A Simulation Analysis of an Influenza Vaccine Production Plant in Areas of High Humanitarian Flow. A Preliminary Study for the Region of Norte de Santander (Colombia)
Abstract
:1. Introduction
2. Materials and Methods
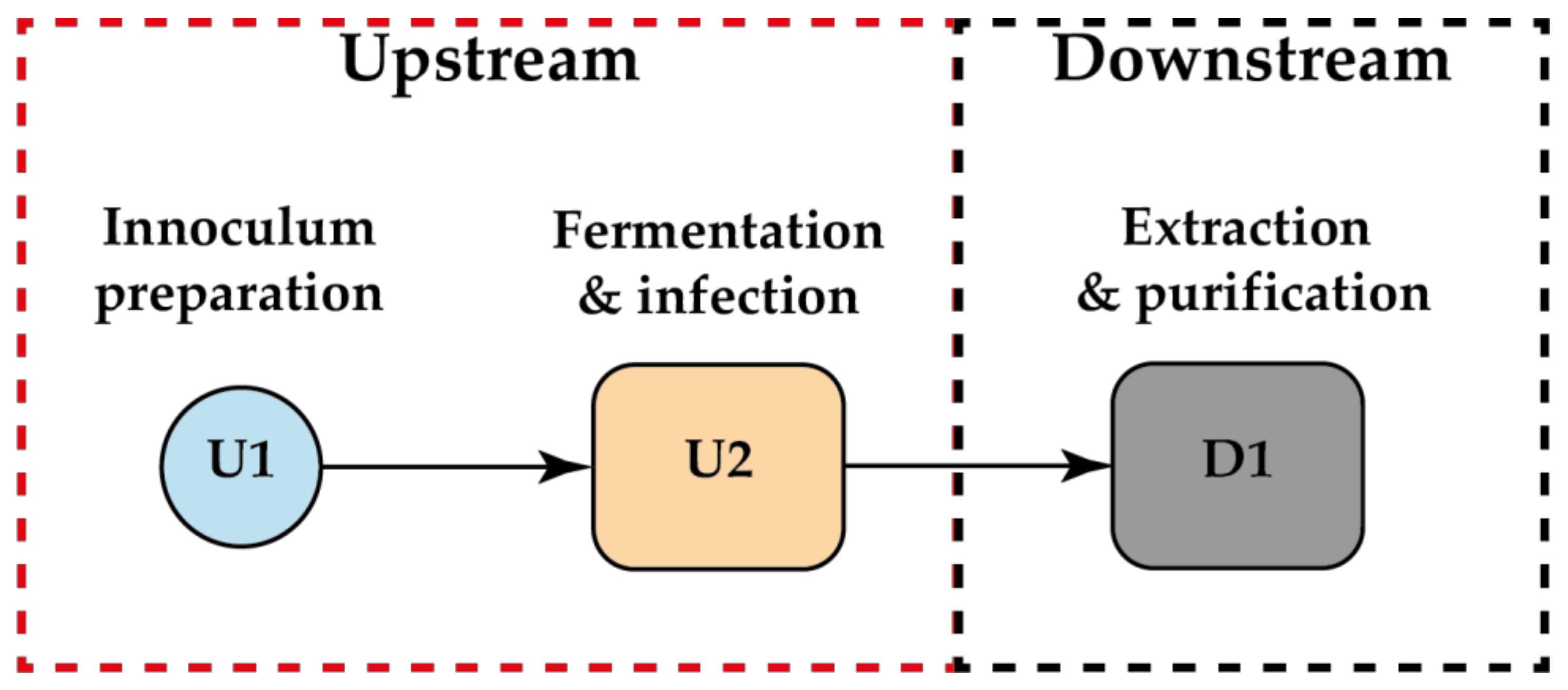
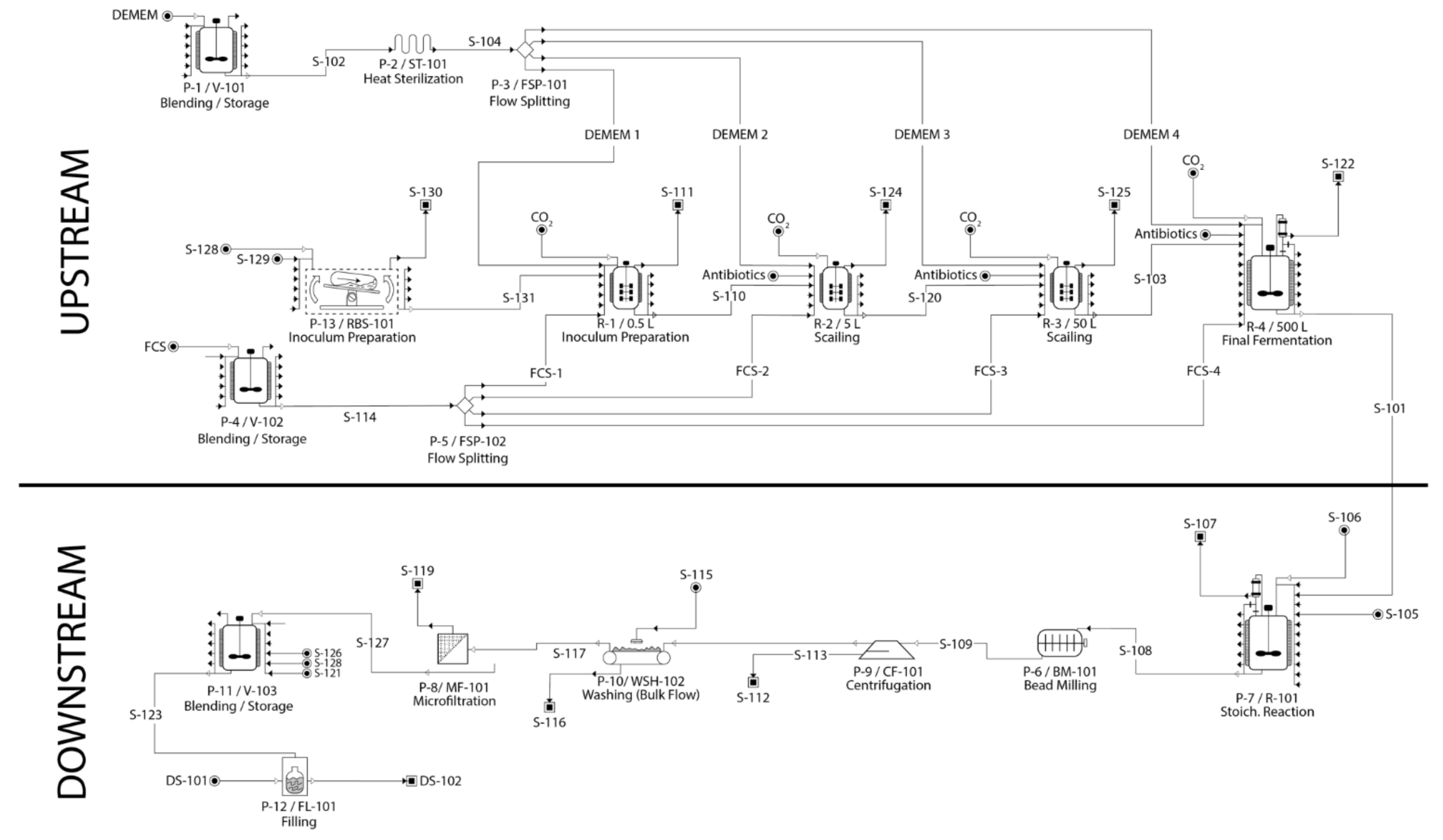
2.1. Process Description
2.2. Plant Simulation
3. Results
3.1. Upstream
3.2. Downstream
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Reed, C.; Chaves, S.S.; Kirley, P.D.; Emerson, R.; Aragon, D.; Hancock, E.B.; Butler, L.; Baumbach, J.; Hollick, G.; Bennett, N.M.; et al. Estimating Influenza Disease Burden from Population-Based Surveillance Data in the United States. PLoS ONE 2015, 10, e0118369. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Salud. Acute Respiratory Infection Event Report, Colombia, 2019. Available online: https://www.ins.gov.co/buscador-eventos/Informesdeevento/INFECCIÓN%20RESPIRATORIA%20AGUDA_2019.pdf (accessed on 11 September 2021).
- International Organization for Migration. DTM Survey—Vocation of Venezuelan Population to Stay in Colombia, Colombia, 2020. Available online: https://colombia.iom.int/sites/colombia/files/EYE/Vocacion/INFORME%20DTM%20VILLA%20DEL%20ROSARIO.pdf (accessed on 10 December 2021).
