Abstract
Adult patients with asthma often access the emergency department (ED) for the management of exacerbations or uncontrolled symptoms. Sometimes the first diagnosis of asthma occurs right in the ED. In the last couple of years, the COVID-19 pandemic spread around the world, causing an acute respiratory syndrome named SARS-CoV-2, characterized mainly by respiratory symptoms, such as cough and shortness of breath, in addition to fever. This clinical pattern partially overlaps with that caused by asthma, thus generating confusion in terms of diagnosis and management. It is also unclear whether asthma may be associated with a worse prognosis in COVID-19 infection. This expert opinion paper provides specific recommendations to ease the challenges related to adult patients with asthma admitted to the ED during the COVID-19 pandemic, with particular reference to diagnosis and treatment. Moreover, it provides well-defined indications to guide decisions on discharge, hospital admission, as well as follow-up. A panel of experts composed of emergency medicine physicians, pulmonologists and allergologists discussed, voted and approved all the recommendations.
1. Introduction
Asthma is a worldwide public health problem, in both children and adults, mainly because of its prevalence (over 300 million people) and chronicity, with a significant burden of morbidity and mortality [1]. Variable airway obstruction, airway hyper-responsiveness to specific triggers (viral infections, allergens, exercise, etc.) and chronic airway inflammation finally leading to an airway remodeling are peculiar aspects of this disease [2,3]. The diagnosis of asthma involves the combination of a characteristic pattern of respiratory symptoms and evidence of a variable expiratory flow limitation on spirometry [2,3]. The typical symptom pattern, especially in adults, consists of recurrent episodes of more than one of shortness of breath, wheezing, coughing and chest tightness worsening at night/early morning, variable in time and intensity and induced by several well-known trigger factors [2,3]. The guidelines emphasize differences in terminology that seem particularly important when talking about asthma in the ED [4]. The difference between uncontrolled and severe asthma is that in the former, symptoms are uncontrolled due to poor adherence or incorrect inhalation technique, whereas in the latter, symptoms are refractory or only partially responsive to treatment [4,5]. Exacerbation is an acute/subacute worsening of asthma from the patient’s usual status. In a minority of cases, it may represent the first presentation of asthma. Exacerbations are classified as mild, moderate and severe, but here, the term “severe” refers to the acute clinical picture and is defined on the basis of signs, symptoms and clinical parameters (see Section 2) [4]. Adult patients with asthma often need access to ED worldwide, requiring care for exacerbations or uncontrolled symptoms (uncontrolled or severe asthma) [4,5]. Sometimes the ED is even where asthma is first diagnosed in patients admitted for ongoing respiratory symptoms [5]. COVID-19 is the infectious disease caused by SARS-CoV-2, a coronavirus belonging to the same family of SARS-CoV-1 and MERS-CoV [6,7]. The main complication of SARS-CoV-2 infection is interstitial pneumonia associated with varying degrees of respiratory involvement, up to acute respiratory distress syndrome [6,8]. During the first pandemic wave and subsequent lockdowns, a significant decrease in emergency healthcare utilization was observed worldwide [9]. During the following waves, instead, the usual overcrowding of the ED returned. The need to properly separate the flows between patients with suspected and unlikely SARS-CoV-2 infection became even more pressing [9]. Separating the two flows is itself a difficult task, but it is even more complicated in patients with asthma.
Viral respiratory infections are well known as triggers for asthma exacerbations, especially in the development of more severe symptoms [10]. Data on clinical outcomes in asthmatic patients infected with SARS or MERS are scarce and conflicting, but asthma did not appear to worsen prognosis [11]. Because of the pandemic spread of SARS-CoV-2 infection, the literature has produced a large number of studies assessing the prevalence of asthma in COVID-19 populations and the influence of asthma and associated treatments on COVID-19 severity [12,13].
In the era of COVID-19, some diagnostic and therapeutic aspects related to asthma management, in the ED and after discharge, deserve to be discussed and addressed by the scientific community.
2. Materials and Methods
This was a survey originated by a multidisciplinary panel of experts in Rome, Italy, who participated in a meeting to develop a consensus on the management of asthma in the ED during the COVID-19 pandemic. The representative experts were emergency medicine physicians (M.G., M.P.R., S.B., F.D.M., P.C.), pulmonologists (M.B., L.F.) and allergologists (C.C.) from three different hospitals in the Rome metropolitan area (one university hospital and two community hospitals). They were recruited by the organizer (F.F.) according to the following selection criteria: publication history and/or direct clinical experience in the management of patients with asthma and/or the organizational and clinical management of the ED in the COVID-19 era. The meeting took place over two different occasions, via videoconference due to the pandemic. During the first meeting (24 September 2021), there was an open discussion facilitated by the chair (F.F.) about the personal experiences of the participants on the management of asthma in outpatient clinics or in the ED during the acute phase of the pandemic. The experts decided to form three workgroups to review the available scientific evidence and controversial aspects of the following key points:
- The “COVID-19 path” for asthma patients in the ED;
- Management of the adult patients with asthma in the ED at the time of the COVID-19 pandemic;
- The role of innovative respiratory hubs and telemedicine in the follow-up of adult patients with severe asthma after discharge from the ED.
Two authors (M.G. and M.B.) were commissioned before a second meeting to create a resource library for the panel members. They conducted an extensive evaluation of international guidelines, reviews and original articles written in English and published between 1 January 2012 and 1 March 2022. They searched PubMed, Scopus, Web of Science and Google Scholar, crossing the following Medical Subject Headings (MeSH): “Asthma”, “Asthma exacerbation”, “COVID-19”, “SARS-CoV-2”, “Emergency”, “Emergency department”, “Path”, “Telemedicine”, “Telehealth”. A manual search of the reference lists of selected articles was also performed. All duplicates were removed. After the screening, the authors (M.G. and A.S.) discussed with the chair (F.F.) and agreed on articles to be included in the final selection. Subsequently, access to this reference library was provided to all panelists, giving them the opportunity to add other relevant articles.
All the panel experts who attended the first meeting were also present at the second (11 March 2022). During the meeting, the three workgroups presented the most important aspects to be discussed for each key point and finally produced the main issues to be voted on. Four rounds of voting took place in the second part of the meeting, following the rules of the Delphi technique [14]. The recommendations in this paper are the result of consensus and majority opinion. Finally, the same authors who provided the literature review were commissioned by the group to prepare the manuscript based on the resource library and approved recommendations. The final version was reviewed and approved by all panel experts.
