1. Introduction
Class III malocclusion is caused by either the deficient growth of the maxilla in the downward and forward direction or excessive growth of the mandible and is considered one of the most difficult cases in orthodontics. Nonsurgical treatment of Class III malocclusion remains a challenge. Current literature on the global prevalence varies significantly among different races, ethnic groups, and geographic regions.
In a study conducted by Soh et al. [
1] to evaluate the occlusal status of an Asian population in Malaysia among the sample of male army recruits (N 339, age 17–22 years), they found that the highest prevalence of Class III malocclusion was in Malay 26.67% followed by Chinese 22.87% and the Indian was the least with 4.76%.
Orthopedic advancement of the maxilla was not successful in adolescent patients and should be accomplished as early as possible before the patient become older than 10 years [
2]. Its effect is limited, although there were some case reports that proved that face masks can still have favorable treatment effects when the patient is over 15 years [
3,
4]. Nowadays, there are mainly three treatment approaches that can provide successful treatment for Class III malocclusion patients, which involves the use of skeletal anchorage, sutural distraction, and alternate rapid maxillary expansion and contraction [
5]. The surgical intervention or orthognathic surgery for correction of maxillary hypoplasia by surgical advancement of the maxillary bone with a Le Fort I osteotomy only can be carried out after the growth had completed. This approach provides a rapid solution that requests limited patient cooperation, direct access for bony correction, treatment of the cross-bite, and makes significant facial morphological changes without any unfavorable dental tipping, which is often accompanied with conventional orthopedic treatment [
6]. The surgical approach has some disadvantages, including the need to delay surgery until growth ceased causing patients suffering from the unaesthetic appearance until an older age, expensive and invasive with a time recovery period from 6 to 8 weeks and always be associated with the patients’ discomfort, soft diet, facial swelling, transient paresthesia, and sometimes permanent loss of neuro sensation [
7].
It was reported that orthopedic protraction of the maxilla is limited in adolescent patients, and this treatment should only be accomplished at a younger age [
2]. Thus, active skeletonized sutural distractor (ASSD) appliance was designed to take advantage of these treatment methods and avoid their limitations.
The objective for this study was to determine the post-treatment skeletal, dental and soft tissue changes in the anteroposterior plane applying ASSD in late adolescent Class III malocclusion patients using lateral cephalometric radiograph.
2. Materials and Methods
After screening 13,500 students from 18 secondary schools, a sample of 26 subjects was recruited for this study, with a mean age of 15(±1.4) years. The ethical approval was obtained from the committee (USM/JEPeM/15120548).
The inclusion criteria for this study were patients who are in late adolescence, which corresponds to the age range between 12 years and 6 months to 16 years in girls and 14 years and 6 months to 17 years in boys [
8], angle Class III malocclusion, and skeletal Class III malocclusion with maxillary retrognathism (Wits appraisal is-4 mm or less) and horizontal changes of maxilla at A point: A-N perp is −3.83 mm (+/−2.97) or less [
9] with or without mandibular protrusion.
2.1. Applications of the ASSD Appliance
- –
The bands for upper and lower first permanent molars in both sides were fitted, then an alginate impression was taken and poured into stone plaster for fabrication of the working model.
- –
Fabrication of the upper and lower parts of the ASSD (
Figure 1).
In the upper jaw, two palatal arms made from 2 mm stainless-steel wire were soldered to the expansion mini-screw, as well as two 1.2 mm stainless-steel wire teardrop loops that are used for insertion of two anterior mini implants at the level of the first premolar connecting it to the upper appliance.
In the lower jaw, a buccal arch made of 2 mm stainless-steel wire was soldered to the first molars band on both sides. Two buccal stainless-steel hooks solder to the buccal arch at the level of the lower canines bilaterally for the attachment of the Class III intraoral elastics (
Figure 2).
- –
Insertion of the appliance.
Insertion of the appliance in the patient’s mouth was performed by bonding it to the teeth by glass ionomer cement (RMGI Cements, 3535TK, 3M, Monrovia, CA, USA). After cementation of the appliance, the mini-implant was inserted at the distal end of the two teardrop loops and passively fit over it, and the expansion screw was opened by 1 mm by the operator. The mini-implant was inserted according to the manufacturer’s instructions using the Cope placement protocol. This protocol is considered the least invasive protocol because, in most cases, there is no need for local anesthesia or flap incision or predrilling.