- Ministerio de Salud y Protección Social de Colombia. Ten-Year Public Health Plan 2012–2021 of Colombia. 2012. Available online: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=8777:2013-plan-decenal-salud-publica-2012-2021-colombia&Itemid=40264&lang=es (accessed on 11 September 2021).
- Ministerio de Salud y Protección Social de Colombia. ABC of the Ten-Year Public Health Plan. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/ED/PSP/IMP_4feb+ABCminsalud.pdf (accessed on 11 September 2021).
- Instituto Departamental de Salud de Norte de Santander. Health Situation Analysis with the Social Determinants Model Norte de Santander Department 2019, Colombia. 2019. Available online: https://ids.gov.co/web/2020/TRANSPARENCIA/ASIS_DPTAL_NTE%20SDER_2019_ABRIL_2020.pdf (accessed on 10 December 2021).
- Athimulam, A.; Kumaresan, S.; Foo, D.; Sarmidi, M.; Aziz, R. Modelling and Optimization of Eurycoma longifolia Water Extract Production. Food Bioprod. Process. 2006, 84, 139–149. [Google Scholar] [CrossRef] [Green Version]
- Sparrow, E.; Wood, J.G.; Chadwick, C.; Newall, A.T.; Torvaldsen, S.; Moen, A.; Torelli, G. Global production capacity of seasonal and pandemic influenza vaccines in 2019. Vaccine 2021, 39, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Jiang, B.; Patel, M.; Glass, R.I. Polio endgame: Lessons for the global rotavirus vaccination program. Vaccine 2019, 37, 3040–3049. [Google Scholar] [CrossRef]
- Canizales, L.; Rojas, F.; Pizarro, C.A.; Caicedo-Ortega, N.H.; Villegas-Torres, M.F. SuperPro Designer®, User-Oriented Software Used for Analyzing the Techno-Economic Feasibility of Electrical Energy Generation from Sugarcane Vinasse in Colombia. Processes 2020, 8, 1180. [Google Scholar] [CrossRef]
- Ernst, S.; Garro, O.A.; Winkler, S.; Venkataraman, G.; Langer, R.; Cooney, C.L.; Sasisekharan, R. Process simulation for recombinant protein production: Cost estimation and sensitivity analysis for heparinase I expressed in Escherichia coli. Biotechnol. Bioeng. 1997, 53, 575–582. [Google Scholar] [CrossRef]
- Huang, D.; Xia-Hou, K.; Liu, X.-P.; Zhao, L.; Fan, L.; Ye, Z.; Tan, W.-S.; Luo, J.; Chen, Z. Rational design of medium supplementation strategy for improved influenza viruses production based on analyzing nutritional requirements of MDCK Cells. Vaccine 2014, 32, 7091–7097. [Google Scholar] [CrossRef]
- Genzel, Y. Designing cell lines for viral vaccine production: Where do we stand? Biotechnol. J. 2015, 10, 728–740. [Google Scholar] [CrossRef]
- Li, I.; Chan, K.; To, K.; Wong, S.; Ho, P.L.; Lau, S.K.P.; Woo, P.C.Y.; Tsoi, H.; Chan, J.F.-W.; Cheng, V.; et al. Differential susceptibility of different cell lines to swine-origin influenza A H1N1, seasonal human influenza A H1N1, and avian influenza A H5N1 viruses. J. Clin. Virol. 2009, 46, 325–330. [Google Scholar] [CrossRef]
- Fontana, D.; Marsili, F.; Garay, E.; Battagliotti, J.; Etcheverrigaray, M.; Kratje, R.; Prieto, C. A simplified roller bottle platform for the production of a new generation VLPs rabies vaccine for veterinary applications. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 70–75. [Google Scholar] [CrossRef]
- Dewannieux, M.; Ribet, D.; Heidmann, T. Risks linked to endogenous retroviruses for vaccine production: A general overview. Biologicals 2010, 38, 366–370. [Google Scholar] [CrossRef]
- George, M.; Farooq, M.; Dang, T.; Cortes, B.; Liu, J.; Maranga, L. Production of cell culture (MDCK) derived live attenuated influenza vaccine (LAIV) in a fully disposable platform process. Biotechnol. Bioeng. 2010, 106, 906–917. [Google Scholar] [CrossRef]
