Evaluation of Body Posture during Class II Functional Treatment with Fränkel II: A Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Orthodontic Treatment
2.3. Posturostabilometric Evaluation
2.4. Data Collection
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar]
- Bozkaya, E.; Kaygısız, E.; Tortop, T.; Güray, Y.; Yüksel, S. Mandibular posterior space in class II division 1 and 2 malocclusion in various age groups. J. Orofac. Orthop. 2020, 81, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Stahl, F.; Baccetti, T.; Franchi, L.; McNamara, J.A. Longitudinal growth changes in untreated subjects with Class II Division 1 malocclusion. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 125–137. [Google Scholar] [CrossRef] [PubMed]
- El-Bokle, D.; Abbas, N.H. A novel method for the treatment of Class II malocclusion. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 599–611. [Google Scholar] [CrossRef] [PubMed]
- D’Antò, V.; Bucci, R.; Franchi, L.; Rongo, R.; Michelotti, A.; Martina, R. Class II functional orthopaedic treatment: A systematic review of systematic reviews. J. Oral Rehabil. 2015, 42, 624–642. [Google Scholar] [PubMed]
- DiBiase, A.T.; Cobourne, M.T.; Lee, R.T. The use of functional appliances in contemporary orthodontic practice. Br. Dent. J. 2015, 218, 123–128. [Google Scholar] [CrossRef]
- Moro, A.; Mattos, C.F.P.; Borges, S.W.; Flores-Mir, C.; Topolski, F. Stability of Class II corrections with removable and fixed functional appliances: A literature review. J. World Fed. Orthod. 2020, 9, 56–67. [Google Scholar]
- Fränkel, R. A functional approach to orofacial orthopaedics. Br. J. Orthod. 1980, 7, 41–51. [Google Scholar] [CrossRef]
- McNamara, J.A.; Bookstein, F.L.; Shaughnessy, T.G. Skeletal and dental changes following functional regulator therapy on class II patients. Am. J. Orthod. 1985, 88, 91–110. [Google Scholar] [CrossRef]
- Freeman, D.C.; McNamara, J.A., Jr.; Baccetti, T.; Franchi, L.; Fränkel, C. Long-term treatment effects of the FR-2 appliance of Fränkel. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 570.e1–570.e6. [Google Scholar] [CrossRef]
- Nobili, A.; Adversi, R. Relationship between posture and occlusion: A clinical and experimental investigation. Cranio J. Craniomandib. Pract. 1996, 14, 274–285. [Google Scholar] [CrossRef] [PubMed]
- D’Attilio, M.; Caputi, S.; Epifania, E.; Festa, F.; Tecco, S. Evaluation of cervical posture of children in skeletal class I, II, and III. Cranio J. Craniomandib. Pract. 2005, 23, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Farronato, G.; Salini, V.; Di Meo, S.; Filippi, M.R.; Festa, F.; D’Attilio, M. Evaluation of cervical spine posture after functional therapy with FR-2: A longitudinal study. Cranio 2005, 23, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Michelotti, A.; Buonocore, G.; Manzo, P.; Pellegrino, G.; Farella, M. Dental occlusion and posture: An overview. Prog. Orthod. 2011, 12, 53–58. [Google Scholar] [CrossRef] [PubMed]
- D’Attilio, M.; Migliore, F.; Moscagiuri, F.; Caroccia, F. Pain Assessment during Gnathological Treatment of Temporomandibular Myofascial Pain through Mandibular Repositioning Splints Designed after a Posture-Stabilometric Evaluation. Appl. Sci. 2021, 11, 8303. [Google Scholar] [CrossRef]
- Bondi, D.; Jandova, T.; Verratti, V.; D’Amico, M.; Kinel, E.; D’Attilio, M.; Di Filippo, E.S.; Fulle, S.; Pietrangelo, T. Static balance adaptations after neuromuscular electrical stimulation on quadriceps and lumbar paraspinal muscles in healthy elderly. Sport Sci. Health 2021, 18, 85–96. [Google Scholar] [CrossRef]
- Sample Size Calculator. Available online: https://clincalc.com/stats/samplesize.aspx (accessed on 3 January 2017).
