Abstract
The objective of this work is to design a rehabilitation mechanism for the index finger that can replicate the finger’s natural movements in the sagittal plane; this mechanism must also be able to adapt to an individual’s anthropometric dimensions. The personalization of the mechanism is made through a parametric model assisted by computer-aided design software. An infrared motion capture system is used to validate the natural finger movements, comparing them to the ones generated by the parametric designed mechanism. The replication of natural finger movements with this mechanism is possible due to the use of virtual centers and the employment of two degrees of freedom. One degree of freedom is proximal phalanx flexion-extension, and the other one is the middle-distal phalanges conjoined movement. The replication of natural motions and the use of personalization techniques offer three main advantages: a diverse set of rehabilitation exercises, an increase in the range of motion of the finger compared to other designs in the literature and the short construction time required for the rehabilitation device.
1. Introduction
Strokes are among the principal causes of disability worldwide. Among its consequences, one of the major ones is the loss of mobility in the upper and lower extremities, limiting the subject’s autonomy in the Activities of Daily Living (ADLs) [1]. Approximately 65% of patients who have suffered a stroke remain severely handicapped even one year after the incident [2]. Frequently, it is the case that the recovery of hand motion is one of the most challenging topics in rehabilitation after a stroke [3,4].
It has been shown that rehabilitation therapy using robotic aid improves the motor function of the upper limbs [5,6]. Rehabilitation gloves with active technologies refer to devices that use external energy to assist with movement during therapy. Generally, active rehabilitation gloves involve the use of mechatronic or robotic systems. The use of such technologies has many advantages, such as an improvement in motor recovery compared to traditional therapies [7,8], shorter rehabilitation time [9] and they can reproduce consistent, high-quality movements during therapy sessions [10]. In the case of hand rehabilitation, most of the devices are designed as a single-action glove, meaning that they only help the patient to open the hand or, in the least of cases, to close it [4,11]. Several rehabilitation gloves that help with finger extension are found in the scientific literature, including:
- Saeboflex [12], which uses springs anchored at the fingertips to produce extension.
- Mobile Digit Assistive System, MIDAS [13], which has adjustable cams that allow for different assistive forces with springs.
- HANDEXOS [14], a cable-driven mechanism actuated by a DC motor.
- Hand-Spring Operated Movement Enhancer (HandSOME) [15], with adjustable spring anchor points and mechanical stops to limit the Range of Motion (ROM) depending on the patient’s needs.
These single-action designs focus on extension assistance because, in stroke patients, hand function is often lost due to flexor hypertonia and weakness in finger extensor muscles [15].
Sang Wook Lee et al. [16] show that a critical success factor in rehabilitation therapy is the intensity and complexity of exercises the patient performs during therapy sessions. Complex hand movements in rehabilitation are essential since these allow for task-oriented training, which shows a favorable improvement in the capacity of the subject to carry ADLs [17]. The number of Degrees Of Freedom (DOFs) is directly related to the complexity and variety of movements that the glove can replicate [18]; therefore, at a surface level, more DOFs are equal to better rehabilitation for the patient. However, by increasing the DOFs, the cost of manufacturing and the difficulty of controlling the mechanism increases. For these reasons, it is necessary to find an equilibrium when selecting the number of DOFs [18].
In order to reproduce complex movements, it is also necessary to keep the assisting mechanism as least intrusive as possible, allowing for the ROM during rehabilitation to be the closest to the natural ROM of a healthy human hand. One solution to make a less intrusive mechanism is using virtual centers and cams, which allow the mechanism’s hinges to be away from the finger’s articulations. A mechanism that uses virtual centers is proposed in studies performed by Susanto [19,20]. Nevertheless, this mechanism only transmits movement to the middle and proximal phalanges while having a limited range of motion, as just one design is made to fit a wide variety of patients.
The ROM of the mechanism can be increased if it is designed specifically for each patient [21]. The quick personalization of a rehabilitation glove is possible thanks to the anatomical properties of the human hand. General anatomical studies of the phalanx and metacarpal bones in adults have found statistical ranges of up to 31.71 mm for the second finger’s bone lengths [22]. This variation indicates a wide disparity of anthropometric measurements in individuals. Nevertheless, multiple studies have shown constant proportions between metacarpals and phalanges bones [23]. For example, in [24], equations have been proposed to obtain the metacarpals, proximal and middle phalanges lengths as a function of the distal phalanx. Other works study the proportions between the phalanges and metacarpals, and they have found these proportions to be different between each finger [25]. Hence, the best approach is to find individual proportions for each finger, as was found in Buryanov’s [24] study.
This research aims to produce a personalized finger rehabilitation mechanism design for the second human digit that has a broad ROM and is easy to manufacture. The proposed rehabilitation mechanism focuses only on finger movements in the sagittal plane. The mechanism in this study has two DOFs, uses virtual centers (through cams) and employs a parametric model to personalize the mechanism’s 3D design. These design choices were made to maximize the patient finger’s ROM and increase the variety and complexity of exercises during rehabilitation. With the help of parametric models and 3D printing technology, the device has a low cost compared to others, while the time needed for designing and manufacturing is also reduced. The main contributions to the rehabilitation field of this work are:
- The ROM for each finger articulation is increased compared to the prototypes proposed in the current literature by using personalized four-bar mechanisms and cams with virtual centers.
- Quickly personalizing finger rehabilitation devices that suit each patient’s need through a parametric model will provide a unique work area for each individual.
- The mechanism is non-invasive, having very little interference with the finger’s natural movements by placing almost every part of the mechanism above the fingers and avoiding the use of physical hinges located at the articulation level.
- Increments in the variety and flexibility of possible rehabilitation exercises, compared to designs mentioned before, by using two DOFs for each finger and having double action.
- Reduction in manufacturing and design time and costs.