- Limonta, M.; Krajnc, N.L.; Vidič, U.; Zumalacárregui, L. Simulation for the recovery of plasmid for a DNA vaccine. Biochem. Eng. J. 2013, 80, 14–18. [Google Scholar] [CrossRef]
- Petrides, D.; Carmichael, D.; Siletti, C.; Koulouris, A. Biopharmaceutical Process Optimization with Simulation and Scheduling Tools. Bioengineering 2014, 1, 154. [Google Scholar] [CrossRef]
- Liu, J.; Mani, S.; Schwartz, R.; Richman, L.; Tabor, D.E. Cloning and assessment of tumorigenicity and oncogenicity of a Madin–Darby canine kidney (MDCK) cell line for influenza vaccine production. Vaccine 2010, 28, 1285–1293. [Google Scholar] [CrossRef]
- Guerriero, V. Power Law Distribution: Method of Multi-Scale Inferential Statistics. J. Mod. Math. Front. JMMF 2012, 1, 21–28. [Google Scholar]
- Youil, R.; Su, Q.; Toner, T.; Szymkowiak, C.; Kwan, W.-S.; Rubin, B.; Petrukhin, L.; Kiseleva, I.; Shaw, A.; DiStefano, D. Comparative study of influenza virus replication in Vero and MDCK cell lines. J. Virol. Methods 2004, 120, 23–31. [Google Scholar] [CrossRef]
- Valero, Y.; Olveira, J.; López-Vázquez, C.; Dopazo, C.; Bandín, I. BEI Inactivated Vaccine Induces Innate and Adaptive Responses and Elicits Partial Protection upon Reassortant Betanodavirus Infection in Senegalese Sole. Vaccines 2021, 9, 458. [Google Scholar] [CrossRef]
- Moyle, P.M. Progress in Vaccine Development. Curr. Protoc. Microbiol. 2015, 36, 18.1.1–18.1.26. [Google Scholar] [CrossRef]
- Frey, S.; Vesikari, T.; Szymczakiewicz-Multanowska, A.; Lattanzi, M.; Izu, A.; Groth, N.; Holmes, S. Clinical Efficacy of Cell Culture–Derived and Egg-Derived Inactivated Subunit Influenza Vaccines in Healthy Adults. Clin. Infect. Dis. 2010, 51, 997–1004. [Google Scholar] [CrossRef]
- Bart, S.; Cannon, K.; Herrington, D.; Mills, R.; Forleo-Neto, E.; Lindert, K.; Mateen, A.A. Immunogenicity and safety of a cell culture-based quadrivalent influenza vaccine in adults: A Phase III, double-blind, multicenter, randomized, non-inferiority study. Hum. Vaccines Immunother. 2016, 12, 2278–2288. [Google Scholar] [CrossRef] [Green Version]
- Hartvickson, R.; Cruz, M.; Ervin, J.; Brandon, D.; Forleo-Neto, E.; Dagnew, A.F.; Chandra, R.; Lindert, K.; Mateen, A.A. Non-inferiority of mammalian cell-derived quadrivalent subunit influenza virus vaccines compared to trivalent subunit influenza virus vaccines in healthy children: A phase III randomized, multicenter, double-blind clinical trial. Int. J. Infect. Dis. 2015, 41, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Ambrozaitis, A.; Groth, N.; Bugarini, R.; Sparacio, V.; Podda, A.; Lattanzi, M. A novel mammalian cell-culture technique for consistent production of a well-tolerated and immunogenic trivalent subunit influenza vaccine. Vaccine 2009, 27, 6022–6029. [Google Scholar] [CrossRef]
- Szymczakiewicz-Multanowska, A.; Groth, N.; Bugarini, R.; Lattanzi, M.; Casula, D.; Hilbert, A.; Tsai, T.; Podda, A. Safety and Immunogenicity of a Novel Influenza Subunit Vaccine Produced in Mammalian Cell Culture. J. Infect. Dis. 2009, 200, 841–848. [Google Scholar] [CrossRef] [Green Version]
- Ministerio de Salud y Protección Social de Colombia. Guidelines for the Management and Administration of the Expanded Program on Immunization—API—2020, Colombia, 2020. Available online: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/PP/ET/lineamientos-nacionales-pai2020.pdf (accessed on 10 December 2021).
