The Influence of Badminton on the Anterior Stability of the Knee in Badminton Players between 10 and 12 Years of Age
Abstract
1. Introduction
2. Materials and Methods
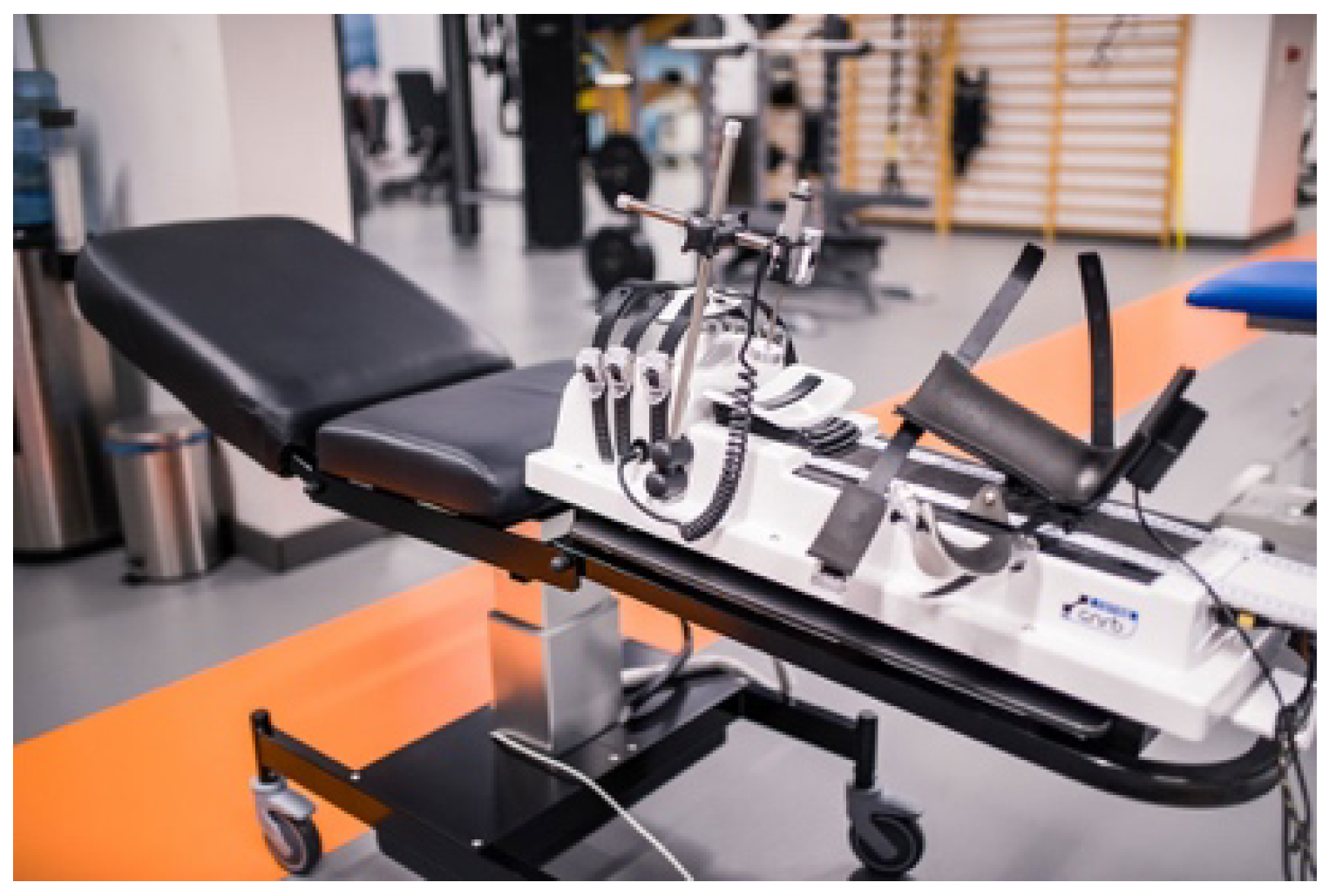
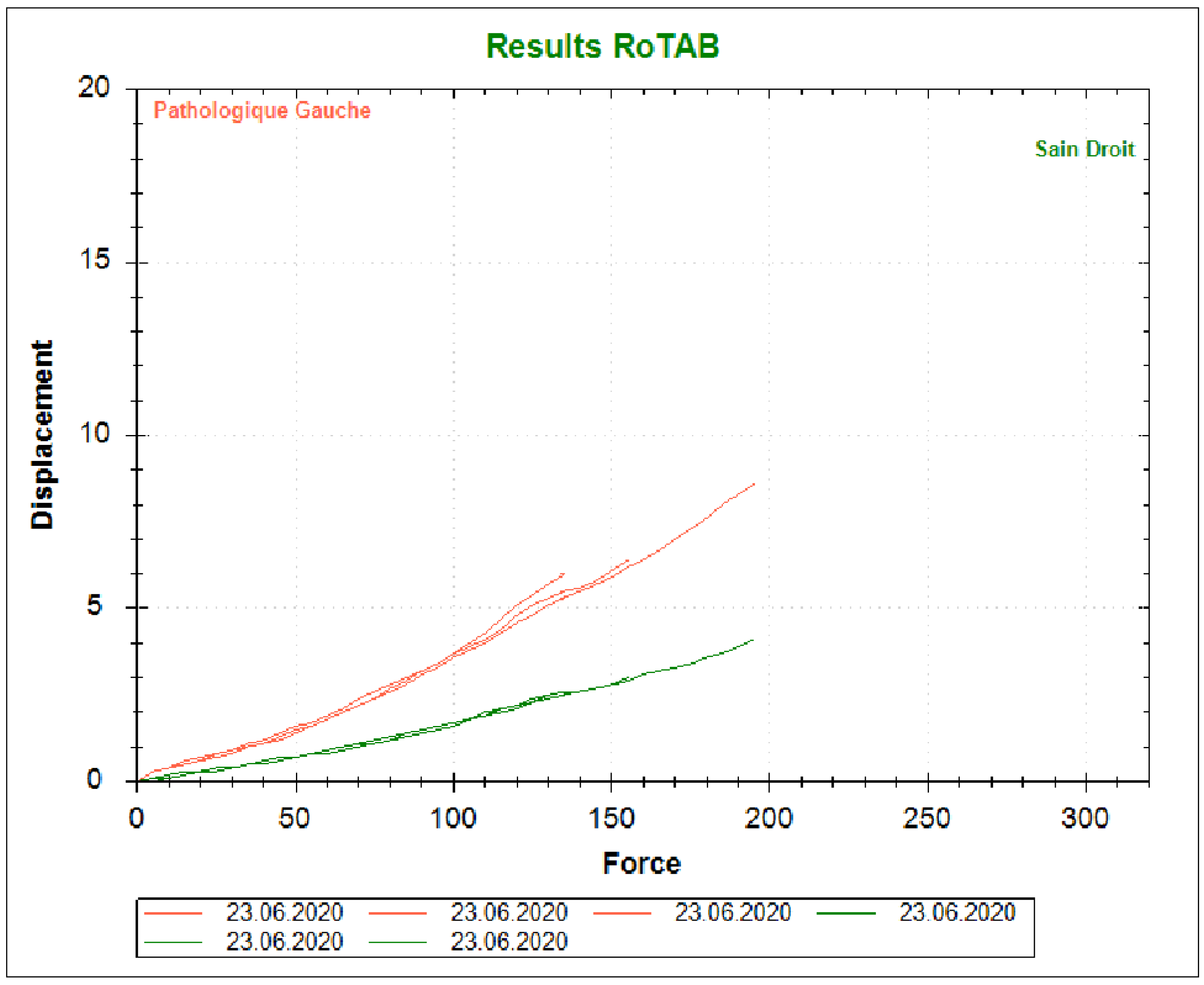
2.1. Materials
2.2. Methods
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kimura, Y.; Ishibashi, Y.; Tsuda, E.; Yamamoto, Y.; Tsukada, H.; Toh, S. Mechanisms for Anterior Cruciate Ligament Injuries in Badminton. Br. J. Sports Med. 2010, 44, 1124–1127. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, G.M.; van Tol, A.W.; Bergink, A.P.; Belo, J.N.; Bernsen, R.M.D.; Reijman, M.; Pols, H.A.P.; Bierma-Zeinstra, S.M.A. Association between Valgus and Varus Alignment and the Development and Progression of Radiographic Osteoarthritis of the Knee. Arthritis Rheum. 2007, 56, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Elias, J.J.; Cech, J.A.; Weinstein, D.M.; Cosgrea, A.J. Reducing the Lateral Force Acting on the Patella Does Not Consistently Decrease Patellofemoral Pressures. Am. J. Sports Med. 2004, 32, 1202–1208. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S., Jr.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, C.E.; Beattie, P.F.; Sacko, R.S.; Hand, A. Risk Factors Associated With Non-Contact Anterior Cruciate Ligament Injury: A Systematic Review. Int. J. Sports Phys. Ther. 2018, 13, 575. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Paterno, M.v.; Quatman, C.E. Mechanisms, Prediction and Prevention of ACL Injuries: Cut Risk with Three Sharpened and Validated Tools. J. Orthop. Res. 2016, 34, 1843–1855. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Schmitz, R.J.; Nguyen, A.D.; Chaudhari, A.M.; Padua, D.A.; McLean, S.G.; Sigward, S.M. ACL Research Retreat V: An Update on ACL Injury Risk and Prevention, March 25–27, 2010, Greensboro, NC. J. Athl. Train. 2010, 45, 499–508. [Google Scholar] [CrossRef]
- Kurihara, Y.; Matsumura, M.; Ohsugi, H.; Kawabe, N.; Matsuda, T. Survey of Sports Injuries of Elementary School Badminton Players. Rigakuryoho Kagaku 2018, 33, 879–882. [Google Scholar] [CrossRef]
