Abstract
Background: Lower molar distalization is considered to be one of the most difficult movements to obtain with clear aligners. The aim of this study was to evaluate the possibility to distalize the lower molars using clear aligners in adults without miniscrews. Material and methods: rx cephalograms of 16 patients (8 males, 8 females; mean age of 25.6 years), who underwent lower molar distalization, were analyzed. Cephalograms were taken before the beginning of treatment (T0) and after the end of treatment (T1). Dental and skeletal changes between T0 and T1 were evaluated. The level of significance was set at p < 0.05. Results: At T1, the lower second molar moved distally 2.47 mm, but there was a significant tipping (p = 0.027); the same result was found at the first molar, with a mean distal movement of 1.16 mm and a significant tipping (p = 0.003). No significant changes were detected on the sagittal and vertical skeletal variables. Conclusion: Clear aligner therapy can provide more distal tipping than bodily movement in the lower molars when a distalization is programmed. This movement could be sufficient to correct the initial malocclusion and gain a class I molar relationship.
1. Introduction
Class III malocclusion could be considered one of the most challenging maxillofacial disorders an orthodontist has to deal with, regardless of the age of the patient [1,2].
The characteristics of Class III malocclusion have been widely documented and include: skeletal components with underdeveloped maxilla, overdeveloped mandible or a combination of them; dentoalveolar components with Class III molar relationship, negative anterior overjet or dental compensation (naturally proclined upper incisors and retroclined lower incisors to achieve normal overjet and function) [3,4]. Correct diagnosis of the components is mandatory in order to provide an appropriate treatment plan.
The prevalence of Class III malocclusion ranges between 0.7% and 19% among the world population, with a mean prevalence of 5.92% among Caucasians and higher values in some Asian regions [5,6].
The multifactorial etiology comprises genetical factors [7], that are not modifiable, and environmental factors such as bad habits (finger suction), swallow and breath disfunction, head or neck traumas; environmental factors alone cannot be responsible for the onset of the malocclusion, but they can play a role during the growth period if genetical tendency is present [8,9,10].
Based on the patient’s skeletal development stage, scientific literature suggests different approaches.
The ideal timing of treatment is during the early mixed dentition age and the aim is to provide a more favorable environment for normal growth and to improve the occlusal relationship [11,12]. The most validated approaches in growing patients are represented by orthopedic therapy using rapid palatal expander, followed by face mask, and functional therapy [13]. The closer the growth peak, the greater the dental effects rather than skeletal ones; consequently, the risk of having side effects, such as periodontal problems and dental compensation without correction of the skeletal malocclusion, increases [14].
When an adult patient presents a Class III malocclusion that is treatable without surgery, the aim of the therapy is to correct the dental relationship, reaching molar and canine Class I, through lower molar and premolar distalization, and normalizing the anterior overjet.
Lower molar distalization is a complex movement to obtain due to the high bone density and molar radicular morphology [15]. Widespread methods are represented by open coil springs on fixed appliances, inter arch elastics and lip bumper device [16,17]. The main undesirable effect during lower molar distalization is anchorage loss in the anterior region, with lower incisor proclination that is disadvantageous to obtain the correction of the overjet [18,19]. The introduction of temporary anchorage devices (TADs) improved the distalization mechanics reducing dental side effects, but mini screws present some disadvantages such as surgical invasiveness for the insertion procedure and high infection risk with consequent mini screw loss. Moreover, an increasing number of adult patients request a more comfortable and less visible treatment; clear aligner treatment (CAT) have been introduced to answer to this request and their efficacy is well demonstrated [20,21].
Efficacy of clear aligner in distalizing upper molars has been shown and they can distalize upper molars even more than 2.7 mm; the use of buccal attachments on involved and anchorage teeth is mandatory to obtain the desired movement [22,23,24].
There are few studies in the literature that analyze lower molar distalization with CAT. It is reasonable that the same principles of upper distalization could be applied on lower distalization, with same feature and same anchorage strategies. The aim of this study is to assess the efficacy of Invisalign system in distalizing lower molars, without any auxiliary and evaluating the quantity of tipping and bodily movement.