2. Materials and Methods
2.1. General Framework
It is essential for modeling a finger’s movement to consider how the tendons are anchored to the bones and the geometry of the hand’s articulations because these restrict the movements of each bone segment [26]. A simplified model of the human finger considering the location of the tendons is proposed in Becker’s study [27]. In Becker’s study, the range of motion (ROM) for each articulation is given by two factors: the tendon length when the finger is fully extended and the radius of each articulation.
Regarding the total ROM of a human index finger in Hume’s work [28], the functional ROMs found for each articulation were the following:
- 0° to 100° for the metacarpophalangeal (MCP) joint.
- 0° to 105° for the proximal interphalangeal (PIP) joint.
- 0° to 85° for the distal interphalangeal (DIP) joint.
Concerning the number DOFs for the flexion and extension of the index finger, it could be said that there are three DOFs in total due to the three articulations in the finger (MCP, PIP, and DIP). However, in [26], it is demonstrated that due to the finger’s anatomy and the ligaments’ position, both movements at the PIP and DIP joints are just one DOF and thus can be modeled as a conjoined movement. Therefore, with just two DOFs, the movements of interest for this work can be replicated: one DOF for the proximal phalanx movement and one for the conjoined motion of the middle and distal phalanges.
The type of mechanism selected for this study is a closed-loop bar rigid mechanism with virtual centers; this implies that the finger’s position is always constant according to the input of the mechanism. On the other hand, by using virtual centers, the hinges that allow for the rotation of the finger’s phalanges can be located away from the biological rotation center of each articulation, thus interfering less with the natural ROM of the human fingers. This mechanism is selected because it contributes the most to the rehabilitation success factors mentioned in the introduction of this work; it allows for a comprehensive set of consistent and complex finger motions, which also makes the implementation of functional motion therapy possible. The rehabilitation mechanism can be divided into two separate sub-mechanisms. The first mechanism is shown in Figure 1, which moves the distal and middle phalanges, while the second mechanism, which moves the proximal phalanx, is represented in Figure 2. As can be seen, the first mechanism is much more important because it must move two phalanges at the same time.
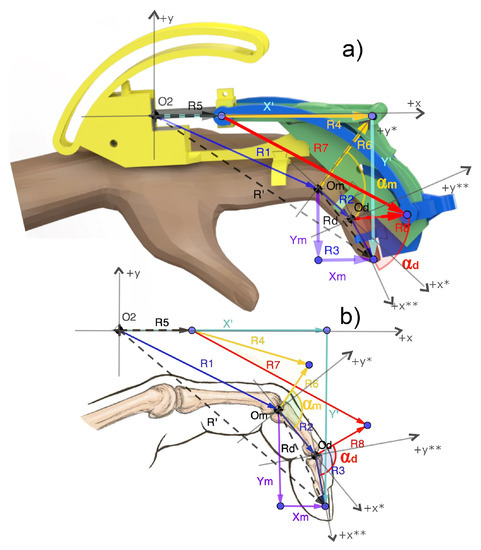
Figure 1.
Figure illustrating the mechanism’s kinematic chains for the middle-distal phalange’s conjoined movement. (a) Shows the vectors superimposed on the mechanism’s 3D model. (b) Shows the vectors on the finger so the virtual centers of rotation and can be appreciated. As can be seen in this figure, there are several vector paths of interest (represented in different colors). Combinations between different vector paths produce kinematic chains that will be used to generate vector loop equations. The * and ** marks indicate local planes of reference.
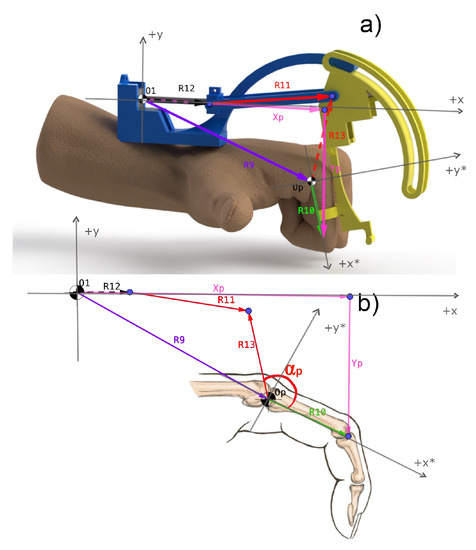
Figure 2.
Figure illustrating the mechanism’s kinematic chains for the proximal phalanx movement. (a) Shows the vectors superimposed on the mechanism’s 3D model. (b) Shows the vectors on the finger so the virtual center of rotation can be appreciated. Similarly to the first mechanism, as it can be seen in this figure, there are several vector paths of interest (represented in different colors). Combinations between different vector paths produce kinematic chains that will be used to generate vector loop equations. The * mark indicates a local plane of reference.
In order to generate the first design of the mechanism (before implementing the parametric model), a series of measurements are taken of a patient’s finger. For taking these dimensions, a scanner is used. The procedure, shown in Figure 3a, consists of taking a scan of the patient’s hand and an element of a known length, which is a scale mark of 50 mm. Then the scanned image is transferred to a video and image analysis software called Tracker. Once within the software, a digital scale is established using the element of known length, allowing the software to scale pixels into millimeters. Then vectors are added in the software to each element of interest within the index finger. In Figure 3a, one vector represents the proximal phalanx from the MCP to the PIP joints (in magenta), another vector is the middle phalanx from the PIP to DIP joints (in cyan) and another for the distal phalanx from the DIP joint to the tip of the finger (in blue). As the last step, the magnitudes of the vectors are extracted from the software. It is important to consider that the distal phalanx length is not directly the magnitude of the vector. According to the study by Buryanov [24], the average length of soft tissue at the tip of the index finger is 3.84 ± 0.59 mm, so in order to get the proper bone length, an offset of 3.84 mm is used to obtain the distal phalanx’s correct length.