- Aliya Mohamad Ros, F.N.; Rahman, N.A.; Ali, J.M.; Anuar, N.; Abdullah, S.R.B.S.; Yusoff, A.F.B.J. Comparative Study between Avian Cell and Mammalian Cell in Production of Influenza Vaccine Shariah Compliance. IOP Conf. Series Mater. Sci. Eng. 2020, 778, 12029. [Google Scholar] [CrossRef]
- Farid, S.S. Process economics of industrial monoclonal antibody manufacture. J. Chromatogr. B 2007, 848, 8–18. [Google Scholar] [CrossRef]
- Nestola, P.; Peixoto, C.; Silva, R.R.J.S.; Alves, P.M.; Mota, J.P.B.; Carrondo, M.J.T. Improved virus purification processes for vaccines and gene therapy. Biotechnol. Bioeng. 2015, 112, 843–857. [Google Scholar] [CrossRef]
- Yang, W.C.; Lu, J.; Kwiatkowski, C.; Yuan, H.; Kshirsagar, R.; Ryll, T.; Huang, Y.-M. Perfusion Seed Cultures Improve Bio-pharmaceutical Fed-Batch Production Capacity and Product Quality. Biotechnol. Prog. 2014, 30, 616–625. [Google Scholar] [CrossRef]
- Tapia, F.; Vázquez-Ramírez, D.; Genzel, Y.; Reichl, U. Bioreactors for high cell density and continuous multi-stage cultivations: Options for process intensification in cell culture-based viral vaccine production. Appl. Microbiol. Biotechnol. 2016, 100, 2121–2132. [Google Scholar] [CrossRef] [Green Version]
- Xu, J.; Xu, X.; Huang, C.; Angelo, J.; Oliveira, C.L.; Xu, M.; Xu, X.; Temel, D.; Ding, J.; Ghose, S.; et al. Biomanufacturing evolution from conventional to intensified processes for productivity improvement: A case study. MAbs 2020, 12, 1770669. [Google Scholar] [CrossRef]
- Rubio, A.P.; Eiros, J.M. Cell culture-derived flu vaccine: Present and future. Hum. Vaccines Immunother. 2018, 14, 1874–1882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, B.Y.; Connor, D.L.; Wateska, A.R.; Norman, B.A.; Rajgopal, J.; Cakouros, B.E.; Chen, S.-I.; Claypool, E.G.; Haidari, L.A.; Karir, V.; et al. Landscaping the structures of GAVI country vaccine supply chains and testing the effects of radical redesign. Vaccine 2015, 33, 4451–4458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, S.-I.; Norman, B.A.; Rajgopal, J.; Assi, T.M.; Lee, B.Y.; Brown, S. A planning model for the WHO-EPI vaccine distribution network in developing countries. IIE Trans. 2014, 46, 853–865. [Google Scholar] [CrossRef]
- Haidari, L.A.; Connor, D.L.; Wateska, A.R.; Brown, S.T.; Mueller, L.E.; Norman, B.A.; Schmitz, M.M.; Paul, P.; Rajgopal, J.; Welling, J.S.; et al. Augmenting Transport versus Increasing Cold Storage to Improve Vaccine Supply Chains. PLoS ONE 2013, 8, e64303. [Google Scholar] [CrossRef]
- Lemmens, S.; Decouttere, C.; Vandaele, N.; Bernuzzi, M. A review of integrated supply chain network design models: Key issues for vaccine supply chains. Chem. Eng. Res. Des. 2016, 109, 366–384. [Google Scholar] [CrossRef]
| Items | (USD $) |
|---|---|
| 1. Equipment Purchase Cost | 7,755,000.00 |
| 2. Installation | 2,004,000.00 |
| 3. Process Piping | 1,680,000.00 |
| 4. Instrumentation | 1,921,000.00 |
| 5. Insulation | 144,000.00 |
| 6. Electrical | 480,000.00 |
| 7. Buildings | 2,161,000.00 |
| 8. Yard Improvement | 720,000.00 |
| 9. Auxiliary Facilities | 1,921,000.00 |
| Total | 18,786,000.00 |
| Items | ($) |
|---|---|