3. Results of the Survey
3.1. The “COVID-19 Path” for Asthma Patients in the ED
The COVID-19 pandemic continues to heavily affect the EDs around the world. In particular, a complete reorganization of the access routes was necessary. First, it is essential to correctly designate incoming patient flows to immediately separate those who are potentially infected from those who probably are not. Patients reporting respiratory symptoms (regardless of the presence of fever) and/or changes in taste and/or smell should flow directly to the “COVID-19 area”. In case of fever associated with clinical symptoms or signs of clear other non-respiratory origin, patients should flow into the “no COVID-19 area”. In this case, performing a point-of-care antigenic swab, if available, could be helpful, as a negative result significantly decreases the possibility of misdiagnosis of SARS-CoV-2 infection [15]. Because of the presence of dyspnea, which is also a common presentation of COVID-19 [2], all patients with a history or suspicion of asthma should initially flow into the COVID-19 path. After a rapid assessment of symptoms and temperature/vital parameters, management of patients with a suspected exacerbation of asthma should initially take place in the isolation area, and they should undergo molecular-based testing for the diagnosis of SARS-CoV-2 infection [16]. After the first medical examination, all such patients should undergo urgent chest radiography. Although not recommended per se in the entire asthmatic population attending the ED [2,17], this examination is useful for rapid screening for the presence of lung infiltrates suggestive of SARS-CoV-2 infection. Non-contrast high-resolution computed tomography (HRCT) shows high accuracy for COVID-19 pneumonia, sometimes preceding the positivity of molecular-based testing for SARS-CoV-2 [18,19]. However, some problems limit the use of HRCT for large-scale screening of COVID-19: its limited availability in many ED and the prolonged waiting times due to the transfer of potentially infected patients and the subsequent need for decontamination. For these reasons, in the ED setting, a dedicated portable chest radiograph can play an important role in the initial screening and diagnosis of COVID-19 [20]. It provides, in fact, lower sensitivity but similar specificity than that provided by the HRCT, for the diagnosis of COVID-19 [21]. Lung ultrasonography showed good sensitivity (similar to that of HRCT) but it is not specific for the diagnosis of COVID-19 (inferior to both HRCT and radiography) [22]. Lung ultrasound requires adequate expertise, but the learning curve is rather short. On the other hand, it involves closer proximity of the operator to the patient for a longer period, thus requiring specific infection prevention and control precautions. It is an alternative modality particularly useful in specific adult subgroups, for example, pregnant women [21].
After a complete clinical examination in the ED, all patients who receive a diagnosis of asthma exacerbation or a new diagnosis of asthma, who have both a negative radiological and nasopharyngeal swab for SARS-CoV-2 and who require further observation or hospitalization can be transferred to the no-COVID-19 area. Patients with a questionable clinical picture for COVID-19, and who cannot be discharged, should remain in the isolation area and repeat the nasopharyngeal swab 24 h after. In case of further negativity, they can switch to the “clean” path.
For more details on our proposal of a rational “COVID-19 path” in the ED, please refer to Figure 1.
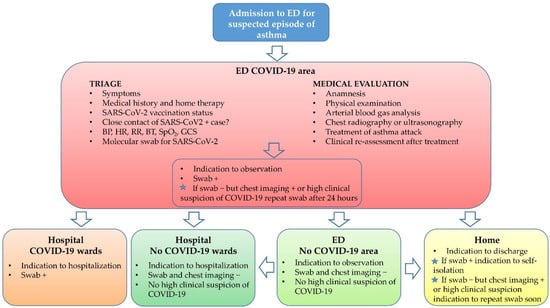
Figure 1.
Panel proposal of a rational “COVID-19 path” during a SARS-CoV-2 pandemic for the management of asthma patients in the emergency department (ED) from admission to discharge. Abbreviations and symbols: BP: blood pressure; HR: heart rate; RR: respiratory rate; BT: body temperature; SpO2: peripheral arterial oxygen saturation; GCS: Glasgow Coma Scale; +: positive; −: negative; swab: molecular nasopharyngeal swab for SARS-CoV-2.
3.2. Management of Adult Patients with Asthma in the ED at the Time of COVID-19 Pandemic
3.2.1. Assessing Patients’ Symptoms
In the ED, the first step in asthma management is to determine the severity of the patient’s symptoms at the time of admission [2]. Asthma exacerbation can be classified as mild, moderate and severe. The initial assessment should always include the ABCDE approach: if the patient shows drowsiness, confusion or silent chest, they are a candidate for intubation and admission to the intensive care unit (ICU). Patients unable to speak a few words, who strive to complete simple sentences, with visibly severe dyspnea, fatigued at rest and who need priority in the assessment and treatment, are cases of severe asthma. Moreover, respiratory rate >25 breaths/min, heart rate >110 beats/min and peripheral arterial oxygen saturation (SpO2) <90% require immediate medical intervention [23].
The symptoms and signs described above, associated with wheezing, bronchospasm and elevated respiratory rate, make the diagnostic hypothesis of asthma likely, even if other alternative diagnoses (e.g., bacterial pneumonia, bronchiectasis, pulmonary embolism, chronic obstructive pulmonary disease) must be ruled out. Yet, in the context of the SARS-CoV-2 pandemic, the diagnosis of asthma is a challenge for emergency physicians because of the overlap with COVID-19 respiratory symptoms [22,24,25].
Patients with severe COVID-19 disease often present with dyspnea, elevated respiratory rate, elevated compensatory heart rate, chest discomfort and dry cough, mimicking a severe asthma attack. A previous history of asthma, the presence of audible wheezing, rapid improvement of symptoms after taking beta-agonists and corticosteroids medications and the absence of fever suggest asthma exacerbation. On the contrary, patients with COVID-19 disease often access the ED with fever and dyspnea, have a history of close contact with positive cases, absence of wheezing and may present other symptoms such as myalgia, fatigue, headache, which are rare in asthma exacerbations. Moreover, they do not improve with inhaled medications.
On the other hand, since asthma patients have an increased susceptibility to viral infections [26], there is the potential to find a mixed picture of asthma exacerbation and COVID-19 infection in the same patient [24]. Current guidelines recommend measurement of peak expiratory flow (PEF), when available directly in the ED, to objectify asthma severity, rather than signs and symptoms alone. In fact, PEF <50% indicates severe asthma, while PEF 50–75% indicates moderate asthma [3,27,28,29,30,31].
Because of the current pandemic and the associated risk of virus spread, experts suggest measuring PEF in an open space. PEF could be also useful in differential diagnosis between asthma and COVID-19, given the absence of an obstructive component in the latter.
However, in our opinion, PEF is not an easy test to perform in the ED because of overcrowding, the small number of open spaces and risk of transmission of COVID-19 by stimulating cough. In addition, a patient with severe asthma exacerbation and severe respiratory distress dyspnea, who is unable to speak, may not be able to undergo PEF.
3.2.2. Asthma and COVID-19: What We Know Today
According to current literature data, patients with asthma have a reduced or at least not increased risk of SARS-CoV-2 infection [32,33]. Since the angiotensin-converting enzyme 2 (ACE-2) receptor is the well-known gateway for virus entry into the human body, the downregulation of its expression observed in asthmatics may help explain the reduced susceptibility of these patients to SARS-CoV-2 infection [13,34,35]. The reduced expression of ACE-2 receptors seems to be the effect of IL-13 activity produced by eosinophil cells [33,34]. In addition, patients with asthma have a similar risk of hospitalization, complications and death compared with the general population [13,24,35,36,37,38,39]. Probably the imbalance toward the T2-type immune response, observed in this population, counteracts the typical T1-type response in COVID-19, reducing the risk of complications due to proinflammatory Th1-cytokines, such as IL-6, among others [33,40,41,42,43,44,45]. Ferastraoaru et al. [46] showed a potential protective role of eosinophilia in asthmatic patients with COVID-19. Specifically, in symptomatic asthmatics with COVID-19 infection, the Th2-asthma phenotype characterized by eosinophilia in peripheral blood (150 cells/mL) was associated with reduced hospitalization.
