Reliability of Polyetherketoneketone as Definitive Implant-Supported Bridges in the Posterior Region—An In Vitro Study of the Ultimate Fracture Load and Vertical Marginal Discrepancy after Artificial Aging
Abstract
1. Introduction
2. Materials and Methods
2.1. Model Construction
2.2. Framework Fabrication
2.3. Veneering of the Frameworks
2.4. Artificial Aging (Thermal Mechanical Cyclic Loading: TMCL)
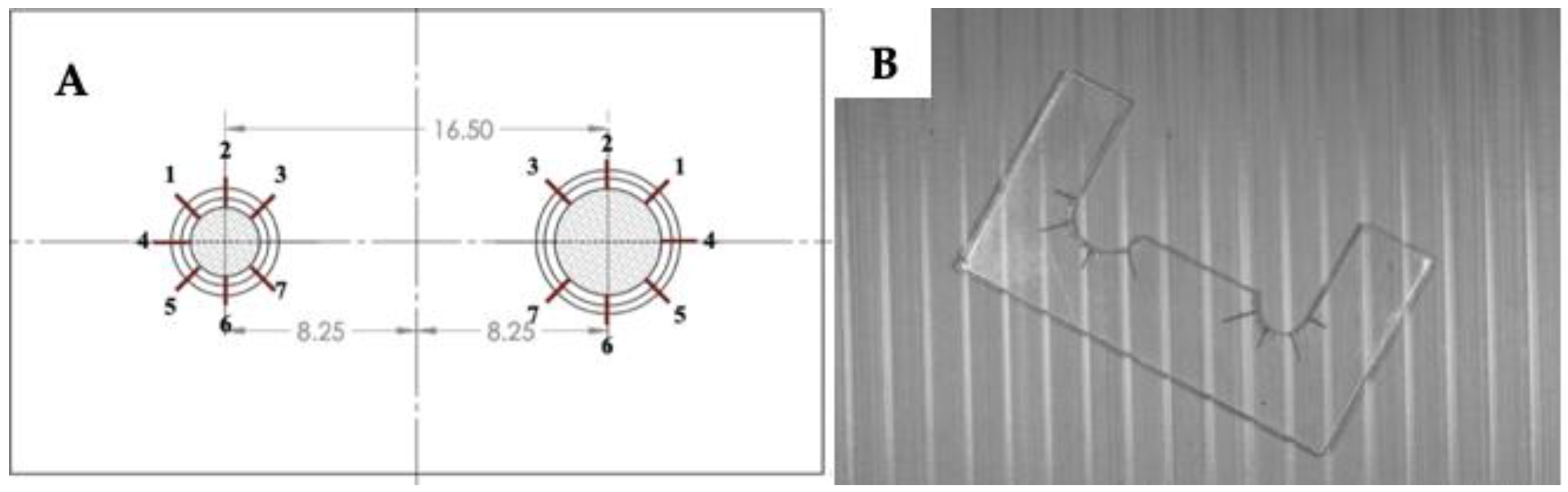
2.5. Marginal Discrepancy
2.6. Fracture Resistance
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The vertical marginal gap of both the PEKK and titanium groups exhibits a clinically acceptable marginal fit of less than 120 µm.
- The thermal aging process affects the marginal fit of PEKK but not that of titanium.
