Three-Dimensional Distance Mapping Method to Evaluate Mandibular Symmetry and Morphology of Adults with Unilateral Premolar Scissors Bite
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
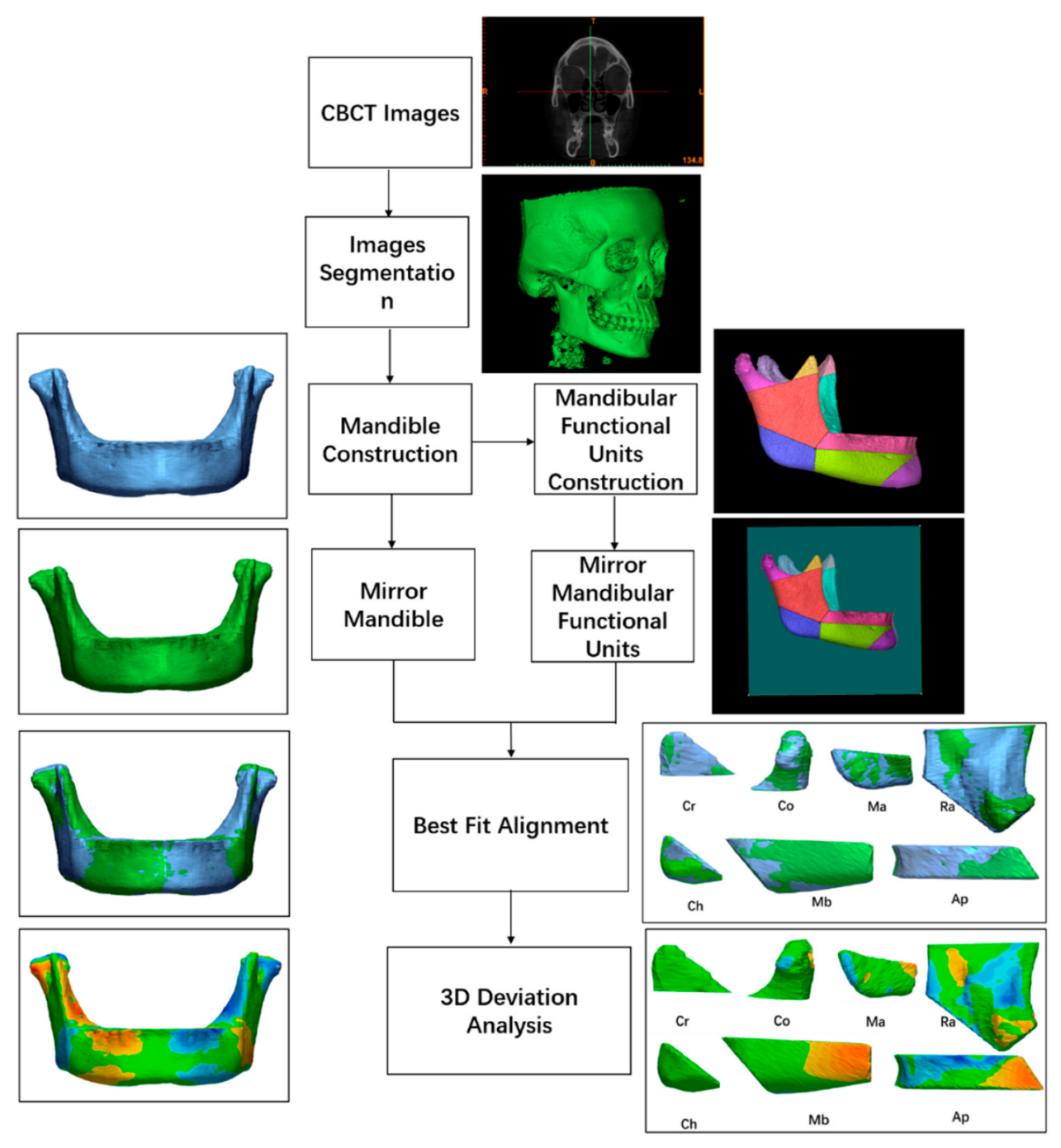
2.2. Workflow
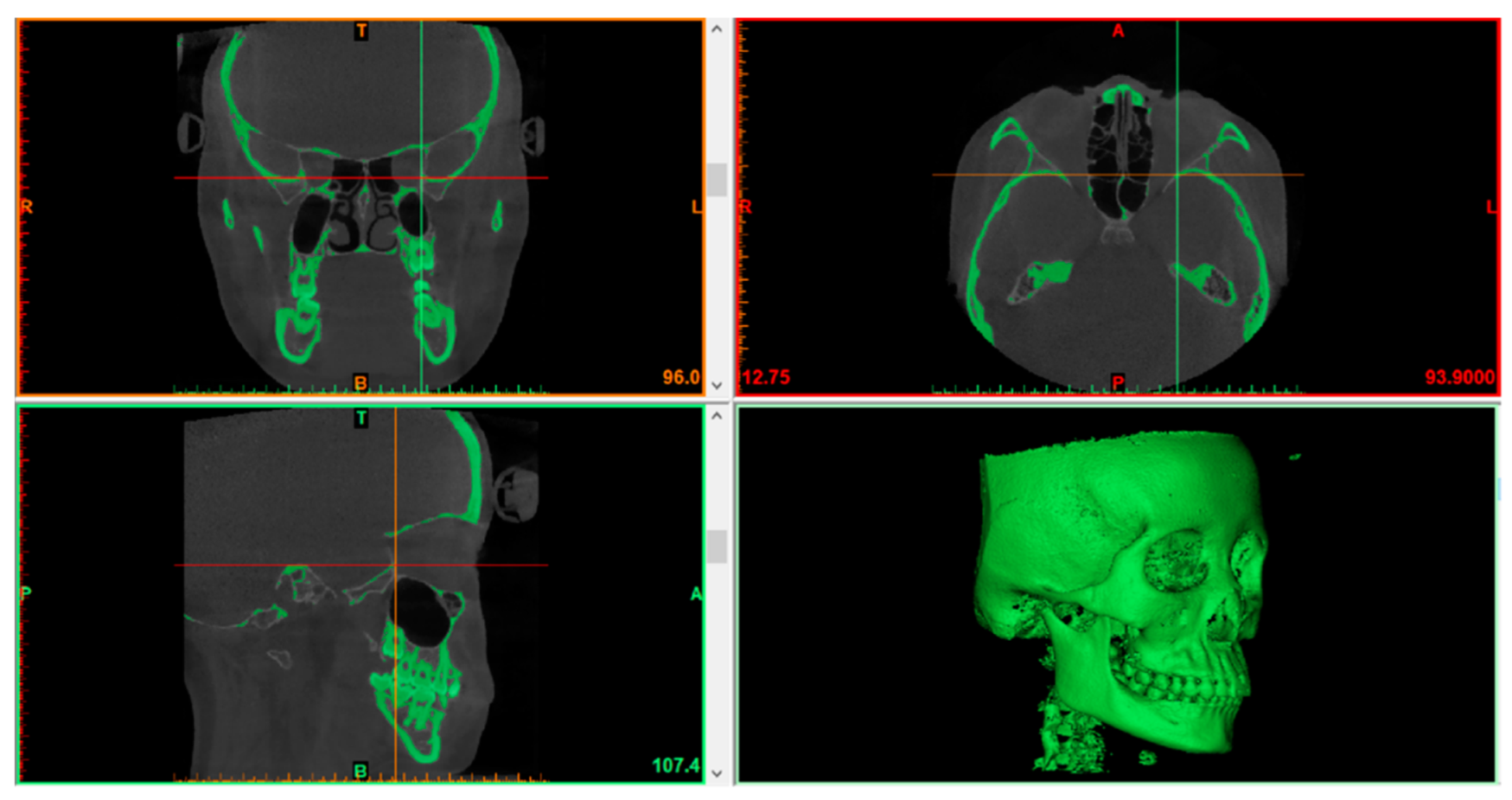
2.2.1. Segmenting Images
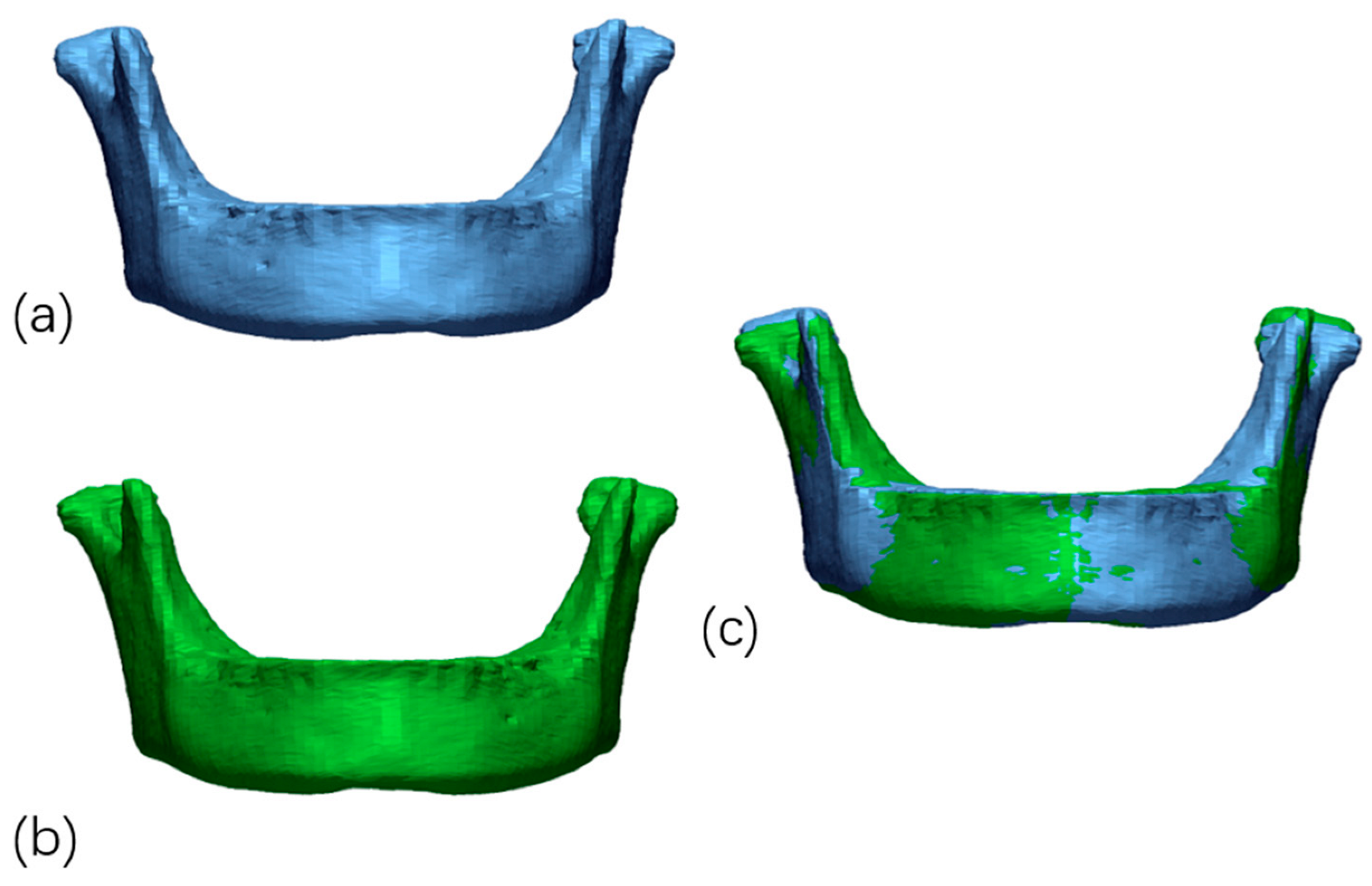
2.2.2. 3D Models Rendering and Mirroring
2.2.3. Automatic Best-Fit Alignment of Mandibles
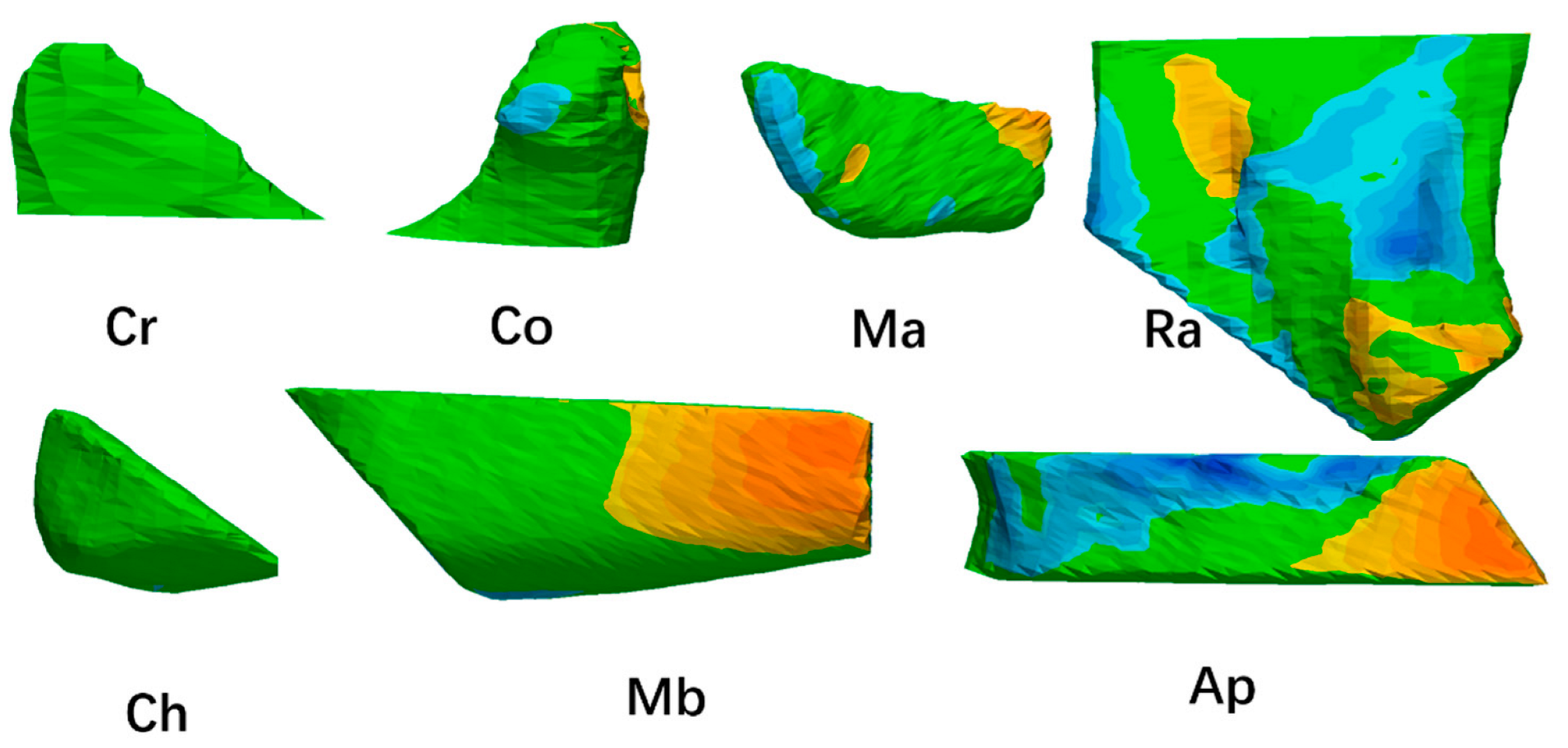
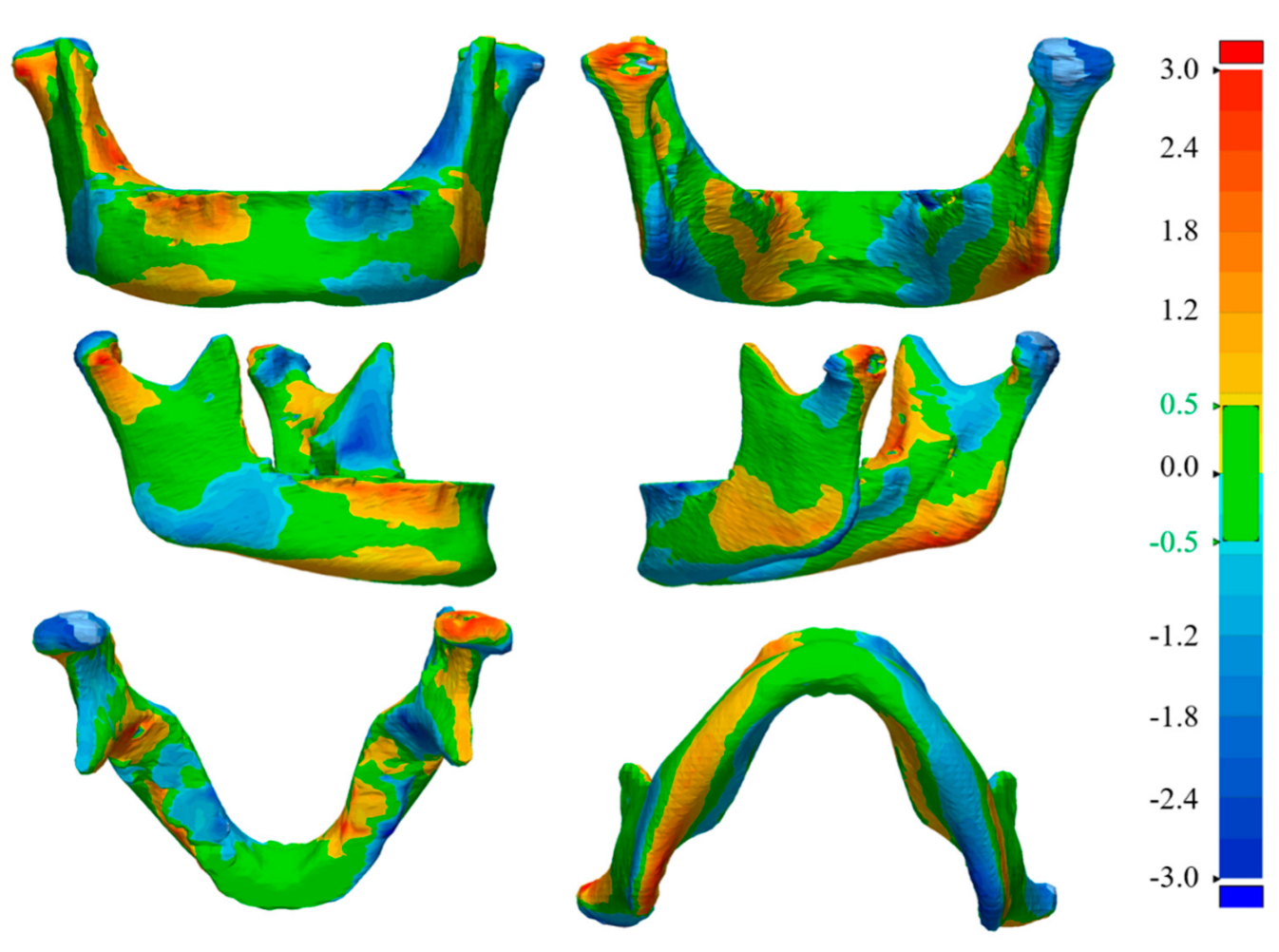
2.2.4. Mandible Distance Mapping
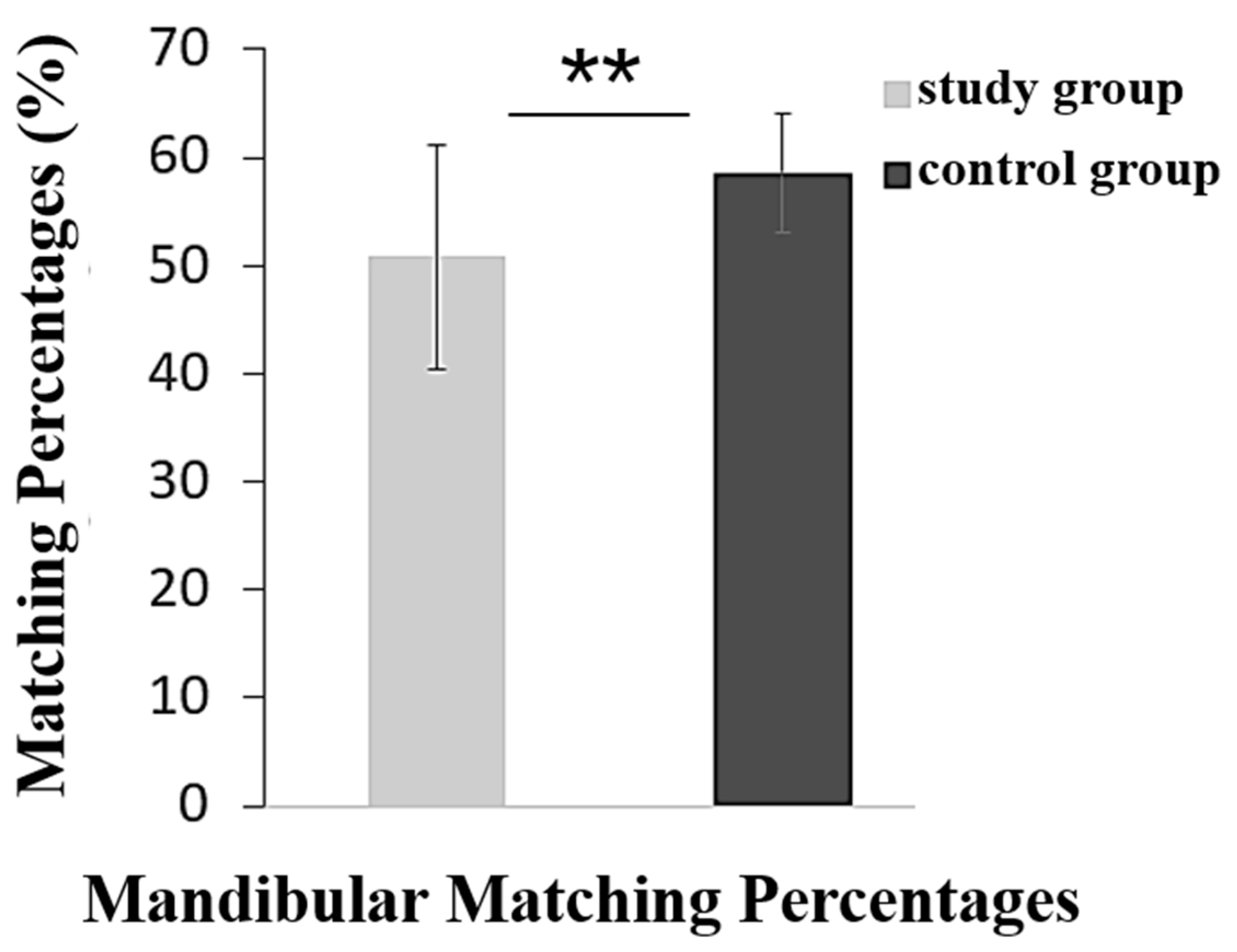
2.2.5. Matching Percentage Calculation of Mandibles
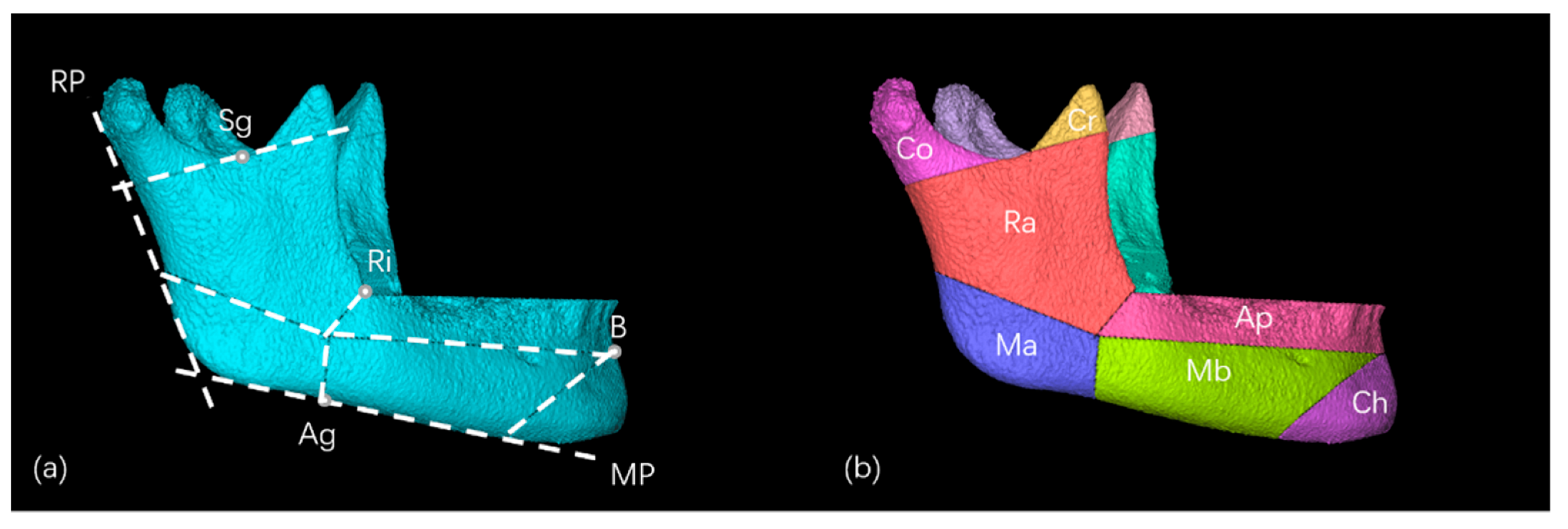
2.2.6. Construction of Mandibular Units
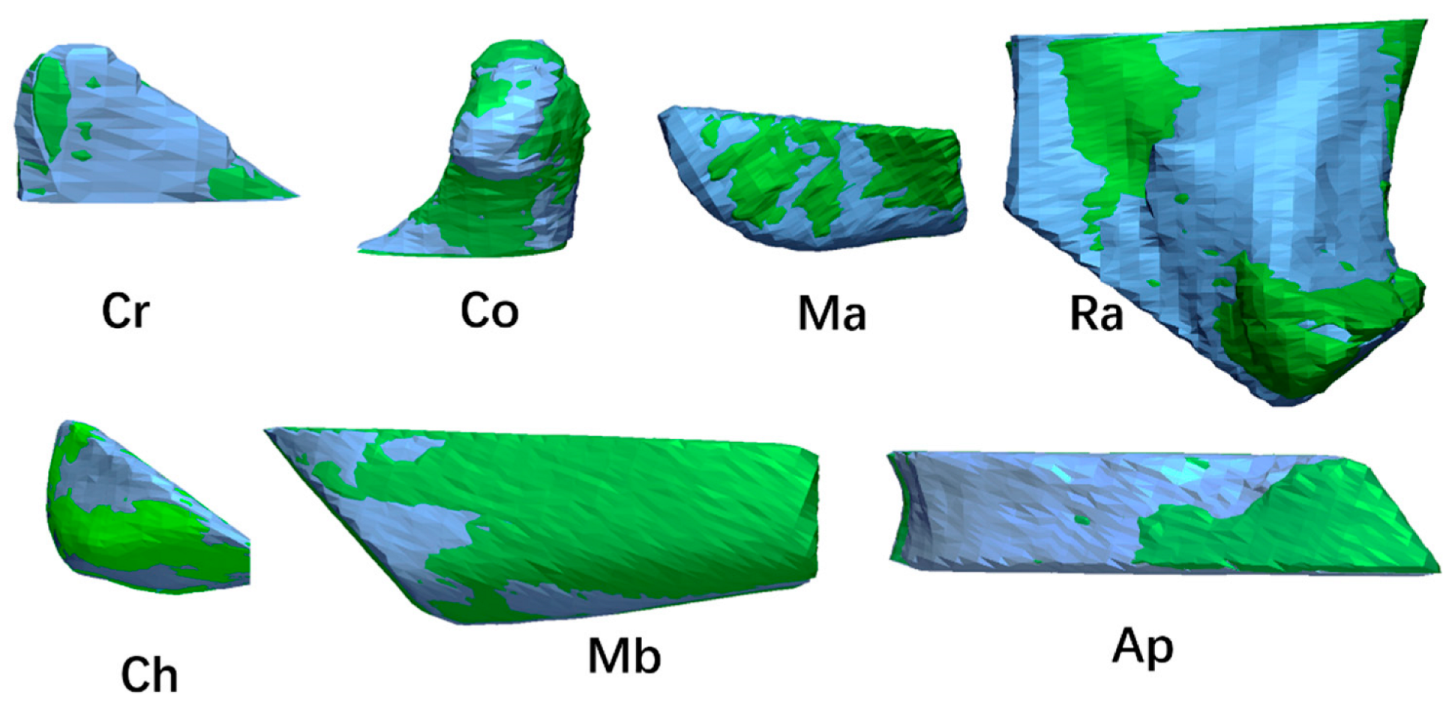
2.2.7. Automatic Best-Fit Alignment and Deviation Analysis of Mandibular Units
2.2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tomonari, H.; Kubota, T.; Yagi, T.; Kuninori, T.; Kitashima, F.; Uehara, S.; Miyawaki, S. Posterior scissors-bite: Masticatory jaw movement and muscle activity. J. Oral Rehabil. 2014, 41, 257–265. [Google Scholar] [CrossRef]
- Doshi, U.H.; Chandorikar, H.; Nagrik, A.; Bhad, W.A.; Chavan, S.J. Early correction of unilateral scissor bite using transforce appliance and modified twin block appliance. J. Orthod. Sci. 2017, 6, 76–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baik, U.-B.; Kim, Y.; Sugawara, J.; Hong, C.; Park, J.H. Correcting severe scissor bite in an adult. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 113–124. [Google Scholar] [CrossRef]