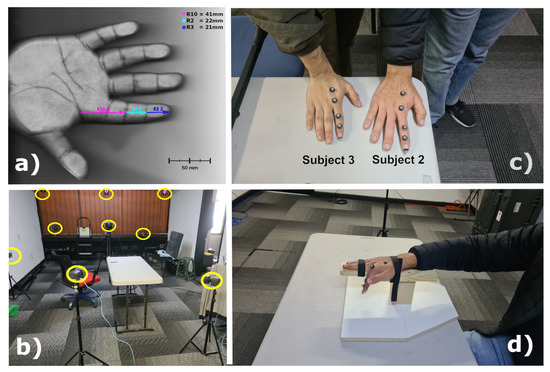
Figure 3.
(a) Image illustrating how the finger measurements are taken. (b) Infrared Camera Layout. (c) Location of the markers during MOCAP experiments. (d) Device used for resting the palm and forearm during experiments to guarantee consistency of the finger trajectories.
An infrared Motion Capture (MOCAP) system and software are used to obtain the finger’s trajectories. The Nexus software and Vantage cameras from the manufacturer Vicon are employed to conduct the experiments to obtain the experimental curves of the index finger’s tip. Twelve infrared cameras are arranged in a circular pattern, as shown in Figure 3b. In Figure 3c, the location of the reflective markers can be seen; 5.5 mm spherical markers are used at the DIP, PIP, MCP joints, and the finger’s tip. Further, one reference marker is used at the metacarpal bones. Three different subjects were tested in this experiment to validate the parametric model. In order to keep the markers’ trajectories as consistent as possible, a support device is used, as shown in Figure 3d, which suppressed the most undesirable movements.
It is important to note that during the MOCAP experimentation, the markers were located on top of the fingers. It is also critical to assess the markers’ location since the mathematical model gives the finger’s trajectory considering the rotation points at the finger’s center. In order to compensate for this difference, one marker radius and half of the finger thickness at the marker’s location were subtracted from the coordinates given by the Vicon software. Despite these corrections, there is still some error produced as the markers shift in position with the contraction and expansion of the soft tissue. These differences also contribute to the discrepancy in the experimental and theoretical trajectories of the finger.
2.2. Parametric Model
The parametric model refers to a mathematical model that is fundamental for this study because, by using this model, the exoskeleton finger glove can be made for each individual efficiently. This model only needs two anatomical measurements from the patient’s finger: the distal phalanx’s length and diameter. In [24], research is conducted on 66 healthy adult patients (from 19 to 78 years old) to determine the length of the middle phalanx, proximal phalanx and metacarpal bones as a proportion of their distal phalanx. Studies before [24] had already found a certain regularity in the proportion of the finger segments. Generally, it was accepted that this relationship followed the Fibonacci sequence [25]; however, this statement was later rejected by studies such as [29]. After seeing that models that use the same proportions for every finger are not very accurate, there were approaches to produce mathematical predictions of the proportions for each phalanx; for example, there are works [22,24].
One potential problem in the studies mentioned is the lack of consistency when taking the phalanx segment measurements, producing different magnitudes of errors within their models. The model proposed by Buryanov [24] is the one selected for this study, as this is one of the few that uses thermograms, bone scans, and X-rays to find the finger segment proportions, giving it an advantage regarding its precision. As a result from [24], the following proportions were found for the index finger: the distal phalanx is the unit of reference, then the middle phalanx is found to be 1.4 the distal phalanx, and the proximal phalanx is 2.5 the distal phalanx.
The process of obtaining a personalized finger rehabilitation mechanism begins by taking only two measurements from the patient: the length and width of the distal phalanx. Then the next step is to introduce these values to a Python program created in this work, which uses the proportions found by Buryanov [24] in its code to get the rest of the measurements needed to produce the new CAD design. The third step is to take the .txt file that is given as an output of the Python program and then transfer this to the folder at the location of the SolidWorks 3D models. Finally, in SolidWorks, the assembly is refreshed; thus, the table of relations inside SolidWorks is updated along with all the mechanism’s 3D models.
There are two main advantages of using the proposed parametrization model:
- The reduction in the time it takes to produce a 3D model of a rehabilitation mechanism that is adapted to an individual’s anatomical dimensions.
- The maximization of the patient articulations’ ROM by making the mechanism fit their individual anatomy.
The proposed model is tested on three healthy male adult subjects.
2.3. Kinematic Model
2.3.1. Direct Model
In order to know the coordinates of the index finger’s tip, the forward kinematic model of the mechanisms needs to be solved. For the case of the system proposed in this study, there are two independent mechanisms with one autonomous DOF for each one.
From hereafter, in order to simplify this work, only one DOF of the mechanism is analyzed; in this case, only the mechanism that moves the middle and distal phalanges is subject to a kinematic analysis. The mechanism for the second DOF (which moves the proximal phalanx) is very similar to the first mechanism, with the only difference being the links’ length and the cams’ diameter; therefore, the steps for analyzing this mechanism are very similar to the ones shown below.
In Table 1, all the variables and constants for the kinematic chains of the first DOF mechanism are shown.

Table 1.
Variables and constants for mechanism 1.
In Figure 1, all the kinematic chains that are needed to be solved for the distal-middle phalanx movement are shown. The variables that are needed to describe the finger’s tip are the coordinates and , which are referenced to the origin at the starting position of the linear actuator.
From Table 1, it can be seen that there are two input variables: , which is the input for the parametric model (the distal phalanx length), and , which is the magnitude of the vector that changes as the actuator moves. In regards to the constants shown in Table 1, , , and are fixed and given by the original mechanism’s design. Similarly, is given by the orientation of the actuator, which, in this case, is a motor connected to a screw; therefore, being linear. Lastly, angles and are constant since they represent the angle between the phalanges and vectors and , respectively, which the designer also gives.
It is crucial for generating the kinematic models to consider where the angles for each vector are being measured. Considering the representation in Figure 1, all vector angles were referenced to the positive -axis of the coordinate system where they originated from, or, in the case of vectors that originated elsewhere, their angle is considered to be measured from the same axis as the previous vector they are connected to.