- Hu, X.; Li, J.X.; Hong, Y.; Wang, L. Characteristics of Plantar Loads in Maximum Forward Lunge Tasks in Badminton. PLoS ONE 2015, 10, e0137558. [Google Scholar] [CrossRef]
- Huang, M.T.; Lee, H.H.; Lin, C.F.; Tsai, Y.J.; Liao, J.C. How Does Knee Pain Affect Trunk and Knee Motion during Badminton Forehand Lunges? J. Sports Sci. 2014, 32, 690–700. [Google Scholar] [CrossRef]
- Kimura, Y.; Ishibashi, Y.; Tsuda, E.; Yamamoto, Y.; Hayashi, Y.; Sato, S. Increased Knee Valgus Alignment and Moment during Single-Leg Landing after Overhead Stroke as a Potential Risk Factor of Anterior Cruciate Ligament Injury in Badminton. Br. J. Sports Med. 2012, 46, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Jaworski, J.; Lech, G.; Żak, M.; Madejski, E.; Szczepanik, K. The Level of Selected Coordination Abilities in Badminton Players at Various Ages and Sport Skill Levels as Compared to Non-Athletes. Balt. J. Health Phys. Act. 2017, 9, 33–43. [Google Scholar] [CrossRef]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of Non-Contact Anterior Cruciate Ligament Injuries in Soccer Players. Part 1: Mechanisms of Injury and Underlying Risk Factors. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 705–729. [Google Scholar] [CrossRef] [PubMed]
- Sarshin, A.; Mohammadi, S.; Shahrabad, H.; Sedighi, M. The Effects of Functional Fatique on Dynamic Postural Control of Badminton Players. Biol. Exerc. 2011, 7. [Google Scholar]
- Kimura, Y.; Tsuda, E.; Hiraga, Y.; Maeda, S.; Sasaki, S.; Sasaki, E.; Fujita, Y.; Ishibashi, Y.; Makino, M. Trunk motion and muscular strength affect knee valgus moment during single-leg landing after overhead stroke in badminton. Br. J. Sports Med. 2014, 48, 620. [Google Scholar] [CrossRef]
- Reeves, J.; Hume, P.; Gianotti, S.; Wilson, B.; Ikeda, E. A Retrospective Review from 2006 to 2011 of Lower Extremity Injuries in Badminton in New Zealand. Sports 2015, 3, 77–86. [Google Scholar] [CrossRef]
