Upper Airway Changes in Diverse Orthodontic Looms: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy for the Identification of Studies
2.2. Study Selection Procedure
2.3. Data Extraction
2.4. Risk of Bias Assessment
2.5. Meta-Analysis
3. Results
3.1. Included Studies
3.2. Study Characteristics
3.3. Clinical Characteristics
3.4. Change in Airway Space
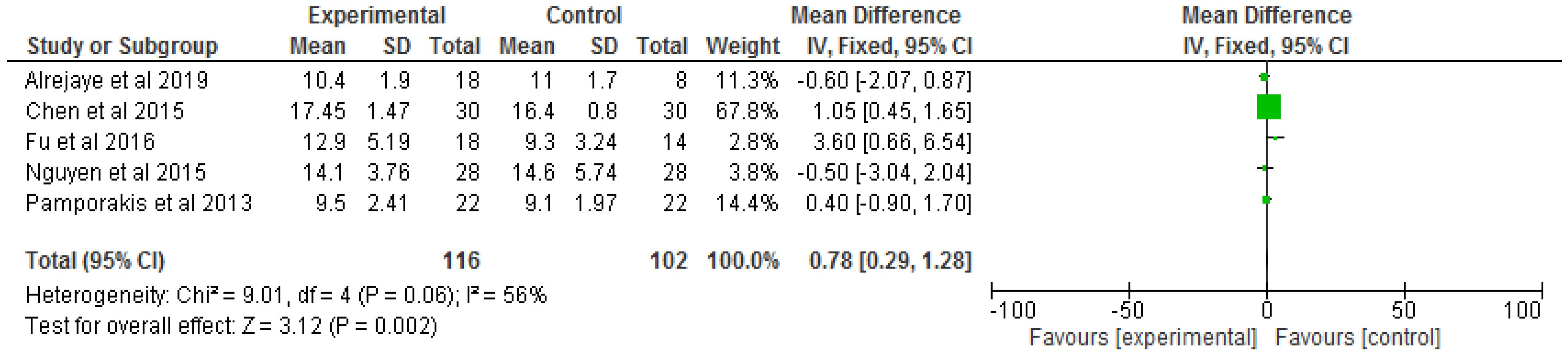
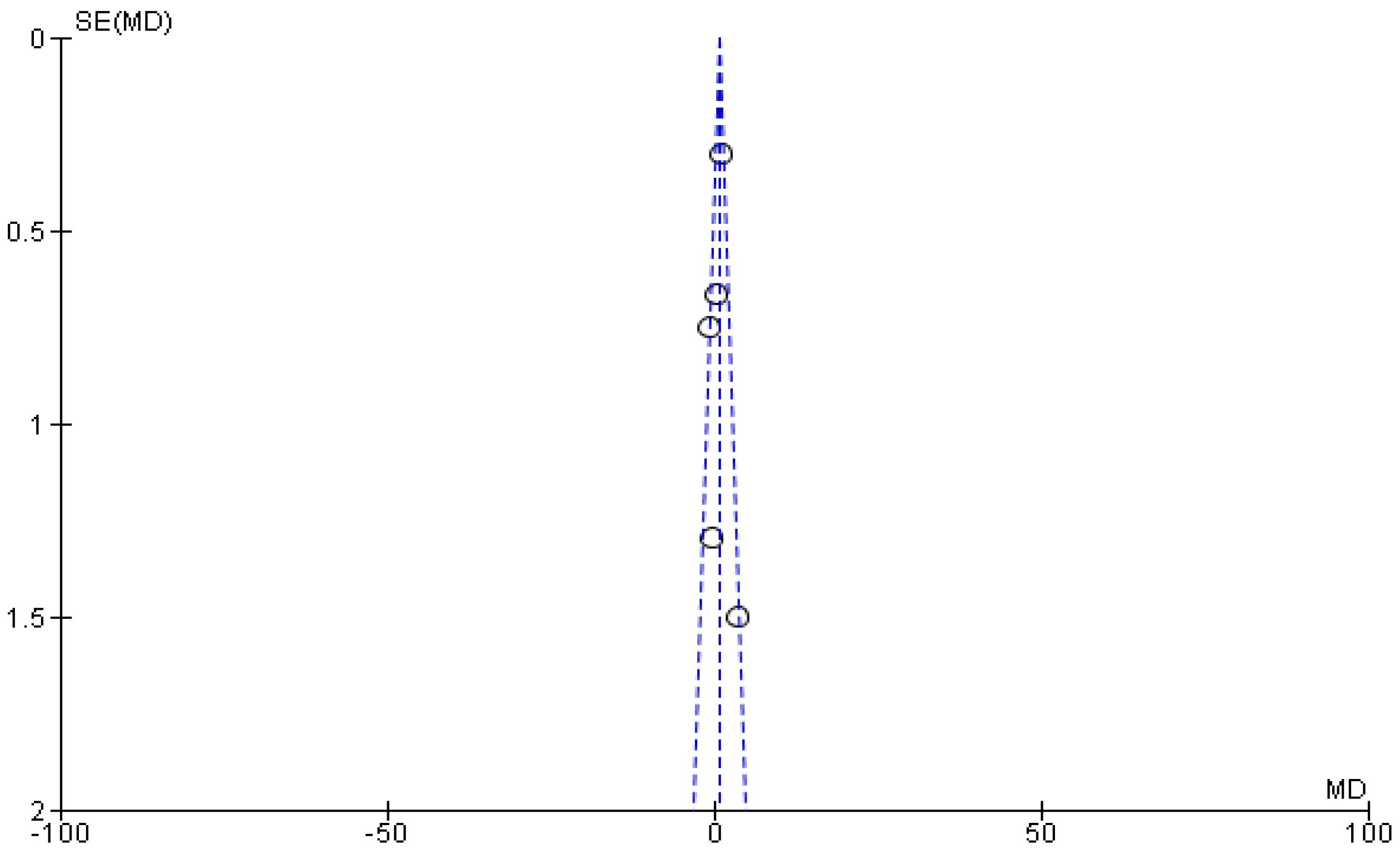
3.4.1. Expansion with Protraction
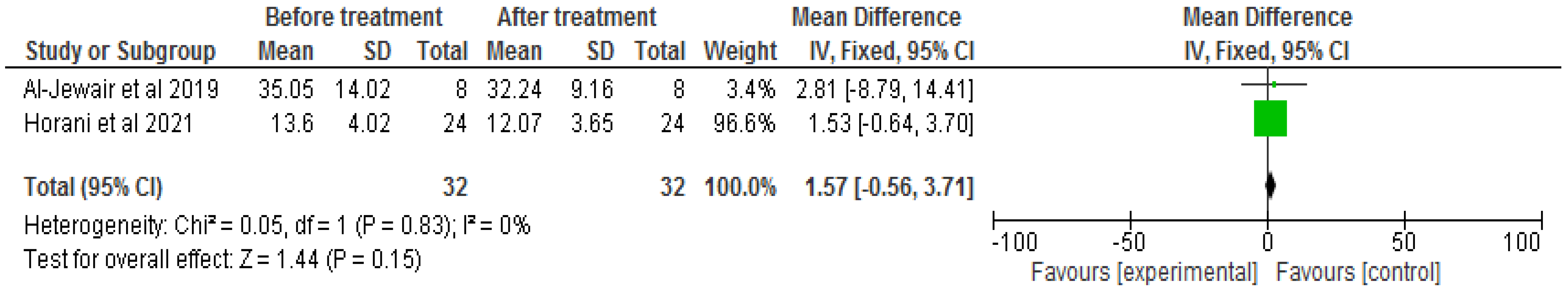
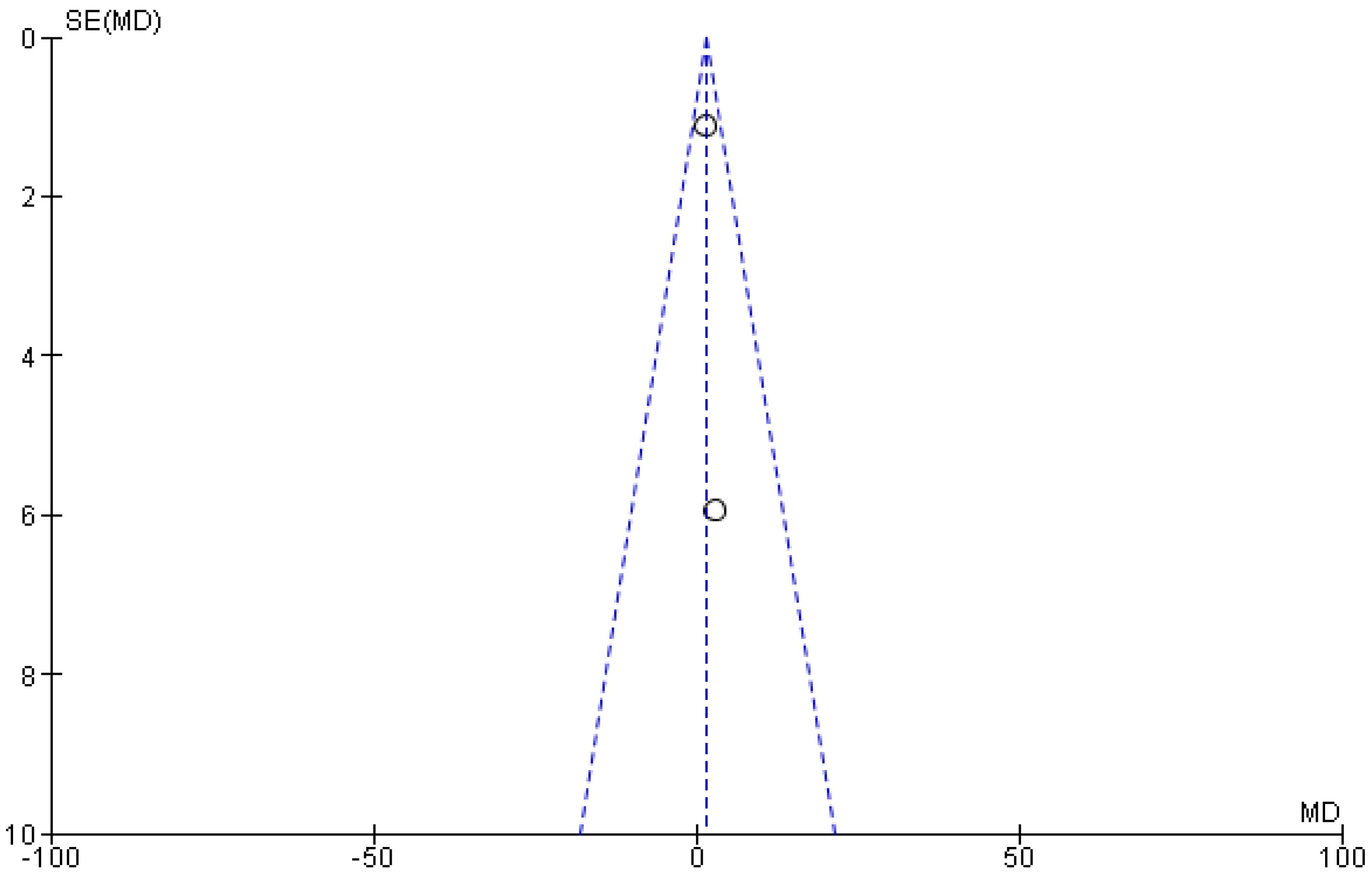
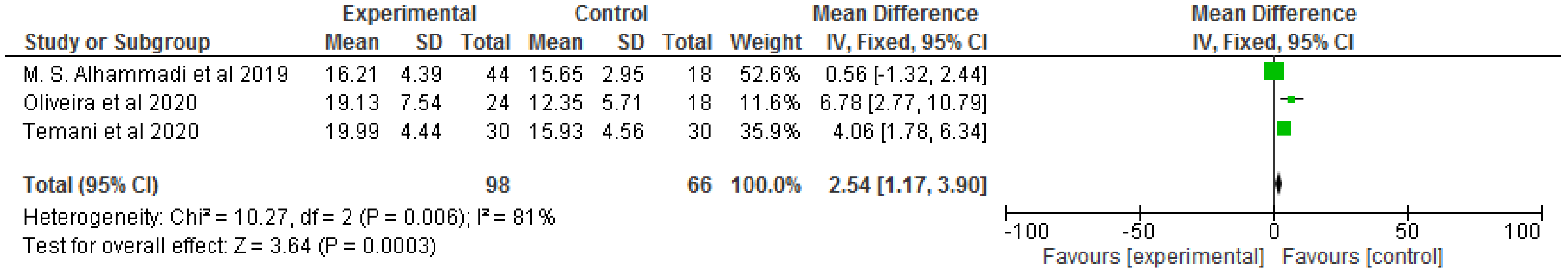
3.4.2. Clean Aligner
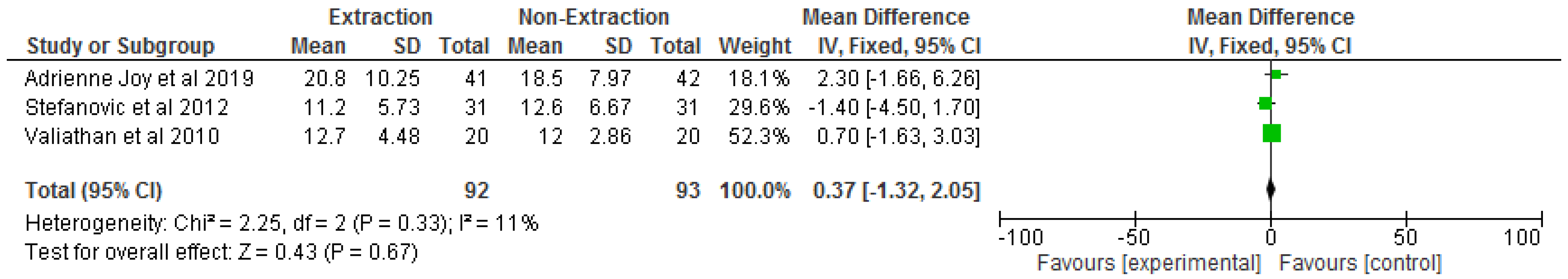
3.4.3. Extraction and Non-Extraction
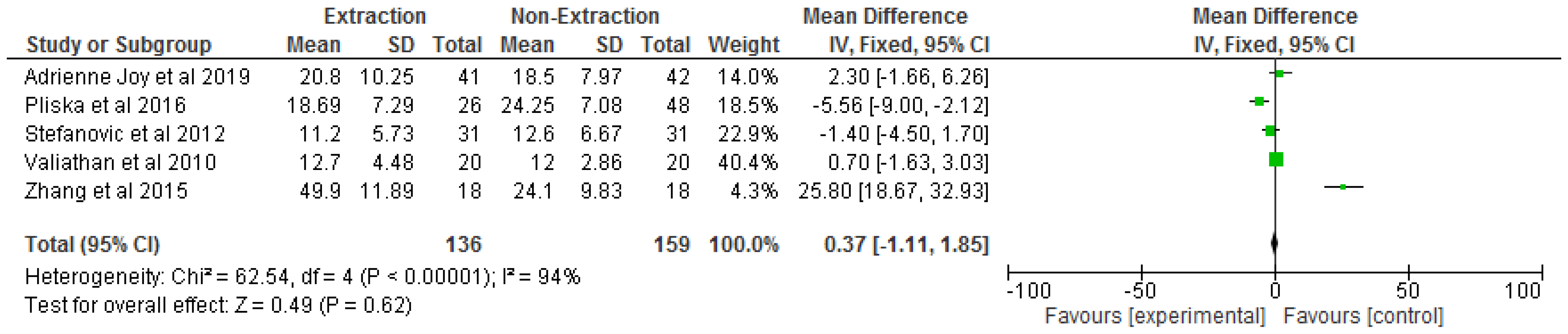
3.4.4. Functional Appliance
3.4.5. Maxillary Expansion
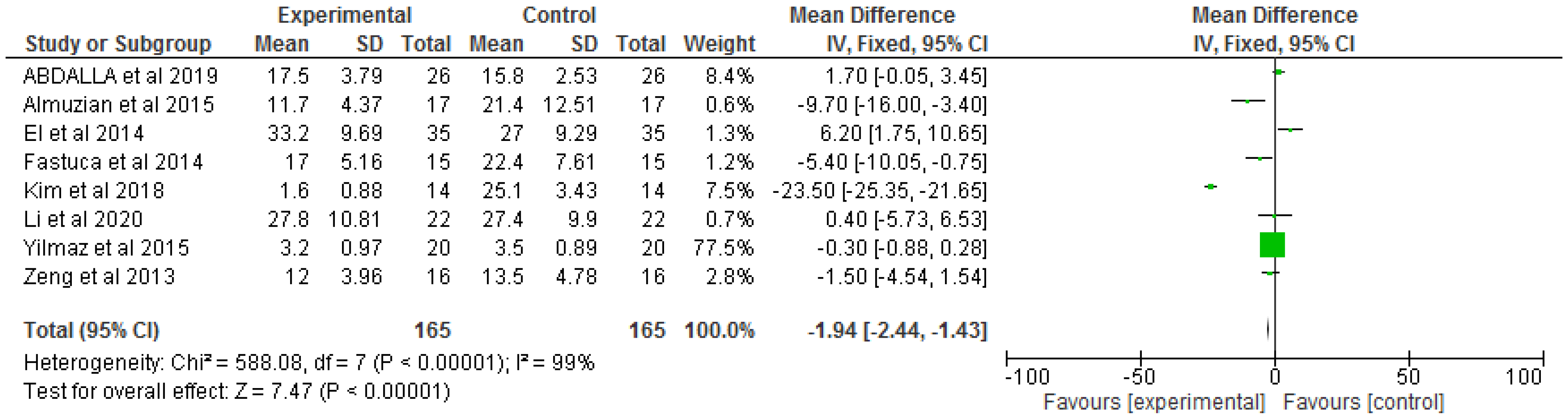
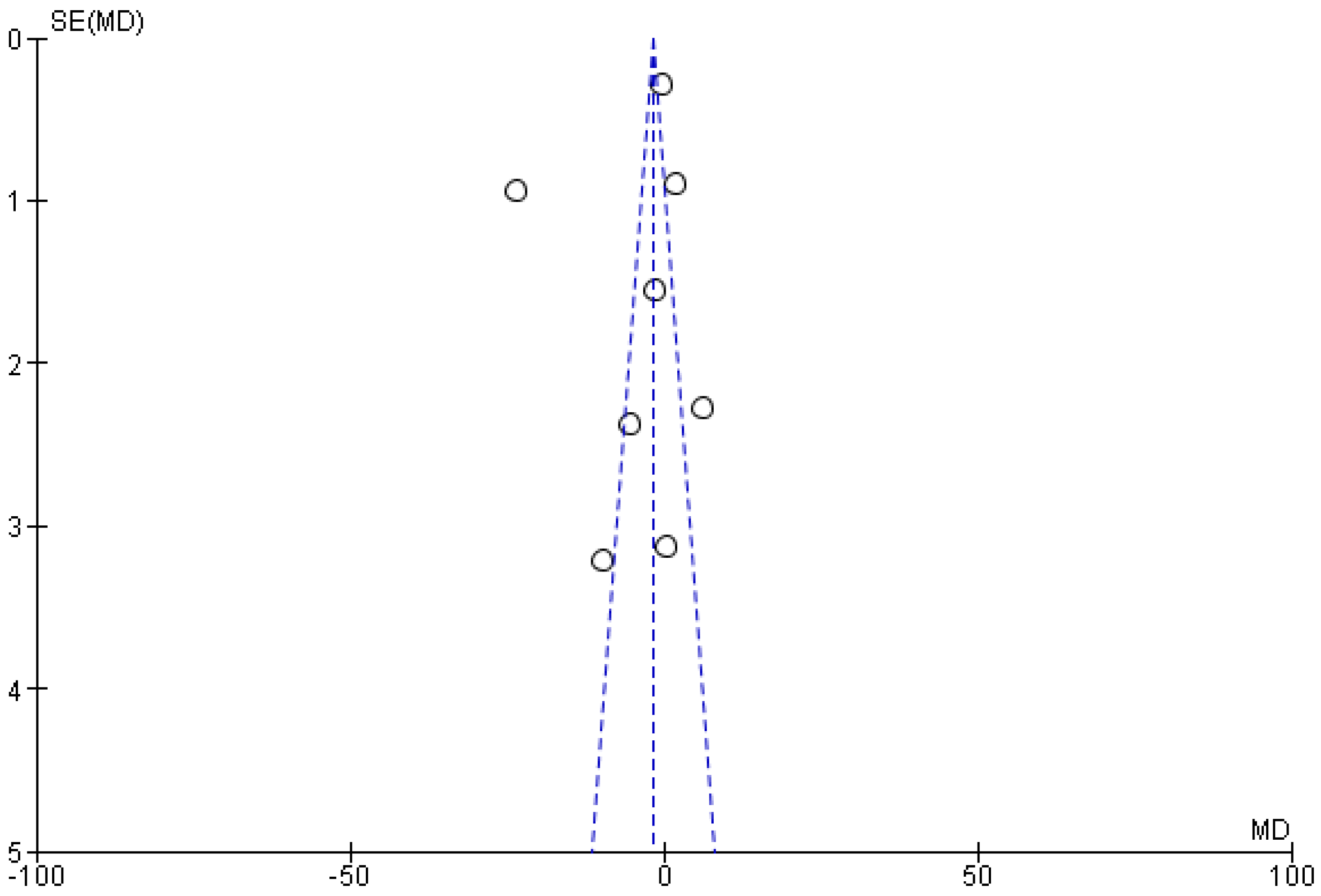
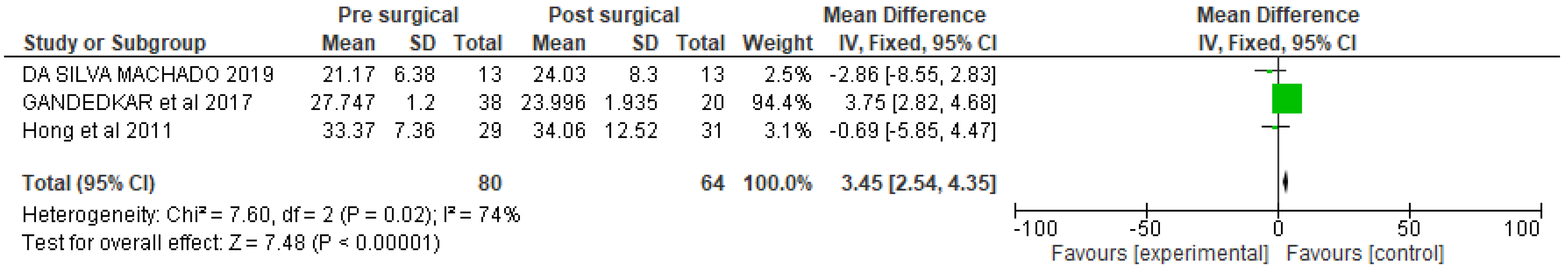
3.4.6. Surgery Class III
3.5. Sensitivity Analysis
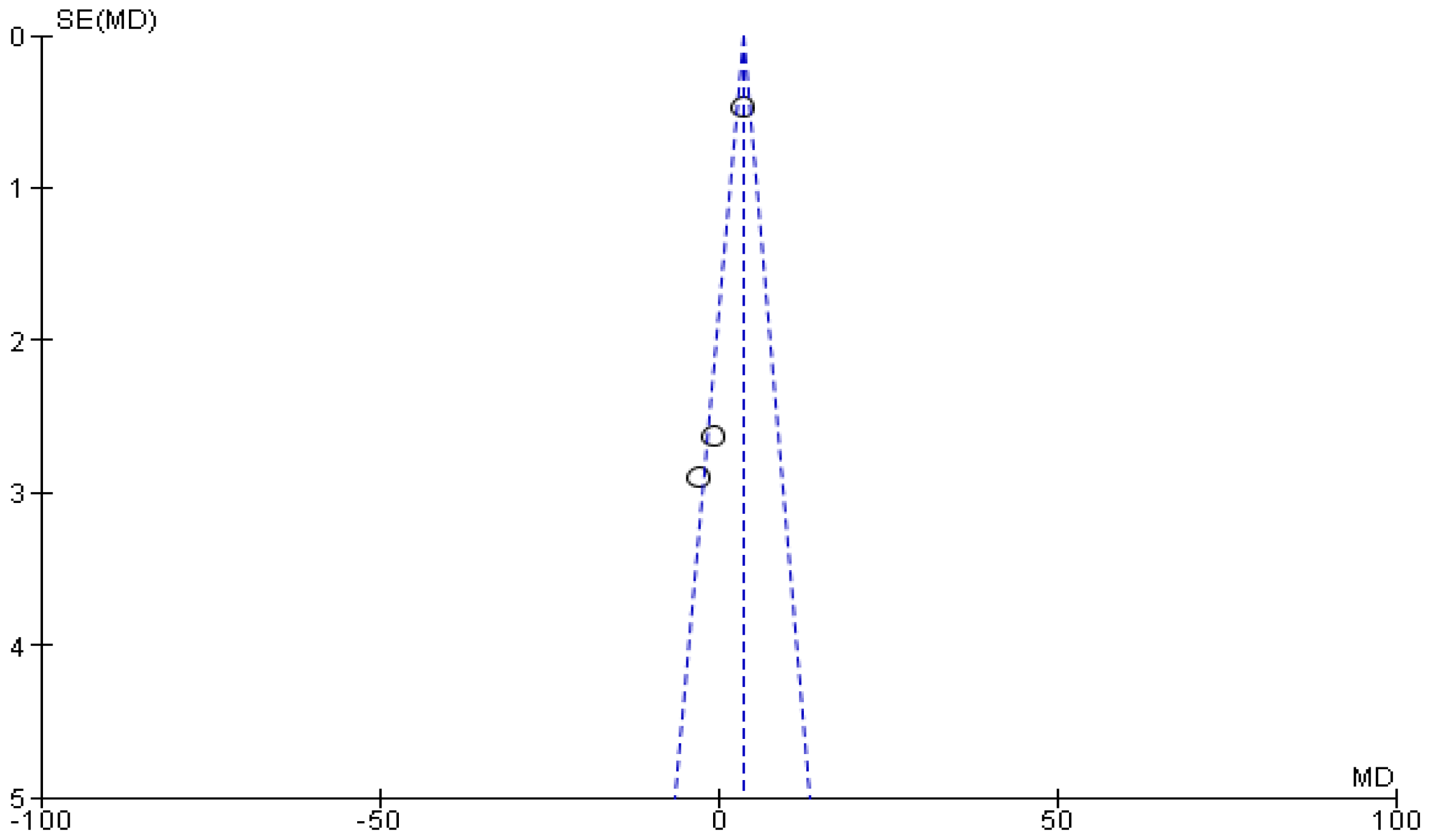
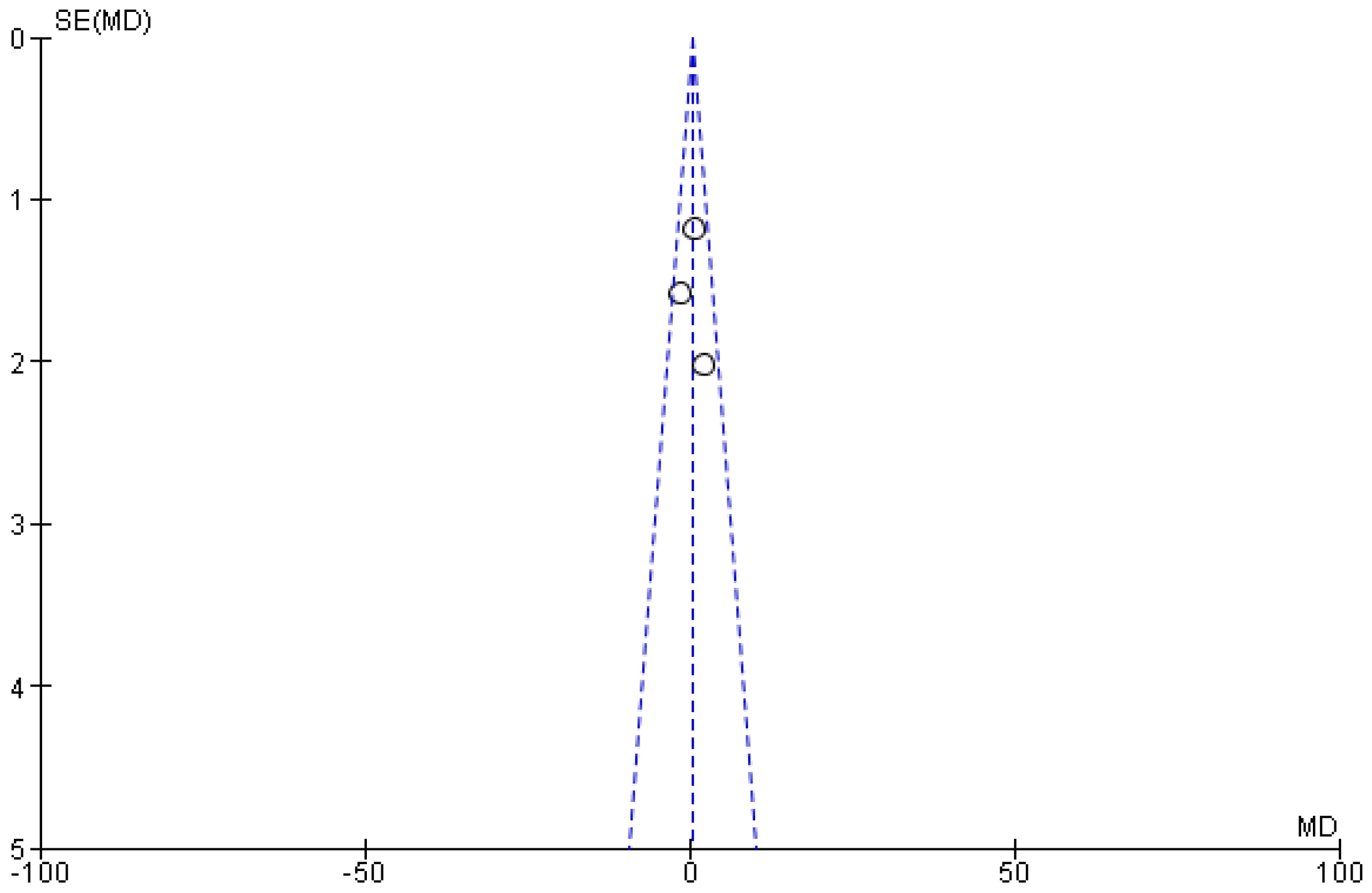
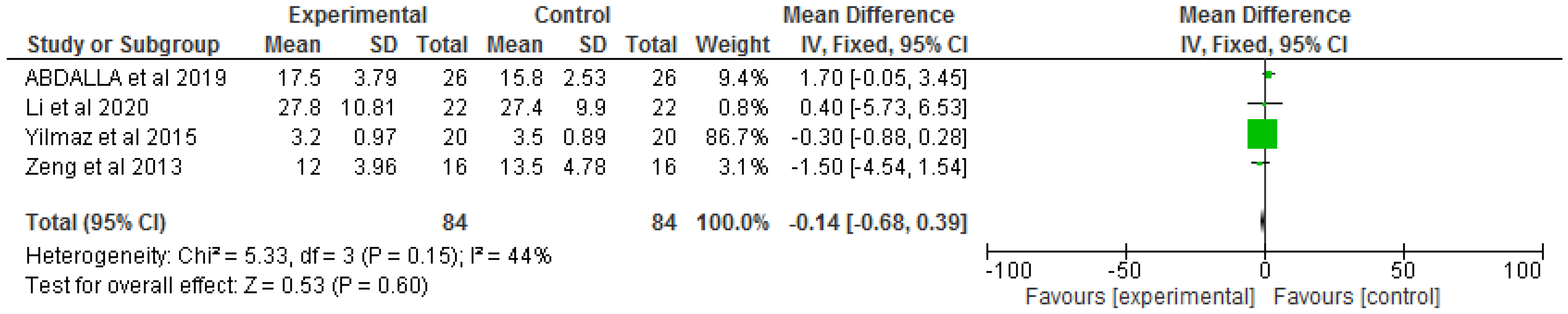
3.5.1. Extraction and Non-Extraction
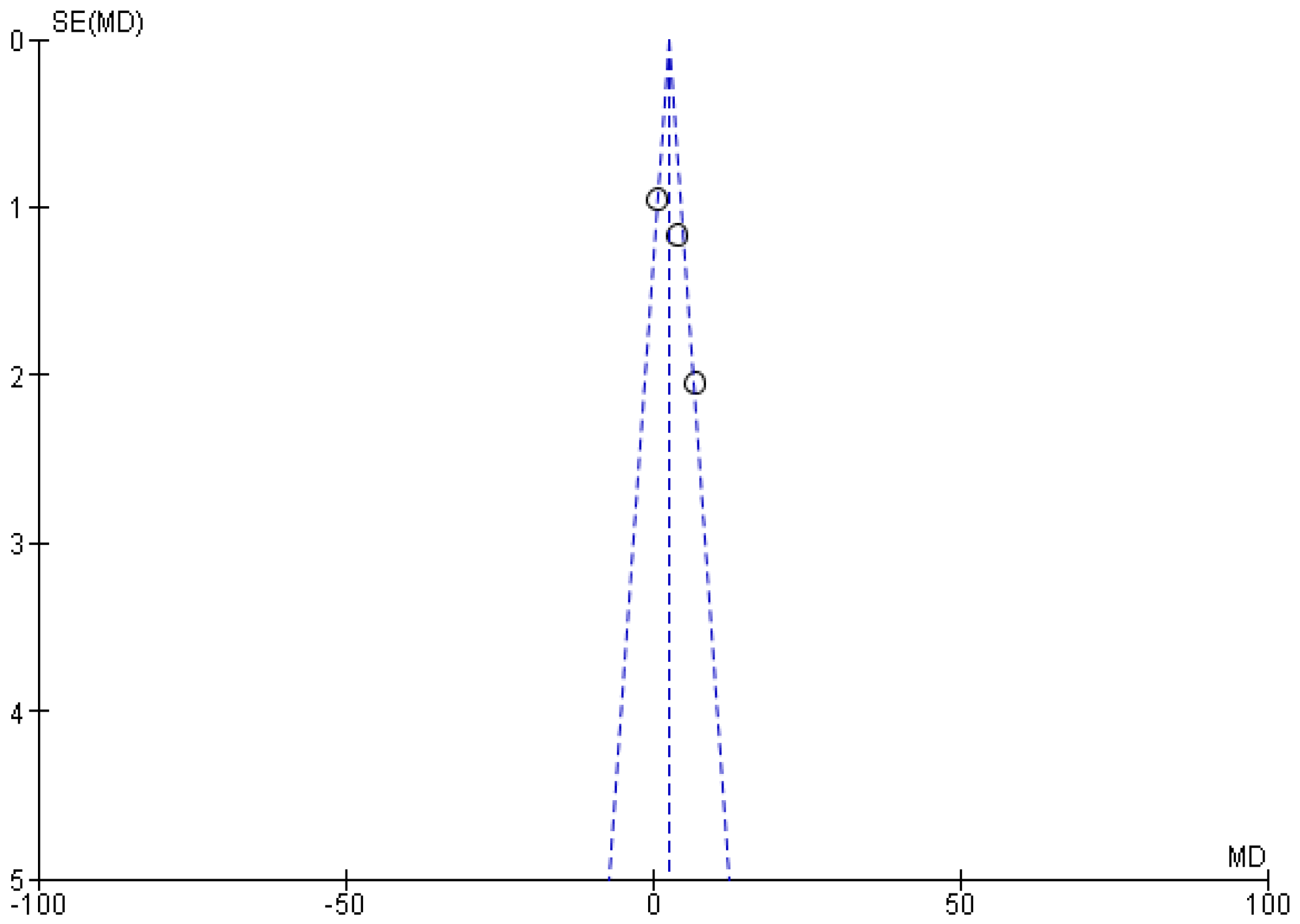
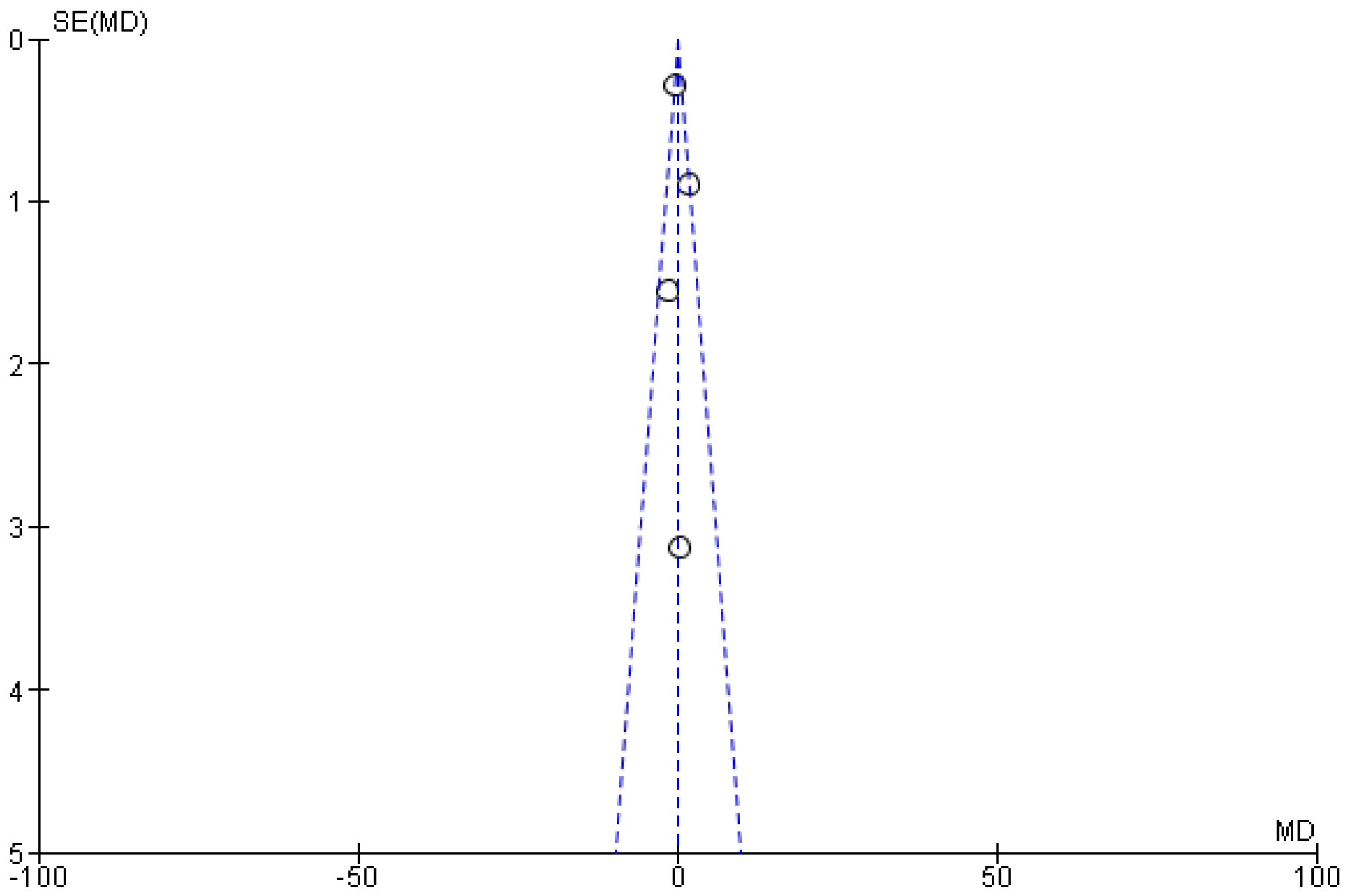
3.5.2. Maxillary Expansion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
List of Tables
| Participants (p) | Studies on Human Participants of Any Gender or Malocclusion Undergo Orthodontic Treatment |
|---|---|
| Intervention (I) | Orthodontic treatment |
| Control (C) | The baseline-airway dimensions prior to orthodontic intervention |
| Outcome (O) | Effect on airway spaces volume assessed with CBCT |
| S.NO | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Risk of Bias | Oliveira et al. | Alhammadi et al., 2019 | Adrienne Joy et al., 2019 | Alrejaye et al., 2019 | Da Silva Machado et al. 2019 | Abdalla et al., 2019 | Kim et al., 2018 | Yuen et al., 2018 | Pliska et al., 2016 | Fu et al., 2016 | Temani et al., 2020 | Almuzian et al., 2015 | Zhang et al. 2015 | Chen et al., 2015 | Nguyen et al., 2015 | Yilmaz et al., 2015 | Pamporakis et al., 2013 | Zeng et al., 2013 | El et al., 2014 | Stefanovic et al., 2013 | Hong et al., 2011 | Valiathan et al., 2010 | Li et al., 2020 | De Sousa Miranda et al. 2015 | Raffaini et al., 2013 | Gandedkar et al., 2017 | Fastuca et al., 2015 | Al-Jewair et al., 2019 | Horani et al., 2021 |
| Was random sequence generation used (i.e., no potential for selection bias)? | L | M | L | H | H | L | M | L | M | M | M | L | L | L | M | M | M | L | H | H | H | H | L | L | H | L | H | L | L |
| Was allocation concealment used (i.e., no potential for selection bias)? | L | L | M | L | M | L | M | L | M | M | H | H | M | M | H | H | H | M | M | H | L | L | L | M | M | M | M | L | M |
| Was there blinding of participants and personnel (i.e., no potential for performance bias)? | M | H | H | M | M | H | L | L | M | H | M | H | H | L | H | L | H | L | M | H | M | H | M | H | M | M | L | H | H |
| Was there blinding of outcome assessment (i.e., no potential for detection bias)? | M | M | H | M | M | H | L | M | L | L | M | L | L | M | L | M | M | M | L | M | L | M | L | L | M | L | H | H | H |
| Was an objective outcome used? | M | L | M | M | M | M | L | M | M | M | M | M | L | L | L | M | M | L | L | M | L | L | M | L | L | M | L | L | L |
| Were more than (80%) a of participants enrolled in trials included in the analysis? (i.e., no potential attrition bias) | M | L | M | M | M | H | M | M | M | M | L | H | H | H | L | M | L | M | L | M | L | M | L | L | H | L | H | M | M |
| Were data reported consistently for the outcome of interest (i.e., no potential selective reporting)? (no potential reporting bias) | H | L | H | H | H | H | L | M | M | L | M | L | H | H | M | H | M | H | M | L | M | L | L | M | H | M | M | L | L |
| No other biases reported? (no potential of other bias) | L | H | M | H | H | M | M | M | M | M | M | L | M | L | M | L | H | M | H | M | H | M | M | H | M | H | H | H | H |
| Did the trials end as scheduled (i.e., not stopped early)? | M | H | H | L | L | M | M | M | L | M | L | L | L | L | M | H | M | H | H | L | L | L | M | H | L | H | L | M | M |
| Inconsistency | |||||||||||||||||||||||||||||
