Treatment of Medial Collateral Ligament Injuries of the Knee with Focused Extracorporeal Shockwave Therapy: A Case Report
Abstract
:1. Introduction
2. Materials and Methods
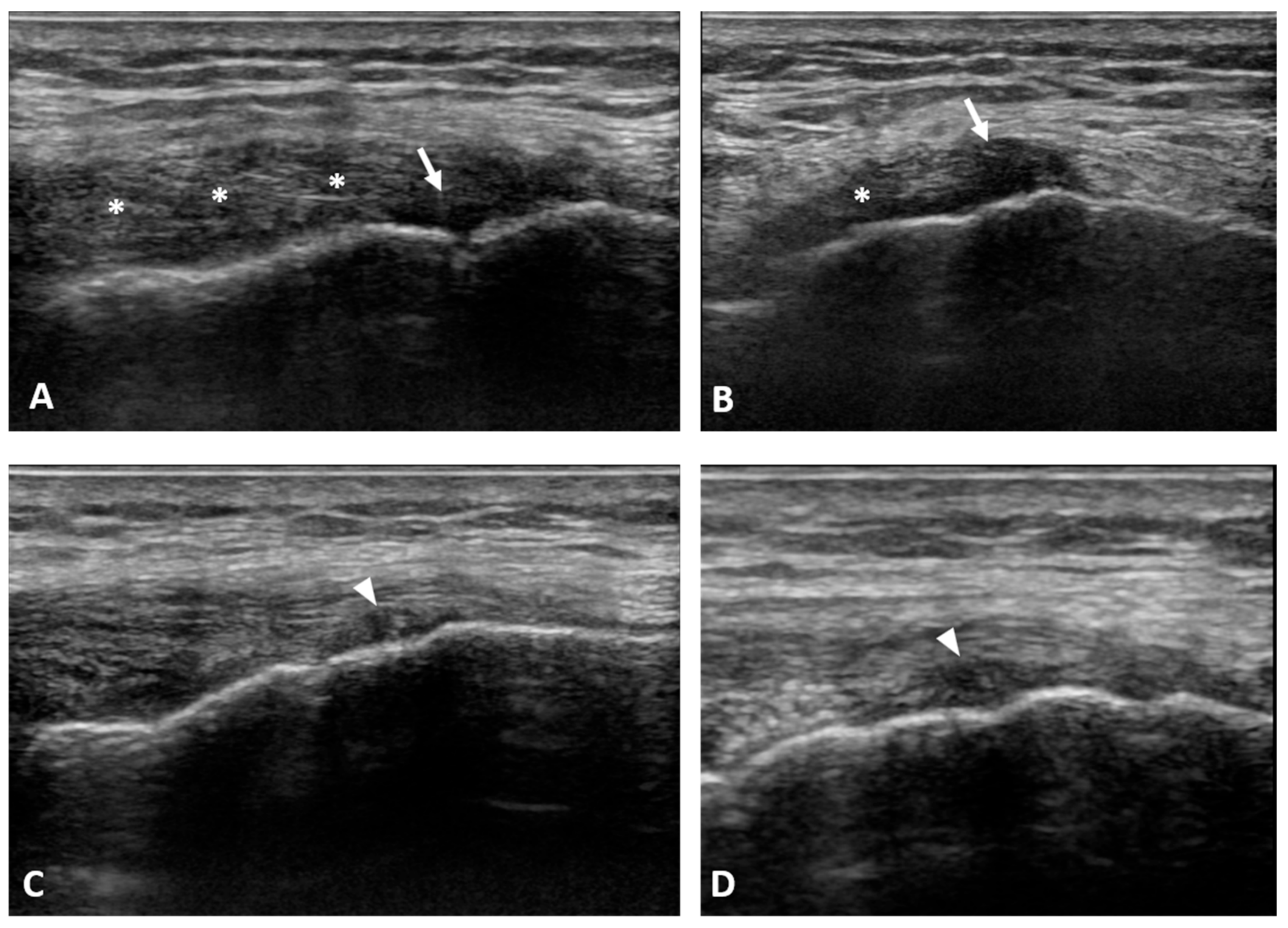
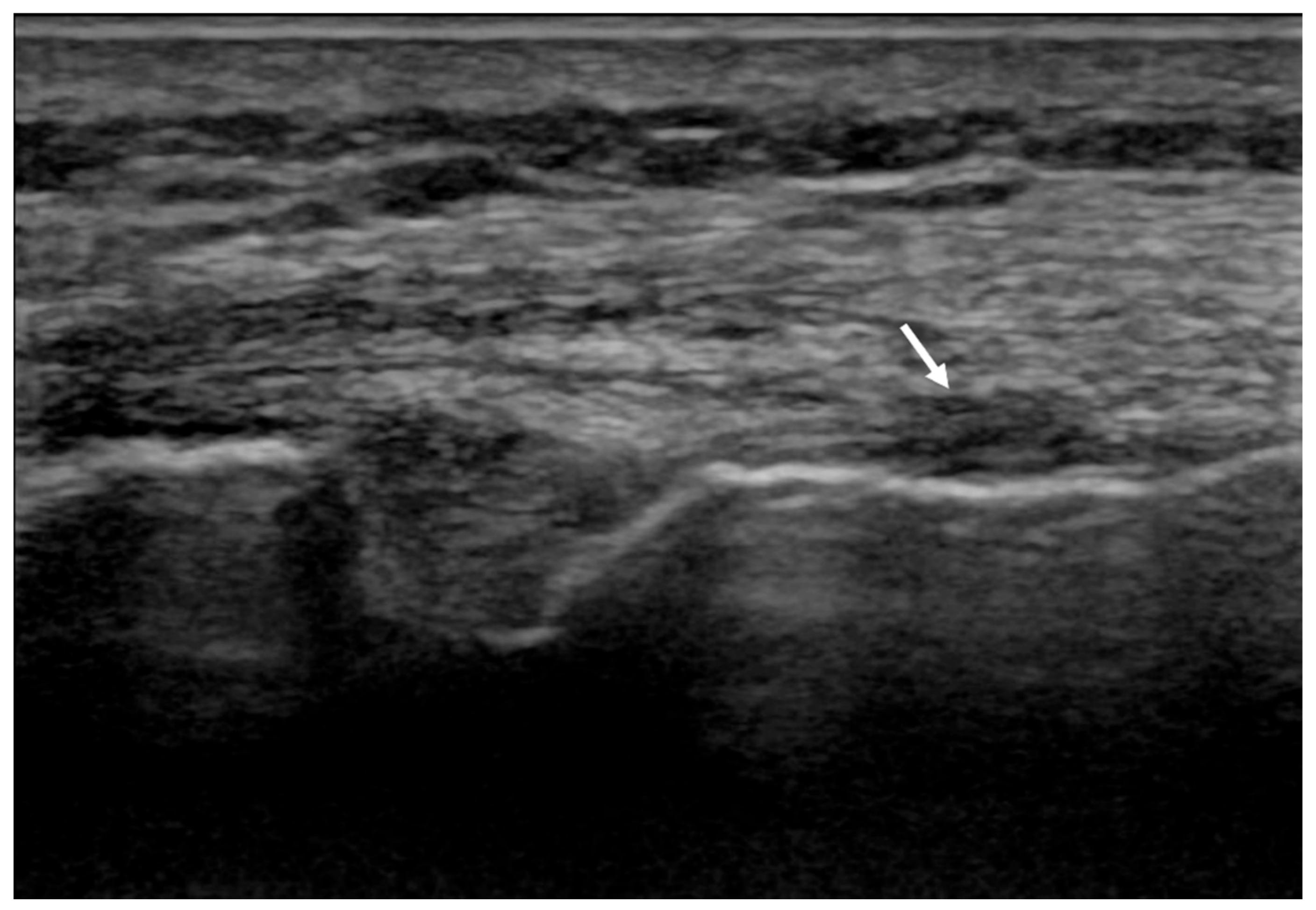
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Memarzadeh, A.; Melton, J.T. Medial collateral ligament of the knee: Anatomy, management and surgical techniques for reconstruction. Orthop. Trauma 2019, 33, 91–99. [Google Scholar] [CrossRef]
- Delong, J.M.; Waterman, B.R. Surgical Techniques for the Reconstruction of Medial Collateral Ligament and Posteromedial Corner Injuries of the Knee: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 2258–2272.e1. [Google Scholar] [CrossRef] [PubMed]
- Fetto, J.F.; Marshall, J.L. Medial collateral ligament injuries of the knee: A rationale for treatment. Clin. Orthop. Relat. Res. 1978, 132, 206–218. [Google Scholar] [CrossRef]
- Varelas, A.N.; Erickson, B.J.; Cvetanovich, G.L.; Bach, B.R. Medial Collateral Ligament Reconstruction in Patients with Medial Knee Instability: A Systematic Review. Orthop. J. Sports Med. 2017, 5, 2325967117703920. [Google Scholar] [CrossRef]
- American Medical Association. Committee on the Medical Aspects of Sports. In Standard Nomenclature of Athletic Injuries; American Medical Association: Chicago, IL, USA, 1966; pp. 99–100. [Google Scholar]
- Reider, B.; Sathy, M.R.; Talkington, J.; Blyznak, N.; Kollias, S. Treatment of Isolated Medial Collateral Ligament Injuries in Athletes with Early Functional Rehabilitation: A Five-year Follow-up Study. Am. J. Sports Med. 1994, 22, 470–477. [Google Scholar] [CrossRef]
- Indelicato, P.A.; Hermansdorfer, J.; Huegel, M. Nonoperative Management of Complete Tears of the Medial Collateral Ligament of the Knee in Intercollegiate Football Players. Clin. Orthop. Relat. Res. 1990, 256, 174–177. [Google Scholar] [CrossRef]