- Sasaki, S.; Nagano, Y.; Ichikawa, H. Loading Differences in Single-Leg Landing in the Forehand- and Backhand-Side Courts after an Overhead Stroke in Badminton: A Novel Tri-Axial Accelerometer Research. J. Sports Sci. 2018, 36, 2794–2801. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Dudley, W.N.; Kong, Y. Identifying Multiplanar Knee Laxity Profiles and Associated Physical Characteristics. J. Athl. Train. 2012, 47, 159–169. [Google Scholar] [CrossRef]
- Klouche, S.; Lefevre, N.; Cascua, S.; Herman, S.; Gerometta, A.; Bohu, Y. Diagnostic Value of the GNRB® in Relation to Pressure Load for Complete ACL Tears: A Prospective Case-Control Study of 118 Subjects. Orthop. Traumatol. Surg. Res. 2015, 101, 297–300. [Google Scholar] [CrossRef]
- Cinar-Medeni, O.; Baltaci, G.; Bayramlar, K.; Yanmis, I. Core Stability, Knee Muscle Strength, and Anterior Translation Are Correlated with Postural Stability in Anterior Cruciate Ligament-Reconstructed Patients. Am. J. Phys. Med. Rehabil. 2015, 94, 280–287. [Google Scholar] [CrossRef]
- Zazulak, B.T.; Hewett, T.E.; Reeves, N.P.; Goldberg, B.; Cholewicki, J. Deficits in Neuromuscular Control of the Trunk Predict Knee Injury Risk: A Prospective Biomechanical-Epidemiologic Study. Am. J. Sports Med. 2007, 35, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Biabanimoghadam, M.; Motealleh, A.; Cowan, S.M. Core Muscle Recruitment Pattern during Voluntary Heel Raises Is Different between Patients with Patellofemoral Pain and Healthy Individuals. Knee 2016, 23, 382–386. [Google Scholar] [CrossRef]
- Myer, G.D.; Ford, K.R.; Hewett, T.E. New Method to Identify Athletes at High Risk of ACL Injury Using Clinic-Based Measurements and Freeware Computer Analysis. Br. J. Sports Med. 2011, 45, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Youdas, J.W.; Hartman, J.P.; Murphy, B.A.; Rundle, A.M.; Ugorowski, J.M.; Hollman, J.H. Magnitudes of Muscle Activation of Spine Stabilizers, Gluteals and Hamstrings during Supine Bridge to Neutral Position. Physiother. Theory Pract. 