It could be said that there are two main kinematic chains for the mechanism. These two main kinematic chains are represented in closed vector loop form in Equations (1) and (2). The path of these chains can be traced in Figure 1.
Besides the two main kinematic chains for the mechanism, there are two more. These other two kinematic chains are the ones that are used to represent the fingertip’s coordinates referenced to the general origin O and the origin at the PIP joint shown in Figure 1. The closed vector loop equations for these chains are (3) for the fingertip’s coordinates with respect to O, and (4) with respect to . Similarly to the loops shown in Equations (1) and (2), the kinematic chains in Equations (3) and (4) can be followed in Figure 1.
In the vector loop form, one of the vectors is fully defined from the start (constant): , there is one input vector: and there are eight unknown vectors, which are the ones that have elements that need a solution (it could be magnitude or direction); , , , , , , , .
At the beginning of the analysis, the constant relationship given by the angles must be considered: between and , and and . The said relationship is shown in Equations (5) and (6).
Since the angles are constant, then and can be found solely from and .
The initial values for , , , , and can be obtained since we know that, in this initial position of the mechanism, the finger is horizontal, which means that the angles for and are 0°. If the initial vector loops are solved, then we can obtain all the magnitudes for the vectors since they are constant through all of the movement of the mechanism (except for , which is an input and has the angle constant but the magnitude changes). The unknown magnitudes are: , , , and , and since the angles and are known for the initial position, then and can be found using Equations (5) and (6) for the initial position.
To find the magnitude of , the parametric model is used, and it is given by Equation (7). The parametric model is explained in further detail in Section 2.2.
For the magnitude of , a quadratic regression is used, in which the independent variable is the length of the distal phalanx (). Equation (8) is obtained from the previously mentioned regression in which the had a value of 0.998. During the regression, the value of is changed, so the final angle of flexion for the distal phalanx is 85°. This is performed for each of the inputs varying from 8 to 40 mm using increments of 1 mm. The distal phalanx length range used in the regression covers most of the population, according to various studies [30,31,32].
Finally, the magnitudes and could be found from the initial position and the already known vectors using the transformation of Equations (1) and (2) into Euler’s identity form since the magnitude of at this moment is zero, then in Equations (9) and (10) is zero.
Now, given all the magnitudes, the angles can be calculated using the Freudeinsetin equation and semi-angular identities to transform the cosines and sines into tangent functions obtaining the following equations, as a result:
Finally, to find the four remaining unknowns: , the Equations (A7)–(A10) are used (contained in Appendix A).
2.3.2. Inverse Model
Regarding the inverse kinematic analysis, Equations (15) to (18) were obtained by using a similar method to the direct kinematic problem. In this case, the input is the trajectory of the distal phalanx’s tip, and the final expected result is to obtain the magnitude of the vector . All the kinematic chain equations are the same as the ones presented from (A1) to (A10); therefore, the only thing that changes is that now is unknown, and and are the input.
The values for , , and are shown in Appendix B, and and can be found by using Equations (5) and (6), respectively. Finally, the magnitude for is given by Equation (18).
2.4. Prototype Description
The final mechanism that is presented in this work can be seen in Figure 4 below.
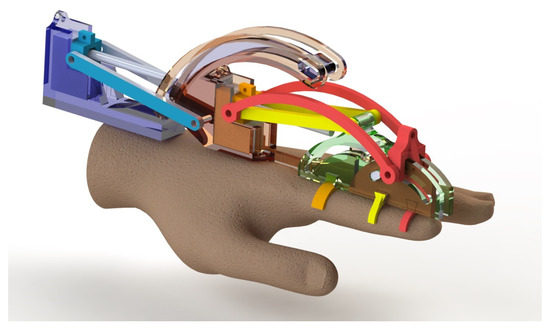
Figure 4.
Mechanism’s 3D model for 2 DOF motion transmission of a human finger.
As mentioned before, the prototype consists of three closed-loop bar mechanisms, which means it is a rigid system. Two of the closed loop bar mechanisms are conjoined and are the ones that transmit movement to the middle and distal phalanges, while the third mechanism is independent and moves the proximal phalanx. A picture of the printed physical mechanism is established in Figure 5.

Figure 5.
Three-dimensional-printed prototype for Subject 1.
As for the material selection, PLA is used to make most of the mechanism’s structure. PLA was selected because of its ease of use in FDM 3D printing, and it also complied with the needed mechanical properties. A static and dynamic software simulation of the forces applied to each mechanism element was used to find the stresses the material should be able to withstand. DC motors with reduction gears were used to transmit movement to a screw mechanism to produce a linear actuator that drove each of the two DOFs.
3. Results and Discussions
In this work, the design and fabrication of a finger exoskeleton are made. The purpose of the exoskeleton is to transmit movement to the index finger of a rehabilitation patient. The type of therapy that the system assists with is ROM or movement therapy. During the design of the mechanism, a parametric model is used, which could be considered the most significant contribution of this work. The parametric model is based on previous studies [24]. With the finger proportions, a program is created in Python. This program produces a .txt file, later imported to SolidWorks and used as a reference for the mechanism dimensions.
After inputting the experimental anatomical values from the parametric program in Python, the experimental and theoretical values for the middle and proximal phalanges were obtained, along with the absolute and relative errors giving Table 2 as a result.

Table 2.
Errors for the index’s phalanges lengths.
Due to document limitations and to keep it concise, only the inputs and numerical results are shown for subject 1 as an example. Nevertheless, further down this section, all the plots comparing the different trajectories for each subject can be seen, so a comparison between the different mechanisms can be made.
For the first DOF mechanism, which is in charge of the conjoined movement of the index and middle finger, the dimensions that were used to find the distal tip theoretical trajectory for subject 1 are the following: = 67.7 mm, = 23.8 mm, = 17 mm, = 61.5 mm, with input varying from 0 to 37 (0.1 increments), = 38.3 mm, = 85.3 mm, = 19.18 mm, = 333.95°, and = 60.82.