Two mini implants were inserted about 3 mm away from the mid-palatal suture. In the anterior palate bilaterally (1.8 mm width and 10 mm length) at the level of the second premolars and about 8 mm posterior to the incisive foramen, in a position that coincides with the plane of maximum resistance of the maxilla and near to the maxillary center of resistance. The length of the mini-implant was determined according to a previous study [
10,
11]. The mobility of the mini-implant was checked with the application of 500 gm of force determined by force gauge (Correx, Orthocare, U.K.), where intraoral elastics (3M, Bummer (heavy) 6oz, 3M, Monrovia, USA) were attached in a direction nearly perpendicular to the mini-implant. This test was made at the start of treatment and every month until the end of the active treatment period [
12].
After 24 h from the fixation of the ASSD in the patient mouth (
Figure 3), the patient was instructed to perform the alternate rapid maxillary expansion and contraction (Alt.RAMEC) according to the schedule given starting from 4 turns/day of open and close the expansion screw, which corresponds to 1 mm until reaching 28 turn/day, which corresponds to 7 mm until end of the active treatment period [
6].
After two weeks of the start of treatment, the patient was asked to wear intraoral elastics (3M, Bummer (heavy) 6oz, 3M, Monrovia, USA), which exerts protraction forces of about 500 gm in each side that was attached to the upper and lower part of the appliance [
13]. To decrease the counterclockwise rotation of the upper occlusal plane, the elastic oriented with a 15–30 degree angle to the occlusal plane [
9]. The oral hygiene of the patients was monitored throughout the treatment.
2.2. Lateral Cephalometric Analysis
The cephalometric X-ray was taken using lateral cephalometric machine Gendex Orthoralix, Italy, at initial observation (T1) before the start of treatment and (T2) at the end of active treatment. Cephalometric tracing was performed using Planmeca Romexis Software, which is considered a reliable tool for lateral cephalometric measurements [
14] and analyzed by a single operator. Tracing and measurements were performed on pre- and post-treatment cephalograms to measure the efficacy of treatment (skeletal, dental, and soft tissue changes) as shown in
Figure 4 according to variables in
Table 1 [
15].
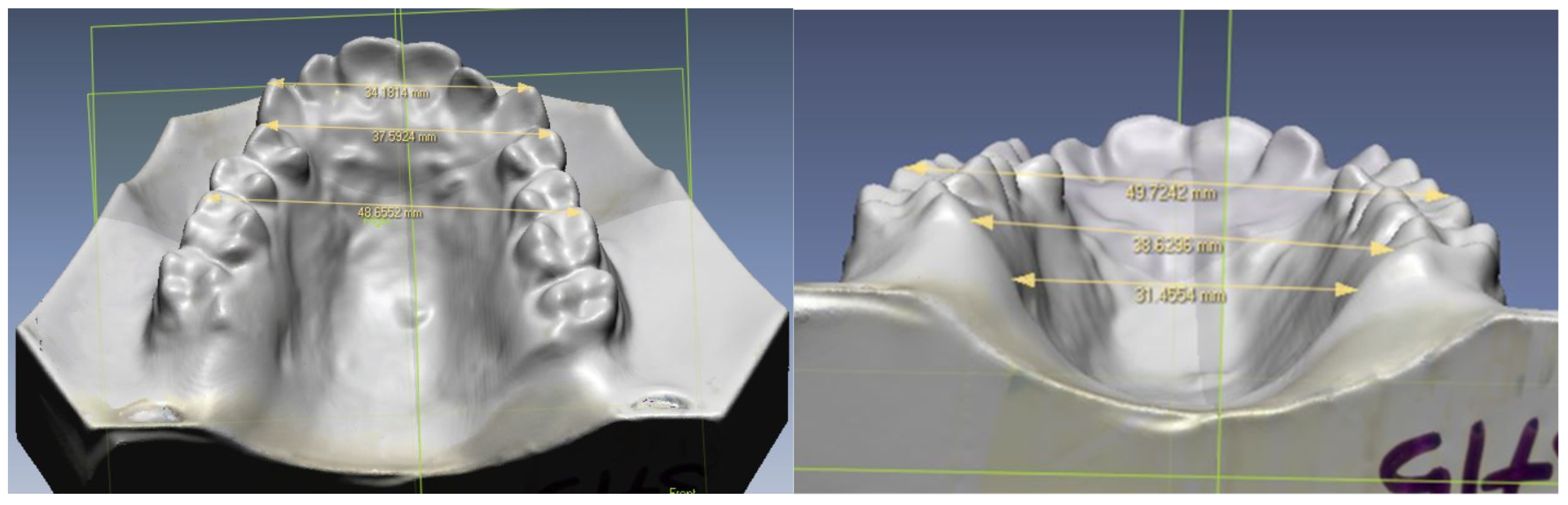
2.3. Upper Study Model Analysis
This step was performed using a 3D laser scanner (Next Engine Inc., Model 2020i, Santa Monica, CA, USA) for pre-and post-dental models. Dental casts of the subjects were obtained from alginate impressions before expansion (D1), before start of treatment and after expansion (D2), at the end of treatment. After image acquisition (
Figure 5), the landmarks (
Table 2) [
16] are digitized, and the transverse measurements were recorded. The variables used per identification and measurements were inter-canine widths (ICW), inter-1st premolar widths (IPW), inter-first molar widths (IMW), and palatal width (PW).