| Point estimates did not vary widely? (i.e., no clinical meaningful inconsistency) | M | L | L | M | M | M | M | M | M | M | M | M | L | M | H | H | M | H | H | M | L | M | L | H | M | H | L | L | L |
| To what extent do confidence intervals overlap? | M | M | L | M | M | L | L | M | H | H | L | L | H | H | H | M | L | M | H | H | L | L | M | L | L | M | M | L | L |
| Was the direction of effect consistent? | H | H | L | L | H | L | L | M | M | M | H | H | L | H | L | M | M | M | L | H | L | H | H | L | H | H | H | L | M |
| What was the magnitude of statistical heterogeneity (as measured by I2)? | H | M | L | M | H | L | L | L | L | M | M | L | M | L | M | L | M | L | L | M | L | M | L | H | L | H | L | H | L |
| Was the test for heterogeneity statistically significant (p < 0.1)? | L | M | M | M | L | M | M | L | L | M | L | M | L | M | L | M | L | M | L | M | L | M | L | H | L | H | L | H | L |
| Indirectness | |||||||||||||||||||||||||||||
| Were the populations in included studies applicable to the target population? | L | M | M | M | M | L | M | L | L | H | H | H | H | M | L | L | M | M | L | M | M | L | M | L | H | L | H | L | H |
| Were the interventions in included studies applicable to target intervention? | L | L | H | H | H | H | M | L | L | M | L | L | M | L | M | L | L | M | L | M | M | M | L | H | L | H | L | H | L |
| Was the included outcome not a surrogate outcome? | H | L | M | H | H | M | L | L | H | M | H | H | M | H | H | L | H | L | H | H | L | H | L | H | L | H | L | L | H |
| Was the outcome timeframe sufficient? | M | M | M | H | L | L | L | H | L | M | L | L | M | L | L | M | M | L | L | M | L | M | L | L | L | M | L | M | L |
| Were the conclusions based on direct comparisons? | H | H | M | M | L | H | H | H | H | M | H | M | H | H | M | H | M | H | L | M | L | H | H | H | M | M | L | H | L |
| Imprecision | |||||||||||||||||||||||||||||
| Was the confidence interval for the pooled estimate not consistent with benefit and harm? | L | L | L | L | L | H | H | H | M | M | L | M | H | L | H | L | H | L | H | L | H | L | H | L | H | L | L | H | L |
| What was the magnitude of the median sample size? | L | L | L | L | L | H | M | H | M | L | M | M | L | M | L | M | L | M | L | H | L | H | L | H | L | H | H | L | L |
| What was the magnitude of the number of included studies? | L | M | M | M | M | M | L | L | L | M | L | M | L | M | L | M | L | M | L | M | L | M | L | H | L | H | H | L | H |
| Was the outcome a common event? (e.g., occurs more than 1/100) a | M | L | M | H | M | L | M | L | H | H | H | H | L | H | L | L | L | M | L | M | L | M | L | M | L | L | M | M | M |
| Was there no evidence of serious harm associated with treatment? | M | L | M | H | L | L | L | L | L | M | L | M | L | M | M | M | M | L | M | H | H | L | H | L | H | H | H | L | H |
| Publication bias | |||||||||||||||||||||||||||||
| Did the authors conduct a comprehensive search? | L | M | H | M | M | L | M | L | M | L | M | L | M | L | M | L | M | L | L | M | L | M | L | M | L | M | L | M | M |
| Did the authors search for grey literature? | M | M | H | L | L | M | H | L | M | L | M | L | L | M | L | M | L | L | H | L | H | L | L | L | H | L | H | L | H |
| Authors did not apply restrictions to study selection on the basis of language? | L | H | L | L | L | M | H | M | L | M | L | M | M | L | M | L | M | L | L | M | L | L | H | H | H | L | H | L | H |
| There was no industry influence on studies included in the review? | L | H | L | L | L | H | M | M | M | L | M | L | L | L | L | M | L | M | H | M | H | M | H | M | M | L | M | L | M |
| There was no evidence of funnel plot asymmetry? | L | L | M | M | M | H | M | M | M | L | M | M | L | M | M | L | M | M | L | M | L | M | L | M | L | M | L | M | M |
| There was no discrepancy in findings between published and upublished trials? | M | M | M | L | M | H | M | L | M | L | M | L | M | L | M | M | L | H | L | H | H | L | H | M | M | H | L | L | M |
| Overall score | M | M | H | M | M | H | M | L | M | M | M | M | L | M | L | L | M | M | L | M | L | M | L | M | M | L | M | L | M |