The initial concern that patients chronically receiving inhaled or oral corticosteroids or biologic drugs could be at risk of worse outcome in the case of SARS-CoV-2 infection has not been confirmed by the literature data available to date [47,48,49,50].
Interestingly, in outpatients with SARS-CoV-2 infection and mild symptoms, inhaled corticosteroids seem to reduce the combined endpoint represented by admission to hospital or death to increase the resolution of symptoms at two weeks [51].
Results from the literature support the benefit of systemic corticosteroids in the treatment of severe asthma and asthma exacerbations [52,53,54]. The RECOVERY trial [52], by far the largest randomized controlled study examining the role of corticosteroids in COVID-19 disease, showed a clear benefit in 28-day mortality with the use of dexamethasone at the dosage of 6 mg/day for 10 days in COVID-19 patients on oxygen supplementation or invasive mechanical ventilation. This benefit was absent in the group not requiring oxygen supplementation, in which a slight increase in mortality was observed but did not reach statistical significance. Based on the evidence available to date [3,22,47,55,56], we suggest that asthmatic patients should continue their prescribed asthma therapy, even when it includes oral or inhaled corticosteroids and/or biological drugs (e.g., omalizumab, mepolizumab, reslizumab, benralizumab, dupilumab, etc.) Physicians could evaluate, case by case, a modification of their therapy if SARS-CoV-2 infection arises.
Similarly, given the literature data, in the presence of asthma and COVID-19 without the need for oxygen supplementation, if there is an indication for corticosteroid use based on the presence of severe asthma or exacerbation of asthma, we recommend starting treatment.
3.2.3. Medical Treatment of Severe Asthma Exacerbations in the COVID-19 Era in the Emergency Department
In the absence of data from targeted studies, the overall treatment of severe asthma exacerbations should not change substantially at the time or in the presence of SARS-CoV-2 infection [3,23,57].
The recurring warning to emergency physicians is to limit aerosol treatments to reduce the virus spread to patients who, due to common overcrowding of ED, are often too many compared to the available space. Some authors emphasized that a pressurized metered dose inhaler (MDI) via a spacer should be preferred to nebulizers (except for life-threatening exacerbations) to minimize aerosol and droplet generation [23]. In addition, a mouthpiece or mask can be added to the spacer if the patients need it [3,31,48,53,57]. Experiences during the COVID-19 pandemic suggest that MDI was comparable to nebulizers (in terms of efficacy and patient acceptance) in treating mild to moderate asthma exacerbations in the ED [58]. However, there is no concrete evidence of a difference in aerosol and droplet generation between these two routes of inhaled drug delivery (MDI vs. nebulizers) [23]. Given this lack of evidence, we recommend using the available devices to minimize the delay in drug delivery, preferring the MDI if possible [59,60]. In the ED, patients with severe asthma should be treated with inhaled β2-agonists (e.g., salbutamol) and inhaled anticholinergics (e.g., ipratropium bromide) with continuous or repeated nebulization.
Concomitant oxygen supplementation is recommended when saturation is <90%. There are no significant differences regarding this cut-off in the case of concomitant COVID-19 [54,55,56]. Administration of systemic corticosteroids should occur early, possibly within 1 h of admission to the ED [61,62,63]. As aforementioned, again, nothing changes if the patient has concomitant SARS-CoV-2 infection, since the potential better clinical outcome of severe COVID-19 with corticosteroids administration.
Intravenous (IV) magnesium sulfate [64], β2-agonists (e.g., salbutamol) and methylxanthines (e.g., theophylline) can be added if clinical improvement is incomplete or absent, up to subcutaneous (SC) administration of epinephrine [17,65,66]. The criteria for intubation of asthma patients remain unchanged. Obviously, asthmatics with concomitant SARS-CoV-2 infection complicated by acute respiratory failure and criteria for ARDS also require aggressive respiratory support with intubation, invasive ventilation and admission to ICU [2,65,66].
There is limited evidence that antibiotic therapy may improve symptoms with respect to standard care or placebo, in asthma exacerbation. Literature evidence is even insufficient to reach firm conclusions about some important outcomes, such as hospital admission and mortality. For these reasons, we recommend not administering antibiotics in patients with asthma exacerbations unless there is clear evidence of bacterial infection/superinfection [67]. Table 1 shows a comparison of some major issues related to asthma management before and during the COVID-19 pandemic.

Table 1.
Comparison of some major issues related to asthma management before and during COVID-19 pandemic in the emergency department (ED). Red face: expert opinion panel against; green face: expert opinion panel in favor. Abbreviations: MDI, pressurized metered dose inhaler; PEF, peak expiratory flow, SpO2, peripheral arterial oxygen saturation.
3.2.4. Hospitalization and Discharge of Asthmatic Patients during COVID-19 Disease
According to the available literature, clinical assessment of patients with asthma attacks admitted to the ED is crucial to decide whether to discharge, observe or hospitalize them [68,69,70,71,72]. Different levels of severity of asthma attacks (mild, moderate, severe, life threatening, fatal, brittle, etc.) influence this choice [34,73,74]. The coexistence of SARS-CoV-2 infection may lead emergency physicians to decide on hospitalization, concerned about the presence of two acute diseases with potential short-term recurrence or evolution [38,65,75,76,77,78]. However, as mentioned above, the association between asthma and SARS-CoV-2 infection should not in itself be an indication of hospitalization. The recovery rate was similar between asthmatics and non-asthmatics [79]. Hospitalization is recommended [3,30,31,54,55,80] for patients with:
- (1)
- Respiratory failure, severe respiratory distress, cyanosis, use of accessory muscles and altered mental status with impaired consciousness, after treatment and reassessment;
- (2)
- Hypoxia with SpO2 < 92% after treatment and elevated PCO2 > 45 mmHg; near fatal asthma; presence of complications (e.g., pneumothorax, pneumomediastinum, atelectasis, arrhythmia);
- (3)
- History of previous severe asthma attacks (e.g., >3 ED visits or >2 hospitalizations in the past 12 months or previous intubation or management in ICU for asthma);
- (4)
- Poor family support or difficulty in reaching the hospital in case of further deterioration;
- (5)
- Significant medical comorbidities; psychological problems with concerns about compliance;
- (6)
- Recent steroid use;
Need for therapy more frequently than every 4 h. Observation may be the best option [3,30,31,54,55,80] for patients:
- (1)
- With stable vital signs, partial response to therapy (beta-2 agonists plus steroids in the ED), with clinical improvement but still presence of wheezing;
- (2)
- Who need medical reassessment because they do not improve adequately with the initial therapy;
- (3)
- Whose discharge is unsafe because of concerns about therapy compliance or follow-up.
Discharge [3,30,31,54,55,80] is indicated for stable patients admitted to the ED with mild to moderate symptoms, who have a good response to inhaled treatments, resolution of bronchospasm, stable oxygen saturation >94% and whose need for fast-acting bronchodilators is <1 dose every 4 h. These patients should be discharged with steroid and nebulizer prescriptions, planned follow-up and counseling for cessation of risk factors when necessary [81].
