A Comparative Study to Evaluate the Effect of Honey and Zinc Oxide Eugenol Dressing for the Treatment of Dry Socket: A Double-Blind Randomized Controlled Trial
Abstract
1. Introduction
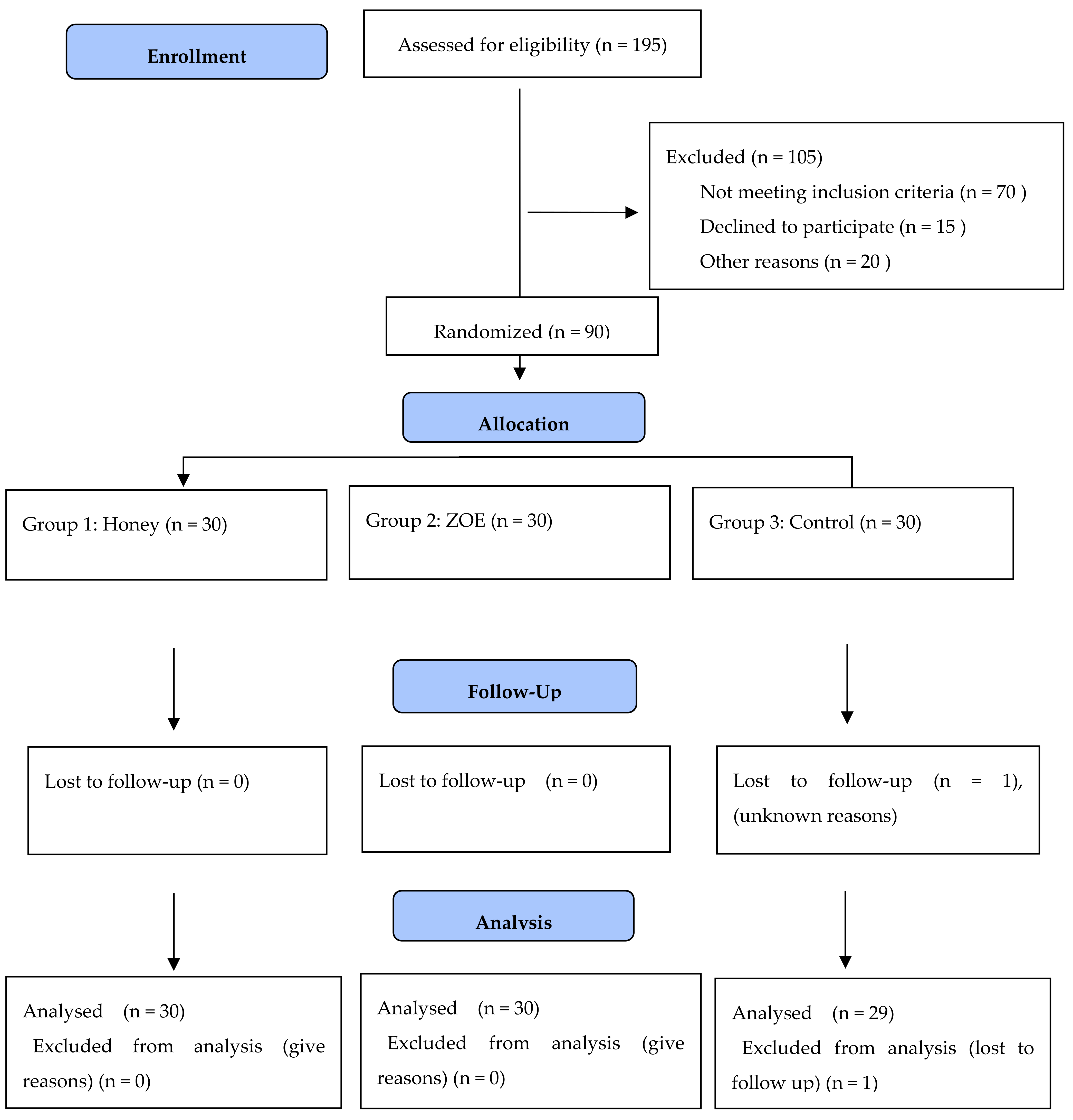
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| VAS | Visual analog scale |
| CRP | C-reactive protein |
| ZOE | Zinc oxide eugenol |
| ADPT | Antimicrobial photodynamic therapy |
| CGF | Concentrated growth factor |
| LLLT | Low-level laser therapy |
References
- Taberner-Vallverdu, M.; Sanchez-Garces, M.; Gay-Escoda, C. Efficacy of Different Methods Used for Dry Socket Prevention and Risk Factor Analysis: A Systematic Review. Med. Oral Patol. Oral y Cir. Bucal 2017, 22, e750. [Google Scholar] [CrossRef]
- Kolokythas, A.; Olech, E.; Miloro, M. Alveolar Osteitis: A Comprehensive Review of Concepts and Controversies. Int. J. Dent. 2010, 2010, 249073. [Google Scholar] [CrossRef]
- Ahmed, N.; Lal, A.; Shakeel, M.; Cyrus, D.; Zehra, F.T.; Ayub, A. Prevalence of Types, Frequency and Risk Factors for Complications after Exodontia. Pak. J. Med. Dent. 2021, 10, 44–49. [Google Scholar]
- Saghiri, M.A.; Asatourian, A.; Sheibani, N. Angiogenesis and the prevention of alveolar osteitis: A review study. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 93. [Google Scholar] [CrossRef]
- Sigron, G.R.; Pourmand, P.P.; Mache, B.; Stadlinger, B.; Locher, M.C. The most common complications after wisdom-tooth removal: Part 1: A retrospective study of 1199 cases in the mandible. Swiss Dent. J. 2014, 124, 1042–1056. [Google Scholar] [PubMed]
- Pourmand, P.P.; Sigron, G.R.; Mache, B.; Stadlinger, B.; Locher, M.C. The most common complications after wisdom-tooth removal: Part 2: A retrospective study of 1562 cases in the maxilla. Swiss Dent. J. 2014, 124, 1047–1061. [Google Scholar] [PubMed]
- Bowe, D.C.; Rogers, S.; Stassen, L.F.A. The management of dry socket/alveolar osteitis. J. Ir. Dent. Assoc. 2021, 57, 305–310. [Google Scholar]
- Blum, I.R. Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int. J. Oral Maxillofac. Surg. 2002, 31, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Nusair, Y.M.; Abu Younis, M.H. Prevalence, clinical picture, and risk factors of dry socket in a Jordanian Dental Teaching Center. J. Contemp. Dent. Pract. 2007, 8, 1–17. [Google Scholar] [CrossRef]
- De SAmaratunga, N.A.; Senaratne, C.M. A clinical study of dry socket in Sri Lanka. Br. J. Oral Maxillofac. Surg. 1988, 26, 410–418. [Google Scholar] [CrossRef]