- The fracture load test indicates the potential for clinical use of PEKK in an implant-supported FPD framework in the molar region.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Han, K.H.; Lee, J.Y.; Shin, S.W. Implant—And Tooth-Supported Fixed Prostheses Using a High-Performance Polymer (Pekkton) Framework. Int. J. Prosthodont. 2016, 29, 451–454. [Google Scholar] [CrossRef] [PubMed]
- Poggio, C.E.; Ercoli, C.; Rispoli, L.; Maiorana, C.; Esposito, M. Metal-free materials for fixed prosthodontic restorations. Cochrane Database Syst. Rev. 2017, 12, CD009606. [Google Scholar] [CrossRef] [PubMed]
- Christensen, G.J. Ceramic vs. porcelain-fused-to-metal crowns: Give your patients a choice. J. Am. Dent. Assoc. 1994, 125, 311–312, 314. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.; Chopra, R.; Sachdev, V. Allergic Reactions to Dental Materials-A Systematic Review. J. Clin. Diagn Res. 2015, 9, ZE04–ZE09. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.H.; Hyde, B.; Hurst, M.; Harris, B.T.; Lin, W.-S. Polyetherketoneketone (PEKK), a framework material for complete fixed and removable dental prostheses: A clinical report. J. Prosthet. Dent. 2018, 119, 867–872. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef]
- Kemmish, D. Update on the Technology and Applications of Polyaryletherketones; iSmithers, Smithers Rapra Pub.: Shropshire, UK, 2010. [Google Scholar]
- Elmougy, A.; Schiemann, A.M.; Wood, D.; Pollington, S.; Martin, N. Characterisation of machinable structural polymers in restorative dentistry. Dent. Mater. 2018, 34, 1509–1517. [Google Scholar] [CrossRef]
- Alsadon, O.; Wood, D.; Patrick, D.; Pollington, S. Comparing the optical and mechanical properties of PEKK polymer when CAD/CAM milled and pressed using a ceramic pressing furnace. J. Mech. Behav. Biomed. Mater. 2019, 89, 234–236. [Google Scholar] [CrossRef]
- Klur, T.; Hasan, I.; Ottersbach, K.; Stark, H.; Fichte, M.; Dirk, C.; Bourauel, C. PEKK-made indirect temporary crowns and bridges: A clinical pilot study. Clin. Oral Investig. 2018, 23, 771–777. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Beuer, F.; Wimmer, T.; Jahn, D.; Sener, B.; Roos, M.; Schmidlin, P.R. Polyetheretherketone-A suitable material for fixed dental prostheses? J. Biomed. Mater. Res. Part B Appl. Biomater. 2013, 101, 1209–1216. [Google Scholar] [CrossRef] [PubMed]
- Nazari, V.; Ghodsi, S.; Alikhasi, M.; Sahebi, M.; Shamshiri, A.R. Fracture Strength of Three-Unit Implant Supported Fixed Partial Dentures with Excessive Crown Height Fabricated from Different Materials. J. Dent. 2016, 13, 400–406. [Google Scholar]
- Bhering, C.L.; Marques Ida, S.; Takahashi, J.M.; Barao, V.A.; Consani, R.L.; Mesquita, M.F. The effect of casting and masticatory simulation on strain and misfit of implant-supported metal frameworks. Mater. Sci. Eng. C Mater. Biol Appl. 2016, 62, 746–751. [Google Scholar] [CrossRef] [PubMed]
- El-Safty, S.; Silikas, N.; Watts, D.C. Creep deformation of restorative resin-composites intended for bulk-fill placement. Dent. Mater. 2012, 28, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Eichberger, M.; Uhrenbacher, J.; Wimmer, T.; Edelhoff, D.; Schmidlin, P.R. Three-unit reinforced polyetheretherketone composite FDPs: Influence of fabrication method on load-bearing capacity and failure types. Dent. Mater. J. 2015, 34, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Taufall, S.; Eichberger, M.; Schmidlin, P.R.; Stawarczyk, B. Fracture load and failure types of different veneered polyetheretherketone fixed dental prostheses. Clin. Oral. Investig. 2016, 20, 2493–2500. [Google Scholar] [CrossRef] [PubMed]