| S.No | Author & Year | Country | Study Design | Sample Size | Gender | Age (Years) Range/Mean/Median | Orthodontic | Type of Malocclusion | Method Used to Assess the Airway | Specific Airway Space That Was Assessed | Variables | Actual Baseline | Follow up Duration | p-Values | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Oliveira et al. [39] | USA | Retrospective | 42 | 25/M & 17/F | Mean-13.8 ± 1.2 | Functional appliance (HERBST) | Class II malocclusion | CBCT | The upper airway was divided into 3 regions: nasal cavity, nasopharynx, and oropharynx | Functional appliance: Experiment: Mean:28.5, SD: 10.8, Control: Mean: 20.6, SD: 9.4 | Class II malocclusion with an ANB angle >4° | NR | Nasal cavity- HAG-0.144 and CG-0.046; Nasopharynx- HAG-0.071 and CG-0.211; Oropharynx- HAG-0.003 and CG-0.666 | Increased the volume of the oropharynx, but no volumetric modifications in the nasal cavity and nasopharynx. |
| 2 | Alhammadi et al. [41] | Egypt | Controlled clinical study | 62 | 62/F | Mean-11.27 ± 1.19 | Functional appliance (Twinblock & Forsus Fatigue Resistance Device) | Class II malocclusion | Pre- and posttreatment/observational cone beam computed tomography | Pharyngeal airway | Functional appliance: Experiment: Mean:16.8, SD: 3.26, Control: Mean: 20.1, SD: 2.7 | NR | Every 4 weeks | TWB (p < 0.001) | Twin block functional appliance induced significant pharyngeal airway changes than Forsus |
| 3 | Adrienne Joy et al. [53] | USA | Retrospective study | 83 | 42/M & 41/F | Mean-26.1 ± 7.1 | Extraction | NR | CBCT | Various airway measures in the nasopharynx, retropalatal, or retroglossal regions. | Extraction: Mean-20.8, SD-10.3, Non-extraction: Mean-18.5, SD-8.0 | baseline MCA was less than 100 mm2 or greater than 200 mm2. | NR | p < 0.001. | No effect |
| 4 | Alrejaye et al. [3] | USA | Retrospective study | 26 | 14/M & 12/F | Mean-8.4 ± 1.7 | Maxillary expansion with protraction | NR | CBCT | Oropharyngeal airway | Experimental: Mean-10.3, SD-, Control: Mean-8.7, SD- | NR | NR | p-value: < 0.0001 | No effect |
| 5 | Da Silva Machado et al. [48] | Brazil | Quasi-experimental study | 13 | NR | NR | Class III surgery | Class III malocclusion | multislice computed tomography | Pharyngeal airway | Surgery Class III Experimental: Mean- 21.2, SD-6.4 Control: Mean- 24.0, SD- 8.3 | NR | NR | p < 0.05 | Increase airway space |
| 6 | Abdalla et al. [21] | Australia | Retrospective study | 26 | 14/F & 12/M | Mean-12 years, 4 months ± 2 years, 4 months | Rapid maxillary expansion | Minor malocclusions | CBCT | Pharyngeal airway | Experimental: Mean-17.5 SD-, Control: Mean-15.8, SD- | NR | NR | p < 0.001 | No effect |
| 7 | Kim et al. [15] | South Korea | Retrospective study | 14 | 10/F & 4/M | Mean-22.7 ± 3.3 | Rapid maxillary expansion | NR | CBCT | Nasal airway | Maxillary Expansion Experimental: Mean-1.6, SD-0.9 Control: Mean- 25.1, SD-3.4 | NR | 12-year | p < 0.05 | Increase |
| 8 | Yuen et al. [54] | USA | Retrospective study | 137 | 126/F & 11/M | NR | Class II surgery | NR | CBCT | Pharyngeal airway | Pre-surgical: Mean-9.0, SD-4.1, Post-surgical: Mean-12.0, SD-5.3 | NR | 1-year after surgery | p-value: < 0.0001 | Increase |
| 9 | Pliska et al. [11] | Minneapolis | Retrospective study | 74 | 25/M & 49/F | Mean-31.9 ± 12.0 | Extraction | NR | CBCT | Orthodontic upper airway | Extraction non extractionExperimental: Mean-20.0564, SD-6.8488 Control: Mean-25.9513, SD-8.1603 | Class II (ANB angle >4° | NR | NR | No change |
| 10 | Fu et al. [26] | China | Longitudinal study | 18 | 13/M & 5/F | Mean-9.6 ± 1.7 | Rapid maxillary expansion with protraction | Class III malocclusion | CBCT | Pharyngeal airway | Expansion with Protraction Experimental: Mean-9.2481, SD-3.237 Control: Mean-12.9176, SD-5.193 | NR | NR | p < 0.001 | Increase |
| 11 | Temani et al. [40] | India | Prospective study | 30 | NR | NR | Functional appliance | Class II malocclusion | CBCT | Pharyngeal airway | Functional appliance: Experiment: Mean:20.0, SD: 4.4, Control: Mean: 15.9, SD: 4.6 | NR | Longer period of follow-up | p < 0.001 | Increase |
| 12 | Almuzian et al. [13] | Australia | Prospective study | 17 | 8/M & 9/F | Mean-12.6 ± 1.8 | Rapid maxillary expansion | NR | CBCT | Nasopharyngeal airway | Experimental: Mean-17.45, SD-1.47, Control: Mean-16.4, SD-0.8 | NR | Longer term follow-up | p < 0.05 | Increase |