In the case of the second DOF, which moves the proximal phalanx, equations similar to those in Section 2.3.1 were used. These equations needed, as input, the following values to find the position of the tip of the proximal phalanx: and : = 71.72 mm, = 42.5 mm, = 64.13 mm, = 27.3 mm, with input varying from 0 to 34 (0.1 increments) mm, = 0°, = 71.12°, and = 108.29°.
Similarly to the direct models, the inverse kinematic needs a series of constants and an input to give its output. Therefore, for the first DOF mechanism, the following values are needed as inputs to solve the inverse kinematic model: as an input taken from the direct kinematic model, as an input taken from the direct kinematic model, = 67.7 mm, = 23.8 mm, = 17 mm, = 85.3 mm, = 19.18 mm, = 333.95°, = 88.821°, and = 89.884°.
On the inverse kinematic model for the second DOF, the input would be the coordinates of the proximal phalanx tip, along with the lengths of the links within the mechanism for this second DOF. This specific mechanism’s input values are the following: as an input taken from the direct kinematic model, as an input taken from the direct kinematic model, = 71.72 mm, = 42.5 mm, = 64.13 mm, = 27.3 mm, = 0°, = 71.12°, and = 108.29°.
A significant amount of time could be saved by producing the parametric model. In the case of the mechanism’s 3D model, thanks to this parametric model, it is not necessary for a human designer to manually change every dimension of the mechanism to fit the patient’s hand, and instead, this is done by the algorithm proposed in this work. This algorithm consists of a program written in Python, which produces a .txt file as an output. Then a SolidWorks assembly searches and uses the values on this .txt file as references for all the mechanisms’ different elements. Additionally, time is saved in the manufacturing process, thanks to the 3D-printing Fused Deposition Modeling (FDM) technology used.
The subsequent trajectory curves, shown in Figure 6, were obtained for subjects 1, 2, and 3 of the first and second DOFs after applying the parametric and kinematic models. On these plots, the blue line represents the theoretical trajectory described by the finger’s tip. At the same time, the red dots are the experimental curves of the finger obtained using the MOCAP system.
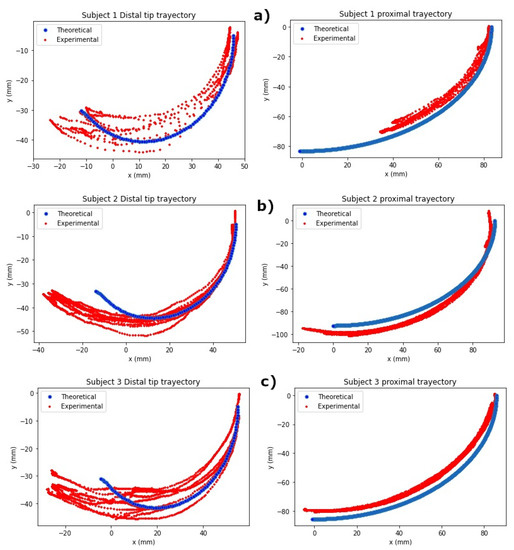
Figure 6.
Experimental vs. theoretical trajectories of the first and second DOF for: (a) subject 1, (b) subject 2, and (c) subject 3.
Regarding the plots in Figure 6, it can be seen that the theoretical curve falls inside the cloud of points from the experimental values. Nevertheless, the experimental trajectories slightly differ from the theoretical one. This discrepancy between the results could be due to a series of factors, including the precision of the instruments and software used to track the phalanges’ tips. There is also a human factor for when the patient is doing the desired movements, the forearm or wrist could move, therefore, producing an offset between each time the finger is flexed and extended. Another factor that possibly influences the results is the differences between the actual anatomy of the fingers’ articulations and the kinematic model, which considers these articulations to be spherical. In addition, there are more anatomical limitations that make the experimental results differ from the theoretical ones, such as how the model considers the phalanges to be one-dimensional, disregarding the actual bone, muscle, and fat that add volume to the finger. In reality, the soft tissue of the finger limits the movement of the phalanges when they are contracted. Therefore, soft tissue is most likely the cause of the difference between trajectories at the end of the contraction movement. As can be observed in the plots in Figure 6b, the most significant deviation in the curves occurs at the end of the contraction movement.
The parametric mechanism design was successful for the three subjects tested during this study. This model’s success is confirmed because the natural trajectories of the subjects’ phalanges tips were very similar to the ones produced by the mechanism, as shown in the plots in Figure 6.
There are apparent anatomical differences between individuals that can affect the phalanges’ ROM. Specifically, in this study, two subjects have very different ROM. While subjects one and two almost have the same theoretical and experimental movement ranges, subject two has a wider experimental ROM than the theoretical one. Addressing these anatomical differences could be an area of opportunity in order to adapt each mechanism for each individual better.
Regarding how this work compares to previous ones, Table 3 summarizes the advantages of the proposed mechanism over other similar works in the literature.

Table 3.
Comparison between different works and the one presented in this document.
The first advantage is that the proposed mechanism has a double action, which can actively assist in flexion and extension motions. In contrast, other works only assist with flexion or extension but not both. On the same topic, some devices are passive, such as the one proposed in [14,33]. Passive mechanisms refer to the ones that have no accurate control of the patient’s movements; they provide only a limited number of rehabilitation exercises and cannot be controlled in real-time.
The proposed design has the advantage over several other models due to the increase in the ROM of each articulation on the index finger. It has a better ROM than most rehabilitation gloves shown in Table 3; only the work performed in [14] has equal ROM at PIP articulation. This increase in the ROM is, in part, thanks to the use of a mechanism that used virtual centers, which can be observed in Figure 1(Om, Od) and Figure 2(Op). Further, the 3D design produced by the parametric model contributes to the maximum ROM angles for each patient. The use of virtual centers made it possible to avoid a more cumbersome design.