- Baccetti, T.; Franchi, L.; McNamara, J.A. The Cervical Vertebral Maturation (CVM) Method for the Assessment of Optimal Treatment Timing in Dentofacial Orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar]
- Pasciuti, E.; Franchi, L.; Baccetti, T.; Milani, S.; Farronato, G. Comparison of three methods to assess individual skeletal maturity. J. Orofac. Orthop. 2013, 74, 397–408. [Google Scholar] [CrossRef]
- Stefanelli, G. Sistema Stomatognatico nel Contesto Posturale, 1st ed.; Edi.Ermes: Milano, Italy, 2003. [Google Scholar]
- Perren, S.M.; Schneider, E. Biomechanics: Current Interdisciplinary Research, 1st ed.; Springer: Dordrecht, The Netherlands, 1985. [Google Scholar]
- Marfurt, C.F.; Rajchert, D.M. Trigeminal primary afferent projections to “non-trigeminal” areas of the rat central nervous system. J. Comp. Neurol. 1991, 303, 489–511. [Google Scholar] [CrossRef]
- Marfurt, C.F. The central projections of trigeminal primary afferent neurons in the cat as determined by the tranganglionic transport of horseradish peroxidase. J. Comp. Neurol. 1981, 203, 785–798. [Google Scholar] [CrossRef]