| 13 | Zhang et al. [12] | China | Retrospective study | 18 | 5/M & 13/F | Mean-24.1 ± 3.8 | Extraction | Class II malocclusion | CBCT | The upper airway was divided into nasopharynx, velopharynx, and hypopharynx | Extraction: Mean-49.8, SD-, Non-extraction: Mean-241, SD- | NR | Greater length of follow-up | p < 0.01 | Decrease |
| 14 | Chen et al. [55] | China | Retrospective study | 60 | 28/F & 32/M | Mean- 7 ± 1.21 | Rapid maxillary expansion with protraction | Class III malocclusion | CBCT | Upper airway of nasopharynx, velopharynx | Experimental: Mean-11.7 SD-4.4, Control: Mean-21.3, SD-12.5 | NR | NR | p < 0.05 | Increase |
| 15 | Nguyen et al. [56] | North Carolina | Prospective study | 28 | 14/F & 14/M | NR | Rapid maxillary expansion with protraction | Class III malocclusion | CBCT | Nasopharyngeal, oropharynx airway | Expansion with Protraction Experimental: Mean-14.14, SD-3.76173 Control: Mean-14.56, SD-5.74 | NR | NR | p < 0.05 | No effect |
| 16 | Yilmaz et al. [57] | Turkey | Prospective study | 20 | 10/F & 10/M | Mean-9 | Rapid maxillary expansion | Class III malocclusion | CBCT | The airway was divided into three parts; pharyngeal, nasal, and anterior nasal compartments | Maxillary Expansion Experimental: Mean-3.1967, SD-0.967 Control: Mean-3.51, SD-0.9 | NR | 9 weeks | p < 0.05 | Increase |
| 17 | Pamporakis et al. [58] | Turkey | Retrospective study | 22 | 14/F & 8/M | Mean-10 | Protraction | Class III malocclusion | CBCT | Pharyngeal airway | Expansion with Protraction Experimental: Mean-9.1, SD-2.0 Control: Mean-9.5, SD-2.4 | NR | NR | p < 0.05 | Increase |
| 18 | Zeng et al. [22] | China | Prospective study | 16 | 6/F & 10/M | Mean-12.73 ± 1.73 | Rapid maxillary expansion | NR | CBCT | Nasopharyngeal airway | Experimental: Mean-12, SD-4 Control: Mean-13.5, SD-4.8 | NR | 5 years | p < 0.0033 | Limited effect |
| 19 | El et al. [4] | USA | Retrospective study | 35 | 15/M & 20/F | Mean-14.02 ± 1.46 | Rapid maxillary expansion | Class I malocclusion | CBCT | Oropharyngeal airway | Experimental: Mean-33.2, SD-9.7 Control: Mean-27.0, SD-9.3 | NR | NR | p < 0.001 | No change |
| 20 | Stefanovic et al. [29] | USA | Retrospective study | 31 | 15/M & 16/F | Mean-12.97 ± 1.15 | Extraction | NR | CBCT | Pharyngeal airway | Extraction: Mean-11.2, SD-5.7, Non-extraction: Mean-12.6, SD-6.7 | NR | NR | p ≤ 0.05 | No change |
| 21 | Hong et al. [59] | Korea | Retrospective study | 60 | 30/M & 30/F | Mean- 26.0 ± 4.5 | Class III surgery | Class III malocclusion | CBCT | Pharyngeal airway | Surgery Class III Experimental: Mean-33.36815, SD-7.3556 Control: Mean-34.0623, SD-12.51731 | NR | NR | p ≤ 0.05 | Increase |
| 22 | Valiathan et al. [30] | USA | Retrospective study | 20 | 10/M & 10/F | Mean-13.8 ± 1.3 | Extraction | Class I malocclusion | CBCT | Oropharyngeal airway | Extraction non extraction Experimental: Mean-12.7, SD-4.5 Control: Mean-12.0, SD- 2.9 | NR | NR | p ≤ 0.05 | No change |
| 23 | Li et al. [23] | China | Retrospective study | 22 | 4/M & 18/F | Mean-22.6 ± 4.5 | Rapid maxillary expansion | NR | CBCT | Upper airway of nasal cavity, nasopharyngeal, retropalatal, retroglossal and hypopharyngeal airway | Experimental: Mean-27.8, SD-10.8, Control: Mean-27.4, SD-10 | NR | NR | p ≤ 0.05 | Increase |
| 24 | De Sousa Miranda et al. [60] | Brazil | Retrospective study | 23 | 8/M & 15/F | Mean-33 | Class II surgery | Class II malocclusion | CBCT | Oropharyngeal airway | Surgery Class II Experimental: Mean-20.4767 Control: Mean-30.5952 | NR | 23 patients be followed-up at a later date | p ≤ 0.05 | Increase |
| 25 | Raffaini et al. [61] | Italy | Retrospective study | 10 | 10/F | NR | Class II surgery | Class II malocclusion | CBCT | Pharyngeal airway | Pre-surgical: Mean-15.3, SD-, Post-surgical: Mean-22.6, SD- | NR | 6 to 12 months after surgery | p ≤ 0.05 | Increase |
| 26 | Gandedkar et al. [49] | Singapore | Retrospective study | 58 | 32/F & 26/M | Mean-13.4 ± 0.5 | Class III surgery | Class III malocclusion | CBCT | Pharyngeal airway | Pre-surgical: Mean-27.7, SD-1.2, Post-surgical: Mean-23.9, SD-1.4 | NR | NR | p ≤ 0.05 | Decrease |