- Krejci, I.; Reich, T.; Lutz, F.; Albertoni, M. An in vitro test procedure for evaluating dental restoration systems. 1. A computer-controlled mastication simulator. Schweiz. Monatsschr. Zahnmed. 1990, 100, 953–960. [Google Scholar] [PubMed]
- Rosentritt, M.; Hahnel, S.; Engelhardt, F.; Behr, M.; Preis, V. In vitro performance and fracture resistance of CAD/CAM-fabricated implant supported molar crowns. Clin. Oral. Investig. 2017, 21, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Segerstrom, S.; Ruyter, I.E. Effect of thermal cycling on flexural properties of carbon-graphite fiber-reinforced polymers. Dent. Mater. 2009, 25, 845–851. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.; Gonzalo, E.; Gomez-Polo, M.; Lopez-Suarez, C.; Suarez, M.J. SEM evaluation of the precision of fit of CAD/CAM zirconia and metal-ceramic posterior crowns. Dent. Mater. J. 2017, 36, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Pasali, B.; Sarac, D.; Kaleli, N.; Sarac, Y.S. Evaluation of marginal fit of single implant-supported metal-ceramic crowns prepared by using presintered metal blocks. J. Prosthet. Dent. 2018, 119, 257–262. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Moris, I.C.M.; Faria, A.C.L.; Ribeiro, R.F.; Fok, A.S.; Rodrigues, R.C.S. Custom Morse taper zirconia abutments: Influence on marginal fit and torque loss before and after thermomechanical cycling. J. Mech. Behav. Biomed. Mater. 2018, 78, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Koc, E.; Ongul, D.; Sermet, B. A comparative study of marginal fit of copings prepared with various techniques on different implant abutments. Dent. Mater. J. 2016, 35, 447–453. [Google Scholar] [CrossRef]
- Bae, S.Y.; Park, J.Y.; Jeong, I.D.; Kim, H.Y.; Kim, J.H.; Kim, W.C. Three-dimensional analysis of marginal and internal fit of copings fabricated with polyetherketoneketone (PEKK) and zirconia. J. Prosthodont. Res. 2017, 61, 106–112. [Google Scholar] [CrossRef]
- Park, J.Y.; Bae, S.Y.; Lee, J.J.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Evaluation of the marginal and internal gaps of three different dental prostheses: Comparison of the silicone replica technique and three-dimensional superimposition analysis. J. Adv. Prosthodont 2017, 9, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.Y.; Teng, M.H.; Wang, Z.J.; Li, X.; Liang, J.Y.; Wang, W.X.; Jiang, S.; Zhao, B.D. Comparative evaluation of BioHPP and titanium as a framework veneered with composite resin for implant-supported fixed dental prostheses. J. Prosthet. Dent. 2019, 122, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Blumer, L.; Schmidli, F.; Weiger, R.; Fischer, J. A systematic approach to standardize artificial aging of resin composite cements. Dent. Mater. 2015, 31, 855–863. [Google Scholar] [CrossRef]
- Ehrenberg, D.S.; Weiner, S. Changes in marginal gap size of provisional resin crowns after occlusal loading and thermal cycling. J. Prosthet. Dent. 2000, 84, 139–148. [Google Scholar] [CrossRef]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef]
- Ehrenberg, D.; Weiner, G.I.; Weiner, S. Long-term effects of storage and thermal cycling on the marginal adaptation of provisional resin crowns: A pilot study. J. Prosthet. Dent. 2006, 95, 230–236. [Google Scholar] [CrossRef]
- Angwarawong, T.; Reeponmaha, T.; Angwaravong, O. Influence of thermomechanical aging on marginal gap of CAD-CAM and conventional interim restorations. J. Prosthet Dent. 2020, 124, 566.e1–566.e6. [Google Scholar] [CrossRef] [PubMed]