2. Materials and Methods
2.1. Subjects
A sample of 21 Caucasian subjects treated in Dental School, University of Turin (Italy) and in orthodontic private practice with Invisalign system were retrospectively recruited between November 2018 and October 2021.
All the patients needed lower molar distalization and the met the following inclusion criteria: (1) adult age (confirmed by CVM method [25]); (2) Full Class III molar relationship at the beginning of the treatment (T0); (3) ≥ 1.5 mm distalization movement programmed on the first Clincheck; (4) standardized treatment protocol; (5) absence of lower wisdom teeth; (6) good compliance; (7) good quality pre-treatment and post-treatment latero-lateral radiographs.
Exclusion criteria were the following: (1) use of orthodontic auxiliaries to obtain the lower distalization or control the loss of anterior anchorage; (2) endodontic and/or prosthodontic therapy on lower molars; (3) periodontal disease; (4) signs or symptoms of Temporomandibular Disorders (TMDs) [26]; (5) bone metabolic disease.
To avoid selection bias, all the patients were included in the study regardless of the final results.
From the initial sample, 5 subjects were excluded according to the defined criteria: endodontic treatment on lower molars (1), prosthesis on lower molars (1), poor radiography quality (2), use of TADs (1). The final sample consisted of 16 adult patients (8 males, 8 females; mean age: 25.6 ± 4.5 years).
This study was performed in accordance with the Declaration of Helsinki; a signed informed consent was obtained from all patients before collecting the data, and researchers provided to protect the privacy.
Thirty-two cephalograms in habitual occlusion were considered for the study. Radiographs were collected at the beginning (T0) and at the end (T1) of the Invisalign therapy.
All the patients were treated using Invisalign System® by three board-certified orthodontists in Dental School—University of Turin (Italy) and orthodontic private practice.
The standardized orthodontic protocol was represented by sequential lower molar and premolar distalization similar to the upper molar distalization one. The ClinCheck® (AlignTech, Santa Monica, CA, USA) is a software developed by Align Technology in order to provide the doctor a virtual 3-D simulation of the planned orthodontic treatment based on the patient’s beginning situation and the doctor’s pre-described treatment plan. Every treatment was planned with a 50% sequential distalization in order to obtain the movement of maximum two distalizing teeth at a time; the distalization starts with the lower second molar, and once the second molar is half of the way, then the lower first molar starts its movement, then premolars, and so on [27]. Third molars, if they were present, were extracted before CAT started, as near as possible to the starting time.
No attachment was needed during the distalization movement on the involved teeth, while a buccal rectangular attachment is positioned on them at the end of their movement; the aim was exclusively to support the movement of the other teeth.
The protocol comprised also intermaxillary Class III elastics [28] (1/4” in. 4.5 oz, ORMCO Corp, Glendora, CA, USA) to counteract the proclination of lower incisors during the entire distalization phase. This protocol was adapted from the existing upper molar distalization protocol for Class II treatment.
All the patients were asked to wear aligners and class III elastics at least 22 h per day as recommended by Align Technology with regular 4-week checks in office.
2.2. Cephalometric Analysis
Thirty-two cephalograms were collected, two for each patient, one pre-treatment (T0) and one post-treatment (T1). Different X-ray devices were used, and for this reason, lateral cephalograms for each patient at T0 and T1 were standardized to life size using the ruler present in each X-ray examination.
Cephalometric analysis was performed on each radiograph using a dedicated software (Dolphin Imaging versione 11.95, Verona, Italy) by two operators blinded about the study (ER, SP). Customized digitization including 56 cephalometric landmarks and 21 variables (6 skeletal and 15 dental), chosen from different cephalometric analyses [29], was set.
As shown in Figure 1, the following parameters were used to measure changes in position of lower incisors and molars: distances between (1) the incisal margin of L1 and the line Co-Go (Condilion-Gonion), (2) mesial apex point of the incisor and Co-Go, (3) mesial crown point of L6 and Co-Go, (4) central occlusal point of L6 and Co-Go, (5) mesial apex point of L6 and Co-Go, (6) mesial crown point of L7 and Co-Go, (7) central occlusal point of L7 and Co-Go, (8) mesial apex point of L7 and Co-Go.