The use of virtual centers would allow for a more versatile rehabilitation glove in the future, as the only way there could be a DOF for each finger at the coronal plane is by using these virtual centers because the MCP articulations are contained within the palm’s muscles. Therefore, it is impossible to use an independent hinge on each MCP articulation.
The type of mechanism used to transmit motion in this work, mechanical linkages with cams, also has advantages over other mechanisms used in different investigations. This work’s mechanism can possibly transmit motion during the contraction and extension motions of the finger using the same mechanical elements; in contrast, a cable-driven mechanism, such as in [14], cannot do this. Compared to soft robotic gloves such as [34] or cable-driven mechanisms [14], which cannot assure a stable position of the fingers, the design proposed here is rigid, thus having more capability in keeping finger location consistent. Some gloves use rigid bar mechanisms [33], but these designs, unlike those proposed here, are often bulky and have to use hinges located at the physical finger’s articulations.
Concerning the number of DOFs used in this work, two were chosen because this allows for replicating most of the finger’s natural movements on the sagittal plane. In comparison to systems that have only one DOF for each finger, such as [14,20,33,34], there is much more variety in exercises that this mechanism can replicate. While using one DOF for each finger allows only a single curve to be followed, using two DOFs allows for an entire family of curves that live on two dimensions, opening the possibilities of rehabilitation exercises the patient could perform. These work areas are personalized through the parametrization model, and thus each patient has their own work area, contrary to most rehabilitation gloves in existence, which have just one curve (in the case of just one DOF) or the work areas are fixed. The work areas for each subject can be seen in Figure 7. These work areas represent the universe of points that the tip of the patient’s finger can take; each patient has a whole family of curves that live within this space, and all these curves represent a broad range possibility of rehabilitation exercises. In this work, one DOF of the exoskeleton transmitted movement to the distal and middle phalanx as this move is naturally due to the tendons’ anatomy and attachment points. Currently, there is a simple interface that allows the finger to move from four positions: claw, proximal pointing down, extended, and flexed finger. Nevertheless, the rehabilitation exercises are not limited to these positions, and more complex rehabilitation routines could be implemented in the system thanks to its flexibility in the future.
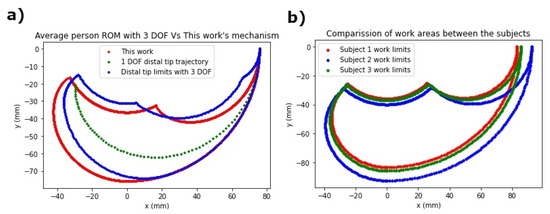
Figure 7.
(a) Work area comparison between subjects. (b) Average work area with 3 DOF vs. work area of this mechanism using an index finger of 73 mm.
In Figure 7a, the variation in the patients’ work areas according to the parametric model can be appreciated; this means that for each patient, the ROM is better suited individually, which is a great advantage because it allows for a wider variety of rehabilitation compared to fixed rehabilitation gloves.
While there are systems with three DOFs for each finger, such as the one presented in [35], or a more comprehensive work area, they have the disadvantage of often being bulky and adding difficulty in design, manufacture, and control, and also increasing the cost of the system. Moreover, the difference in the work area is not too significant. An example of the work area that may be lost by using 2 DOF compared to a 3 DOF mechanism is shown in Figure 7b. For this comparison, an index finger of 73 mm in length is used as a reference and the ROM for each articulation was determined using the average ROM stated in [28].
It is apparent from Figure 7b that, in some parts, the 3 DOF model has an advantage over the mechanism of this work. Nevertheless, because this mechanism has more ROM in the MCP and DIP joints, it also has some work areas that the 3 DOF model cannot reach. The green dotted line in Figure 7b represents the only trajectory that a 1 DOF finger rehabilitation mechanism could follow; this is a very limiting factor on these kinds of devices that trade the simplicity of the mechanism over the versatility and variety of rehabilitation exercises.
4. Conclusions
It could be said that several opportunity areas mentioned in the introduction were addressed during this work. Some opportunity areas improved in this work are the increase in the variety of possible rehabilitation exercises, the possibility of ADLs reproduction during therapy sessions, the reduction in manufacturing and design time and costs, and the customization of the rehabilitation mechanism for each individual. By using two DOFs, a 2D space of trajectories is possible, and also, by increasing the ROM of each phalanx, the variety of possible rehabilitation exercises is significantly improved compared to one DOF rehabilitation device or system with significant limitations in the phalanges’ ROM. To see if there is a contribution to the ROM increase, we can observe previous, similar models that also proposed a mechanism that used virtual centers [20]. The proposed mechanism by [20] has a ROM of 55° in the MCP articulation and 65° at the PIP articulation. Comparing the ROM of previous similar designs, it can be observed that there is, in fact, an increase in these values; the proposed mechanism in this work reached at least 85° for the DIP joint, 90° for the PIP joint, and in the case of the MCP joint, the range is increased to 90°. The use of rigid bar mechanisms allows for a precise, controlled motion that will ensure consistency in rehabilitation routines. All of the contributions mentioned in this section aim to increase the chance of successful rehabilitation for the patient and reduce the time it takes to regain the mobility of their finger articulations. Regarding the ongoing research being made, the most critical points are: validate the model using more test subjects, test for the patient’s ROM recovery after therapy using this device, and reproduce the index model for the rest of the fingers to create a whole hand exoskeleton.