- Gonzalez, H.E.; Manns, A. Forward head posture: Its structural and functional influence on the stomatognathic system, a conceptual study. Cranio J. Craniomandib. Pract. 1996, 14, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Lippold, C.; Danesh, G.; Hoppe, G.; Drerup, B.; Hackenberg, L. Sagittal spinal posture in relation to craniofacial morphology. Angle Orthod. 2006, 76, 625–631. [Google Scholar] [PubMed]
- Archer, S.Y.; Vig, P.S. Effects of head position on intraoral pressures in Class I and Class II adults. Am. J. Orthod. 1985, 87, 311–318. [Google Scholar] [CrossRef]
- Perinetti, G. Dental occlusion and body posture: No detectable correlation. Gait Posture 2006, 24, 165–168. [Google Scholar] [CrossRef]
- Michelotti, A.; Manzo, P.; Farella, M.; Martina, R. Occlusion and posture: Is there evidence of correlation. Minerva Stomatol. 1999, 48, 525–534. [Google Scholar]

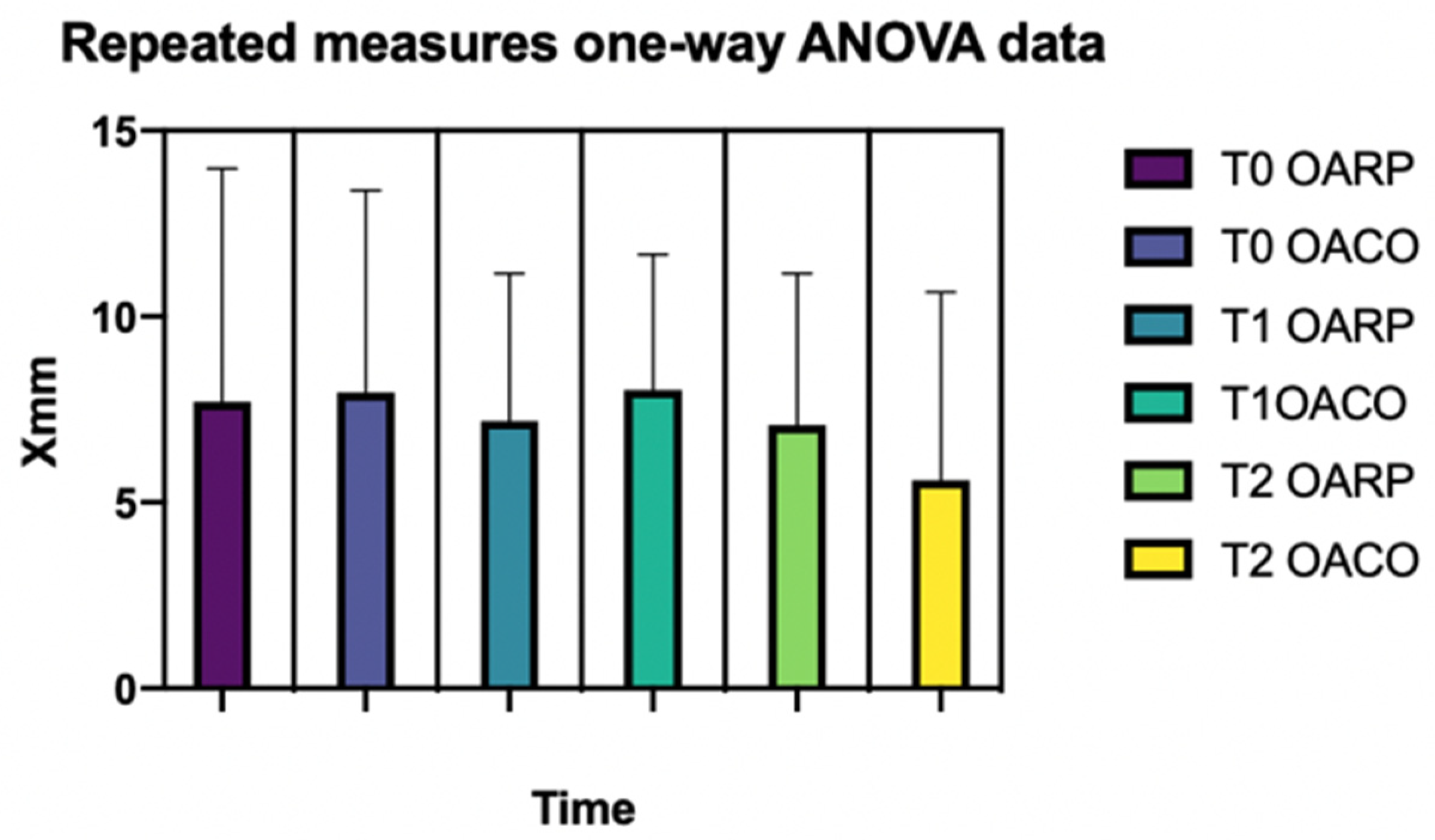
| TIME | RP | CO | p-Value | ||
|---|---|---|---|---|---|
| MEAN | DEV. ST. | MEAN | ST. DEV. | ||
| T0 | 7.7 7.2 7.1 | 6.3 | 7.9 8.0 5.6 | 5.4 | |
| T1 | 4.0 | 3.6 | |||
| T2 | 4.0 | 5.1 | |||
| 0.2741 | |||||