- Kemmish, D. Practical Guide to High. In Performance Engineering Plastics; iSmithers, Smithers Rapra Pub.: Shropshire, UK, 2011. [Google Scholar]
- Young, R.J.; Lovell, P.A. Introduction to Polymers, 3rd ed.; Taylor & Francis: Oxfordshire, UK, 2011. [Google Scholar]
- Cverna, F.; ASMIMPD Committee. ASM Ready Reference: Thermal Properties of Metals; ASM International: Almere, The Netherlands, 2002. [Google Scholar]
- Ruttermann, S.; Kruger, S.; Raab, W.H.; Janda, R. Polymerization shrinkage and hygroscopic expansion of contemporary posterior resin-based filling materials—A comparative study. J. Dent. 2007, 35, 806–813. [Google Scholar] [CrossRef] [PubMed]
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Loffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical characterization of polyetheretherketone and current esthetic dental CAD/CAM polymers after aging in different storage media. J. Prosthet. Dent. 2016, 115, 321–328.e322. [Google Scholar] [CrossRef] [PubMed]
- McKeen, L. The Effect of Creep and Other Time Related Factors on Plastics and Elastomers, 2nd ed.; William Andrew Pub.: Norwich, NY, USA, 2009. [Google Scholar]
- Ferguson, S.J.; Visser, J.M.; Polikeit, A. The long-term mechanical integrity of non-reinforced PEEK-OPTIMA polymer for demanding spinal applications: Experimental and finite-element analysis. Eur. Spine J. 2006, 15, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Stappert, C.F.; Dai, M.; Chitmongkolsuk, S.; Gerds, T.; Strub, J.R. Marginal adaptation of three-unit fixed partial dentures constructed from pressed ceramic systems. Br. Dent. J. 2004, 196, 766–770, discussion 760, quiz 780. [Google Scholar] [CrossRef]
- Jørgensen, K. Factors Affecting the Film Thickness of Zinc Phosphate Cements. Acta Odontol. Scand. 2009, 18, 479–490. [Google Scholar] [CrossRef]
- Owittayakul, D.; Lertrid, W.; Anatamana, C.; Pittayachawan, P. The comparison of the marginal gaps of zirconia framework luted with different types of phosphate based-resin cements The comparison of the marginal gaps of zirconia framework luted with different types of phosphate based-resin cements. Mahidol. Dent. J. 2015, 35, 237–251. [Google Scholar]
- Meshreky, M.; Halim, C.; Katamish, H. Vertical Marginal Gap Distance of CAD/CAM Milled BioHPP PEEK Coping Veneered by HIPC Compared to Zirconia Coping Veneered by CAD-On lithium disilicate “In-Vitro Study”. J Adv. Dent. J. 2020, 2, 43–50. [Google Scholar] [CrossRef][Green Version]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef]
- Groten, M.; Axmann, D.; Probster, L.; Weber, H. Determination of the minimum number of marginal gap measurements required for practical in-vitro testing. J. Prosthet. Dent. 2000, 83, 40–49. [Google Scholar] [CrossRef]
- Gassino, G.; Barone Monfrin, S.; Scanu, M.; Spina, G.; Preti, G. Marginal adaptation of fixed prosthodontics: A new in vitro 360-degree external examination procedure. Int. J. Prosthodont. 2004, 17, 218–223. [Google Scholar] [PubMed]
- Chitmongkolsuk, S.; Heydecke, G.; Stappert, C.; Strub, J.R. Fracture strength of all-ceramic lithium disilicate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur. J. Prosthodont. Restor. Dent. 2002, 10, 15–22. [Google Scholar] [PubMed]