All scanned data coordinates (in x, y, z) are transferred into ScanStudio HD software in DXF format to be measured. Spatial linear measurements are measured with a digital caliper (using computer mouse) accurate to 0.5 mm, and the average value is used. For the equipment calibration, the 3D laser scanner and software were autocalibated from time to time, and manual calibration was repeated by comparing the value with the direct measurement from a few study casts to ensure accuracy and reliability. The accuracy of the measurements from a 3D laser scanner is up to 0.05 [
17].
2.4. Error Measurement
The reliability of the cephalometric and dental cast measurements was tested by repeating the measurements on randomly selected subjects (20% of total sample size) by two examiners. The reliability of the method was analyzed using Dahlberg’s formula [
18].
4. Discussion
The study was conducted to measure the effectiveness of ASSD appliances in treating severe Class III malocclusion cases that were indicated for surgical treatment. There were some unique characteristics to this study. First, the sample of the study was collected from 18 secondary schools by a screening of 13,500 students. It was considered a very big number in comparison to similar studies, which collect smaller sample sizes from the outpatient clinic, not by screening of the target population. In addition, many studies were carried out to investigate the effects of using rigid skeletal anchorage, Alt.RAMEC and sutural distraction method for treatment of Class III malocclusion, but as far as we are aware, no study had been performed to investigate the effect of combining these three approaches.
Furthermore, we innovated a unique design for the ASSD appliance, which involves a small size maxillary expander that is not presented in any other similar studies making the appliance suitable for any patients who have different palatal shape and height. Next, the effects on the craniofacial skeleton induced by facemask therapy have seldom been investigated in adequate samples, especially in late adolescent subjects, as evident in this study [
19].
The result of this study showed that the ASSD was effective in the treatment of Class III malocclusion in late adolescent subjects. Although most of the subjects showed improvement of the Class III malocclusion, the amount of the correction varied greatly among patients, as did their level of cooperation.
Assessment of the results demonstrated significant changes in the maxilla as well as in the mandible that favored correction of Class III malocclusion. The maxilla became more forward due to a significant increase in the maxillary position (SNA), increase in maxillary length (CO-A), and forward movement of A point (A-N perp).
The skeletal point A forward changes by 3.69 mm revealed that maxillary growth was achieved in the ASSD treatment group and that the ASSD effectively facilitated skeletal growth of the maxilla. In spite of differences between ASSD treatment protocols and the other similar studies, a common trend was observed in similar studies for A-point advancement in the horizontal plane as a result of bone-anchored orthopedic treatment.
Morales-Fernandez et al. [
20] compared the results of conventional orthopedic appliances with those obtained from recent bone-anchored orthopedics for Class III malocclusion treatment. In those studies, using skeletal anchorage, there was forward movement in the horizontal plane with a mean A-point advancement of 5.2 mm [
21,
22,
23].
In addition, the maxilla became more forward due to an increase in the maxillary position (SNA) by 2.73°, similar to the finding of Nienkemper et al. [
24] by 2.4° as well as Katyal et al. [
25] by 2° with more increments. These differences may be attributed to the differences in the subject’s characteristics, treatment protocol, and treatment durations (14 months). In addition to that, an increase in maxillary length (Co-A) was significant as well (4.62 mm), and this was in agreement with [
6,
24,
25].