- Nettelhoff, L.; Grimm, S.; Jacobs, C.; Walter, C.; Pabst, A.M.; Goldschmitt, J.; Wehrbein, H. Influence of mechanical compression on human periodontal ligament fibroblasts and osteoblasts. Clin. Oral Investig. 2016, 20, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Rakhshan, V. Common risk factors of dry socket (alveolitis osteitis) following dental extraction: A brief narrative review. J. Stomatol. Oral Maxillofac. Surg. 2018, 119, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Abu Younis, M.H.; Abu Hantash, R.O. Dry socket: Frequency, clinical picture, and risk factors in a palestinian dental teaching center. Open Dent. J. 2011, 5, 7–12. [Google Scholar]
- Preetha, S. An Overview of Dry Socket and Its Management. IOSR J. Dent. Med. Sci. 2014, 13, 32–35. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Hoppenreijs, T.J.; Xi, T.; Fennis, J.P.; Maal, T.J.; Bergé, S.J.; Meijer, G.J. Postoperative socket irrigation with drinking tap water reduces the risk of inflammatory complications following surgical removal of third molars: A multicenter randomized trial. Clin. Oral Investig. 2017, 21, 71–83. [Google Scholar] [CrossRef]
- Supe, N.; Choudhary, S.; Yamyar, S.; Patil, K.; Choudhary, A.; Kadam, V. Efficacy of alvogyl (Combination of Iodoform + Butylparaminobenzoate) and zinc oxide eugenol for dry socket. Ann. Maxillofac. Surg. 2018, 8, 193. [Google Scholar] [PubMed]
- Ansari, A.; Joshi, S.; Garad, A.; Mhatre, B.; Bagade, S.; Jain, R. A study to evaluate the efficacy of honey in the management of dry socket. Contemp. Clin. Dent. 2019, 10, 52. [Google Scholar] [CrossRef]
- Neel, A.; Bozec, L.; Perez, R.A.; Kim, H.-W.; Knowles, J.C. Nanotechnology in dentistry: Prevention, diagnosis, and therapy. Int. J. Nanomed. 2015, 10, 6371. [Google Scholar] [CrossRef]
- Magro Filho, O.; de Carvalho, A.C. Application of propolis to dental sockets and skin wounds. J. Nihon Univ. Sch. Dent. 1990, 32, 4–13. [Google Scholar] [CrossRef]
- Soni, N.; Singh, V.; Mohammad, S.; Singh, R.K.; Pal, U.S.; Singh, R.; Aggrwal, J.; Pal, M. Effects of honey in the management of alveolar osteitis: A study. Natl. J. Maxillofac. Surg. 2016, 7, 136. [Google Scholar]
- Torres-Lagares, D.; Infante-Cossio, P.; Gutierrez-Perez, J.L.; Romero-Ruiz, M.M.; Garcia-Calderon, M.; Serrera-Figallo, M.A. Intra-alveolar chlorhexidine gel for the prevention of dry socket in mandibular third molar surgery. A pilot study. Med. Oral Patol. Oral Cir. Bucal 2006, 11, E179–E184. [Google Scholar] [PubMed]
- Bortoluzzi, M.C.; Manfro, R.; De Déa, B.E.; Dutra, T.C. Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J. Contemp. Dent. Pract. 2010, 11, E33–E40. [Google Scholar] [CrossRef]
- Singh, V.; Pal, U.; Singh, R.; Soni, N. Honey a sweet approach to alveolar osteitis: A study. Natl. J. Maxillofac. Surg. 2014, 5, 31. [Google Scholar] [CrossRef] [PubMed]
- El-Kased, R.F.; Amer, R.I.; Attia, D.; Elmazar, M.M. Honey-based hydrogel: In vitro and comparative In vivo evaluation for burn wound healing. Sci. Rep. 2017, 7, 9692. [Google Scholar] [CrossRef]