3.3. The Role of Innovative Respiratory Hubs and Telemedicine in the Follow-Up of Adult Patients with Severe Asthma after Discharge from the ED
The COVID-19 pandemic keeps challenging national and international healthcare systems, overwhelmed in their emergency care units and often unable to provide adequate management of chronic diseases. Recommendations for social distancing and patients’ fear of infection during face-to-face visits led, at least initially, to a dramatic reduction in routine clinical follow-ups and execution of diagnostic tests. This has a significant impact on patients with chronic respiratory diseases, particularly severe asthmatics, with an increased risk of worsening airway symptoms, impaired quality of life, acute exacerbations and, as a result, admission to ICU.
Therefore, the usual clinical setting of an outpatient asthma clinic needs complete rethinking and restructuring according to a new concept of medical assistance that can ensure patient safety against SARS-CoV-2 infection while delivering high-quality care. From a practical point of view, respiratory healthcare professionals, who are supposed to perform pulmonary function tests and exhaled breath measurements, should adopt protective measures such as gloves, filtering face masks (FFP) 2 or 3, full eye protection, powered air-purifying respirators (PAPRs) and protective clothing [2,82]. Furthermore, it is recommended to limit direct patient contact and promote compliance with general hygiene measures. In addition, the outpatient clinic should be set as a COVID-free space, with a wide waiting area separated from the consulting room, featuring a good ventilation system. Visits should be scheduled at proper time intervals, prioritizing patients with a clear need for in-person consultation. Among them, special attention should be given to patients recently discharged from the ED and/or the hospital, recovering from asthma exacerbation episodes, or with severe symptoms despite adequate chronic treatment. Close and effective collaboration between ED physicians and pulmonologists is crucial for a multidisciplinary asthma approach and for setting up a fast track aimed to guarantee timely specialist respiratory management once the acute phase of the disease has resolved. Such a prompt clinical assessment is critical to achieving optimal disease control and preventing new acute exacerbations, with a consequent ED overstay and overcrowding [82].
Guidelines [2,4] recommend arranging early follow-up after any exacerbation, within 2–7 days for adults. All patients should be followed regularly until symptoms are controlled and lung function returns to normal. At each follow-up visit, it is important to review modifiable risk factors, reliever and controller medications, inhaler techniques, patient self-monitoring, adherence, patient concerns and the short- and long-term asthma action plan [2,4]. Moreover, asthma patients need to obtain lung function measures by spirometry at least every 1 to 2 years. The timing of follow-up should be personalized according to patients’ needs. It can be arranged every 2 to 6 weeks while the patient gains symptom control, every 1 to 6 months to monitor symptom control, every 3 months if asthma is well controlled, and a step down in therapy is needed, to reduce inhaled corticosteroids. Thereafter, it should be performed every 6 months for patients with well-controlled asthma [83,84]. In our opinion, concomitant SARS-CoV-2 infection does not change the scheduled follow-up period, which should occur, as described above, according to the patient’s needs and symptoms.
On the other hand, the recommendation to maintain social distancing and reschedule any non-essential visit and procedure has provided several opportunities for the expansion of electronic health, a novel approach defined as “an emerging field at the intersection of medical informatics, public health and business, referring to health services and information delivered or enhanced through the internet and related technologies”. E-health encompasses a wide variety of subdomains such as telemedicine, digital apps, mobile health, virtual healthcare teams, electronic health records (EHRs), medication trackers and clinical decision support systems. Specifically, telemedicine refers to the use of telecommunications and information technology (IT), with the aim of providing easier and personalized health assessment, including diagnosis, management, consultation and information from distance. Although technological improvements in the recent past have dramatically increased the accessibility and quality of medical care through digital media, this process has accelerated further in the context of the ongoing COVID-19 pandemic. Telemedicine has the potential to improve the quality of care and adherence to therapy and allow early detection of disease worsening through continuous monitoring and real-time feedback to patients. Telemedicine strategies have been shown to be effective in the management of a range of chronic diseases, including asthma, by enabling patient empowerment and behavior changes [85,86]. Moreover, there is a growing demand from patients to use electronic-based solutions to deal with their diseases. Potential additional benefits of telemedicine include cost reduction and social distancing [4,5]. Through a reshaped outpatient asthma clinic healthcare, some tools could also be used for a triage process, assisting physicians to differentiate COVID-19 symptoms from those due to the common cold and asthma. Moreover, virtual platforms can be set to facilitate interactions between providers and patients, using e-mails, text messages and video chat via computer or other electronic devices (e.g., smartphones, tablets). This interactive internet-based asthma care can lead to remote patient monitoring through home spirometry results, peak flow reading and analysis of asthma diaries and symptom questionnaires. It has been demonstrated that the adoption of a special reminder system can be a valuable tool to improve proper inhalation technique and treatment adherence [87]. Telemedicine can also support patients treated with biological agents by facilitating the transmission of laboratory/radiological markers needed for eligibility and monitoring, as well as medical prescriptions and treatment plans.
The ongoing COVID-19 outbreak has challenged healthcare systems worldwide. The traditional approach has demonstrated intrinsic problems and limitations, such as overwhelmed public hospitals, dire shortage of personal protective equipment and difficulties in remote patient assistance. However, the pandemic points towards reforms that could improve our ability to serve new healthcare needs. Therefore, a reorganization and digital evolution of the asthma outpatient clinic may improve diagnosis and management of the disease.
4. Discussion
This paper is the result of the consensus of an expert panel on the main issues related to the management of adult asthma patients in the ED during the COVID-19 pandemic.
Patients with acute or worsening or exacerbating asthma are often guests in our EDs [5]. However, clinical studies on this setting (especially of high-quality) are lacking, and most guidelines and review articles did not assess this specific topic or treat it marginally [3,57,88,89,90,91,92,93,94,95].
To best care for such type of patient, especially in the current era, it is essential to identify the right COVID-19 path and best management in the ED and, after hospital discharge, the most innovative and functional follow-up options.
Regarding the first key point, no literature data are available on which is the right COVID-19 path for adult asthma patients. In EDs around the world, it was necessary to revise clinical paths and create separate areas to prevent the spread of in-hospital infection from SARS-CoV-2. In light of the literature evidence and, perhaps more importantly, of the common sense of those who know the dynamics of the ED in depth, the expert panel suggested a plausible COVID-19 path to be used for asthma patients. Although pre-COVID-19 guidelines do not recommend first-line chest imaging in all asthmatics attending the ED, our suggestion to perform it arose from the rationale of assessing for possible concomitant SARS-CoV-2 pneumonia [20,21].
There is also a lack of specific data in the literature on the management of asthma attacks in adult patients within the ED. The proposal of several scientific societies or review articles to avoid nebulizers for the administration of bronchodilators and topic corticosteroids arose in the context of appropriate infection control precautions. Our expert panel agreed with this preference but, in the absence of solid evidence, suggested utilizing the available devices to minimize the delay in drug administration. This applies not only to severe attacks, where there is generally no doubt about the indication for nebulization, but also to non-severe ones, because in acute asthma, prompt therapy prevents worsening of the clinical picture. Moreover, in the absence of specific literature data, the pharmacological treatment of acute asthma and the indication of oxygen support and/or respiratory assistance remain unchanged, also in case of concomitant COVID-19. There is no strong evidence against the administration of systemic corticosteroids, even in patients with SARS-CoV-2 infection, if indicated for asthmatic clinical picture. Thus, our suggestion was in line with the literature data and is similar to most guidelines and review articles that specifically address the issue of administration of these drugs in patients with asthma exacerbation.