- Lee, S.-A.; Chang, C.C.; Roberts, W.E. Severe unilateral scissors-bite with a constricted mandibular arch: Bite turbos and extra-alveolar bone screws in the infrazygomatic crests and mandibular buccal shelf. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 554–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Türp, J.C.; Schindler, H. The dental occlusion as a suspected cause for TMDs: Epidemiological and etiological considerations. J. Oral Rehabil. 2012, 39, 502–512. [Google Scholar] [CrossRef]
- Favero, V.; Sbricoli, L.; Favero, L. Scissor bite in a young patient treated with an orthodontic-orthopedic device. A case report. Eur. J. Paediatr. Dent. 2013, 141, 153–155. [Google Scholar]
- Li, J.; Lu, S.-J.; Shi, Y.-J.; Lu, P.; Tian, Y.-L. Effect of premolars scissor bite on the sagittal position of mandible. Shanghai Kou Qiang Yi Xue 2019, 28, 179–183. [Google Scholar]
- Gil Choi, I.G.; Cortes, A.R.G.; Arita, E.S.; Georgetti, M.A.P. Comparison of conventional imaging techniques and CBCT for periodontal evaluation: A systematic review. Imaging Sci. Dent. 2018, 48, 79–86. [Google Scholar] [CrossRef]
- Kakumoto, T.; Barsoum, A.; Froum, S.J. Accuracy of Cone-Beam Computed Tomography Versus Periapical Radiography Measurements When Planning Placement of Implants in the Posterior Maxilla: A Retrospective Study. Compend. Contin. Educ. Dent. 2021, 42, e1–e4. [Google Scholar] [PubMed]
- Evangelista, K.; Valladares-Neto, J.; Silva, M.A.G.; Cevidanes, L.H.S.; Ruellas, A.C.D.O. Three-dimensional assessment of mandibular asymmetry in skeletal Class I and unilateral crossbite malocclusion in 3 different age groups. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Muraglie, S.; Leonardi, R.; Aboulazm, K.; Stumpo, C.; Loreto, C.; Grippaudo, C. Evaluation of structural skeletal asymmetry of the glenoid fossa in adult patients with unilateral posterior crossbite using surface-to-surface matching on CBCT images. Angle Orthod. 