2015, 31, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Nguyen, A.D.; Levine, B.J. The Relationship between Lower Extremity Alignment Characteristics and Anterior Knee Joint Laxity. Sports Health 2009, 1, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Fleming, B.C.; Peura, G.D.; Abate, J.A.; Beynnon, B.D. Accuracy and Repeatability of Roentgen Stereophotogrammetric Analysis (RSA) for Measuring Knee Laxity in Longitudinal Studies. J. Biomech. 2001, 34, 1355–1359. [Google Scholar] [CrossRef]
- Blackburn, J.T.; Norcross, M.F.; Cannon, L.N.; Zinder, S.M. Hamstrings Stiffness and Landing Biomechanics Linked to Anterior Cruciate Ligament Loading. J. Athl. Train. 2013, 48, 764–772. [Google Scholar] [CrossRef]
- Adamczyk, J.G.; Pepłowski, M.; Boguszewski, D.; Białoszewski, D. Ocena funkcjonalna zawodników uprawiających podnoszenie ciężarów z zastosowaniem Testu Functional Movement Screen./Functional evaluation of competitors practising weightlifting with using Functional Movement Screen Test. Pol. J. Sports Med./Med. Sports 2012, 28, 267–276. [Google Scholar]
- Zahradnik, D.; Jandacka, D.; Farana, R.; Uchytil, J.; Hamill, J. Identification of Types of Landings after Blocking in Volleyball Associated with Risk of ACL Injury. Eur. J. Sport Sci. 2017, 17, 241–248. [Google Scholar] [CrossRef]
- Clifton, D.R.; Grooms, D.R.; Onate, J.A. Overhead deep squat performance predicts functional movement screenTM score. Int. J. Sports Phys. Ther. 2015, 10, 622. [Google Scholar]
- Kiesel, K.; Plisky, P.; Butler, R. Functional Movement Test Scores Improve Following a Standardized Off-Season Intervention Program in Professional Football Players. Scand. J. Med. Sci. Sports 2011, 21, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Rzepka, R. Wykorzystanie treningu funkcjonalnego w przygotowaniu motorycznym koszykarza. In Współczesny System Szkolenia W Zespołowych Grach Sportowych; Zając, A., Chmura, J., Eds.; AWF Katowice: Katowice, Poland, 2016. [Google Scholar]
- Cook, G. Functional Movement Systems. 2011. Available online: https://www.stancountysafety.org/sites/default/files/webform/pdf-movement-functional-movement-systems-screening-assessment-cor-gray-cook-pdf-download-free-book-301b564.pdf (accessed on 15 May 2019).