Author Contributions
Conceptualization, I.A.N.-T., M.C.E.-E., H.C.-C. and A.E.F.-G.; methodology, I.A.N.-T., M.C.E.-E., H.C.-C. and A.E.F.-G.; software, I.A.N.-T.; validation, I.A.N.-T. and M.C.E.-E.; formal analysis, I.A.N.-T., M.C.E.-E. and H.C.-C.; investigation, I.A.N.-T., M.C.E.-E., H.C.-C. and A.E.F.-G.; resources, I.A.N.-T. and M.C.E.-E.; data curation, I.A.N.-T.; writing—original draft preparation, I.A.N.-T.; writing—review and editing, I.A.N.-T., M.C.E.-E., H.C.-C. and A.E.F.-G.; visualization, I.A.N.-T., M.C.E.-E., H.C.-C. and A.E.F.-G.; supervision, M.C.E.-E., H.C.-C. and A.E.F.-G.; project administration, I.A.N.-T. and M.C.E.-E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding except for a scholarship from the Mexican government institution CONACyT for the doctoral studies of Iyari Alejandro Nava-Téllez.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Datasets are available at the following link: https://drive.google.com/drive/folders/1Vpk6Y76zyhonWMpko1ONieMANoekgAjp?usp=sharing.
Acknowledgments
The authors give thanks for the motion capture equipment and installations provided by the representatives of Vicon in México (HCG). Thanks to Carlos Vilchis for allowing the use of his MOCAP laboratory and equipment. Thanks to Andrea Bueyes and Carlos Soriano for the help provided during the motion capture sessions and for the technical support regarding this matter. Iyari Alejandro Nava-Téllez thanks the Mexican governmental institution CONACyT and Instituto Tecnologico y de Estudios Superiores de Monterrey for its support through a doctoral studies scholarship.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| CAD | Computer-Aided Design |
| ADL | Activities of Daily Living |
| DOF | Degree of Freedom |
| ROM | Range of Motion |
| MCP | Metacarpophalangeal |
| PIP | Proximal Interphalangeal |
| DIP | Distal Interphalangeal |
| MOCAP | MOtion CApture |
| FDM | Fused Deposition Modeling |
Appendix A. Direct Kinematic Model in Detail
In this appendix, the direct kinematic model is presented in detail so the reader can see how it was solved step by step.
Vector represents the distal phalanx, while vector is the middle phalanx; thus if the parametric model is incorporated within the kinematic equations, then can be represented as: . Therefore, Equations (A3) and (A4) are rewritten as Equations (A5) and (A6).
As it can be seen from Equations (A1) to (A10), there are equations in which two angles are unknown. Therefore, the middle angle theorem is used in order to solve for the unknowns. Initially, it may seem as if there are not enough equations to solve the system, but in reality, there are two constant relationships: one between angles and and another between and . This relationship is defined by the mechanical design; it is fixed, and is represented by Equations (5) and (6).
After performing the corresponding algebra and solving for all the unknowns, the following Equations (A11)–(A29) are obtained.
where A, B, C are given by:
and by:
Appendix B. Inverse Kinematic Model in Detail
In this appendix, the inverse kinematic model is presented in detail so the reader can see how it was solved step by step.
where and , are given by:
and , and are equal to:
Next, angle is found by using Equation (A39).
References
- Stilli, A.; Cremoni, A.; Bianchi, M.; Ridolfi, A.; Gerii, F.; Vannetti, F.; Wurdemann, H.A.; Allotta, B.; Althoefer, K. AirExGlove—A novel pneumatic exoskeleton glove for adaptive hand rehabilitation in post-stroke patients. In Proceedings of the 2018 IEEE International Conference on Soft Robotics (RoboSoft), Livorno, Italy, 24–28 April 2018; pp. 579–584. [Google Scholar] [CrossRef]
- Mcconnell, A.; Moioli, R.; Brasil, F.; Vallejo, M.; Corne, D.; Vargas, P.; Stokes, A. Robotic devices and brain-machine interfaces for hand rehabilitation post-stroke. J. Rehabil. Med. 2017, 49, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Yue, Z.; Zhang, X.; Wang, J. Hand Rehabilitation Robotics on Poststroke Motor Recovery. Behav. Neurol. 2017, 2017, 3908135. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Meng, Q.; Meng, Q.; Li, X.; Yu, H. Design and Development of a Portable Exoskeleton for Hand Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2376–2386. [Google Scholar] [CrossRef] [PubMed]
- Khalid, S.; Alnajjar, F.; Gochoo, M.; Renawi, A.; Shimoda, S. Robotic assistive and rehabilitation devices leading to motor recovery in upper limb: A systematic review. Disabil. Rehabil. Assist. Technol. 2021, 1–15. [Google Scholar] [CrossRef]
- Prange, G.; Jannink, M.; Groothuis-Oudshoorn, C.; Hermens, H.; IJzerman, M. Systematic review of the effect of robot-aided therapy on recovery of the hemiparetic arm after stroke. J. Rehabil. Res. Dev. 2006, 43, 171–184. [Google Scholar] [CrossRef]
- Gonzalez, A.; Garcia, L.; Kilby, J.; McNair, P. Robotic devices for paediatric rehabilitation: A review of design features. BioMed. Eng. OnLine 2021, 20, 89. [Google Scholar] [CrossRef]
- Burgar, C.; Lum, P.; Shor, P.; der Loos, H.M.V. Development of robots for rehabilitation therapy: The Palo Alto VA/Stanford experience. J. Rehabil. Res. Dev. 2000, 376, 663–673. [Google Scholar]
- Colombo, R.; Pisano, F.; Micera, S.; Mazzone, A.; Delconte, C.; Carrozza, M.C.; Dario, P.; Minuco, G. Robotic Techniques for Upper Limb Evaluation and Rehabilitation of Stroke Patients. IEEE Trans. Neural Syst. Rehabil. Eng. A Publ. IEEE Eng. Med. Biol. Soc. 2005, 13, 311–324. [Google Scholar] [CrossRef]