Even in the case of the third key point, namely the suggestion to implement an e-health system for the management and follow-up of adult patients with asthma discharged from the ED, the suggestion of the panel agreed with the available literature and guideline recommendations.
In our view, the main strength of this paper was to provide the first focused, most comprehensive, up-to-date and educational guideline possible for the management of asthma patients in the ED at the time of COVID-19. To do so, we combined an exhaustive review of the available literature with a consensus among experts from the three main disciplines involved in the management of asthma (emergency medicine physicians, pulmonologists and allergists), balancing the presence of specialists from university and community hospitals. This process allowed discussion of best practices in the absence of high-quality evidence. In fact, lacking robust literature data, it was not possible to provide a systematic literature review consistent with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards [96]. However, the absence of targeted and high-quality findings on which to base recommendations remains a limit. Large-scale prospective trials on this type of patient are desirable in the near future. In our view, another limitation was the fact that the panel consisted of a small group of experts and that they all came from the same geographical area. This could have made the process used to acquire the final recommendations less effective and these recommendations less generalizable on a large scale.
5. Conclusions
Asthma management in the SARS-CoV-2 era represents a challenge for all physicians, particularly those working in emergency care settings. Indeed, clear evidence is still lacking, and many questions remain open. Table 2 summarizes the key points that emerged from this survey to guide the management of patients with asthma in the emergency department.

Table 2.
Key points to guide the management of adult patients with asthma in the emergency department (ED).
A multidisciplinary approach particularly for the most complex cases is desirable for an optimal, tailored and safe diagnostic and therapeutic approach to adult patients with asthma during the COVID-19 pandemic period. It is reasonable to assume that accurate phenotyping of clinical severity of the asthma patient with SARS-CoV-2 infection may confirm the hypothesis that there is a phenotype that is less vulnerable towards a more severe evolution of coronavirus infection.
Author Contributions
Conceptualization, F.F., S.B. and M.P.R.; methodology, F.F., C.C., L.F. (Leonello Fuso), P.C. and M.G.; resources, F.F. and F.D.M.; data curation, F.D.M.; writing—original draft preparation, M.G., A.S., M.B. and C.B.; writing—review and editing, F.F., L.F. (Laura Franza), M.B. and C.C.; visualization, M.G. and M.B.; project administration, F.F.; funding acquisition, F.F. All authors have read and agreed to the published version of the manuscript.
Funding
After acceptance of the article, a support for open access fee was provided by Novartis Farma S.p.A.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Holgate, S.T.; Wenzel, S.; Postma, D.S.; Weiss, S.T.; Renz, H.; Sly, P.D. Asthma. Nat. Rev. Dis. Primers 2015, 1, 15025. [Google Scholar] [CrossRef] [PubMed]
- McCracken, J.L.; Veeranki, S.P.; Ameredes, B.T.; Calhoun, W.J. Diagnosis and Management of Asthma in Adults: A Review. JAMA 2017, 318, 279–290. [Google Scholar] [CrossRef]
- Reddel, H.K.; Bacharier, L.B.; Bateman, E.D.; Brightling, C.E.; Brusselle, G.G.; Buhl, R.; Cruz, A.A.; Duijts, L.; Drazen, J.M.; FitzGerald, J.M.; et al. Global Initiative for Asthma Strategy 2021: Executive summary and rationale for key changes. Eur. Respir. J. 2022, 59, S1–S18. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 2014, 43, 343–373. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, F.R.; Guglielmelli, E.; Angelini, D.; Cicchini, C.; Castaldo, E.; Di Girolamo, F.; Fedeli, A.; Ronzoni, D.; Rumi, F.; Franceschi, F. Pharmacoeconomic management of patient with severe asthma in the Emergency Department: Retrospective multicentric and cost of illness study. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 11729–11739. [Google Scholar] [CrossRef] [PubMed]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Carius, B.M.; Chavez, S.; Liang, S.Y.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Clinical update on COVID-19 for the emergency clinician: Presentation and evaluation. Am. J. Emerg. Med. 2022, 54, 46–57. [Google Scholar] [CrossRef]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Mantica, G.; Riccardi, N.; Terrone, C.; Gratarola, A. Non-COVID-19 admissions to the emergency department during the pandemic second wave in Italy: What is changed from the first wave? Am. J. Emerg. Med. 2021, 45, 625–626. [Google Scholar] [CrossRef]
- Busse, W.W.; Lemanske, R.F., Jr.; Gern, J.E. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet 2010, 376, 826–834. [Google Scholar] [CrossRef]
- Yin, Y.; Wunderink, R.G. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018, 23, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Gabrielli, M.; Pignataro, G.; Candelli, M.; Sacco Fernandez, M.; Bizzarri, M.; Esperide, A.; Franceschi, F.; Gemelli Against, C. Asthma in patients admitted to emergency department for COVID-19: Prevalence and risk of hospitalization. Intern. Emerg. Med. 2022, 17, 917–920. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Yu, P.; Li, Y.; Wang, J.; Li, Z.; Qiu, J.; Cui, L.; Mou, Y.; Sun, Y. Asthma does not influence the severity of COVID-19: A meta-analysis. J. Asthma 2021, 59, 1188–1194. [Google Scholar] [CrossRef] [PubMed]
- McMillan, S.S.; King, M.; Tully, M.P. How to use the nominal group and Delphi techniques. Int. J. Clin. Pharm. 2016, 38, 655–662. [Google Scholar] [CrossRef]