- Yıldız, S. Relationship between Functional Movement Screen and Athletic Performance in Children Tennis Players. Univers. J. Educ. Res. 2018, 6, 1647–1651. [Google Scholar] [CrossRef]
- Kuszewski, M. Kontuzje i urazy sportowe-geneza i profilaktyka. In Współczesny System Szkolenia W Zespołowych Grach Sportowych; Zając, A., Chmura, J., Eds.; AWF Katowice: Katowice, Poland, 2016. [Google Scholar]
- Flynn, J.M.; Mackenzie, W.; Kolstad, K.; Sandifer, E.; Jawad, A.F.; Galinat, B. Objective Evaluation of Knee Laxity in Children. J. Pediatr. Orthop. 2000, 20, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Mouton, C.; Theisen, D.; Meyer, T.; Agostinis, H.; Nührenbörger, C.; Pape, D.; Seil, R. Combined Anterior and Rotational Knee Laxity Measurements Improve the Diagnosis of Anterior Cruciate Ligament Injuries. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2859–2867. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Schmitz, R.J.; Cone, J.R.; Henson, R.A.; Montgomery, M.M.; Pye, M.L.; Tritsch, A.J. Changes in Fatigue, Multiplanar Knee Laxity, and Landing Biomechanics during Intermittent Exercise. J. Athl. Train. 2015, 50, 486–497. [Google Scholar] [CrossRef]
- Anderson, B.E.; Neumann, M.L.; Huxel Bliven, K.C. Functional Movement Screen Differences between Male and Female Secondary School Athletes. J. Strength Cond. Res. 2015, 29, 1098–1106. [Google Scholar] [CrossRef]
| Variable | Experimental Group (N = 68) | Control Group (N = 48) | p |
|---|---|---|---|
| Gender | |||
| Boys | 32 (47.1%) | 23 (47.9%) | 0.927 |
| Girls | 36 (52.9%) | 25 (52.1%) | |
| Age 1 | 10.2 ± 0.4 | 10.4 ± 0.5 | 0.999 |
| Body height (cm) | 143.6 ± 3.4 | 141.5 ± 4.2 | 0.010 * |
| Body weight (kg) | 39.2 ± 1.4 | 43.9 ± 3.5 | 0.001 * |
| BMI (kg/m2) | 17.9 ± 0.6 | 20.1 ± 1.6 | 0.001 * |
| Variable | Measurements | Experimental Group (N = 68) | Control Group (N = 48) | p (E-C) | r (E-C) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | Me | p (I-II) | r (I-II) | M | SD | Me | p (I-II) | r (I-II) | ||||
| Translation R | I | 7.48 | 1.89 | 7.25 | 0.309 | 0.12 | 6.84 | 1.75 | 6.80 | 0.010 * | 0.37 | 0.120 | 0.14 |
| II | 7.44 | 1.67 | 7.10 | 7.33 | 1.55 | 7.45 | 0.864 | 0.02 | |||||
| Translation L | I | 7.26 | 1.96 | 7.20 | 0.415 | 0.10 | 6.99 | 1.54 | 7.15 | 0.066 | 0.27 | 0.497 | 0.06 |
| II | 7.61 | 1.56 | 7.60 | 7.25 | 1.36 | 7.15 | 0.250 | 0.11 | |||||
| Stability index | I | 1.00 | 0.93 | 0.70 | 0.015 * | 0.29 | 0.73 | 0.59 | 0.60 | 0.757 | 0.04 | 0.213 | 0.12 |
| II | 0.82 | 0.93 | 0.50 | 0.73 | 0.51 | 0.60 | 0.550 | −0.06 | |||||