The mandible has a backward rotation manifested by a significant increase in mandibular plane angle (MP/SN) and SNB value. The lower anterior facial height (ANS-Gn) showed a significant increase as a reflection of the backward rotation of the mandible.
The negative change in SNB in the ASSD group shared similar results with previous studies [
3,
4,
21] and was lower than that reported by Nienkemper et al. [
24] by 1.7°. This difference may be attributed to limited downward decedents of the maxilla due to using of the skeletal anchorage and hence lower backward rotation of the mandible and lower changes in the SNB angle. The negative numerical value change in SNB indicated that mandible growth is limited and that the forward change at the B point is controlled.
The smaller increase in mandibular plane angle (MP/SN) by 2.35°, occlusal plane angle (OP/SN) by 1.46°, and the lower anterior facial height (ANS-Gn) by 1.6 mm reflected the limited effects of ASSD on increasing the vertical dimension, which is primarily important in treating patients having Class III malocclusion with increased lower facial height. This finding was similar to the finding reported in other studies [
6,
25].
The inter-arch relationship was also improved as there was an improvement in Wits appraisal value (AO-BO) as well as ANB value. The improvement in Wits appraisal value (AO-BO) was 6.4 mm, and this was much more than the finding of other studies [
24,
25], where the changes were 4.5 and 3.4 mm, respectively. Moreover, the ANB value improved by 3.29°, which was more than the finding of Nienkemper et al. [
24] as well as Katyal et al. [
25] as it was 1.9° and 2.4° respectively.
These differences in the improvement of the Wits appraisal as well as the ANB values may be attributed to the differences in the treatment protocol used in the present study from that used in the other studies. As in both studies performed by Nienkemper et al. [
24] and Katyal et al. [
25], the improvement was lesser than in the present study because they used only skeletal anchorage without performing the repetitive cycles of Alt.RAMEC.
Reports of maxillary orthopedic protraction using skeletal anchorage and intraoral forces are rare in contemporary orthodontic literature. Three-dimensional imaging studies by De Clerck et al. [
21] showed that bone-anchored maxillary protraction stimulated forward displacement and modeling of the maxillary and zygomatic bones as well as affecting mandibular shape.
It was evident that the ASSD group in the present study and those of De Clerck et al. [
23] were similar in relation to the pretreatment Wits value. However, age at commencement was older in the ASSD group than that in the De Clerck et al. [
21] study as the age of the subjects in the present study was in the post-adolescent stage of growth while the subjects were in the pre-pubertal stage.
It was interesting to note that a slightly greater improvement in Wits value of 6.4 mm was found in the present study than that found by De Clerck et al. [
21] 4 mm at the end of treatment. It may be argued that the difference in Wits improvement between the two studies is valuable and could be attributed to the unique protocol used in the present study that combined three different treatment approaches in one appliance.
These differences also could have been due to variations in the sample size, demographics, compliance of the patients, or the measurements obtained on three-dimensional images compared with two-dimensional imaging. An advantage of the ASSD protocol over the protocol used by De Clerck et al. [
21] and Katyal et al. [
25] is that we could only obtain the skeletal anchorage by inserting two mini-screws in the palate and avoiding the invasive surgical placement and removal of the surgical mini-plates that were used with these treatment protocols (four and two mini-plates, respectively).
The dental relation showed a great improvement in increasing overjet clinically due to the improvement of the skeletal relations of both maxilla and mandible. This finding is also supported and is in line with Stephen, 2011 [
6] and Katyal et al. 2016 [
25]. Dental compensation was recorded due to the lip bumper effect of the lower labial arch, and spacing was noticed between incisors and/or premolars. This finding agreed with a study by Won 2013 [
26].
The soft tissue profile also showed an improvement as it became more convex due to a significant increase in the upper lip thickness (Ls-NB) as well as an increase in its protrusion (Ls-EL) [
27,
28]. A more protrusive position of the lower lip (Li-EL) was found, which may be attributed to the pressure from the labial bow of the lower part of the ASSD appliance.
The limitation encountered in this present study was the patients’ drop-out mainly because of the lack of patient compliance and motivation, the difficulty in following the study protocol in terms of the Alt. RAMEC of the ASSD appliances. In terms of the fabrication of ASSD appliances, there is a need for high technical and very skillful technicians as it is fully custom-made and easy to break at the solder joint.