- Al-Waili, N.S.; Salom, K.; Butler, G.; Al Ghamdi, A.A. Honey and Microbial Infections: A Review Supporting the Use of Honey for Microbial Control. J. Med. Food 2011, 14, 1079–1096. [Google Scholar] [CrossRef] [PubMed]
- Yaghoobi, R.; Kazerouni, A.; Kazerouni, O. Evidence for Clinical Use of Honey in Wound Healing as an Anti-bacterial, Anti-inflammatory Anti-oxidant and Anti-viral Agent: A Review. Jundishapur J. Nat. Pharm. Prod. 2013, 8, 100–104. [Google Scholar] [CrossRef]
- González-Serrano, J.; López-Pintor, R.; Cecilia-Murga, R.; Torres, J.; Hernández, G.; López-Quiles, J. Application of propolis extract, nanovitamin C and nanovitamin E to prevent alveolar osteitis after impacted lower third molar surgery. A randomized, double-blind, split-mouth, pilot study. Med. Oral Patol. Oral y Cir. Bucal 2021, 26, e118–e125. [Google Scholar] [CrossRef]
- Chaurasia, N.K.; Upadhyaya, C.; Dixit, S. Comparative Study to Determine the efficacy of Zinc Oxide Eugenol and Alveogyl in Treatment of Dry Socket. Kathmandu Univ. Med. J. (KUMJ) 2017, 15, 203–206. [Google Scholar]
- Faizel, S.; Thomas, S.; Yuvaraj, V.; Prabhu, S.; Tripathi, G. Comparision Between Neocone, Alvogyl and Zinc Oxide Eugenol Packing for the Treatment of Dry Socket: A Double Blind Randomised Control Trial. J. Maxillofac. Oral Surg. 2015, 14, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.; Salman, B.; Razak, N.H.A.; Samsudin, A.R. A Comparative Clinical Study between Concentrated Growth Factor and Low-Level Laser Therapy in the Management of Dry Socket. Eur. J. Dent. 2020, 14, 613–620. [Google Scholar] [CrossRef]
- Chakravarthi, S. Platelet rich fibrin in the management of established dry socket. J. Korean Assoc. Oral Maxillofac. Surg. 2017, 43, 160. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Akinbami, B.O.; Godspower, T. Dry Socket: Incidence, Clinical Features, and Predisposing Factors. Int. J. Dent. 2014, 2014, 796102. [Google Scholar] [CrossRef] [PubMed]
| Region in the Arch | Teeth | Maxilla | Mandible | ||
|---|---|---|---|---|---|
| Single Extraction | Multiple Extraction | Single Extraction | Multiple Extraction | ||
| Anterior | Incisor | NR | 8 (40%) | NR | 10 (50%) |
| Canine | 2 (10%) | NR | NR | NR | |
| Posterior | Premolar | NR | 7 (10%) | NR | 12 (17.14%) |
| Molar | 11 (15.71%) | 14 (20%) | 10 (14.28%) | 16 (22.85%) | |
| Groups | N | Mean | Standard Deviation |
|---|---|---|---|
| Group 1: Honey | 30 | 8.50 | 0.97 |
| Group 2: Zinc Oxide Eugenol | 30 | 8.90 | 0.76 |
| Group 3: Control (Normal Saline) | 29 | 8.10 | 0.80 |