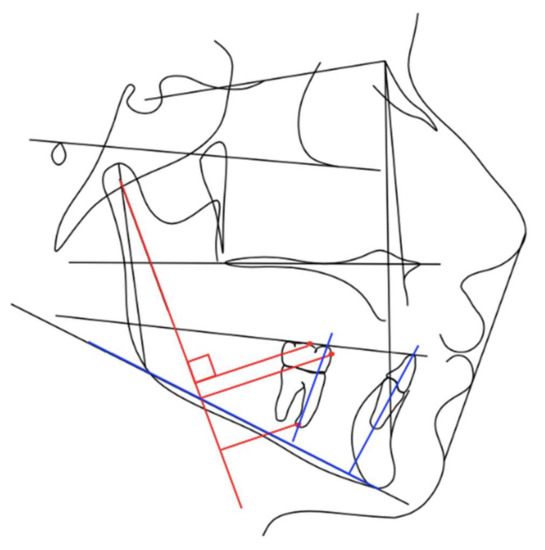
Figure 1.
Cephalometric analysis performed.
The following parameters were used to measure changes in angulation of lower incisors and molars: angles between (1) L1 long axis and the line Go-Me (Gonion-Menton), (2) L6 long axis and Go-Me, (3) L7 long axis and Go-Me.
2.3. Statistical Analysis
Normality assumption of the data was evaluated with the Shapiro–Wilk test; homoscedasticity and autocorrelation of the variables were assessed using the Breusch–Pagan and Durbin–Watson tests.
For each variable studied, a multiple regression model was performed to estimate the differences during follow-up (post vs. pre), adjusting for age and gender, with 95% IC.
Descriptive values were shown considering the main indicators of distribution and variability. The level of significance was set at p < 0.05.
The sample size calculation is based on the parameter α = 0.05. Subjects were enrolled for the study in order to detect 80% of statistical power. The study was able to detect an MD (mean difference) ≥|1.02| during follow-up, which can be considered an efficient cut-off for the included variables in this specific context.
Statistical analyses were conducted using the R statistical package (version 3.5.3, R Core Team, Foundation for Statistical Computing, Vienna, Austria).
3. Results
All the patients achieved a Class I molar relationship at the end of treatment and the mean duration of CAT treatment was 19.7 ± 2.6 months.
Mean, standard deviation and 95% IC values of the change in dental and skeletal variables are reported in Table 1.

Table 1.
Cephalometric values analyzed.
No significant changes in sagittal skeletal variables SNA (p = 0.827), SNB (p = 0.853) and ANB (p = 0.996) are reported.
Vertical skeletal variables reported a slight but non-significant increase (SN-MP = 0.14°, p = 0.946; PP-MP = 0.81°, p = 0.744).
No significant variation was reported for overjet and overbite, even if clinically there was an improvement with mean increases of +1.27 mm (p = 0.127) and +0.23 (p = 0.744).
Significant changes were revealed by first and second lower molars tipping; lower first molar showed a mean decrease of −4.56° (p = 0.032; 95% IC = −8.55, −0.57) with respect to Co-Go line and of −5.03 (p = 0.003; 95% IC = −8.15, −1.91) with respect to Go-Me line; lower second molar showed significant changes only for the mesio-distal inclination with respect to the Go-Me line, with a mean decrease of −4.47 (p = 0.027; 95% IC = −8.24, −0.69). The global position of lower molars, measured considering the distance from Co-Go line and occlusal and root references, did not show any significant changes.
The inclination of the lower incisor to Go-Me line changed significantly (MD = −4.78°; p = 0.037; 95% IC = −9.09, −0.47), while its sagittal position did not change (distance between incisal point and Co-Go line).
4. Discussion
The aim of the study was to assess the lower molar distalization using clear aligners and evaluate the possibility of gaining tipping or bodily movement.
Results suggests that the sequential distalization protocol for lower molars determines mainly a tipping movement rather than a true distal translation.