| 27 | Fastuca et al. [14] | Italy | Retrospective study | 15 | 11/F & 4/M | Mean-7.5 ± 0.3 | Rapid maxillary expansion | NR | CBCT | Nasal airway | Maxillary Expansion Experimental: Mean-17.0 Control: Mean- 2.4 | NR | Long term follow-up | p < 0.001 | No change |
| 28 | Al-Jewair et al. [62] | USA | Prospective study | 8 | 5/F & 3/M | Mean-44.6 | Clear aligner | Class II malocclusion | CBCT | The upper airway was divided into three regions: the nasopharynx (NP), oropharynx (OP), and hypopharynx (HP). | Clear aligner Before Treatment: Mean-35.05, SD-14.02 After Treatment: Mean-32.24, SD-9.16 | NR | NR | p = 0.250 | Increase |
| 29 | Al-Jewair et al. [62] | USA | Retrospective study | 24 | 16/F & 8/M | Mean- 35.33 ± 11.14 | Clear aligner | Class III malocclusion | CBCT | Pharyngeal airway | Before: Mean-13.6, SD-4.02, After: Mean-12.07, SD-3.65 | NR | NR | p ≤ 0.05 | Decrease |
References
- Rasmus, R.L.; Jacobs, R.M. Mouth breathing and malocclusion: Quantitative technique for measurement of oral and nasal air-flow velocities. Angle Orthod. 1969, 39, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Mcnamara, J.R. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981, 51, 269–300. [Google Scholar] [CrossRef]
- Alrejaye, N.; Gao, J.; Hatcher, D.; Oberoi, S. Effect of maxillary expansion and protraction on the oropharyngeal airway in individuals with non-syndromic cleft palate with or without cleft lip. PLoS ONE 2019, 14, e90972. [Google Scholar] [CrossRef] [Green Version]
- El, H.; Palomo, J.M. Three-dimensional evaluation of upper airway following rapid maxillary expansion A CBCT study. Angle Orthod. 2014, 84, 265–273. [Google Scholar] [CrossRef]
- Ming, Y.; Hu, Y.; Li, Y.; Yu, J.; He, H.; Zheng, L. Effects of maxillary protraction appliances on airway dimensions in growing class III maxillary retrognathic patients: A systematic review and meta-analysis. Int. J. Pediatr. Otorhinolaryngol. 2018, 105, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.H.; Song, Y.L.; Yap, A.U.J. Effects of bicuspid extractions and incisor retraction on upper airway of Asian adults and late adolescents: A systematic review. J. Oral Rehabil. 2019, 46, 1071–1087. [Google Scholar] [CrossRef] [PubMed]
- Di Carlo, G.; Saccucci, M.; Ierardo, G.; Luzzi, V.; Occasi, F.; Zicari, A.M.; Duse, M.; Polimeni, A. Rapid Maxillary Expansion and Upper Airway Morphology: A Systematic Review on the Role of Cone Beam Computed Tomography. Biom Res. Int. 2017, 2017, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Niu, X.; Di Carlo, G.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional analyses of short- and long-term effects of rapid maxillary expansion on nasal cavity and upper airway: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2020, 23, 250–276. [Google Scholar] [CrossRef] [PubMed]
- Moher, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Pliska, B.T.; Tam, I.T.; Lowe, A.A.; Madson, A.M.; Almeida, F.R. Effect of orthodontic treatment on the upper airway volume in adults. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 937–944. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, G.; Li, W.; Xu, T.; Gao, X. Upper airway changes after orthodontic extraction treatment in adults: A preliminary study using cone beam computed tomography. PLoS ONE 2015, 10, e0143233. [Google Scholar] [CrossRef]
- Almuzian, M.; Ju, X.; Almukhtar, A.; Ayoub, A.; Al-Muzian, L.; McDonald, J.P. Does rapid maxillary expansion affect nasopharyngeal airway? A prospective Cone Beam Computerised Tomography (CBCT) based study. Surgeon 2018, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fastuca, R.; Perinetti, G.; Zecca, P.A.; Nucera, R.; Caprioglio, A. Airway compartments volume and oxygen saturation changes after rapid maxillary expansion: A longitudinal correlation study. Angle Orthod. 2015, 85, 955–961. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Park, Y.C.; Lee, K.J.; Lintermann, A.; Han, S.S.; Yu, H.S.; Choi, Y.J. Assessment of changes in the nasal airway after nonsurgical miniscrew-assisted rapid maxillary expansion in young adults. Angle Orthod. 2018, 88, 435–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Concato, J.; Shah, N.; Horwitz, R.I. Randomized, Controlled Trials, Observational Studies, and the Hierarchy of Research Designs. N. Engl. J. Med. 2000, 342, 1887–1892. [Google Scholar] [CrossRef] [Green Version]