2020, 90, 376–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leonardi, R.; Muraglie, S.; Lo Giudice, A.; Aboulazm, K.S.; Nucera, R. Evaluation of mandibular symmetry and morphology in adult patients with unilateral posterior crossbite: A CBCT study using a surface-to-surface matching technique. Eur. J. Orthod. 2020, 42, 650–657. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Muraglie, S.; Bennici, O.; Cavallini, C.; Spampinato, C. Three-dimensional analysis of mandibular functional units in adult patients with unilateral posterior crossbite: A cone beam study with the use of mirroring and surface-to-surface matching techniques. Angle Orthod. 2019, 89, 590–596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lintz, F.; Jepsen, M.; Netto, C.D.C.; Bernasconi, A.; Ruiz, M.; Siegler, S. Distance mapping of the foot and ankle joints using weightbearing CT: The cavovarus configuration. Foot Ankle Surg. 2021, 27, 412–420. [Google Scholar] [CrossRef]
- Moss, M.L.; Rankow, R.M. The role of the functional matrix in mandibular growth. Angle Orthod. 1968, 38, 95–103. [Google Scholar] [CrossRef]
- Mun, S.H.; Park, M.; Lee, J.; Lim, H.J.; Kim, B.C. Volumetric characteristics of prognathic mandible revealed by skeletal unit analysis. Ann. Anat. Anat. Anz. 2019, 226, 3–9. [Google Scholar] [CrossRef]
- Liu, C.; Kaneko, S.; Soma, K. Glenoid Fossa Responses to Mandibular Lateral Shift in Growing Rats. Angle Orthod. 2007, 77, 660–667. [Google Scholar] [CrossRef]