All the cases presented good occlusion at the end of the treatment, with Class I molar and canine relationship, adequate anterior overjet and overbite and no signs or symptoms of TMD were revealed during or after the therapy. One of the key factors in class III cases, is the control of interincisal angle. The planning was set with the aim of a final stable incisal angle of approximately 131°. Reaching this angulation, it is possible to correct anterior relationship, starting from an edge-to-edge bite or anterior crossbite to a normal overjet relationship.
Currently, in the scientific literature analysis of this type of treatment is lacking, there are just few case reports. The predictability of maxillary molar distalization using aligners is high (88%) and well demonstrated by Simon et al. [30]. The paper published by Ravera et al. [31] confirmed these results. Therefore, aligners seem to be effective in preventing distal tipping and extrusion when an upper molar distalization is programmed.
According to the results of the study, no distal bodily movement was always achieved, so it is reasonable to think that uprighting is enough to correct the dental relationship. This statement is confirmed by the results that, although not statistically significant, showed a distal movement of the second molar, with a mean decrease of 2.47 mm of the distance between the central point on the occlusal surface of the second molar and CoGo line, and the first molar, with a mean decrease of 1.16 mm of the distance between the central point on the occlusal surface and CoGo line; both these changes are clinically evident. As a matter of fact, in an adult patient, the correction of the dental relationship through molar distalization requires about 2 mm of space distally. In order to gain it, it is necessary to create space, which is why it is considered useful to extract the third molars before starting the treatment, if they were present. Furthermore, as the patients enrolled in the study are adults, an increase in mandibular size is not expected during treatment due to the normal growth process and this represents a favorable data for correction.
A potential side effect of molar uprighting is the formation of premature contacts at the level of the mesial cusps caused by the relative extrusion of molars indeed. The patient’s vertical skeletal pattern is an important factor to consider when planning molar distalization as it can vary unfavorably, especially in hyperdivergent patients in whom an increase in vertical dimension during treatment is not desirable [32]. A clockwise rotation of the mandible caused by dental precontacts that appeared during the distalization movement can in fact worsen the profile and cause anterior open bite. The statistical non-significance of the variations associated with the SN-MP and PP-MP parameters demonstrates the possibility of maintaining control of verticality in the patient during orthodontic therapy and this could be determined by the thickness of the aligners and the consequent bite-block effect [29].
Regarding the skeletal variables considered, no statistically significant changes were detected not only in the vertical plane, but also in the sagittal plane. All patients included in the study had a CS5 vertebral maturation phase (according to the CVM classification) at the start of treatment; therefore, skeletal growth could be considered complete and further changes in terms of mandibular development were not likely [11].
Significant data that emerged from this study is the variation of lower incisors inclination towards lingual direction. In the dental correction of a malocclusion, it is essential to consider the need for anchorage since, as demonstrated by Kim [18], every intraoral force applied in the distal direction produces an equal and opposite reaction in the opposite region, i.e., a loss of anterior anchorage, and this applies to both the arches; the same effect was documented by Fontana et al. [19]. Specifically, a force applied to the molars is reflected on the incisors as a loss of anchorage and therefore as a tendency to proclination. The side dental effects of molar distalization with traditional fixed orthodontic devices and with the aid of TADs are well documented in the literature [33,34]. Aligner deflection during the distalization phase produces the same type of effect [22]. The significance of the variation in terms of endo-inclination of the lower incisor, however, suggests that the Invisalign system allows for better control over the torque of the anterior elements, intended as a side effect of molar distalization and this is in agreement with data in the literature. However, it is advisable to use interarch elastics with class III vector during the entire distalization phase, exactly as in the upper molar distalization protocol [29]. Although the results of this study already provide useful information on the effectiveness of lower molar distalization with aligners, this topic deserves to be further explored with clinical trials and a larger sample size. Among the biases that can negatively influence the results of the study, we must remember the selection biases linked to the retrospectivity of the study itself. Conducting a retrospective study on an uncommon orthodontic procedure such as this also presents difficulties, and for this reason, the participation of private orthodontic activity was requested and the retrospective design of the study seemed the most suitable one. Other limitations of the study are represented by the difficulty of evaluating the dental effects caused by the class III elastics and by the lack of monitoring of patient collaboration. Class III elastics, considered necessary to prevent the loss of anterior anchorage, were used in all patients throughout the lower molar distalization phase, but some continued to wear these elastics in later stages to reduce the risk of proclination of the lower incisors; therefore, the results relating to changes in position and inclination of the lower incisors may have been influenced.
