M.; Hitchcock, H.P. The Gliding Path of the Mandible along the Skull. J. Am. Dent. Assoc. 1980, 100, 670–675. [Google Scholar] [CrossRef]
- Hitchcock, H.P. The Curve of Spee in Stone Age Man. Am. J. Orthod. 1983, 84, 248–253. [Google Scholar] [CrossRef]
- Marshall, S.D.; Caspersen, M.; Hardinger, R.R.; Franciscus, R.G.; Aquilino, S.A.; Southard, T.E. Development of the Curve of Spee. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Andrews, L.F. The Six Keys to Normal Occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Osborn, J.W. Relationship between the Mandibular Condyle and the Occlusal Plane during Hominid Evolution: Some of Its Effects on Jaw Mechanics. Am. J. Phys. Anthropol. 1987, 73, 193–207. [Google Scholar] [CrossRef] [PubMed]
- De Praeter, J.; Dermaut, L.; Martens, G.; Kuijpers-Jagtman, A.-M. Long-Term Stability of the Leveling of the Curve of Spee. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 266–272. [Google Scholar] [CrossRef]
- Tamizharasi, S.; Senthil Kumar, K. Significance of Curve of Spee: An Orthodontic Review. J. Pharm. Bioallied Sci. 2012, 4, 323. [Google Scholar] [CrossRef]
- Orthlieb, J.-D. The Curve of Spee: Understanding the Sagittal Organization of Mandibular Teeth. CRANIO® 1997, 15, 333–340. [Google Scholar] [CrossRef]
- Xu, H.; Suzuki, T.; Muronoi, M.; Ooya, K. An Evaluation of the Curve of Spee in the Maxilla and Mandible of Human Permanent Healthy Dentitions. J. Prosthet. Dent. 2004, 92, 536–539. [Google Scholar] [CrossRef]
- Baldridge, D.W. Leveling the Curve of Spee: Its Effect on Mandibular Arch Length. JPO J. Pract. Orthod. 1969, 3, 26–41. [Google Scholar]
- Braun, S.; Hnat, W.P.; Johnson, B.E. The Curve of Spee Revisited. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 206–210. [Google Scholar] [CrossRef]
- Afzal, A.; Ahmed, I. Leveling Curve of Spee and Its Effect on Mandibular Arch Length. J. Coll. Physicians Surg. Pak. 2006, 16, 709–711. [Google Scholar]
- Ahmed, I.; Nazir, R.; e-Erum, G.; Ahsan, T. Influence of Malocclusion on the Depth of Curve of Spee. JPMA J. Pak. Med. Assoc. 2011, 61, 1056–1059. [Google Scholar]
- Matalova, E.; Fleischmannova, J.; Sharpe, P.T.; Tucker, A.S. Tooth Agenesis: From Molecular Genetics to Molecular Dentistry. J. Dent. Res. 2008, 87, 617–623. [Google Scholar] [CrossRef]
- Symons, A.L.; Stritzel, F.; Stamation, J. Anomalies Associated with Hypodontia of the Permanent Lateral Incisor and Second Premolar. J. Clin. Pediatr. Dent. 1993, 17, 109–111. [Google Scholar]
- Bergström, K. An Orthopantomographic Study of Hypodontia, Supernumeraries and Other Anomalies in School Children between the Ages of 8-9 Years. An Epidemiological Study. Swed. Dent. J. 1977, 1, 145–157. [Google Scholar]
- Polder, B.J.; Van’t Hof, M.A.; Van der Linden, F.P.G.M.; Kuijpers-Jagtman, A.M. A Meta-Analysis of the Prevalence of Dental Agenesis of Permanent Teeth. Community Dent. Oral Epidemiol. 2004, 32, 217–226. [Google Scholar] [CrossRef]
- Haselden, K.; Hobkirk, J.A.; Goodman, J.K.; Jones, S.P.; Hemmings, K.W. Root Resorption in Retained Deciduous Canine and Molar Teeth without Permanent Successors in Patients with Severe Hypodontia. Int. J. Paediatr. Dent. 2001, 11, 171–178. [Google Scholar] [CrossRef]
- Chung, L.-K.L.; Hobson, R.S.; Nunn, J.H.; Gordon, P.H.; Carter, N.E. An Analysis of the Skeletal Relationships in a Group of Young People with Hypodontia. J. Orthod. 2000, 27, 315–318. [Google Scholar] [CrossRef]
- Øgaard, B.; Krogstad, O. Craniofacial Structure and Soft Tissue Profile in Patients with Severe Hypodontia. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 472–477. [Google Scholar] [CrossRef]
- Al-Zoubi, E.M.; Al-Nimri, K.S. A Comparative Study between the Effect of Reverse Curve of Spee Archwires and Anterior Bite Turbos in the Treatment of Deep Overbite Cases. Angle Orthod 2022, 92, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Sayar, G.; Oktay, H. Department of Orthodontics, Istanbul Medipol University, School of Dentistry, Istanbul, Turkey Assessment of Curve of Spee in Different Malocclusions. Eur. Oral Res. 2019, 52, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Veli, I.; Ozturk, M.A.; Uysal, T. Curve of Spee and Its Relationship to Vertical Eruption of Teeth among Different Malocclusion Groups. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Eşian, D.; Bica, C.I.; Stoica, O.E.; Dako, T.; Vlasa, A.; Bud, E.S.; Salcudean, D.; Beresescu, L. Prevalence and Manifestations of Dental Ankylosis in Primary Molars Using Panoramic X-Rays: A Cross-Sectional Study. Children 2022, 9, 1188. [Google Scholar] [CrossRef] [PubMed]