- Fourneron, M.; Morant, F.; Boutin, F.; Frapier, L. Is the Quad Helix more efficient to correct mandibular asymmetry before age 7? A retrospective comparative study. Int. Orthod. 2020, 18, 443–450. [Google Scholar] [CrossRef]
- Ramirez-Yañez, G.O.; Stewart, A.; Franken, E.; Campos, K. Prevalence of mandibular asymmetries in growing patients. Eur. J. Orthod. 2011, 33, 236–242. [Google Scholar] [CrossRef] [Green Version]
- Wiens, J.P.; Goldstein, G.R.; Andrawis, M.; Choi, M.; Priebe, J.W. Defining centric relation. J. Prosthet. Dent. 2018, 120, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J. Oral Rehabil. 2017, 44, 908–923. [Google Scholar] [CrossRef] [PubMed]
- Lim, W.H.; Choi, B.; Lee, J.-Y.; Ahn, S.-J. Dentofacial characteristics in orthodontic patients with centric relation–maximum intercuspation discrepancy. Angle Orthod. 2014, 84, 939–945. [Google Scholar] [CrossRef]
- Qi, K.; Guo, S.-X.; Xu, Y.; Deng, Q.; Liu, L.; Li, B.; Wang, M.-Q. An investigation of the simultaneously recorded occlusal contact and surface electromyographic activity of jaw-closing muscles for patients with temporomandibular disorders and a scissors-bite relationship. J. Electromyogr. Kinesiol. 2016, 28, 114–122. [Google Scholar] [CrossRef]
- Yamada, T.; Sugiyama, G.; Mori, Y. Masticatory muscle function affects the pathological conditions of dentofacial deformities. Jpn. Dent. Sci. Rev. 2020, 56, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Sella-Tunis, T.; Pokhojaev, A.; Sarig, R.; O’Higgins, P.; May, H. Human mandibular shape is associated with masticatory muscle force. Sci. Rep. 2018, 8, 6042. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, L.; Traina, A.A.; Nakamai, L.F.; Luz, J.G.D.C. Effects of the unilateral removal and dissection of the masseter muscle on the facial growth of young rats. Braz. Oral Res. 2009, 23, 89–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chouinard, A.-F.; Kaban, L.B.; Peacock, Z.S. Acquired Abnormalities of the Temporomandibular Joint. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 83–96. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, M.; Yonemitsu, I.; Takei, M.; Kure-Hattori, I.; Ono, T. The imbalance of masticatory muscle activity affects the asymmetric growth of condylar cartilage and subchondral bone in rats. Arch. Oral Biol. 2016, 63, 22–31. [Google Scholar] [CrossRef] [Green Version]
- Kwon, T.-G.; Lee, K.-H.; Park, H.-S.; Ryoo, H.-M.; Kim, H.-J.; Lee, S.-H. Relationship Between the Masticatory Muscles and Mandibular Skeleton in Mandibular Prognathism With and Without Asymmetry. J. Oral Maxillofac. Surg. 2007, 65, 1538–1543. [Google Scholar] [CrossRef]
- Seo, S.-A.; Baik, H.-S.; Hwang, C.-J.; Yu, H.-S. Analysis of masseter muscle in facial asymmetry before and after orthognathic surgery using 3-dimensional computed tomography. Korean J. Orthod. 2009, 39, 18–27. [Google Scholar] [CrossRef] [Green Version]
- Hua, X.; Xiong, H.; Han, G.; Cheng, X. Correction of a dental arch-width asymmetric discrepancy with a slow maxillary contraction appliance. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 842–853. [Google Scholar] [CrossRef]
- Deffrennes, G.; Deffrennes, D. Management of Brodie bite: Note on surgical treatment. Int. Orthod. 2017, 15, 640–676. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, Y.; Kuroda, S.; Sugawara, Y.; Kurosaka, H.; Takano-Yamamoto, T.; Yamashiro, T. Long-term stability of implant-anchored orthodontics in an adult patient with a Class II Division 2 malocclusion and a unilateral molar scissors-bite. Am. J. Orthod. Dentofac. Orthop. 2014, 145, S100–S113. [Google Scholar] [CrossRef] [PubMed]