- Möckel, M.; Corman, V.M.; Stegemann, M.S.; Hofmann, J.; Stein, A.; Jones, T.C.; Gastmeier, P.; Seybold, J.; Offermann, R.; Bachmann, U.; et al. SARS-CoV-2 antigen rapid immunoassay for diagnosis of COVID-19 in the emergency department. Biomarkers 2021, 26, 213–220. [Google Scholar] [CrossRef]
- Hanson, K.E.; Altayar, O.; Caliendo, A.M.; Arias, C.A.; Englund, J.A.; Hayden, M.K.; Lee, M.J.; Loeb, M.; Patel, R.; El Alayli, A.; et al. The Infectious Diseases Society of America Guidelines on the Diagnosis of COVID-19: Antigen Testing. Clin. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Cloutier, M.M.; Dixon, A.E.; Krishnan, J.A.; Lemanske, R.F., Jr.; Pace, W.; Schatz, M. Managing Asthma in Adolescents and Adults: 2020 Asthma Guideline Update From the National Asthma Education and Prevention Program. JAMA 2020, 324, 2301–2317. [Google Scholar] [CrossRef]
- Ai, T.; Yang, Z.; Hou, H.; Zhan, C.; Chen, C.; Lv, W.; Tao, Q.; Sun, Z.; Xia, L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology 2020, 296, E32–E40. [Google Scholar] [CrossRef]
- Lee, E.Y.P.; Ng, M.Y.; Khong, P.L. COVID-19 pneumonia: What has CT taught us? Lancet Infect. Dis. 2020, 20, 384–385. [Google Scholar] [CrossRef]
- Jacobi, A.; Chung, M.; Bernheim, A.; Eber, C. Portable chest X-ray in coronavirus disease-19 (COVID-19): A pictorial review. Clin. Imaging 2020, 64, 35–42. [Google Scholar] [CrossRef]
- Islam, N.; Ebrahimzadeh, S.; Salameh, J.P.; Kazi, S.; Fabiano, N.; Treanor, L.; Absi, M.; Hallgrimson, Z.; Leeflang, M.M.; Hooft, L.; et al. Thoracic imaging tests for the diagnosis of COVID-19. Cochrane Database Syst. Rev. 2021, 3, Cd013639. [Google Scholar] [CrossRef] [PubMed]
- Beasley, R.; Hills, T.; Kearns, N. Asthma and COVID-19: Preconceptions about Predisposition. Am. J. Respir. Crit. Care Med. 2021, 203, 799–801. [Google Scholar] [CrossRef] [PubMed]
- Beaney, T.; Salman, D.; Samee, T.; Mak, V. Assessment and management of adults with asthma during the covid-19 pandemic. BMJ 2020, 369, m2092. [Google Scholar] [CrossRef] [PubMed]
- Alberca, R.W.; Yendo, T.; Aoki, V.; Sato, M.N. Asthmatic patients and COVID-19: Different disease course? Allergy 2021, 76, 963–965. [Google Scholar] [CrossRef]
- Mendes, N.F.; Jara, C.P.; Mansour, E.; Araújo, E.P.; Velloso, L.A. Asthma and COVID-19: A systematic review. Allergy Asthma Clin. Immunol. 2021, 17, 5. [Google Scholar] [CrossRef]
- Mikhail, I.; Grayson, M.H. Asthma and viral infections: An intricate relationship. Ann. Allergy Asthma Immunol. 2019, 123, 352–358. [Google Scholar] [CrossRef]
- Mauer, Y.; Taliercio, R.M. Managing adult asthma: The 2019 GINA guidelines. Clevel. Clin. J. Med. 2020, 87, 569–575. [Google Scholar] [CrossRef]
- Saglani, S.; Menzie-Gow, A.N. Approaches to Asthma Diagnosis in Children and Adults. Front. Pediatr. 2019, 7, 148. [Google Scholar] [CrossRef]
- Drake, S.M.; Simpson, A.; Fowler, S.J. Asthma Diagnosis: The Changing Face of Guidelines. Pulm. Ther. 2019, 5, 103–115. [Google Scholar] [CrossRef]
- Ish, P.; Malhotra, N.; Gupta, N. GINA 2020: What’s new and why? J. Asthma 2021, 58, 1273–1277. [Google Scholar] [CrossRef]
- Boulet, L.P.; Reddel, H.K.; Bateman, E.; Pedersen, S.; FitzGerald, J.M.; O’Byrne, P.M. The Global Initiative for Asthma (GINA): 25 years later. Eur. Respir. J. 2019, 54, 1900598. [Google Scholar] [CrossRef] [PubMed]
- Bonser, L.R.; Eckalbar, W.L.; Rodriguez, L.; Shen, J.; Koh, K.D.; Ghias, K.; Zlock, L.T.; Christenson, S.; Woodruff, P.G.; Finkbeiner, W.E.; et al. The Type 2 Asthma Mediator IL-13 Inhibits Severe Acute Respiratory Syndrome Coronavirus 2 Infection of Bronchial Epithelium. Am. J. Respir. Cell Mol. Biol. 2022, 66, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.B.; Wang, L.; Fu, X.; Wallace, Z.S.; Long, A.A.; Zhang, Y.; Camargo, C.A., Jr.; Blumenthal, K.G. COVID-19 severity in asthma patients: A multi-center matched cohort study. J. Asthma 2022, 59, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Lee, S.; Krings, J.G.; Rauseo, A.M.; Reynolds, D.; Presti, R.; Goss, C.; Mudd, P.A.; O’Halloran, J.A.; Wang, L. Asthma in patients with suspected and diagnosed coronavirus disease 2019. Ann. Allergy Asthma Immunol. 2021, 126, 535–541.e2. [Google Scholar] [CrossRef]
- Sunjaya, A.P.; Allida, S.M.; Di Tanna, G.L.; Jenkins, C. Asthma and risk of infection, hospitalization, ICU admission and mortality from COVID-19: Systematic review and meta-analysis. J. Asthma 2022, 59, 866–879. [Google Scholar] [CrossRef]
- Liu, S.; Cao, Y.; Du, T.; Zhi, Y. Prevalence of Comorbid Asthma and Related Outcomes in COVID-19: A Systematic Review and Meta-Analysis. J. Allergy Clin. Immunol. Pract. 2021, 9, 693–701. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, J.; Chen, W.; Liu, L.; Dong, M.; Ji, J.; Hu, D.; Zhang, N. Does Asthma Increase the Mortality of Patients with COVID-19?: A Systematic Review and Meta-Analysis. Int. Arch. Allergy Immunol. 2021, 182, 76–82. [Google Scholar] [CrossRef]
- Garcia-Pachon, E.; Grau-Delgado, J.; Soler-Sempere, M.J.; Zamora-Molina, L.; Baeza-Martinez, C.; Ruiz-Alcaraz, S.; Padilla-Navas, I. Low prevalence of post-COVID-19 syndrome in patients with asthma. J. Infect. 2021, 82, 276–316. [Google Scholar] [CrossRef]
- Skene, I.P.; Pfeffer, P.E. Improved asthma control during the COVID-19 pandemic: Are there lessons to be learnt? Thorax 2021, 76, 852–853. [Google Scholar] [CrossRef]
- Kannan, S.; Shaik Syed Ali Pakeer, P.; Sheeza Ali, A.; Hemalatha, K. Reply Letter—COVID-19 (Novel Coronavirus 2019)—Recent trends. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 6482–6483. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; van den Berge, M.; Boccabella, C.; Bonini, M.; Caruso, C.; Couto, M.; Erkekol, F.; Rukhadze, M.; Sanchez-Garcia, S.; Del Giacco, S.; et al. Real-life impact of COVID-19 pandemic lockdown on the management of pediatric and adult asthma: A survey by the EAACI Asthma Section. Allergy 2021, 76, 2776–2784. [Google Scholar] [CrossRef]
- Wang, L.; Wang, Y.; Ye, D.; Liu, Q. Review of the 2019 novel coronavirus (SARS-CoV-2) based on current evidence. Int. J. Antimicrob. Agents 2020, 55, 105948. [Google Scholar] [CrossRef]