- Phisitkul, P.; James, S.L.; Wolf, B.; Amendola, A. MCL injuries of the knee: Current concepts review. Iowa Orthop. J. 2006, 26, 77–90. [Google Scholar]
- Simplicio, C.L.; Purita, J.; Murrell, W.; Santos, G.S.; dos Santos, R.G.; Lana, J.F.S.D. Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J. Clin. Orthop. Trauma 2020, 11, S309–S318. [Google Scholar] [CrossRef]
- Schroeder, A.N.; Tenforde, A.S.; Jelsing, E.J. Extracorporeal Shockwave Therapy in the Management of Sports Medicine Injuries. Curr. Sports Med. Rep. 2021, 20, 298–305. [Google Scholar] [CrossRef]
- Tognolo, L.; Giordani, F.; Biz, C.; Bernini, A.; Ruggieri, P.; Stecco, C.; Frigo, A.C.M.S. Myofascial points treatment with focused extracorporeal shock waves (f-ESW) for plantar fasciitis: An open label randomized clinical trial. Eur. J. Phys. Rehabil. Med. 2021. [Google Scholar] [CrossRef]
- Bosch, G.; de Mos, M.; van Binsbergen, R.; van Schie, H.T.M.; van de Lest, C.H.A.; van Weeren, P.R. The effect of focused extracorporeal shock wave therapy on collagen matrix and gene expression in normal tendons and ligaments. Equine Vet. J. 2009, 41, 335–341. [Google Scholar] [CrossRef]
- Caminoto, E.H.; Alves, A.L.G.; Amorim, R.L.; Thomassian, A.; Hussni, C.A.; Nicoletti, J.L.M. Ultrastructural and immunocytochemical evaluation of the effects of extracorporeal shock wave treatment in the hind limbs of horses with experimentally induced suspensory ligament desmitis. Am. J. Vet. Res. 2005, 66, 892–896. [Google Scholar] [CrossRef]
- Paavola, M.; Kannus, P.; Järvinen, T.A.; Khan, K.; Józsa, L.J.M. Achilles tendinopathy. J. Bone Jt. Surg. Am. 2002, 84, 2062–2076. [Google Scholar] [CrossRef]
- Maffulli, N.; Kader, D. Tendinopathy of tendo Achillis. J. Bone Jt. Surg. Br. 2002, 84, 1–8. [Google Scholar] [CrossRef]
- Reider, B. Medial Collateral Ligament Injuries in Athletes. Sports Med. 1996, 21, 147–156. [Google Scholar] [CrossRef]