- Suda, N.; Tominaga, N.; Niinaka, Y.; Amagasa, T.; Moriyama, K. Orthognathic treatment for a patient with facial asymmetry associated with unilateral scissors-bite and a collapsed mandibular arch. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Lopatienė, K.; Trumpytė, K. Relationship between unilateral posterior crossbite and mandibular asymmetry during late adolescence. Stomatologija 2018, 20, 90–95. [Google Scholar]
- Habets, L.L.M.H.; Bezuur, J.N.; Naeiji, M.; Hansson, T.L. The Orthopantomogram®, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J. Oral Rehabil. 1988, 15, 465–471. [Google Scholar] [CrossRef]
- Miresmaeili, A.; Salehisaheb, H.; Farhadian, M.; Borjali, M. Mandibular asymmetry in young adult patients with unilateral posterior crossbite: A controlled retrospective CBCT study. Int. Orthod. 2021, 19, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.M.; Aboulazm, K.; Giudice, A.L.; Ronsivalle, V.; D’Antò, V.; Lagravère, M.; Isola, G. Evaluation of mandibular changes after rapid maxillary expansion: A CBCT study in youngsters with unilateral posterior crossbite using a surface-to-surface matching technique. Clin. Oral Investig. 2021, 25, 1775–1785. [Google Scholar] [CrossRef]
- Siegler, S.; Konow, T.; Belvedere, C.; Ensini, A.; Kulkarni, R.; Leardini, A. Analysis of surface-to-surface distance mapping during three-dimensional motion at the ankle and subtalar joints. J. Biomech. 2018, 76, 204–211. [Google Scholar] [CrossRef]