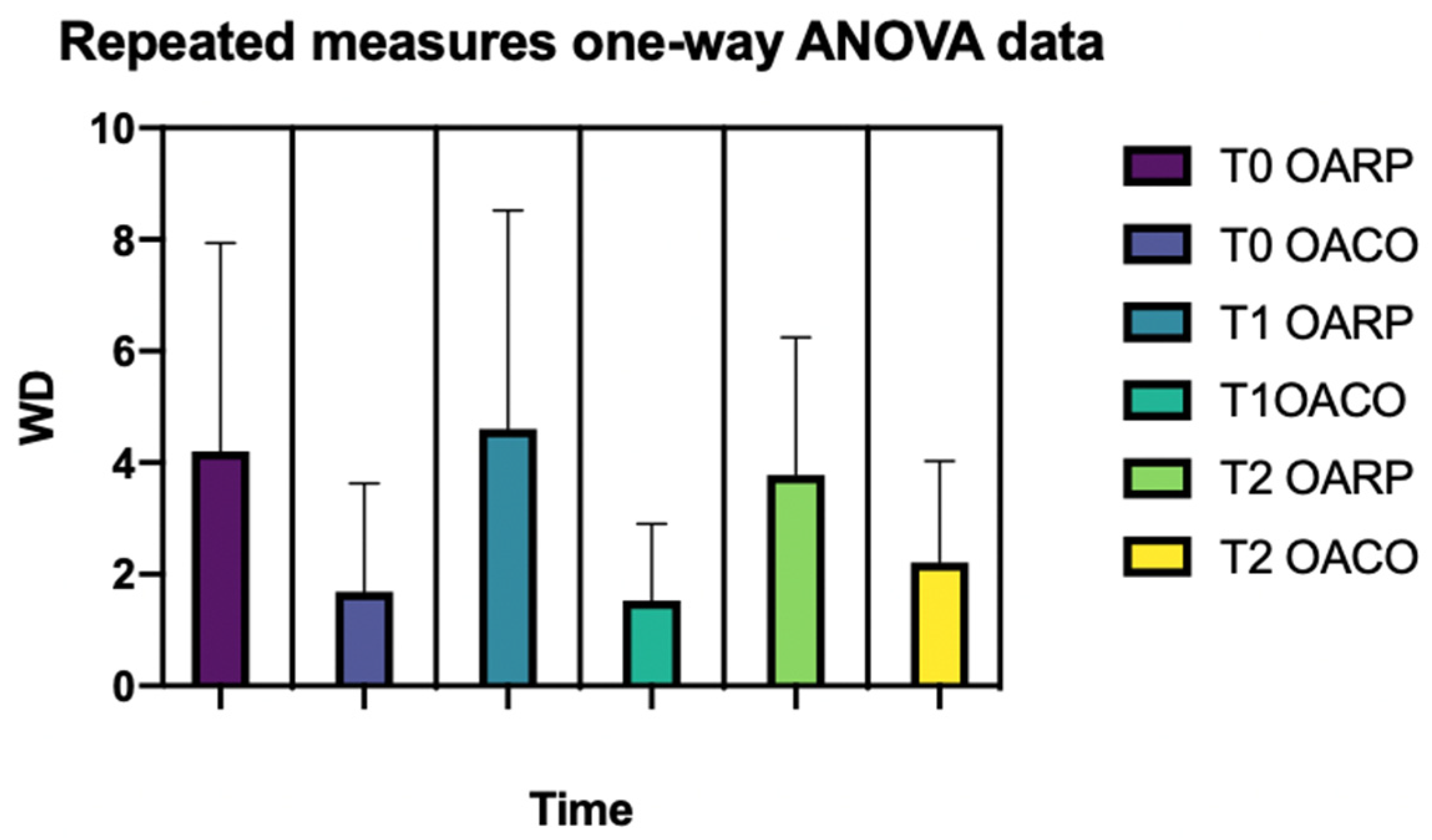
| TIME | RP | CO | p-Value | ||
|---|---|---|---|---|---|
| MEAN | DEV.ST. | MEAN | ST. DEV. | ||
| T0 | 4.2 4.6 3.7 | 3.7 | 1.7 1.5 2.2 | 1.9 | |
| T1 | 3.9 | 1.4 | |||
| T2 | 2.5 | 1.8 | |||
| 0.0154 | |||||
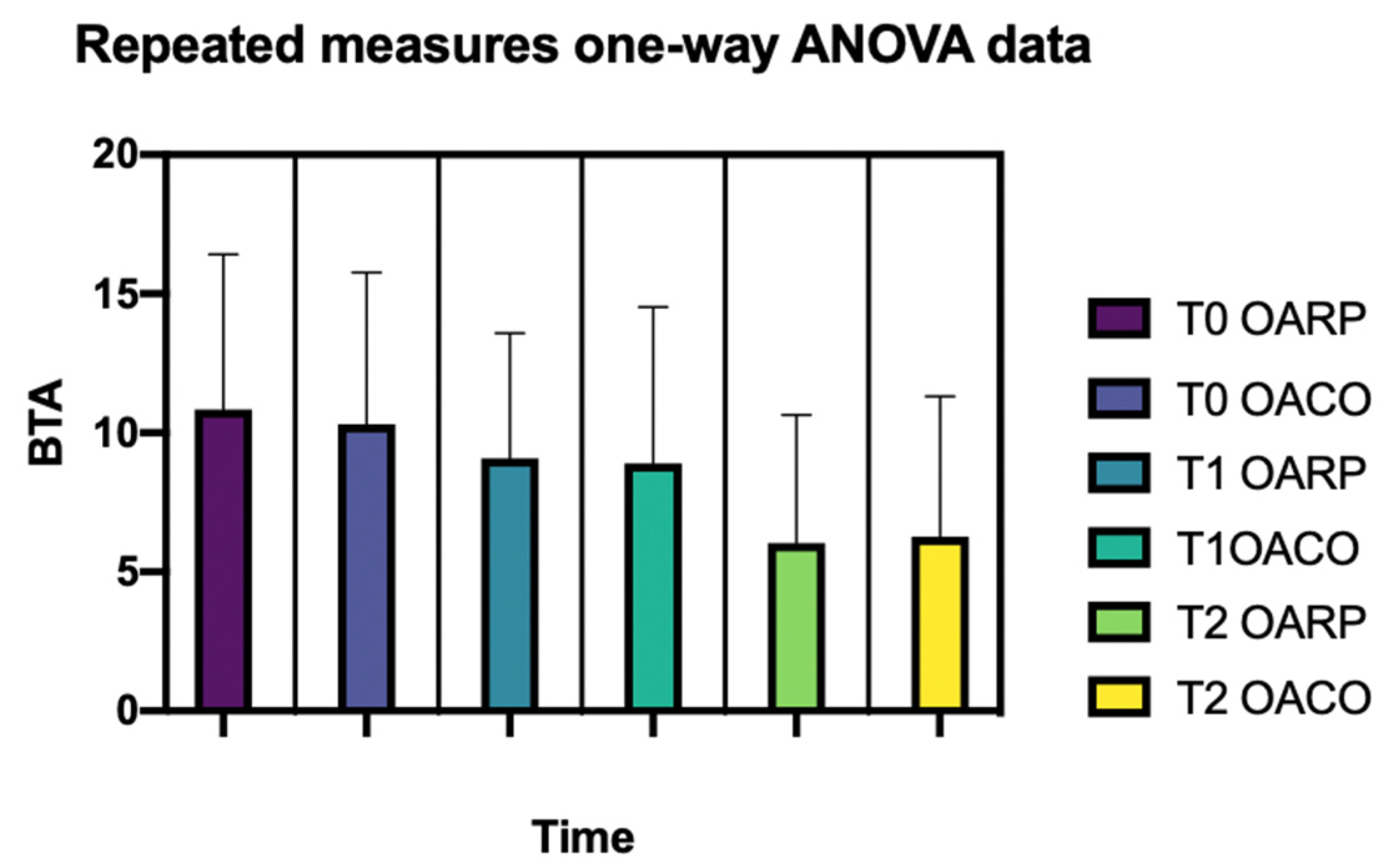
| TIME | RP | CO | p-Value | ||
|---|---|---|---|---|---|
| MEAN | DEV. ST. | MEAN | DEV. ST. | ||
| T0 | 10.85 9.1 6.04 | 5.6 | 10.3 8.9 6.3 | 5.5 | |
| T1 | 4.5 | 5.6 | |||
| T2 | 7.2 | 6.2 | |||
| 0.0003 | |||||
| Multiple Comparisons Test | Mean Differences | p-Value |
|---|---|---|
| T0 RP vs. T0 CO | 0.53 | 0.7687 |
| T0 RP vs. T1 RP | 1.77 | 0.4964 |
| T0 RP vs. T1 CO | 1.94 | 0.5482 |
| T0 RP vs. T2 RP | 4.81 | 0.0195 |
| T0 RP vs. T2 CO | 4.57 | 0.0071 |
| T0 CO vs. T1 RP | 1.23 | 0.6921 |
| T0 CO vs. T1 CO | 1.40 | 0.7913 |
| T0 CO vs. T2 RP | 4.27 | 0.0330 |
| T0 CO vs. T2 CO | 4.04 | 0.0085 |
| T1 RP vs. T1 CO | 0.17 | 0.9998 |
| T1 RP vs. T2 RP | 3.04 | 0.0444 |
| T1 RP vs. T2 CO | 2.80 | 0.0204 |
| T1 CO vs. T2 RP | 2.87 | 0.0521 |
| T1 CO vs. T2 CO | 2.63 | 0.0570 |