- Aboudara, C.; Nielsen, I.; Huang, J.C.; Maki, K.; Miller, A.J.; Hatcher, D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 468–479. [Google Scholar] [CrossRef] [PubMed]
- Schütz-Fransson, U.; Kurol, J. Rapid Maxillary Expansion Effects on Nocturnal Enuresis in Children. Angle Orthod. 2008, 78, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Gray, L.P. Rapid maxillary expansion and impaired nasal respiration. Ear Nose Throat J. 1987, 66, 248–251. [Google Scholar]
- Camacho, M.; Chang, E.T.; Song, S.A.; Abdullatif, J.; Zaghi, S.; Pirelli, P.; Certal, V.; Guilleminault, C. Rapid maxillary expansion for pediatric obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope 2017, 127, 1712–1719. [Google Scholar] [CrossRef]
- Abdalla, Y.; Brown, L.; Sonnesen, L. Effects of rapid maxillary expansion on upper airway volume: A three-dimensional cone-beam computed tomography study. Angle Orthod. 2019, 89, 917–923. [Google Scholar] [CrossRef] [Green Version]
- Zeng, J.; Gao, X. A prospective CBCT study of upper airway changes after rapid maxillary expansion. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 1805–1810. [Google Scholar] [CrossRef]
- Li, Q.; Tang, H.; Liu, X.; Luo, Q.; Jiang, Z.; Martin, D.; Guo, J. Comparison of dimensions and volume of upper airway before and after mini-implant assisted rapid maxillary expansion. Angle Orthod. 2020, 90, 432–441. [Google Scholar] [CrossRef] [Green Version]
- Pirelli, P.; Saponara, M.; Guilleminault, C. Rapid maxillary expansion (RME) for pediatric obstructive sleep apnea: A 12-year follow-up. Sleep Med. 2015, 16, 933–935. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.W.; Hagg, U.; Yiu, C.; Wei, S.H.Y. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin. Orthod. 1997, 3, 255–264. [Google Scholar] [CrossRef]
- Fu, Z.; Lin, Y.; Ma, L.; Li, W. Effects of maxillary protraction therapy on the pharyngeal airway in patients with repaired unilateral cleft lip and palate: A 3-dimensional computed tomographic study. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Jia, H.; Li, W.; Lin, J. Maxillary protraction effects on anterior crossbites: Repaired unilateral cleft versus noncleft prepubertal boys. Angle Orthod. 2008, 78, 617–624. [Google Scholar] [CrossRef]
- Sharma, J.N. Skeletal and Soft Tissue Point A and B Changes Following Orthodontic Treatment of Nepalese Class I Bimaxillary Protrusive Patients. Angle Orthod. 2010, 80, 91–96. [Google Scholar] [CrossRef]
- Stefanovic, N.; El, H.; Chenin, D.L.; Glisic, B.; Palomo, J.M. Three-dimensional pharyngeal airway changes in orthodontic patients treated with and without extractions. Orthod. Craniofacial Res. 2013, 16, 87–96. [Google Scholar] [CrossRef]
- Valiathan, M.; El, H.; Hans, M.G.; Palomo, M.J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010, 80, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.C.; Jeffres, M.N.; Miller, A.; Hatcher, D.C. Three-dimensional airway evaluation in 387 subjects from one university orthodontic clinic using cone beam computed tomography. Angle Orthod. 2012, 82, 985–992. [Google Scholar] [CrossRef]
- Chen, Y.; Hong, L.; Wang, C.; Zhang, S.; Cao, C.; Wei, F.; Lv, T.; Zhang, F.; Liu, D. Effect of large incisor retraction on upper airway morphology in adult bimaxillary protrusion patients. Angle Orthod. 2012, 82, 964–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Q.; Jia, P.; Anderson, N.K.; Wang, L.; Lin, J. Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary protrusion. Angle Orthod. 2012, 82, 115–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miles, P.G.; Vig, P.S.; Weyant, R.J.; Forrest, T.D.; Rockette, H.E. Craniofacial structure and obstructive sleep apnea syndrome—a qualitative analysis and meta-analysis of the literature. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 163–172. [Google Scholar] [CrossRef]