The evaluation of compliance was instead evaluated by simply asking patients to fill in a diary in which to write the number of hours the aligners were worn.
The possibility of applying optimized attachments (or not) could represent an interesting variable to analyze since, as demonstrated by Rossini et al. [31,35], the presence of one or more attachments on the teeth in the active phase of movement and on the anchoring teeth could allow better control of the distalization movement, thus reducing tipping.
The use CAT in class III patients can be considered a valid therapeutic option in cases where it is necessary to perform uprighting or to correct minor class III dental discrepancies that involve the displacement of the lower posterior elements in the distal direction in order to achieve Class I molar relationship; even the simple uprighting of the molars allows for the recovery of mesial space, thus allowing the backward movement of the middle and anterior elements of the lower arch and reducing the need for interproximal reduction of the enamel (IPR) anteriorly in case of crowding.
5. Conclusions
This study suggests that the Invisalign System could be effective in moving distally lower molars but gaining mainly a tipping movement rather than bodily movement.
The use of interarch elastics with class III vector seems to be advisable in order to reduce the loss of anterior anchorage, caused by the deformation of the aligner in the phases in which it pushes the molars distally.
However, these results must be considered influenced by the small sample size and the limitations of a retrospective study.
Author Contributions
Conceptualization, T.C. and A.D.; methodology, T.C.; validation, A.D., T.C. and S.P.; formal analysis, E.R.; investigation, K.M. and G.M.; resources, G.C.; data curation, G.C.; writing—original draft preparation, S.P. and E.R.; writing—review and editing, A.D., G.M. and T.C.; supervision, A.D., T.C. and K.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chang, H.P.; Tseng, Y.C.; Chang, H.F. Treatment of mandibular prognathism. J. Formos. Med. Assoc. 2006, 105, 781–790. [Google Scholar] [CrossRef] [Green Version]
- Kakali, L.; Christopoulou, I.; Tsolakis, I.A.; Sabaziotis, D.; Alexiou, A.; Sanoudos, M.; Tsolakis, A.I. Mid-term follow up effectiveness of facemark treatment in class III malocclusion: A systematic review. Int. Orthod. 2021, 19, 365–376. [Google Scholar] [CrossRef]
- Chang, H.P. Components of Class III malocclusion in Taiwanese. Kaohsiung J. Med. Sci. 1985, 1, 144–155. [Google Scholar]
- Jacobson, A.; Evans, W.G.; Preston, C.B. Mandibular prognathism. Am. J. Orthod. 1974, 66, 140–171. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dental Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef]
- Staudt, C.B.; Kiliaridis, S. Different skeletal types underlying Class III malocclusion in a random population. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Dehesa-Santos, A.; Iber-Diaz, P.; Iglesias-Linares, A. Genetic factors contributing to skeletal Class III malocclusion: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 1587–1612. [Google Scholar] [CrossRef]
- Due, F.; Wong, R.; Rabie, A. Genes, genetics and Class III malocclusion. Orthod. Craniofacial Res. 2010, 13, 69–74. [Google Scholar]
- Linder-Aronson, S. Naso-respiratory function and craniofacial growth. Monograph 1979, 9, 121–147. [Google Scholar]
- Scott, J.H. Studies on the growth of the upper jaw. Dent. Rec. 1948, 68, 277–291. [Google Scholar]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. Growth in the untreated Class III subjects. Semin. Orthod. 2007, 13, 130–142. [Google Scholar] [CrossRef]
- Reyes, B.C.; Baccetti, T.; McNamara, J.A., Jr. An estimate of craniofacial growth in Class III malocclusion. Angle Orthod. 2006, 76, 577–584. [Google Scholar]
- Rongo, R.; D’Antò, V.; Bucci, R.; Polito, I.; Martina, R.; Michelotti, A. Skeletal and dental effects of Class III orthopedic treatment: A systematic review and meta-analysis. J. Oral Rehabil. 2017, 44, 545–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westwood, P.V.; McNamara, J.A., Jr.; Baccetti, T.; Franchi, L.; Sarver, D.M. Long-term effects of Class III treatment with rapid maxillary expansion and facemark therapy followed by fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 306–320. [Google Scholar] [CrossRef] [Green Version]