| FMS | I | 14.21 | 1.96 | 14.00 | 0.006 * | 0.33 | 13.38 | 1.91 | 13.50 | 0.0001 * | 0.61 | 0.045 * | 0.19 |
| II | 14.60 | 2.10 | 14.00 | 14.15 | 1.86 | 14.00 | 0.210 | 0.12 | |||||
| Measurement I | Measurement II | Stability II-I | Stability II-I (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Translation R | Translation L | Stability | Translation R | TranslationL | Stability | |||
| Experimental group (N = 68) | ||||||||
| FMS I | 0.09 | 0.06 | 0.02 | 0.10 | 0.09 | −0.10 | −0.07 | −0.17 |
| FMS II | 0.19 | 0.24 * | 0.01 | 0.13 | 0.19 | −0.04 | 0.00 | −0.09 |
| FMS II-I | 0.14 | 0.32 * | −0.05 | 0.05 | 0.14 | 0.14 | 0.22 | 0.23 |
| FMS II-I (%) | 0.13 | 0.30 * | −0.06 | 0.04 | 0.13 | 0.14 | 0.23 | 0.25 * |
| Control group (N = 48) | ||||||||
| FMS I | −0.23 | −0.26 | 0.09 | −0.08 | −0.26 | 0.18 | 0.08 | 0.04 |
| FMS II | −0.13 | −0.18 | 0.04 | 0.01 | −0.16 | 0.21 | 0.12 | 0.08 |
| FMS II-I | 0.23 | 0.11 | −0.05 | 0.11 | 0.04 | 0.04 | 0.05 | 0.05 |
| FMS II-I (%) | 0.29 * | 0.17 | −0.05 | 0.16 | 0.10 | 0.02 | 0.04 | 0.05 |
| Body Height (cm) | Body Weight (kg) | BMI | |
|---|---|---|---|
| Experimental group | |||
| Stability II-I | 0.10 | −0.04 | −0.04 |
| Stability II-I (%) | 0.04 | 0.00 | 0.00 |
| FMS II-I | 0.05 | 0.15 | 0.15 |
| FMS II-I (%) | 0.05 | 0.15 | 0.15 |
| Control group | |||
| Stability II-I | −0.21 | −0.01 | −0.01 |
| Stability II-I (%) | −0.22 | −0.03 | −0.03 |
| FMS II-I | −0.18 | −0.03 | −0.03 |
| FMS II-I (%) | −0.20 | 0.00 | 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubasik, W.; Rodak, P.; Przednowek, K.; Kluczniok, K.; Ficek, K. The Influence of Badminton on the Anterior Stability of the Knee in Badminton Players between 10 and 12 Years of Age. Appl. Sci. 2022, 12, 10575. https://doi.org/10.3390/app122010575
Kubasik W, Rodak P, Przednowek K, Kluczniok K, Ficek K. The Influence of Badminton on the Anterior Stability of the Knee in Badminton Players between 10 and 12 Years of Age. Applied Sciences. 2022; 12(20):10575. https://doi.org/10.3390/app122010575
Chicago/Turabian StyleKubasik, Wojciech, Piotr Rodak, Krzysztof Przednowek, Kamila Kluczniok, and Krzysztof Ficek. 2022. "The Influence of Badminton on the Anterior Stability of the Knee in Badminton Players between 10 and 12 Years of Age" Applied Sciences 12, no. 20: 10575. https://doi.org/10.3390/app122010575
APA StyleKubasik, W., Rodak, P., Przednowek, K., Kluczniok, K., & Ficek, K. (2022). The Influence of Badminton on the Anterior Stability of the Knee in Badminton Players between 10 and 12 Years of Age. Applied Sciences, 12(20), 10575. https://doi.org/10.3390/app122010575