- Lowe, A.A.; Santamaria, J.D.; Fleetham, J.A.; Price, C. Facial morphology and obstructive sleep apnea. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 484–491. [Google Scholar] [CrossRef]
- Restrepo, C.; Santamaría, A.; Peláez, S.; Tapias, A. Oropharyngeal airway dimensions after treatment with functional appliances in class II retrognathic children. J. Oral Rehabil. 2011, 38, 588–594. [Google Scholar] [CrossRef] [PubMed]
- Koretsi, V.; Zymperdikas, V.F.; Papageorgiou, S.N.; Papadopoulos, M.A. Treatment effects of removable functional appliances in patients with Class II malocclusion: A systematic review and meta-analysis. Eur. J. Orthod. 2015, 37, 418–434. [Google Scholar] [CrossRef] [PubMed]
- Zymperdikas, V.F.; Koretsi, V.; Papageorgiou, S.N.; Papadopoulos, M.A. Treatment effects of fixed functional appliances in patients with Class II malocclusion: A systematic review and meta-analysis. Eur. J. Orthod. 2016, 38, 113–126. [Google Scholar] [CrossRef]
- Oliveira, P.M.; Cheib-Vilefort, P.L.; de Pársia Gontijo, H.; Melgaço, C.A.; Franchi, L.; McNamara, J.A.; Souki, B.Q. Three-dimensional changes of the upper airway in patients with Class II malocclusion treated with the Herbst appliance: A cone-beam computed tomography study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 205–211. [Google Scholar] [CrossRef]
- Temani, P.; Jain, P.; Rathee, P.; Temani, R. Volumetric changes in pharyngeal airway in Class II division 1 patients treated with Forsus-fixed functional appliance: A three-dimensional cone-beam computed tomography study. Contemp. Clin. Dent. 2016, 7, 31–35. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Elfeky, H.Y.; Fayed, M.S.; Ishaq, R.A.R.; Halboub, E.; Al-mashraqi, A.A. Three-dimensional skeletal and pharyngeal airway changes following therapy with functional appliances in growing skeletal Class II malocclusion patients: A controlled clinical trial. J. Orofac. Orthop. 2019, 80, 254–265. [Google Scholar] [CrossRef]
- Xiang, M.; Hu, B.; Liu, Y.; Sun, J.; Song, J. Changes in airway dimensions following functional appliances in growing patients with skeletal class II malocclusion: A systematic review and meta-analysis. Int. J. Pediatr. Otorhinolaryngol. 2017, 97, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhan, S. Effect of functional appliances on the airway in Class II malocclusions. J. World Fed. Orthod. 2020, 9, S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-J.; Hong, J.-S.; Hwang, Y.-I.; Park, Y.-H. Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 306.e1–306.e11. [Google Scholar] [CrossRef] [PubMed]
- El, H.; Palomo, J.M. An airway study of different maxillary and mandibular sagittal positions. Eur. J. Orthod. 2013, 35, 262–270. [Google Scholar] [CrossRef] [Green Version]
- Jakobsone, G.; Neimane, L.; Krumina, G. Two- and three-dimensional evaluation of the upper airway after bimaxillary correction of Class III malocclusion. Oral Surgery Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 110, 234–242. [Google Scholar] [CrossRef]
- Chen, F.; Terada, K.; Hua, Y.; Saito, I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 372–377. [Google Scholar] [CrossRef]
- da Silva Machado, V.; Cantharino de Carvalho, B.A.; Vedovello, S.A.S.; Valdrighi, H.; Santamaria Júnior, M. Pharyngeal Airway Modifications in Skeletal Class III Patients Undergoing Bimaxillary Advancement Surgery. J. Oral Maxillofac. Surg. 2019, 77, 2126.e1–2126.e8. [Google Scholar] [CrossRef] [PubMed]
- Gandedkar, N.H.; Chng, C.K.; Basheer, M.A.; Chen, P.Y.; Yeow, V.K.L. Comparative evaluation of the pharyngeal airway space in unilateral and bilateral cleft lip and palate individuals with noncleft individuals: A cone beam computed tomography study. Cleft Palate-Craniofac. J. 2017, 54, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Christovam, I.O.; Lisboa, C.O.; Ferreira, D.M.T.P.; Cury-Saramago, A.A.; Mattos, C.T. Upper airway dimensions in patients undergoing orthognathic surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 460–471. [Google Scholar] [CrossRef]
- Giralt-Hernando, M.; Valls-Ontañón, A.; Guijarro-Martínez, R.; Masià-Gridilla, J.; Hernández-Alfaro, F. Impact of surgical maxillomandibular advancement upon pharyngeal airway volume and the apnoea–hypopnoea index in the treatment of obstructive sleep apnoea: Systematic review and meta-analysis. BMJ Open Respir. Res. 2019, 6, e000402. [Google Scholar] [CrossRef] [PubMed]