- Qian, Z.; Bi, Z. Recent Development of Rehabilitation Robots. Adv. Mech. Eng. 2014, 7, 563062. [Google Scholar] [CrossRef]
- Ben Abdallah, I.; Bouteraa, Y.; Rekik, C. Design and development of 3D printed myoelectric robotic exoskeleton for hand rehabilitation. Int. J. Smart Sens. Intell. Syst. 2017, 10, 341–366. [Google Scholar] [CrossRef]
- Andriske, L.; Verikios, D.; Hitch, D. Patient and Therapist Experiences of the SaeboFlex: A Pilot Study. Occup. Ther. Int. 2017, 2017, 5462078. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.; Bitikofer, C.; Sobbi, B.; Perry, J. Design of MobIle Digit Assistive System (MIDAS): A Passive Hand Extension Exoskeleton for Post Stroke Rehabilitation. In Proceedings of the 4th International Symposium on Wearable Robotics, WeRob2018, Pisa, Italy, 16–20 October 2018; pp. 535–539. [Google Scholar] [CrossRef]
- Chiri, A.; Giovacchini, F.; Vitiello, N.; Cattin, E.; Roccella, S.; Vecchi, F.; Carrozza, M.C. HANDEXOS: Towards an exoskeleton device for the rehabilitation of the hand. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 10–15 October 2009; pp. 1106–1111. [Google Scholar] [CrossRef]
- Brokaw, E.; Black, I.; Holley, R.; Lum, P. Hand Spring Operated Movement Enhancer (HandSOME): A Portable, Passive Hand Exoskeleton for Stroke Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Landers, K.; Park, H. Development of a Biomimetic Hand Exotendon Device (BiomHED) for Restoration of Functional Hand Movement Post-Stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 886–898. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; Peppen, R.; Wagenaar, R.; Wood-Dauphinee, S.; Richards, C.; Ashburn, A.; Miller, K.; Lincoln, N.; Partridge, C.; Wellwood, I.; et al. Effects of Augmented Exercise Therapy Time After Stroke: A Meta-Analysis. Stroke 2004, 35, 2529–2539. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Yi, J.; Chen, X.; Liu, Z.; Wang, Z. BCL-13: A 13-DOF Soft Robotic Hand for Dexterous Grasping and In-hand Manipulation. IEEE Robot. Autom. Lett. 2018, 3, 3379–3386. [Google Scholar] [CrossRef]
- Susanto, E.; Tong, R.K.Y.; Ockenfeld, C.; Ho, N.S. Efficacy of robot-assisted fingers training in chronic stroke survivors: A pilot randomized-controlled trial. J. Neuroeng. Rehabil. 2015, 12, 1–9. [Google Scholar] [CrossRef]
- Ho, N.S.; Tong, K.Y.; Hu, X.; Fung, K.; Wei, X.; Rong, W.; Susanto, E. An EMG-driven exoskeleton hand robotic training device on chronic stroke subjects: Task training system for stroke rehabilitation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011. [Google Scholar]
- Cafolla, D. A personalized flexible exoskeleton for finger rehabilitation: A conceptual design. In Advances in Mechanism and Machine Science; Uhl, T., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 73–82. [Google Scholar]
- Case, D.; Ross, A. Sex Determination from Hand and Foot Bone Lengths. J. Forensic Sci. 2007, 52, 264–270. [Google Scholar] [CrossRef]
- Hu, D.; Xiong, C.H.; Liu, M.J. Exploring the existence of better hands for manipulation than the human hand based on hand proportions. J. Theor. Biol. 2018, 440, 100–111. [Google Scholar] [CrossRef]
- Buryanov, A.; Kotiuk, V. Proportions of Hand Segments. Int. J. Morphol. 2010, 28, 755–758. [Google Scholar] [CrossRef]
- Hamilton, R.; Dunsmuir, R. Radiographic Assessment of the Relative Lengths of the Bones of the Fingers of the Human Hand. J. Hand Surg. 2002, 27, 546–548. [Google Scholar] [CrossRef]
- Thompson, D. Biomechanics of the Hand. 2001. Available online: https://ouhsc.edu/bserdac/dthompso/web/namics/hand.htm (accessed on 5 November 2020).
- Becker, J.; Thakor, N. A study of the range of motion of human fingers with application to anthropomorphic designs. IEEE Trans. Biomed. Eng. 1988, 35, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Hume, M.; Gellman, H.; Mckellop, H.; Brumfield, R. Functional range of motion of the joints of the hand. J. Hand Surg. 1990, 152, 240–243. [Google Scholar] [CrossRef]
- Littler, J. On The Adaptability of Man’s Hand (with Reference to the Equiangular Curve). Hand 1973, 5, 187–191. [Google Scholar] [CrossRef]
- Johnson, P.W.; Blackstone, J.M. Children and gender—Differences in exposure and how anthropometric differences can be incorporated into the design of computer input devices. Scand. J. Work. Environ. Health 2007, 33, 26–32. [Google Scholar]
- Gillam, L.; McDonald, R.; Ebling, F.; Mayhew, T. Human 2D (index) and 4D (ring) finger lengths and ratios: Cross-sectional data on linear growth patterns, sexual dimorphism and lateral asymmetry from 4 to 60 years of age. J. Anat. 2008, 213, 325–335. [Google Scholar] [CrossRef]
- Singh, B.K. Assessment of stature from hand and phalange length. Int. J. Med. Health Res. 2017, 3, 136–137. [Google Scholar]
- Bataller, A.; Cabrera, J.; Clavijo, M.; Castillo, J.J. Evolutionary synthesis of mechanisms applied to the design of an exoskeleton for finger rehabilitation. Mech. Mach. Theory 2016, 105, 31–43. [Google Scholar] [CrossRef]
- Polygerinos, P.; Lyne, S.; Wang, Z.; Nicolini, L.F.; Mosadegh, B.; Whitesides, G.; Walsh, C. Towards a soft pneumatic glove for hand rehabilitation. In Proceedings of the 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems, Tokyo, Japan, 3–7 November 2013; pp. 1512–1517. [Google Scholar]
- Ali, H.F.; Khan, A.M.; Baek, H.; Shin, B.; Kim, Y. Modeling and control of a finger-like mechanism using bending shape memory alloys. Microsyst. Technol. 2021, 27, 2481–2492. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).