- Iglesias-Linares, A.; Morford, L.A.; Hartsfield, J.K., Jr. Bone density and dental external apical root resorption. Curr. Osteoporos. Rep. 2016, 14, 292–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalaf, K.; Mustafa, A.; Wazzan, M.; Omar, M.; Estaitia, M.; El-Kishawi, M. Clinical effectiveness of space maintainers and space regainers in the mixed dentition: A systematic review. Saudi Dent. J. 2022, 4, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, J.; Daimaruya, T.; Umemori, M.; Nagasaka, H.; Takahashi, I.; Kawamura, H.; Mitani, H. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am. J. Orthodo. Dentofac. Orthop. 2004, 125, 130–138. [Google Scholar] [CrossRef]
- Kim, Y.H.; Han, U.K.; Lim, D.D.; Serraon, M.L.P. Stability of anterior open bite correction with multi loop edgewise arch wire therapy: A cephalometric follow-up study. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 43–54. [Google Scholar] [CrossRef] [Green Version]
- Fontana, M.; Cozzani, M.; Caprioglio, A. Non-compliance maxillary molar distalizing appliances: An overview of the last decade. Prog. Orthod. 2012, 13, 173–184. [Google Scholar] [CrossRef]
- Meier, B.; Wiemer, K.B.; Miethke, R.R. Invisalign: Patient profiling—Analysis of a prospective study. J. Orofac. Orthop. 2003, 64, 352–358. [Google Scholar] [CrossRef]
- Garino, F.; Castroflorio, T.; Daher, S. Effectiveness of composite attachments in controlling upper- molar movement with aligners. J. Clin. Orthod. 2016, 50, 341–347. [Google Scholar] [PubMed]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Forces and moments generated by removable thermoplastic aligners: Incisor torque, premolar derotation, and molar distalization. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 728–736. [Google Scholar] [CrossRef]
- Bowman, S.J.; Celenza, F.; Sparaga, J.; Papadopoulos, M.A.; Ojima, K.; Lin, J.C. Creative adjuncts for clear aligners, part 1: Class II treatment. J. Clin. Orthod. 2015, 49, 83–94. [Google Scholar] [PubMed]
- Fuziy, A.; Rodrigues de Almeida, R.; Janson, G.; Angeileri, F.; Pinzan, A. Sagittal, vertical and transverse changes consequent to maxillary molar distalization with the Pendulum appliance. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; McNamara, J.A., Jr. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin. Orthod. 2005, 11, 119–129. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Daher, S. Dr. Sam Daher’s Techniques for Class II Correction with Invisalign and Elastics; Align Technology: Santa Clara, CA, USA, 2011. [Google Scholar]
- McNamara, J.A., Jr. A method of cephalometric evaluation. Am. J. Orthod. 1984, 86, 449–469. [Google Scholar] [CrossRef]
- Giancotti, A.; Farina, A. Treatment of collapsed arches using the Invisalign system. J. Clin. Orthod. 2010, 44, 416–425. [Google Scholar]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment outcome and efficacy of an aligner technique: Regarding incisor torque, premolar derotation and molar distalization. BMC Oral Health 2014, 11, 68. [Google Scholar] [CrossRef] [Green Version]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary molar distalization with aligners in adult patients: A multi-center retrospective study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [CrossRef] [Green Version]
- Grippaudo, C.; Oliva, B.; Greco, A.L.; Sferra, S.; Deli, R. Relationship between vertical facial patterns and dental arch form in class II malocclusion. Prog. Orthod. 2013, 14, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poletti, L.; Aimara, A.A.; Huanca, L. Dentoalveolar class III treatment using retromolar ministre anchorage. Prog. Orthod. 2013, 14, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kook, Y.A.; Park, J.H.; Bayome, M.; Kim, S.; Han, E.; Kim, C.H. Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 364–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).