- Anderson, D.R.; Weiss, J.A.; Takai, S.; Ohland, K.J.; Woo, S.L.-Y. Healing of the medial collateral ligament following a triad injury: A biomechanical and histological study of the knee in rabbits. J. Orthop. Res. 1992, 10, 485–495. [Google Scholar] [CrossRef]
- Lin, T.-Y.; Chen, J.-T.; Chen, Y.-Y.; Chen, T.-W.; Lee, C.-L.; Chen, C.-H.; Huang, M.-H. The efficacy of ultrasound-guided extracorporeal shockwave therapy in patients with cervical spondylosis and nuchal ligament calcification. Kaohsiung J. Med. Sci. 2015, 31, 337–343. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.-J.; Ko, J.-Y.; Chou, W.-Y.; Hsu, S.-L.; Ko, S.-F.; Huang, C.-C.; Chang, H.-W. Shockwave therapy improves anterior cruciate ligament reconstruction. J. Surg. Res. 2014, 188, 110–118. [Google Scholar] [CrossRef]
- Leong, N.L.; Kator, J.L.; Clemens, T.L.; James, A.; Dds, M.E.; Jiang, J. Tendon and Ligament Healing and Current Approaches to Tendon and Ligament Regeneration. J. Orthop. Res. 2020, 38, 7–12. [Google Scholar] [CrossRef]
- Bobzin, L.; Roberts, R.R.; Chen, H.-J.; Crump, J.G.; Merrill, A.E. Development and maintenance of tendons and ligaments. Development 2021, 148, 186916. [Google Scholar] [CrossRef]
- Rumian, A.P.; Wallace, A.L.; Birch, H. Tendons and ligaments are anatomically distinct but overlap in molecular and morphological features—A comparative study in an ovine model. J. Orthop. Res. 2007, 25, 458–464. [Google Scholar] [CrossRef]
- Waguespack, R.W.; Burba, D.J.; Hubert, J.D.; Vidal, M.A.; Lomax, L.G.; Chirgwin, S.R.; Lopez, M.J. Effects of Extracorporeal Shock Wave Therapy on Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon in the Horse. Vet. Surg. 2011, 40, 450–456. [Google Scholar] [CrossRef]
- Weihs, A.M.; Fuchs, C.; Teuschl, A.; Hartinger, J.; Slezak, P.; Mittermayr, R.; Redl, H.; Junger, W.G.; Sitte, H.; Rünzler, D. Shock Wave Treatment Enhances Cell Proliferation and Improves Wound Healing by ATP Release-coupled Extracellular Signal-regulated Kinase (ERK) Activation. J. Biol. Chem. 2014, 289, 27090–27104. [Google Scholar] [CrossRef] [Green Version]