| 10. Engineering | 3,958,000.00 |
| 11. Construction | 5,541,000.00 |
| Total | 9,499,000.00 |
| Items | ($) |
|---|---|
| 12. Contractor’s Fee | 1,267,000.00 |
| 13. Contingency | 2,533,000.00 |
| CFC = 12 + 13 | 3,800,000.00 |
| Operator | Labor (h/yr) | Labor (h/h) | Labor (h/kg MP) |
|---|---|---|---|
| V-101:P-I | 11,314.29 | 1.43 | N/A |
| ST-IOI:p-2 | 5657.14 | 0.71 | N/A |
| 50 L:R-3. | 11,314.29 | 1.43 | N/A |
| 5L:R-2 | 11,312.29 | 1.43 | N/A |
| 500:R-4 | 11,314.29 | 1.43 | N/A |
| O,5L:R-1 | 11,312.29 | 1.43 | N/A |
| V-102:P-4 | 11,314.29 | 1.43 | N/A |
| R-IOI:P-7 | 11,312.29 | 1.43 | N/A |
| BM-IOI:P-6 | 5657.14 | 0.71 | N/A |
| CF-IOI:P-9 | 1131.43 | 0.14 | N/A |
| WSH-102:P-10 | 5657.14 | 0.71 | N/A |
| MF-IOI:P-8 | 13,200.00 | 1.67 | N/A |
| V-103:P-11 | 11,314.29 | 1.43 | N/A |
| FL-IOI:P-12 | 565.71 | 0.07 | N/A |
| RBS-IOI:P-13. | 1346.00 | 0.17 | N/A |
| Section Total | 123,728.86 | 15.62 | NIA |
| TOTAL | 123,728.86 | 15.62 | N/A |
| Bulk Material | Unit Cost ($) | Annual Amount (kg) | Annual Cost ($) | % |
|---|---|---|---|---|
| CO2 | 0.15 | 33,342.91 | 5001.44 | 0.00 |
| DMEM | 140.00 | 4,356,000.00 | 609,840,000.00 | 34.75 |
| DPBS | 2704.68 | 15,840.00 | 42,842,131.20 | 2.45 |
| FCS | 680.00 | 475,200.00 | 323,136,000.00 | 18.40 |
| MDCK | 320.00 | 39,600.00 | 12,672,000.00 | 0.71 |
| Penicillin/strep | 250.10 | 3,064,545.92 | 766,136,492.50 | 43.65 |
| Potassium alum | 0.18 | 616,713.92 | 111,008.51 | 0.02 |
| VIRUS | 1458.00 | 79.2 | 115,473.60 | 0.02 |
| TOTAL | 976,095,107.25 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Contreras-Ropero, J.E.; Ruiz-Roa, S.L.; García-Martínez, J.B.; Urbina-Suarez, N.A.; López-Barrera, G.L.; Barajas-Solano, A.F.; Zuorro, A. A Simulation Analysis of an Influenza Vaccine Production Plant in Areas of High Humanitarian Flow. A Preliminary Study for the Region of Norte de Santander (Colombia). Appl. Sci. 2022, 12, 183. https://doi.org/10.3390/app12010183
Contreras-Ropero JE, Ruiz-Roa SL, García-Martínez JB, Urbina-Suarez NA, López-Barrera GL, Barajas-Solano AF, Zuorro A. A Simulation Analysis of an Influenza Vaccine Production Plant in Areas of High Humanitarian Flow. A Preliminary Study for the Region of Norte de Santander (Colombia). Applied Sciences. 2022; 12(1):183. https://doi.org/10.3390/app12010183
Chicago/Turabian StyleContreras-Ropero, Jefferson E., Silvia L. Ruiz-Roa, Janet B. García-Martínez, Néstor A. Urbina-Suarez, Germán L. López-Barrera, Andrés F. Barajas-Solano, and Antonio Zuorro. 2022. "A Simulation Analysis of an Influenza Vaccine Production Plant in Areas of High Humanitarian Flow. A Preliminary Study for the Region of Norte de Santander (Colombia)" Applied Sciences 12, no. 1: 183. https://doi.org/10.3390/app12010183
APA StyleContreras-Ropero, J. E., Ruiz-Roa, S. L., García-Martínez, J. B., Urbina-Suarez, N. A., López-Barrera, G. L., Barajas-Solano, A. F., & Zuorro, A. (2022). A Simulation Analysis of an Influenza Vaccine Production Plant in Areas of High Humanitarian Flow. A Preliminary Study for the Region of Norte de Santander (Colombia). Applied Sciences, 12(1), 183. https://doi.org/10.3390/app12010183