| Groups | 5 min Post-op VAS Score Mean ± SD | 30 min Post-op VAS Score Mean ± SD | 60 min Post-op VAS Score Mean ± SD | 2nd day Post-op VAS Score Mean ± SD | 4th day Post-op VAS Score Mean ± SD | 7th day Post-op VAS Score Mean ± SD |
|---|---|---|---|---|---|---|
| Group 1: Honey | 4.26 ± 0.73 | 2.20 ± 0.71 | 1.16 ± 0.69 | 0.33 ± 0.48 | 0.06 ± 0.25 | 0.00 ± 0.00 |
| Group 2: Zinc Oxide Eugenol | 4.40 ± 0.81 | 1.93 ± 0.25 | 0.93 ± 0.25 | 0.00 ± 00 | 0.00 ± 00 | 0.00 ± 00 |
| Group 3: Control | 5.83 ± 0.38 | 4.60 ± 0.50 | 2.00 ± 0.00 | 1.00± 0.00 | 0.60 ± 0.50 | 0.00 ± 00 |
| Groups | Mean | Standard Deviation | Standard Error Mean | t-Value | df | p-Value |
|---|---|---|---|---|---|---|
| Group 1: Honey and Group 2: Zinc Oxide Eugenol | 0.13 | 0.57 | 0.10 | 1.23 | 29 | 0.229 |
| Group 1: Honey and Group 3: Control | −1.00 | 0.43 | 0.08 | −12.58 | 29 | 0.001 |
| Group 2: Zinc Oxide Eugenol and Group 3: Control | −1.12 | 0.22 | 0.04 | −28.41 | 29 | 0.001 |
| Gender | N | Mean | Standard Deviation | Standard Error Mean | Mean Difference | t-Value | df | p-Value |
|---|---|---|---|---|---|---|---|---|
| Male | 45 | 1.84 | 0.84 | 0.12 | −0.31 | −1.82 | 87.87 | 0.07 |
| Female | 44 | 2.15 | 0.76 | 0.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, Z.A.; Prabhu, N.; Ahmed, N.; Lal, A.; Issrani, R.; Maqsood, A.; Alam, M.K.; Alanazi, S.; Aljohani, F.M.; Almndel, M.N.; et al. A Comparative Study to Evaluate the Effect of Honey and Zinc Oxide Eugenol Dressing for the Treatment of Dry Socket: A Double-Blind Randomized Controlled Trial. Appl. Sci. 2022, 12, 6. https://doi.org/10.3390/app12010006
Khan ZA, Prabhu N, Ahmed N, Lal A, Issrani R, Maqsood A, Alam MK, Alanazi S, Aljohani FM, Almndel MN, et al. A Comparative Study to Evaluate the Effect of Honey and Zinc Oxide Eugenol Dressing for the Treatment of Dry Socket: A Double-Blind Randomized Controlled Trial. Applied Sciences. 2022; 12(1):6. https://doi.org/10.3390/app12010006
Chicago/Turabian StyleKhan, Zafar Ali, Namdeo Prabhu, Naseer Ahmed, Abhishek Lal, Rakhi Issrani, Afsheen Maqsood, Mohammad Khursheed Alam, Sarah Alanazi, Fahad Muqbil Aljohani, Msleh Naim Almndel, and et al. 2022. "A Comparative Study to Evaluate the Effect of Honey and Zinc Oxide Eugenol Dressing for the Treatment of Dry Socket: A Double-Blind Randomized Controlled Trial" Applied Sciences 12, no. 1: 6. https://doi.org/10.3390/app12010006
APA StyleKhan, Z. A., Prabhu, N., Ahmed, N., Lal, A., Issrani, R., Maqsood, A., Alam, M. K., Alanazi, S., Aljohani, F. M., Almndel, M. N., & Alolait, M. A. A. (2022). A Comparative Study to Evaluate the Effect of Honey and Zinc Oxide Eugenol Dressing for the Treatment of Dry Socket: A Double-Blind Randomized Controlled Trial. Applied Sciences, 12(1), 6. https://doi.org/10.3390/app12010006