- Amelya, A.; Kim, J.E.; Woo, C.W.; Otgonbold, J.; Lee, K.W. Load-Bearing Capacity of Posterior CAD/CAM Implant-Supported Fixed Partial Dentures Fabricated with Different Esthetic Materials. Int. J. Prosthodont. 2019, 32, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Varga, S.; Spalj, S.; Lapter Varga, M.; Anic Milosevic, S.; Mestrovic, S.; Slaj, M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur. J. Orthod. 2011, 33, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Cosme, D.C.; Baldisserotto, S.M.; Canabarro Sde, A.; Shinkai, R.S. Bruxism and voluntary maximal bite force in young dentate adults. Int. J. Prosthodont. 2005, 18, 328–332. [Google Scholar] [PubMed]




| Group (n) | Mean Marginal Gap (SD) | ||||||
|---|---|---|---|---|---|---|---|
| Initial | After Thermocycling | p-Value | After Cyclic Loading | p-Value | After Five-Year Thermomechanical Aging | p-Value | |
| Titanium (12) Percentile: 25/75 | 44.04 (24.16) 30.12/59.32 | 44.65 (24.15) 29.15/58.24 | 0.209 | 44.72 (24.11) 28.61/60.83 | 1.00 | 44.72 28.61/60.83 | 0.071 |
| PEKK (12) Percentile: 25/75 | 81.75 (44.53) 36.36/120.50 | 84.99 (44.28) 39.11/121.65 | 0.000 a | 85.31 (44.43) 39.31/123.85 | 0.323 | 85.31 39.31/123.85 | 0.000 a |
| Group (n) | Mean of Marginal Gap Change (SD) | ||
|---|---|---|---|
| Post-Thermocycling | Post-Cyclic Loading | Post-Five-Year Thermomechanical Aging | |
| Titanium (12) | 0.04 (2.07) | 0.93 (2.71) | 0.71 (1.23) |
| PEKK (12) | 3.24 (2.01) | 0.32 (1.07) | 3.56 (2.02) |
| p-value | 0.003 a | 0.45 | 0.002 a |
| Group | Position | Mean Marginal Gap Change (Δ) According to Position (µm) | ||
|---|---|---|---|---|
| ΔPost Thermocycling | ΔPost Cyclic loading | ΔPost Five-Year Aging | ||
| Titanium | 1 | −0.45 | 1.90 | 1.45 |
| 2 | 0.61 | 1.38 | 1.99 | |
| 3 | 1.49 | −0.84 | 0.65 | |
| 4 | 0.85 | −0.03 | 0.33 | |
| 5 | −0.63 | 1.53 | 2.75 | |
| 6 | −0.53 | 1.34 | 0.81 | |
| 7 | 0.50 | −0.80 | −0.70 | |
| p-value | 0.679 | 0.829 | 0.631 | |
| PEKK | 1 | 3.17 | 0.25 | 3.42 |
| 2 | 2.18 | 0.97 | 3.15 | |
| 3 | 2.04 | 0.19 | 2.22 | |
| 4 | 3.77 | 0.65 | 4.41 | |
| 5 | 2.36 | 0.84 | 3.20 | |
| 6 | 4.46 | −0.80 | 3.66 | |
| 7 | 5.11 | 0.12 | 5.23 | |
| p-value | 0.514 | 0.532 | 0.532 | |
| Ultimate Fracture Load (N) | p-Value | ||
|---|---|---|---|
| Titanium | PEKK | ||
| Mean (SD) | 3050.18 (385.30) | 1359.14 (205.49) | 0.000 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Visuttiwattanakorn, S.; Suthamwat, A.; Urapepon, S.; Kiattavorncharoen, S. Reliability of Polyetherketoneketone as Definitive Implant-Supported Bridges in the Posterior Region—An In Vitro Study of the Ultimate Fracture Load and Vertical Marginal Discrepancy after Artificial Aging. Appl. Sci. 2022, 12, 11454. https://doi.org/10.3390/app122211454
Visuttiwattanakorn S, Suthamwat A, Urapepon S, Kiattavorncharoen S. Reliability of Polyetherketoneketone as Definitive Implant-Supported Bridges in the Posterior Region—An In Vitro Study of the Ultimate Fracture Load and Vertical Marginal Discrepancy after Artificial Aging. Applied Sciences. 2022; 12(22):11454. https://doi.org/10.3390/app122211454
Chicago/Turabian StyleVisuttiwattanakorn, Surakit, Apitchaya Suthamwat, Somchai Urapepon, and Sirichai Kiattavorncharoen. 2022. "Reliability of Polyetherketoneketone as Definitive Implant-Supported Bridges in the Posterior Region—An In Vitro Study of the Ultimate Fracture Load and Vertical Marginal Discrepancy after Artificial Aging" Applied Sciences 12, no. 22: 11454. https://doi.org/10.3390/app122211454
APA StyleVisuttiwattanakorn, S., Suthamwat, A., Urapepon, S., & Kiattavorncharoen, S. (2022). Reliability of Polyetherketoneketone as Definitive Implant-Supported Bridges in the Posterior Region—An In Vitro Study of the Ultimate Fracture Load and Vertical Marginal Discrepancy after Artificial Aging. Applied Sciences, 12(22), 11454. https://doi.org/10.3390/app122211454