- Bertl, M.H.; Bertl, K.; Wagner, M.; Gahleitner, A.; Stavropoulos, A.; Ulm, C.; Mitteroecker, P. Second Premolar Agenesis Is Associated with Mandibular Form: A Geometric Morphometric Analysis of Mandibular Cross-Sections. Int. J. Oral Sci. 2016, 8, 254–260. [Google Scholar] [CrossRef]
- Wan, Y.; Bi, M.; Han, H.; Wang, J. A three-dimensional finite element study of the temporomandibular joint with different curve of Spee. Zhonghua Kou Qiang Yi Xue Za Zhi Zhonghua Kouqiang Yixue Zazhi Chin. J. Stomatol. 2012, 47, 277–280. [Google Scholar] [CrossRef]
- Bhateja, N.K.; Fida, M.; Shaikh, A. Deep Bite Malocclusion: Exploration Of The Skeletal And Dental Factors. J. Ayub Med. Coll. 2016, 28, 449–454. [Google Scholar]
- Carter, G.A.; McNamara, J.A. Longitudinal Dental Arch Changes in Adults. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 88–99. [Google Scholar] [CrossRef]
- Bishara, S.E.; Jakobsen, J.R.; Treder, J.E.; Stasl, M.J. Changes in the Maxillary and Mandibular Tooth Size-Arch Length Relationship from Early Adolescence to Early Adulthood. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 46–59. [Google Scholar] [CrossRef]
- Sondhi, A.; Cleall, J.F.; BeGole, E.A. Dimensional Changes in the Dental Arches of Orthodontically Treated Cases. Am. J. Orthod. 1980, 77, 60–74. [Google Scholar] [CrossRef]
- Karani, J.; Idrisi, A.; Mistry, S.; Badwaik, P.; Pai, A.; Yadav, S. Comparative Evaluation of the Depth of Curve of Spee between Individuals with Normal Dentition and Individuals with Occlusal Wear Using Conventional and Digital Software Analysis Techniques: An in Vivo Study. J. Indian Prosthodont. Soc. 2018, 18, 61–67. [Google Scholar] [CrossRef]
- Mohan, M.; D′Souza, M.; Kamath, G.; Parolia, A. Comparative Evaluation of the Curve of Spee in Two Age Groups and Its Relation to Posterior Teeth Disclusion. Indian J. Dent. Res. 2011, 22, 179. [Google Scholar] [CrossRef]
- Shannon, K.R.; Nanda, R.S. Changes in the Curve of Spee with Treatment and at 2 Years Posttreatment. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 589–596. [Google Scholar] [CrossRef]
- de Araújo Paes-Souza, S.; Marañón-Vásquez, G.A.; Galisteu-Luiz, K.; Ferreira, D.M.T.P.; Maia, L.C.; de Cunha Gonçalves Nojima, M. Is There Variation in the Depth of the Curve of Spee in Individuals with Different Dentoskeletal Patterns? A Systematic Review with Meta-Analysis. Eur. J. Orthod. 2022, 44, 491–502. [Google Scholar] [CrossRef]
- Tseng, L.L.Y.; Chang, C.H.; Roberts, W.E. Diagnosis and Conservative Treatment of Skeletal Class III Malocclusion with Anterior Crossbite and Asymmetric Maxillary Crowding. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 555–566. [Google Scholar] [CrossRef]
- Halimi, A.; Benyahia, H.; Azeroual, M.-F.; Bahije, L.; Zaoui, F. Relationship between the Curve of Spee and Craniofacial Variables: A Regression Analysis. Int. Orthod. 2018, 16, 361–373. [Google Scholar] [CrossRef]
- Kumari, N.; Fida, M.; Shaikh, A. Exploration of Variations in Positions of Upper and Lower Incisors, Overjet, Overbite, and Irregularity Index in Orthodontic Patients with Dissimilar Depths of Curve of Spee. J. Ayub Med. Coll. 2016, 28, 766–772. [Google Scholar]
- Rozzi, M.; Mucedero, M.; Pezzuto, C.; Cozza, P. Leveling the Curve of Spee with Continuous Archwire Appliances in Different Vertical Skeletal Patterns: A Retrospective Study. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 758–766. [Google Scholar] [CrossRef]
- Rozzi, M.; Mucedero, M.; Pezzuto, C.; Lione, R.; Cozza, P. Long-Term Stability of Curve of Spee Levelled with Continuous Archwires in Subjects with Different Vertical Patterns: A Retrospective Study. Eur. J. Orthod. 2019, 41, 286–293. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).