- Turow, A.; Bulstra, A.E.; Oldhoff, M.; Hayat, B.; Doornberg, J.; White, J.; Jaarsma, R.L.; Bain, G.I. 3D mapping of scaphoid fractures and comminution. Skelet. Radiol. 2020, 49, 1633–1647. [Google Scholar] [CrossRef]
- Hayashi, T.; Arai, Y.; Chikui, T.; Hayashi-Sakai, S.; Honda, K.; Indo, H.; Kawai, T.; Kobayashi, K.; Murakami, S.; Nagasawa, M.; et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol. 2018, 34, 89–104. [Google Scholar] [CrossRef]
- Hiles, P.; Gilligan, P.; Damilakis, J.; Briers, E.; Candela-Juan, C.; Faj, D.; Foley, S.; Frija, G.; Granata, C.; Gala, H.D.L.H.; et al. European consensus on patient contact shielding. Insights Into Imaging 2021, 12, 194. [Google Scholar] [CrossRef]
- Ludlow, J.B.; Ivanovic, M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2008, 106, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Jaju, P.P.; Jaju, S.P. Cone-beam computed tomography: Time to move from ALARA to ALADA. Imaging Sci. Dent. 2015, 45, 263–265. [Google Scholar] [CrossRef] [Green Version]
- Neagos, A.; Vrinceanu, D.; Dumitru, M.; Costache, A.; Cergan, R. Demographic, anthropometric, and metabolic characteristics of obstructive sleep apnea patients from Romania before the COVID-19 pandemic. Exp. Ther. Med. 2021, 22, 1487. [Google Scholar] [CrossRef] [PubMed]
- Ferlias, N.; Gjørup, H.; Doherty, M.A.; Haagerup, A.; Pedersen, T.K. Obstructive Sleep Apnoea in pycnodysostosis; a three-dimensional upper airway analysis. Orthod. Craniofacial Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kiaee, B.; Nucci, L.; Sarkarat, F.; Talaeipour, A.R.; Eslami, S.; Amiri, F.; Jamilian, A. Three-dimensional assessment of airway volumes in patients with unilateral cleft lip and palate. Prog. Orthod. 2021, 22, 35. [Google Scholar] [CrossRef] [PubMed]