- Wu, D.; Wu, T.; Liu, Q.; Yang, Z. The SARS-CoV-2 outbreak: What we know. Int. J. Infect. Dis. 2020, 94, 44–48. [Google Scholar] [CrossRef]
- Singhal, T. A Review of Coronavirus Disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef]
- Ashour, H.M.; Elkhatib, W.F.; Rahman, M.M.; Elshabrawy, H.A. Insights into the Recent 2019 Novel Coronavirus (SARS-CoV-2) in Light of Past Human Coronavirus Outbreaks. Pathogens 2020, 9, 186. [Google Scholar] [CrossRef]
- Ferastraoaru, D.; Hudes, G.; Jerschow, E.; Jariwala, S.; Karagic, M.; de Vos, G.; Rosenstreich, D.; Ramesh, M. Eosinophilia in Asthma Patients Is Protective Against Severe COVID-19 Illness. J. Allergy Clin. Immunol. Pract. 2021, 9, 1152–1162.e1153. [Google Scholar] [CrossRef]
- Lafaurie, M.; Martin-Blondel, G.; Delobel, P.; Kamar, N.; Charpentier, S.; Sommet, A.; Moulis, G. Impact of previous exposure to systemic corticosteroids on unfavorable outcome in patients hospitalized for COVID-19. BMC Pharmacol. Toxicol. 2021, 22, 14. [Google Scholar] [CrossRef]
- Halpin, D.M.G.; Singh, D.; Hadfield, R.M. Inhaled corticosteroids and COVID-19: A systematic review and clinical perspective. Eur. Respir. J. 2020, 55, 2001009. [Google Scholar] [CrossRef]
- Choi, J.C.; Jung, S.Y.; Yoon, U.A.; You, S.H.; Kim, M.S.; Baek, M.S.; Jung, J.W.; Kim, W.Y. Inhaled Corticosteroids and COVID-19 Risk and Mortality: A Nationwide Cohort Study. J. Clin. Med. 2020, 9, 3406. [Google Scholar] [CrossRef]
- Adir, Y.; Humbert, M.; Saliba, W. COVID-19 risk and outcomes in adult asthmatic patients treated with biologics or systemic corticosteroids: Nationwide real-world evidence. J. Allergy Clin. Immunol. 2021, 148, 361–367.e13. [Google Scholar] [CrossRef]
- Griesel, M.; Wagner, C.; Mikolajewska, A.; Stegemann, M.; Fichtner, F.; Metzendorf, M.I.; Nair, A.A.; Daniel, J.; Fischer, A.L.; Skoetz, N. Inhaled corticosteroids for the treatment of COVID-19. Cochrane Database Syst. Rev. 2022, 3, Cd015125. [Google Scholar] [CrossRef] [PubMed]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Shi, L.; Xu, J.; Xiao, W.; Wang, Y.; Jin, Y.; Chen, S.; Duan, G.; Yang, H. Asthma in patients with coronavirus disease 2019: A systematic review and meta-analysis. Ann. Allergy Asthma Immunol. 2021, 126, 524–534. [Google Scholar] [CrossRef]
- Busse, W.W.; Fang, J.; Marvel, J.; Tian, H.; Altman, P.; Cao, H. Uncontrolled asthma across GINA treatment steps 2 - 5 in a large US patient cohort. J. Asthma 2022, 59, 1051–1062. [Google Scholar] [CrossRef]
- Kuprys-Lipinska, I.; Kolacinska-Flont, M.; Kuna, P. New approach to intermittent and mild asthma therapy: Evolution or revolution in the GINA guidelines? Clin. Transl. Allergy 2020, 10, 19. [Google Scholar] [CrossRef]
- Motta, L.P.; Silva, P.; Borguezan, B.M.; Amaral, J.; Milagres, L.G.; Bóia, M.N.; Ferraz, M.R.; Mogami, R.; Nunes, R.A.; Melo, P.L. An emergency system for monitoring pulse oximetry, peak expiratory flow, and body temperature of patients with COVID-19 at home: Development and preliminary application. PLoS ONE 2021, 16, e0247635. [Google Scholar] [CrossRef]
- Levin, M.; Ansotegui, I.J.; Bernstein, J.; Chang, Y.S.; Chikhladze, M.; Ebisawa, M.; Fiocchi, A.; Heffler, E.; Martin, B.; Morais-Almeida, M.; et al. Acute asthma management during SARS-CoV2-pandemic 2020. World Allergy Organ J. 2020, 13, 100125. [Google Scholar] [CrossRef] [PubMed]
- Koh, H.P.; Shamsudin, N.S.; Tan, M.M.Y.; Mohd Pauzi, Z. The outcomes and acceptance of pressurized metered-dose inhaler bronchodilators with venturi mask modified spacer in the outpatient emergency department during the COVID-19 pandemic. J. Clin. Pharm. Ther. 2021, 46, 1129–1138. [Google Scholar] [CrossRef]
- Goldstein, K.M.; Ghadimi, K.; Mystakelis, H.; Kong, Y.; Meng, T.; Cantrell, S.; Von Isenburg, M.; Gordon, A.; Ear, B.; Gierisch, J.M.; et al. Risk of Transmitting Coronavirus Disease 2019 During Nebulizer Treatment: A Systematic Review. J. Aerosol. Med. Pulm. Drug Deliv. 2021, 34, 155–170. [Google Scholar] [CrossRef]
- Tran, K.; Cimon, K.; Severn, M.; Pessoa-Silva, C.L.; Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS ONE 2012, 7, e35797. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, J.A.; Davis, S.Q.; Naureckas, E.T.; Gibson, P.; Rowe, B.H. An umbrella review: Corticosteroid therapy for adults with acute asthma. Am. J. Med. 2009, 122, 977–991. [Google Scholar] [CrossRef] [PubMed]
- Rowe, B.H.; Spooner, C.H.; Ducharme, F.M.; Bretzlaff, J.A.; Bota, G.W. Corticosteroids for preventing relapse following acute exacerbations of asthma. Cochrane Database Syst. Rev. 2001, 1, Cd000195. [Google Scholar] [CrossRef]
- Rowe, B.H.; Spooner, C.; Ducharme, F.M.; Bretzlaff, J.A.; Bota, G.W. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst. Rev. 2001, 1, Cd002178. [Google Scholar] [CrossRef] [PubMed]
- Rowe, B.H.; Camargo, C.A., Jr. The role of magnesium sulfate in the acute and chronic management of asthma. Curr. Opin. Pulm. Med. 2008, 14, 70–76. [Google Scholar] [CrossRef]
- Calzetta, L.; Matera, M.G.; Coppola, A.; Rogliani, P. Prospects for severe asthma treatment. Curr. Opin. Pharmacol. 2021, 56, 52–60. [Google Scholar] [CrossRef]
- Papiris, S.A.; Manali, E.D.; Kolilekas, L.; Triantafillidou, C.; Tsangaris, I. Acute severe asthma: New approaches to assessment and treatment. Drugs 2009, 69, 2363–2391. [Google Scholar] [CrossRef]
- Normansell, R.; Sayer, B.; Waterson, S.; Dennett, E.J.; Del Forno, M.; Dunleavy, A. Antibiotics for exacerbations of asthma. Cochrane Database Syst. Rev. 2018, 6, Cd002741. [Google Scholar] [CrossRef]
- Papaioannou, A.I.; Kostikas, K.; Zervas, E.; Kolilekas, L.; Papiris, S.; Gaga, M. Control of asthma in real life: Still a valuable goal? Eur. Respir. Rev. 2015, 24, 361–369. [Google Scholar] [CrossRef]
- Papiris, S.; Kotanidou, A.; Malagari, K.; Roussos, C. Clinical review: Severe asthma. Crit. Care 2002, 6, 30–44. [Google Scholar] [CrossRef]