| T2 RP vs. T2 CO | −0.23 | 0.9989 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caroccia, F.; Lopes, C.; Pipitone, R.; D’Addazio, G.; Moscagiuri, F.; D’Attilio, M. Evaluation of Body Posture during Class II Functional Treatment with Fränkel II: A Longitudinal Study. Appl. Sci. 2022, 12, 8900. https://doi.org/10.3390/app12178900
Caroccia F, Lopes C, Pipitone R, D’Addazio G, Moscagiuri F, D’Attilio M. Evaluation of Body Posture during Class II Functional Treatment with Fränkel II: A Longitudinal Study. Applied Sciences. 2022; 12(17):8900. https://doi.org/10.3390/app12178900
Chicago/Turabian StyleCaroccia, Francesco, Chiara Lopes, Rossana Pipitone, Gianmaria D’Addazio, Francesco Moscagiuri, and Michele D’Attilio. 2022. "Evaluation of Body Posture during Class II Functional Treatment with Fränkel II: A Longitudinal Study" Applied Sciences 12, no. 17: 8900. https://doi.org/10.3390/app12178900
APA StyleCaroccia, F., Lopes, C., Pipitone, R., D’Addazio, G., Moscagiuri, F., & D’Attilio, M. (2022). Evaluation of Body Posture during Class II Functional Treatment with Fränkel II: A Longitudinal Study. Applied Sciences, 12(17), 8900. https://doi.org/10.3390/app12178900