| Mandibular Units | Study Group | Control Group | Significance |
|---|---|---|---|
| Mandibular ramus | 62.52 ± 11.00 | 68.60 ± 7.56 | ** |
| Mandibular angle | 69.16 ± 12.39 | 71.44 ± 10.07 | NS |
| Condylar process | 62.78 ± 13.56 | 67.58 ± 10.32 | * |
| Coracoid process | 87.03 ± 6.99 | 89.73 ± 7.68 | NS |
| Alveolar process | 67.00 ± 12.68 | 73.83 ± 8.88 | ** |
| Mandibular body | 66.62 ± 9.44 | 72.37 ± 8.69 | ** |
| Chin | 80.75 ± 9.86 | 85.23 ± 6.80 | ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, Y.; Lyu, X.; Liu, Y.; Zeng, R.; Liao, Y.; Tan, J. Three-Dimensional Distance Mapping Method to Evaluate Mandibular Symmetry and Morphology of Adults with Unilateral Premolar Scissors Bite. Appl. Sci. 2022, 12, 5814. https://doi.org/10.3390/app12125814
Xie Y, Lyu X, Liu Y, Zeng R, Liao Y, Tan J. Three-Dimensional Distance Mapping Method to Evaluate Mandibular Symmetry and Morphology of Adults with Unilateral Premolar Scissors Bite. Applied Sciences. 2022; 12(12):5814. https://doi.org/10.3390/app12125814
Chicago/Turabian StyleXie, Yajuan, Xinwei Lyu, Yuyao Liu, Runling Zeng, Yuwei Liao, and Jiali Tan. 2022. "Three-Dimensional Distance Mapping Method to Evaluate Mandibular Symmetry and Morphology of Adults with Unilateral Premolar Scissors Bite" Applied Sciences 12, no. 12: 5814. https://doi.org/10.3390/app12125814
APA StyleXie, Y., Lyu, X., Liu, Y., Zeng, R., Liao, Y., & Tan, J. (2022). Three-Dimensional Distance Mapping Method to Evaluate Mandibular Symmetry and Morphology of Adults with Unilateral Premolar Scissors Bite. Applied Sciences, 12(12), 5814. https://doi.org/10.3390/app12125814