- Caruso, C.; Colantuono, S.; Urbani, S.; Heffler, E.; Canonica, G.W.; Andriollo, G.; Di Michele, L.; Scarlata, S.; Zennaro, D.; Rigon, A.; et al. Real-life survey on severe asthma patients during COVID-19 lockdown in Italy. Expert Rev. Respir. Med. 2021, 15, 1057–1060. [Google Scholar] [CrossRef]
- Heffler, E.; Detoraki, A.; Contoli, M.; Papi, A.; Paoletti, G.; Malipiero, G.; Brussino, L.; Crimi, C.; Morrone, D.; Padovani, M.; et al. COVID-19 in Severe Asthma Network in Italy (SANI) patients: Clinical features, impact of comorbidities and treatments. Allergy 2021, 76, 887–892. [Google Scholar] [CrossRef]
- Calmes, D.; Graff, S.; Maes, N.; Frix, A.N.; Thys, M.; Bonhomme, O.; Berg, J.; Debruche, M.; Gester, F.; Henket, M.; et al. Asthma and COPD Are Not Risk Factors for ICU Stay and Death in Case of SARS-CoV2 Infection. J. Allergy Clin. Immunol. Pract. 2021, 9, 160–169. [Google Scholar] [CrossRef]
- Toungoussova, O.; Foschino Barbaro, M.P.; Esposito, L.M.; Carpagnano, G.E.; Salerno, F.G.; Dal Negro, R.W.; Spanevello, A. Brittle asthma. Monaldi Arch. Chest Dis. 2007, 67, 102–105. [Google Scholar] [CrossRef]
- Skevaki, C.; Karsonova, A.; Karaulov, A.; Fomina, D.; Xie, M.; Chinthrajah, S.; Nadeau, K.C.; Renz, H. SARS-CoV-2 infection and COVID-19 in asthmatics: A complex relationship. Nat. Rev. Immunol. 2021, 21, 202–203. [Google Scholar] [CrossRef]
- Li, X.; Xu, S.; Yu, M.; Wang, K.; Tao, Y.; Zhou, Y.; Shi, J.; Zhou, M.; Wu, B.; Yang, Z.; et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020, 146, 110–118. [Google Scholar] [CrossRef]
- Lu, X.; Chen, T.; Wang, Y.; Wang, J.; Yan, F. Adjuvant corticosteroid therapy for critically ill patients with COVID-19. Crit. Care 2020, 24, 241. [Google Scholar] [CrossRef]
- Lei, Z.; Luo, Q.; Yang, W.; Su, Q.; Zuo, Y. Meta-analysis of competitive antagonists in asthma treatment. Ann. Palliat. Med. 2021, 10, 3235–3246. [Google Scholar] [CrossRef]
- Rogliani, P.; Ritondo, B.L.; Calzetta, L. Triple therapy in uncontrolled asthma: A network meta-analysis of phase III studies. Eur. Respir. J. 2021, 58, 2004233. [Google Scholar] [CrossRef]
- Eggert, L.E.; He, Z.; Collins, W.; Lee, A.S.; Dhondalay, G.; Jiang, S.Y.; Fitzpatrick, J.; Snow, T.T.; Pinsky, B.A.; Artandi, M.; et al. Asthma phenotypes, associated comorbidities, and long-term symptoms in COVID-19. Allergy 2022, 77, 173–185. [Google Scholar] [CrossRef]
- Pérez de Llano, L.; Dacal Rivas, D.; Blanco Cid, N.; Martin Robles, I. Phenotype-Guided Asthma Therapy: An Alternative Approach to Guidelines. J. Asthma Allergy 2021, 14, 207–217. [Google Scholar] [CrossRef]
- Pena, M.E.; Kazan, V.M.; Helmreich, M.N.; Mace, S.E. Care of Respiratory Conditions in an Observation Unit. Emerg. Med. Clin. N. Am. 2017, 35, 625–645. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.; Jit, M.; Warren-Gash, C.; Guthrie, B.; Wang, H.H.X.; Mercer, S.W.; Sanderson, C.; McKee, M.; Troeger, C.; Ong, K.L.; et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: A modelling study. Lancet Glob. Health 2020, 8, e1003–e1017. [Google Scholar] [CrossRef]
- Schatz, M.; Rachelefsky, G.; Krishnan, J.A. Follow-up after acute asthma episodes: What improves future outcomes? J. Emerg. Med. 2009, 37 (Suppl. 2), S42–S50. [Google Scholar] [CrossRef]
- Munoz-Cano, R.; Torrego, A.; Bartra, J.; Sanchez-Lopez, J.; Palomino, R.; Picado, C.; Valero, A. Follow-up of patients with uncontrolled asthma: Clinical features of asthma patients according to the level of control achieved (the COAS study). Eur. Respir. J. 2017, 49, 1501885. [Google Scholar] [CrossRef]
- Bajowala, S.; Shih, J.; Varshney, P.; Elliott, T. The Future of Telehealth for Allergic Disease. J. Allergy Clin. Immunol. Pract. 2022. [Google Scholar] [CrossRef]
- Lin, C.H.; Cerrone, D.A. Shifts in Asthma Evaluation and Management During COVID-19. Curr. Treat. Options Allergy 2022, 9, 42–51. [Google Scholar] [CrossRef]
- Kannan, S.; Shaik Syed Ali, P.; Sheeza, A.; Hemalatha, K. COVID-19 (Novel Coronavirus 2019)—Recent trends. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 2006–2011. [Google Scholar] [CrossRef]
- Bousquet, J.; Jutel, M.; Akdis, C.A.; Klimek, L.; Pfaar, O.; Nadeau, K.C.; Eiwegger, T.; Bedbrook, A.; Ansotegui, I.J.; Anto, J.M.; et al. ARIA-EAACI statement on asthma and COVID-19 (June 2, 2020). Allergy 2021, 76, 689–697. [Google Scholar] [CrossRef]
- Assaf, S.M.; Tarasevych, S.P.; Diamant, Z.; Hanania, N.A. Asthma and severe acute respiratory syndrome coronavirus 2019: Current evidence and knowledge gaps. Curr. Opin. Pulm. Med. 2021, 27, 45–53. [Google Scholar] [CrossRef]
- Adir, Y.; Saliba, W.; Beurnier, A.; Humbert, M. Asthma and COVID-19: An update. Eur. Respir. Rev. 2021, 30, 210152. [Google Scholar] [CrossRef]
- Ong, K.Y.; Tan, T.L.; Chan, A.K.W.; Tan, K.L.L.; Koh, M.S. Managing asthma in the COVID-19 pandemic and current recommendations from professional bodies: A review. J. Asthma 2021, 58, 1536–1543. [Google Scholar] [CrossRef]
- Taillé, C.; Chenivesse, C.; Devouassoux, G.; Bourdin, A.; Garcia, G. Management of asthma during the Coronavirus disease 2019 outbreak. Respir. Med. Res. 2020, 78, 100762. [Google Scholar] [CrossRef]
- British Toracic Society. Advice for Healthcare Professionals Treating People with Asthma (Adults) in Relation to COVID-19. 2020. Available online: https://www.brit-thoracic.org.uk/document-library/quality-improvement/covid-19/bts-advice-for-healthcare-professionals-treating-patients-with-asthma/ (accessed on 18 July 2022).
- GINA Scientific Committee. Global Strategy for Asthma Management and Prevention Updated 2022. 2022. Available online: https://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-Report-2022-FINAL-22-07-01-WMS.pdf (accessed on 18 July 2022).
- National Asthma Council Australia. Australian Asthma Handbook—Managing Asthma during the COVID-19 (SARS-CoV-2) Pandemic 2020. 2021. Available online: https://www.asthmahandbook.org.au/clinical-issues/covid-19 (accessed on 18 July 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).