- Burnstock, G.; Verkhratsky, A. Long-term (trophic) purinergic signalling: Purinoceptors control cell proliferation, differentiation and death. Cell Death Dis. 2010, 1, e9. [Google Scholar] [CrossRef] [Green Version]
- Werner, F.; Feinberg, M.W.; Jain, M.K.; Sibinga, N.E.; Wiesel, P.; Wang, H.; Lee, M.E. Transforming growth factor-b1 inhibits cytokinemediated induction of human metalloelastase in marcophages. J. Biol. Chem. 2000, 275, 25766–25773. [Google Scholar] [CrossRef] [Green Version]
- Lana, J.F.; Macedo, A.; Ingrao, I.L.G.; Huber, S.C.; Santos, G.S.; Santana, M.H.A. Leukocyte-rich PRP for knee osteoarthritis: Current concepts. J. Clin. Orthop. Trauma 2019, 10, S179–S182. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tognolo, L.; Coraci, D.; Bernini, A.; Masiero, S. Treatment of Medial Collateral Ligament Injuries of the Knee with Focused Extracorporeal Shockwave Therapy: A Case Report. Appl. Sci. 2022, 12, 234. https://doi.org/10.3390/app12010234
Tognolo L, Coraci D, Bernini A, Masiero S. Treatment of Medial Collateral Ligament Injuries of the Knee with Focused Extracorporeal Shockwave Therapy: A Case Report. Applied Sciences. 2022; 12(1):234. https://doi.org/10.3390/app12010234
Chicago/Turabian StyleTognolo, Lucrezia, Daniele Coraci, Andrea Bernini, and Stefano Masiero. 2022. "Treatment of Medial Collateral Ligament Injuries of the Knee with Focused Extracorporeal Shockwave Therapy: A Case Report" Applied Sciences 12, no. 1: 234. https://doi.org/10.3390/app12010234
APA StyleTognolo, L., Coraci, D., Bernini, A., & Masiero, S. (2022). Treatment of Medial Collateral Ligament Injuries of the Knee with Focused Extracorporeal Shockwave Therapy: A Case Report. Applied Sciences, 12(1), 234. https://doi.org/10.3390/app12010234