- Ingman, T. Cephalometric comparison of pharyngeal changes in subjects with upper airway resistance syndrome or obstructive sleep apnoea in upright and supine positions. Eur. J. Orthod. 2004, 26, 321–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joy, A.; Park, J.; Chambers, D.W.; Oh, H. Airway and cephalometric changes in adult orthodontic patients after premolar extractions. Angle Orthod. 2020, 90, 39–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yuen, H.; Rossouw, P.E.; Wolford, L.M.; Wang, H. Pharyngeal Airway Space Changes After Condylar Replacement and Mandibular Advancement Surgery. J. Oral Maxillofac. Surg. 2018, 76, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, D.; Liu, J.; Wu, Z.; Xie, Y.; Li, L.; Liu, H.; Guo, T.; Chen, C.; Zhang, S. Three-dimensional evaluation of the upper airway morphological changes in growing patients with skeletal class III malocclusion treated by protraction headgear and rapid palatal expansion: A comparative research. PLoS ONE 2015, 10, e0135273. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; De Clerck, H.; Wilson, M.; Golden, B. Effect of class III bone anchor treatment on airway. Angle Orthod. 2015, 85, 591–596. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, B.S.; Kucukkeles, N. Skeletal, soft tissue, and airway changes following the alternate maxillary expansions and constrictions protocol. Angle Orthod. 2015, 85, 117–126. [Google Scholar] [CrossRef] [Green Version]
- Pamporakis, P.; Nevzatoǧlu, Ş.; Küçükkeleş, N. Three-dimensional alterations in pharyngeal airway and maxillary sinus volumes in Class III maxillary deficiency subjects undergoing orthopedic facemask treatment. Angle Orthod. 2014, 84, 701–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hong, J.S.; Oh, K.M.; Kim, B.R.; Kim, Y.J.; Park, Y.H. Three-dimensional analysis of pharyngeal airway volume in adults with anterior position of the mandible. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e161–e169. [Google Scholar] [CrossRef]
- De Sousa Miranda, W.; Álvares De Castro Rocha, V.; Lara Dos Santos Marques, K.; Trindade Neto, A.I.; Do Prado, C.J.; Zanetta-Barbosa, D. Three-dimensional evaluation of superior airway space after orthognathic surgery with counterclockwise rotation and advancement of the maxillomandibular complex in Class II patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Raffaini, M.; Pisani, C. Clinical and cone-beam computed tomography evaluation of the three-dimensional increase in pharyngeal airway space following maxillo-mandibular rotation-advancement for Class II-correction in patients without sleep apnoea (OSA). J. Cranio-Maxillof. Surg. 2013, 41, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Al-Jewair, T.; Kurtzner, K.; Giangreco, T.; Warunek, S.; Lagravère-Vich, M. Effects of clear aligner therapy for Class II malocclusion on upper airway morphology and daytime sleepiness in adults: A case series. Int. Orthod. 2020, 18, 154–164. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alswairki, H.J.; Alam, M.K.; Rahman, S.A.; Alsuwailem, R.; Alanazi, S.H. Upper Airway Changes in Diverse Orthodontic Looms: A Systematic Review and Meta-Analysis. Appl. Sci. 2022, 12, 916. https://doi.org/10.3390/app12020916
Alswairki HJ, Alam MK, Rahman SA, Alsuwailem R, Alanazi SH. Upper Airway Changes in Diverse Orthodontic Looms: A Systematic Review and Meta-Analysis. Applied Sciences. 2022; 12(2):916. https://doi.org/10.3390/app12020916
Chicago/Turabian StyleAlswairki, Haytham Jamil, Mohammad Khursheed Alam, Shaifulizan Ab Rahman, Rayan Alsuwailem, and Sarah Hatab Alanazi. 2022. "Upper Airway Changes in Diverse Orthodontic Looms: A Systematic Review and Meta-Analysis" Applied Sciences 12, no. 2: 916. https://doi.org/10.3390/app12020916
APA StyleAlswairki, H. J., Alam, M. K., Rahman, S. A., Alsuwailem, R., & Alanazi, S. H. (2022). Upper Airway Changes in Diverse Orthodontic Looms: A Systematic Review and Meta-Analysis. Applied Sciences, 12(2), 916. https://doi.org/10.3390/app12020916







